Feasibility and Effectiveness of a Novel Intervention Integrating Physical Therapy Exercise and Dance Movement Therapy on Fall Risk in Community-Dwelling Older Women: A Randomized Pilot Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.2.1. Eligibility Criteria
2.2.2. Random Assignment
2.3. Interventions- PTE+DMT and PTE
2.4. Measurements
2.4.1. Participant Characteristics
2.4.2. Fall Risk
2.4.3. Functioning in ADL
2.4.4. Objective Balance
2.4.5. FOF
2.4.6. FSe
2.4.7. Balance Confidence
2.4.8. FOF Avoidance Behavior
2.4.9. Self-Perceived Health Status
2.4.10. Therapist–Patient Bond
2.4.11. Home Exercise Adherence
2.5. Procedure
2.6. Data Analysis
2.7. Ethical Issues
3. Results
3.1. Participants
3.2. Pre-Test and Post-Test between Groups Differences
3.3. Pre-Test and Post-Test within-Groups Differences
3.4. Comparison of Percentage Changes between Groups
3.5. Sample Size for a Future Study
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Falls. Available online: https://www.who.int/news-room/fact-sheets/detail/falls (accessed on 26 April 2021).
- Montero-Odasso, M.; van der Velde, N.; Martin, F.C.; Petrovic, M.; Tan, M.P.; Ryg, J.; Aguilar-Navarro, S.; Alexander, N.B.; Becker, C.; Blain, H.; et al. World guidelines for falls prevention and management for older adults: A global initiative. Age Ageing 2022, 51, afac205. [Google Scholar] [CrossRef] [PubMed]
- Ganz, D.A.; Yuan, A.H.; Greene, E.J.; Latham, N.K.; Araujo, K.; Siu, A.L.; Magaziner, J.; Gurwitz, J.H.; Wu, A.W.; Alexander, N.B.; et al. Effect of the STRIDE fall injury prevention intervention on falls, fall injuries, and health-related quality of life. J. Am. Geriatr. Soc. 2022, 70, 3221–3229. [Google Scholar] [CrossRef] [PubMed]
- Appeadu, M.; Bordoni, B. Falls and Fall Prevention in the Elderly. Available online: https://www.statpearls.com/ArticleLibrary/viewarticle/79102 (accessed on 7 August 2021).
- Sharif, S.I.; Al-Harbi, A.B.; Al-Shihabi, A.M.; Al-Daour, D.S.; Sharif, R.S. Falls in the elderly: Assessment of prevalence and risk factors. Pharm. Pract. 2018, 16, 1206. [Google Scholar] [CrossRef]
- World Health Organization. Ageing and Health. Available online: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health (accessed on 1 October 2022).
- Byun, M.; Kim, J.; Kim, J.E. Physical and psychological factors contributing to incidental falls in older adults Who perceive themselves as unhealthy: A cross-sectional study. Int. J. Environ. Res. Public Health 2021, 18, 3738. [Google Scholar] [CrossRef]
- Zhang, Y.; Xiong, Y.; Yu, Q.; Shen, S.; Chen, L.; Lei, X. The activity of daily living (ADL) subgroups and health impairment among Chinese elderly: A latent profile analysis. BMC Geriatr. 2021, 21, 30. [Google Scholar] [CrossRef]
- Cunningham, C.; O’Sullivan, R.; Caserotti, P.; Tully, M.A. Consequences of physical inactivity in older adults: A systematic review of reviews and meta-analyses. Scand. J. Med. Sci. Sport. 2020, 30, 816–827. [Google Scholar] [CrossRef]
- Angulo, J.; El Assar, M.; Alvarez-Bustos, A.; Rodriguez-Manas, L. Physical activity and exercise: Strategies to manage frailty. Redox Biol. 2020, 35, 101513. [Google Scholar] [CrossRef]
- Sherrington, C.; Fairhall, N.J.; Wallbank, G.K.; Tiedemann, A.; Michaleff, Z.A.; Howard, K.; Clemson, L.; Hopewell, S.; Lamb, S.E. Exercise for preventing falls in older people living in the community. Cochrane Database Syst. Rev. 2019, 1, CD012424. [Google Scholar] [CrossRef]
- Chiu, H.L.; Yeh, T.T.; Lo, Y.T.; Liang, P.J.; Lee, S.C. The effects of the Otago Exercise Programme on actual and perceived balance in older adults: A meta-analysis. PLoS ONE 2021, 16, e0255780. [Google Scholar] [CrossRef]
- Kocic, M.; Stojanovic, Z.; Nikolic, D.; Lazovic, M.; Grbic, R.; Dimitrijevic, L.; Milenkovic, M. The effectiveness of group Otago exercise program on physical function in nursing home residents older than 65years: A randomized controlled trial. Arch. Gerontol. Geriatr. 2018, 75, 112–118. [Google Scholar] [CrossRef]
- Lee, S.H.; Yu, S. Effectiveness of multifactorial interventions in preventing falls among older adults in the community: A systematic review and meta-analysis. Int. J. Nurs. Stud. 2020, 106, 103564. [Google Scholar] [CrossRef] [PubMed]
- Pettersson, B.; Lundin-Olsson, L.; Skelton, D.A.; Liv, P.; Zingmark, M.; Rosendahl, E.; Sandlund, M. Effectiveness of a self-managed digital exercise programme to prevent falls in older community-dwelling adults: Study protocol for the Safe Step randomised controlled trial. BMJ Open 2020, 10, e036194. [Google Scholar] [CrossRef] [PubMed]
- Hughes, C.C.; Kneebone, I.I.; Jones, F.; Brady, B. A theoretical and empirical review of psychological factors associated with falls-related psychological concerns in community-dwelling older people. Int. Psychogeriatr. 2015, 27, 1071–1087. [Google Scholar] [CrossRef] [PubMed]
- Pauelsen, M.; Jafari, H.; Strandkvist, V.; Nyberg, L.; Gustafsson, T.; Vikman, I.; Roijezon, U. Frequency domain shows: Fall-related concerns and sensorimotor decline explain inability to adjust postural control strategy in older adults. PLoS ONE 2020, 15, e0242608. [Google Scholar] [CrossRef]
- Pauelsen, M.; Nyberg, L.; Roijezon, U.; Vikman, I. Both psychological factors and physical performance are associated with fall-related concerns. Aging Clin. Exp. Res. 2018, 30, 1079–1085. [Google Scholar] [CrossRef]
- Young, W.R.; Mark Williams, A. How fear of falling can increase fall-risk in older adults: Applying psychological theory to practical observations. Gait Posture 2015, 41, 7–12. [Google Scholar] [CrossRef]
- Scheffer, A.C.; Schuurmans, M.J.; van Dijk, N.; van der Hooft, T.; de Rooij, S.E. Fear of falling: Measurement strategy, prevalence, risk factors and consequences among older persons. Age Ageing 2008, 37, 19–24. [Google Scholar] [CrossRef]
- Peeters, G.; Bennett, M.; Donoghue, O.A.; Kennelly, S.; Kenny, R.A. Understanding the aetiology of fear of falling from the perspective of a fear-avoidance model-A narrative review. Clin. Psychol. Rev. 2020, 79, 101862. [Google Scholar] [CrossRef]
- Rivasi, G.; Kenny, R.A.; Ungar, A.; Romero-Ortuno, R. Predictors of Incident Fear of Falling in Community-Dwelling Older Adults. J. Am. Med. Dir. Assoc. 2020, 21, 615–620. [Google Scholar] [CrossRef]
- Hajek, A.; König, H. What are the psychosocial consequences when fear of falling starts or ends? Evidence from an asymmetric fixed effects analysis based on longitudinal data from the general population. Int. J. Geriatr. Psychiatry 2020, 35, 1028–1035. [Google Scholar] [CrossRef]
- Schoene, D.; Heller, C.; Aung, Y.N.; Sieber, C.C.; Kemmler, W.; Freiberger, E. A systematic review on the influence of fear of falling on quality of life in older people: Is there a role for falls? Clin. Interv. Aging 2019, 14, 701–719. [Google Scholar] [CrossRef] [PubMed]
- Fang, Q.; Ghanouni, P.; Anderson, S.E.; Touchett, H.; Shirley, R.; Fang, F.; Fang, C. Effects of exergaming on balance of healthy older Adults: A systematic review and meta-analysis of randomized controlled trials. Games Health J. 2020, 9, 11–23. [Google Scholar] [CrossRef] [PubMed]
- Liu, M.; Hou, T.; Li, Y.; Sun, X.; Szanton, S.L.; Clemson, L.; Davidson, P.M. Fear of falling is as important as multiple previous falls in terms of limiting daily activities: A longitudinal study. BMC Geriatr. 2021, 21, 350. [Google Scholar] [CrossRef] [PubMed]
- Loft, C.C.; Jones, F.W.; Kneebone, I.I. Falls self-efficacy and falls incidence in community-dwelling older people: The mediating role of coping. Int. Psychogeriatr. 2018, 30, 727–733. [Google Scholar] [CrossRef] [PubMed]
- Kuo, C.T.; Chen, D.R.; Chen, Y.M.; Chen, P.Y. Validation of the short falls efficacy scale-international for Taiwanese community-dwelling older adults: Associations with fall history, physical frailty, and quality of life. Geriatr. Nurs. 2021, 42, 1012–1018. [Google Scholar] [CrossRef] [PubMed]
- McCarty, K.; Kennedy, W.; Logan, S.; Levy, S. Examining the relationship between falls self-efficacy and postural sway in community-dwelling older adults. J. Kinesiol. Wellness 2021, 10, 21–30. [Google Scholar] [CrossRef]
- Yoshikawa, A.; Ramirez, G.; Smith, M.L.; Lee, S.; Ory, M.G. Systematic review and meta-analysis of fear of falling and fall-related efficacy in a widely disseminated community-based fall prevention program. Arch. Gerontol. Geriatr. 2020, 91, 104235. [Google Scholar] [CrossRef]
- Argent, R.; Daly, A.; Caulfield, B. Patient involvement with home-based exercise programs: Can connected health interventions influence adherence? JMIR Mhealth Uhealth 2018, 6, e8518. [Google Scholar] [CrossRef]
- Bjerk, M.; Brovold, T.; Skelton, D.A.; Bergland, A. A falls prevention programme to improve quality of life, physical function and falls efficacy in older people receiving home help services: Study protocol for a randomised controlled trial. BMC Health Serv. Res. 2017, 17, 559. [Google Scholar] [CrossRef]
- de Groot, G.C.; Fagerstrom, L. Older adults’ motivating factors and barriers to exercise to prevent falls. Scand. J. Occup. Ther. 2011, 18, 153–160. [Google Scholar] [CrossRef]
- Finnegan, S.; Bruce, J.; Seers, K. Life after falls prevention exercise-experiences of older people taking part in a clinical trial: A phenomenological study. BMC Geriatr. 2021, 21, 91. [Google Scholar] [CrossRef]
- Franco, M.R.; Sherrington, C.; Tiedemann, A.; Pereira, L.S.; Perracini, M.R.; Faria, C.S.G.; Negrão-Filho, R.F.; Pinto, R.Z.; Pastre, C.M. Effect of Senior Dance (DanSE) on Fall Risk Factors in Older Adults: A Randomized Controlled Trial. Phys. Ther. 2020, 100, 600–608. [Google Scholar] [CrossRef]
- Teng, B.; Rosbergen, I.C.M.; Gomersall, S.; Hatton, A.; Brauer, S.G. Physiotherapists’ experiences and views of older peoples’ exercise adherence with respect to falls prevention in Singapore: A qualitative study. Disabil. Rehabil. 2021, 44, 5530–5538. [Google Scholar] [CrossRef]
- Finnegan, S.; Seers, K.; Bruce, J. Long-term follow-up of exercise interventions aimed at preventing falls in older people living in the community: A systematic review and meta-analysis. Physiotherapy 2019, 105, 187–199. [Google Scholar] [CrossRef] [PubMed]
- Worum, H.; Lillekroken, D.; Roaldsen, K.S.; Ahlsen, B.; Bergland, A. Reflections of older people about their experience of fall prevention exercise in the community-a qualitative study exploring evidence-based practice. BMC Public Health 2020, 20, 1671. [Google Scholar] [CrossRef] [PubMed]
- Association, A.D.T. What Is Dance/Movement Therapy? Available online: https://adta.memberclicks.net/ (accessed on 30 December 2022).
- Koch, S.C.; Riege, R.F.F.; Tisborn, K.; Biondo, J.; Martin, L.; Beelmann, A. Effects of Dance Movement Therapy and Dance on Health-Related Psychological Outcomes. A Meta-Analysis Update. Front. Psychol. 2019, 10, 1806. [Google Scholar] [CrossRef] [PubMed]
- Ho, R.T.H.; Fong, T.C.T.; Chan, W.C.; Kwan, J.S.K.; Chiu, P.K.C.; Yau, J.C.Y.; Lam, L.C.W. Psychophysiological Effects of Dance Movement Therapy and Physical Exercise on Older Adults With Mild Dementia: A Randomized Controlled Trial. J. Gerontol. B Psychol. Sci. Soc. Sci. 2020, 75, 560–570. [Google Scholar] [CrossRef] [PubMed]
- Lowen, A.; Lowen, L. The Vibrant Way to Health: A Manual of Exercises; Harper & Row: Manhattan, NY, USA, 1977. [Google Scholar]
- Pitluk, M.; Elboim-Gabyzon, M.; Engelhard, E.S. Validation of the grounding assessment tool for identifying emotional awareness and emotion regulation. Arts Psychother. 2021, 75, 101821. [Google Scholar] [CrossRef]
- Shuper Engelhard, E.; Pitluk, M.; Elboim-Gabyzon, M. Grounding the Connection Between Psyche and Soma: Creating a Reliable Observation Tool for Grounding Assessment in an Adult Population. Front. Psychol. 2021, 12, 621958. [Google Scholar] [CrossRef]
- Norcross, J.C.; Lambert, M.J. Psychotherapy relationships that work III. Psychotherapy 2018, 55, 303–315. [Google Scholar] [CrossRef] [PubMed]
- de Tord, P.; Bräuninger, I. Grounding: Theoretical application and practice in dance movement therapy. Arts Psychother. 2015, 43, 16–22. [Google Scholar] [CrossRef]
- Clauer, J. Neurobiology and psychological development of grounding and embodiment. Applications in the treatment of clients with early disorders. Bioenerg. Anal. 2011, 21, 17–56. [Google Scholar]
- Ko, K.S. A broken heart from a wounded land: The use of Korean scarf dance as a dance/movement therapy intervention for a Korean woman with haan. Arts Psychother. 2017, 55, 64–72. [Google Scholar] [CrossRef]
- Moher, D.; Hopewell, S.; Schulz, K.F.; Montori, V.; Gotzsche, P.C.; Devereaux, P.J.; Elbourne, D.; Egger, M.; Altman, D.G. Consolidated Standards of Reporting Trials, G. CONSORT 2010 Explanation and Elaboration: Updated guidelines for reporting parallel group randomised trials. J. Clin. Epidemiol. 2010, 63, e1–e37. [Google Scholar] [CrossRef]
- Campbell, A.J.; Robertson, M.C.; Gardner, M.M.; Norton, R.N.; Tilyard, M.W.; Buchner, D.M. Randomised controlled trial of a general practice programme of home based exercise to prevent falls in elderly women. BMJ Br. Med. J. 1997, 315, 1065–1069. [Google Scholar] [CrossRef] [PubMed]
- Rubenstein, L.Z.; Vivrette, R.; Harker, J.O.; Stevens, J.A.; Kramer, B.J. Validating an evidence-based, self-rated fall risk questionnaire (FRQ) for older adults. J. Saf. Res. 2011, 42, 493–499. [Google Scholar] [CrossRef] [PubMed]
- Mahoney, F.I. Functional evaluation: The Barthel index. Md. State Med. J. 1965, 14, 61–65. [Google Scholar]
- Letts, L.; Bosch, J. Measuring occupational performance in basic activities of daily living. In Measuring Occupational Performance: Supporting Best Practice in Occupational Therapy; Law, M., Baum, C., Dunn, W., Eds.; SLACK Incorporated: Thorofare, NJ, USA, 2005; Volume 2, pp. 179–247. [Google Scholar]
- Podsiadlo, D.; Richardson, S. The timed “Up & Go”: A test of basic functional mobility for frail elderly persons. J. Am. Geriatr. Soc. 1991, 39, 142–148. [Google Scholar] [CrossRef]
- Whitney, S.L.; Wrisley, D.M.; Marchetti, G.F.; Gee, M.A.; Redfern, M.S.; Furman, J.M. Clinical measurement of sit-to-stand performance in people with balance disorders: Validity of data for the Five-Times-Sit-to-Stand Test. Phys. Ther. 2005, 85, 1034–1045. [Google Scholar] [CrossRef] [PubMed]
- Shumway-Cook, A.; Brauer, S.; Woollacott, M. Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go Test. Phys. Ther. 2000, 80, 896–903. [Google Scholar] [CrossRef]
- Bohannon, R.W. Reference values for the five-repetition sit-to-stand test: A descriptive meta-analysis of data from elders. Percept. Mot. Ski. 2006, 103, 215–222. [Google Scholar] [CrossRef]
- Bohannon, R.W.; Shove, M.E.; Barreca, S.R.; Masters, L.M.; Sigouin, C.S. Five-repetition sit-to-stand test performance by community-dwelling adults: A preliminary investigation of times, determinants, and relationship with self-reported physical performance. Isokinet. Exerc. Sci. 2007, 15, 77–81. [Google Scholar] [CrossRef]
- Schaubert, K.L.; Bohannon, R.W. Reliability and validity of three strength measures obtained from community-dwelling elderly persons. J. Strength Cond. Res. 2005, 19, 717–720. [Google Scholar] [CrossRef] [PubMed]
- Lachman, M.E.; Howland, J.; Tennstedt, S.; Jette, A.; Assmann, S.; Peterson, E.W. Fear of falling and activity restriction: The survey of activities and fear of falling in the elderly (SAFE). J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 1998, 53, P43–P50. [Google Scholar] [CrossRef] [PubMed]
- Bower, E.S.; Wetherell, J.L.; Merz, C.C.; Petkus, A.J.; Malcarne, V.L.; Lenze, E.J. A new measure of fear of falling: Psychometric properties of the fear of falling questionnaire revised (FFQ-R). Int. Psychogeriatr. 2015, 27, 1121–1133. [Google Scholar] [CrossRef] [PubMed]
- Kempen, G.I.; Yardley, L.; Van Haastregt, J.C.; Zijlstra, G.R.; Beyer, N.; Hauer, K.; Todd, C. The Short FES-I: A shortened version of the falls efficacy scale-international to assess fear of falling. Age Ageing 2008, 37, 45–50. [Google Scholar] [CrossRef]
- Powell, L.E.; Myers, A.M. The activities-specific balance confidence (ABC) scale. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 1995, 50, M28–M34. [Google Scholar] [CrossRef]
- Elboim-Gabizon, M.; Barzilai, N.; Chemel, I.; Lahav, D.; Sulam, H. Validity and reliability of the Hebrew version of the Activities-specific Balance Confidence Scale. J. Isr. Phys. Ther. Soc. (JIPTS) 2008, 10, 26–28. [Google Scholar]
- Landers, M.R.; Durand, C.; Powell, D.S.; Dibble, L.E.; Young, D.L. Development of a scale to assess avoidance behavior due to a fear of falling: The Fear of Falling Avoidance Behavior Questionnaire. Phys. Ther. 2011, 91, 1253–1265. [Google Scholar] [CrossRef]
- Ware Jr, J.E.; Kosinski, M.; Keller, S.D. A 12-Item Short-Form Health Survey: Construction of scales and preliminary tests of reliability and validity. Med. Care 1996, 34, 220–233. [Google Scholar] [CrossRef]
- Gandek, B.; Ware, J.E.; Aaronson, N.K.; Apolone, G.; Bjorner, J.B.; Brazier, J.E.; Bullinger, M.; Kaasa, S.; Leplege, A.; Prieto, L. Cross-validation of item selection and scoring for the SF-12 Health Survey in nine countries: Results from the IQOLA Project. J. Clin. Epidemiol. 1998, 51, 1171–1178. [Google Scholar] [CrossRef]
- Amir, M.; Lewin-Epstein, N.; Becker, G.; Buskila, D. Psychometric properties of the SF-12 (Hebrew version) in a primary care population in Israel. Med. Care 2002, 40, 918–928. [Google Scholar] [CrossRef]
- Bentur, N.; King, Y. The challenge of validating SF-12 for its use with community-dwelling elderly in Israel. Qual. Life Res. 2010, 19, 91–95. [Google Scholar] [CrossRef] [PubMed]
- Horvath, A.O.; Greenberg, L.S. Development and validation of the Working Alliance Inventory. J. Couns. Psychol. 1989, 36, 223. [Google Scholar] [CrossRef]
- Orkibi, H.; Azoulay, B.; Regev, D.; Snir, S. Adolescents’ dramatic engagement predicts their in-session productive behaviors: A psychodrama change process study. Arts Psychother. 2017, 55, 46–53. [Google Scholar] [CrossRef]
- Newman-Beinart, N.A.; Norton, S.; Dowling, D.; Gavriloff, D.; Vari, C.; Weinman, J.A.; Godfrey, E.L. The development and initial psychometric evaluation of a measure assessing adherence to prescribed exercise: The Exercise Adherence Rating Scale (EARS). Physiotherapy 2017, 103, 180–185. [Google Scholar] [CrossRef] [PubMed]
- Terwee, C.B.; Bot, S.D.; de Boer, M.R.; van der Windt, D.A.; Knol, D.L.; Dekker, J.; Bouter, L.M.; de Vet, H.C. Quality criteria were proposed for measurement properties of health status questionnaires. J. Clin. Epidemiol. 2007, 60, 34–42. [Google Scholar] [CrossRef]
- Brown, L.M.; Sawyer, L.M.; Lensing, S.Y.; Taylor, T.; Bopp, M.M.; Ferrier, I.; Sullivan, D.H. An outpatient Tai Chi program: Effects on veterans’ functional outcomes. Nurs. Forum 2020, 56, 448–452. [Google Scholar] [CrossRef]
- Kristensen, M.T.; Bloch, M.L.; Jonsson, L.R.; Jakobsen, T.L. Interrater reliability of the standardized Timed Up and Go Test when used in hospitalized and community-dwelling older individuals. Physiother. Res. Int. 2019, 24, e1769. [Google Scholar] [CrossRef]
- Bégin, D.; Janecek, M.; Macedo, L.G.; Richardson, J.; Wojkowski, S. The relationship between fear of falling and functional ability following a multi-component fall prevention program: An analysis of clinical data. Physiother. Theory Pract. 2022, 1–12. [Google Scholar] [CrossRef]
- Wetherell, J.L.; Johnson, K.; Chang, D.; Ward, S.R.; Bower, E.S.; Merz, C.; Petkus, A.J. Activity, balance, learning, and exposure (ABLE): A new intervention for fear of falling. Int. J. Geriatr. Psychiatry 2016, 31, 791–798. [Google Scholar] [CrossRef]
- Wu, C.-C.; Xiong, H.-Y.; Zheng, J.-J.; Wang, X.-Q. Dance movement therapy for neurodegenerative diseases: A systematic review. Front. Aging Neurosci. 2022, 14, 975711. [Google Scholar] [CrossRef]
- Rosendahl, S.; Sattel, H.; Lahmann, C. Effectiveness of Body Psychotherapy. A Systematic Review and Meta-Analysis. Front. Psychiatry 2021, 12, 709798. [Google Scholar] [CrossRef] [PubMed]
- Wulf, G. Attentional focus and motor learning: A review of 15 years. Int. Rev. Sport Exerc. Psychol. 2013, 6, 77–104. [Google Scholar] [CrossRef]
- Wulf, G.; Prinz, W. Directing attention to movement effects enhances learning: A review. Psychon. Bull. Rev. 2001, 8, 648–660. [Google Scholar] [CrossRef]
- Becker, K.A.; Georges, A.F.; Aiken, C.A. Considering a holistic focus of attention as an alternative to an external focus. J. Mot. Learn. Dev. 2019, 7, 194–203. [Google Scholar] [CrossRef]
- Chiviacowsky, S.; Wulf, G.; Wally, R. An external focus of attention enhances balance learning in older adults. Gait Posture 2010, 32, 572–575. [Google Scholar] [CrossRef]
- Rhea, C.K.; Diekfuss, J.A.; Fairbrother, J.T.; Raisbeck, L.D. Postural control entropy is increased when adopting an external focus of attention. Mot. Control 2019, 23, 230–242. [Google Scholar] [CrossRef]
- Abedanzadeh, R.; Becker, K.; Mousavi, S.M.R. Both a holistic and external focus of attention enhance the learning of a badminton short serve. Psychol. Res. 2022, 86, 141–149. [Google Scholar] [CrossRef]
- Aiken, C.A.; Becker, K.A. Utilising an internal focus of attention during preparation and an external focus during execution may facilitate motor learning. Eur. J. Sport Sci. 2022, 23, 1–8. [Google Scholar] [CrossRef]
- Shih, M.C.; Wang, R.Y.; Cheng, S.J.; Yang, Y.R. Effects of a balance-based exergaming intervention using the Kinect sensor on posture stability in individuals with Parkinson’s disease: A single-blinded randomized controlled trial. J. Neuroeng. Rehabil. 2016, 13, 78. [Google Scholar] [CrossRef]
- Yang, C.M.; Chen Hsieh, J.S.; Chen, Y.C.; Yang, S.Y.; Lin, H.K. Effects of Kinect exergames on balance training among community older adults: A randomized controlled trial. Medicine 2020, 99, e21228. [Google Scholar] [CrossRef]
- Beaton, D.E.; Boers, M.; Wells, G.A. Many faces of the minimal clinically important difference (MCID) a literature review and directions for future research. Curr. Opin. Rheumatol. 2002, 12, 109–114. [Google Scholar] [CrossRef] [PubMed]
- Wells, G.; Beaton, D.; Shea, B.; Boers, M.; Simon, L.; Strand, V.; Brooks, P.; Tugwell, P. Minimal clinically important differences: Review of methods. J. Rheumatol. 2001, 28, 406–412. [Google Scholar] [PubMed]
- Kruisbrink, M.; Delbaere, K.; Kempen, G.; Crutzen, R.; Ambergen, T.; Cheung, K.L.; Kendrick, D.; Iliffe, S.; Zijlstra, G.A.R. Intervention Characteristics Associated With a Reduction in Fear of Falling Among Community-Dwelling Older People: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Gerontologist 2021, 61, e269–e282. [Google Scholar] [CrossRef] [PubMed]
- Veronese, N.; Maggi, S.; Schofield, P.; Stubbs, B. Dance movement therapy and falls prevention. Maturitas 2017, 102, 1–5. [Google Scholar] [CrossRef]
- Arai, T.; Obuchi, S.; Inaba, Y.; Nagasawa, H.; Shiba, Y.; Watanabe, S.; Kimura, K.; Kojima, M. The effects of short-term exercise intervention on falls self-efficacy and the relationship between changes in physical function and falls self-efficacy in Japanese older people: A randomized controlled trial. Am. J. Phys. Med. Rehabil. 2007, 86, 133–141. [Google Scholar] [CrossRef]
- Soh, S.L. Measures of falls efficacy, balance confidence, or balance recovery confidence for perturbation-based balance training. Front. Sport. Act. Living 2022, 4, 1025026. [Google Scholar] [CrossRef]
- Soh, S.L.; Tan, C.W.; Thomas, J.I.; Tan, G.; Xu, T.; Ng, Y.L.; Lane, J. Falls efficacy: Extending the understanding of self-efficacy in older adults towards managing falls. J. Frailty Sarcopenia Falls 2021, 6, 131–138. [Google Scholar] [CrossRef]
- Hoang, O.T.; Jullamate, P.; Piphatvanitcha, N.; Rosenberg, E. Factors related to fear of falling among community-dwelling older adults. J. Clin. Nurs. 2017, 26, 68–76. [Google Scholar] [CrossRef]
- Kempen, G.I.; van Haastregt, J.C.; McKee, K.J.; Delbaere, K.; Zijlstra, G.R. Socio-demographic, health-related and psychosocial correlates of fear of falling and avoidance of activity in community-living older persons who avoid activity due to fear of falling. BMC Public Health 2009, 9, 170. [Google Scholar] [CrossRef]
- Kumar, A.; Carpenter, H.; Morris, R.; Iliffe, S.; Kendrick, D. Which factors are associated with fear of falling in community-dwelling older people? Age Ageing 2014, 43, 76–84. [Google Scholar] [CrossRef]
- Magen, O.; Waxman, J.G.; Makov-Assif, M.; Vered, R.; Dicker, D.; Hernan, M.A.; Lipsitch, M.; Reis, B.Y.; Balicer, R.D.; Dagan, N. Fourth Dose of BNT162b2 mRNA Covid-19 Vaccine in a Nationwide Setting. N. Engl. J. Med. 2022, 386, 1603–1614. [Google Scholar] [CrossRef] [PubMed]
- Hoffman, G.J.; Malani, P.N.; Solway, E.; Kirch, M.; Singer, D.C.; Kullgren, J.T. Changes in activity levels, physical functioning, and fall risk during the COVID-19 pandemic. J. Am. Geriatr. Soc. 2022, 70, 49–59. [Google Scholar] [CrossRef] [PubMed]
- de Maio Nascimento, M.; da Silva Neto, H.R.; de Fatima Carreira Moreira Padovez, R.; Neves, V.R. Impacts of Social Isolation on the Physical and Mental Health of Older Adults During Quarantine: A Systematic Review. Clin. Gerontol. 2022, 1–21. [Google Scholar] [CrossRef]
- Briguglio, M.; Giorgino, R.; Dell’Osso, B.; Cesari, M.; Porta, M.; Lattanzio, F.; Banfi, G.; Peretti, G.M. Consequences for the Elderly After COVID-19 Isolation: FEaR (Frail Elderly amid Restrictions). Front. Psychol. 2020, 11, 565052. [Google Scholar] [CrossRef]
- Wei, L.; Hu, Y.; Tao, Y.; Hu, R.; Zhang, L. The Effects of Physical Exercise on the Quality of Life of Healthy Older Adults in China: A Systematic Review. Front. Psychol. 2022, 13, 895373. [Google Scholar] [CrossRef]
- Alcaniz, M.; Sole-Auro, A. Feeling good in old age: Factors explaining health-related quality of life. Health Qual. Life Outcomes 2018, 16, 48. [Google Scholar] [CrossRef]
- Kim, H.; Di Domenico, S.I.; Connelly, B.S. Self-Other Agreement in Personality Reports: A Meta-Analytic Comparison of Self- and Informant-Report Means. Psychol. Sci. 2019, 30, 129–138. [Google Scholar] [CrossRef]
- Meier, S.T. Investigation of causes of ceiling effects on working alliance measures. Front. Psychol. 2022, 13, 949326. [Google Scholar] [CrossRef] [PubMed]
- Meier, S.T.; Feeley, T.H. Ceiling effects indicate a possible threshold structure for working alliance. J. Couns. Psychol. 2022, 69, 235–245. [Google Scholar] [CrossRef]
- National Academies of Sciences, Engineering, and Medicine. Social Isolation and Loneliness in Older Adults: Opportunities for the Health Care System; National Academies Press: Washington, DC, USA, 2020. [Google Scholar]
- Zilcha-Mano, S. Is the alliance really therapeutic? Revisiting this question in light of recent methodological advances. Am. Psychol. 2017, 72, 311–325. [Google Scholar] [CrossRef]
- Zilcha-Mano, S. Toward personalized psychotherapy: The importance of the trait-like/state-like distinction for understanding therapeutic change. Am. Psychol. 2021, 76, 516–528. [Google Scholar] [CrossRef] [PubMed]
- Paap, D.; Schepers, M.; Dijkstra, P.U. Reducing ceiling effects in the Working Alliance Inventory-Rehabilitation Dutch Version. Disabil. Rehabil. 2020, 42, 2944–2950. [Google Scholar] [CrossRef] [PubMed]
- Collado-Mateo, D.; Lavin-Perez, A.M.; Penacoba, C.; Del Coso, J.; Leyton-Roman, M.; Luque-Casado, A.; Gasque, P.; Fernandez-Del-Olmo, M.A.; Amado-Alonso, D. Key Factors Associated with Adherence to Physical Exercise in Patients with Chronic Diseases and Older Adults: An Umbrella Review. Int. J. Environ. Res. Public Health 2021, 18, 2023. [Google Scholar] [CrossRef] [PubMed]
- Essery, R.; Geraghty, A.W.; Kirby, S.; Yardley, L. Predictors of adherence to home-based physical therapies: A systematic review. Disabil. Rehabil. 2017, 39, 519–534. [Google Scholar] [CrossRef] [PubMed]
- Ángeles, C.-M.M.; Laura, A.-M.; Consuelo, C.-S.M.; Manuel, R.-R.; Eva, A.-C.; Covadonga, G.-P.A.; Group, O.P.W. The effect that the Otago Exercise Programme had on fear of falling in community dwellers aged 65–80 and associated factors. Arch. Gerontol. Geriatr. 2022, 99, 104620. [Google Scholar] [CrossRef]
- Park, C.; Atique, M.M.U.; Mishra, R.; Najafi, B. Association between Fall History and Gait, Balance, Physical Activity, Depression, Fear of Falling, and Motor Capacity: A 6-Month Follow-Up Study. Int. J. Environ. Res. Public Health 2022, 19, 10785. [Google Scholar] [CrossRef]
| Characteristics | PTE+DMT Group (n = 5) | PTE Group (n = 3) | p-Value |
|---|---|---|---|
| Age (years) | 90 (81–91) | 85 (81–87) | 0.45 |
| Falls in the past year (n) | 2 | 3 | 0.18 |
| Assistive device (n) | 2 | 1 | 0.56 |
| Living alone (n) | 5 | 2 | 0.38 |
| Variable | PTE+DMT Group (n = 5) | PTE Group (n = 3) | PTE+DMT Group vs. PTE Group | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Median (IQR) | Z | p-Value | Median (IQR) | Z | p-Value | Pre-Test | Post-Test | |||||
| Pre-Test | Post-Test | Pre-Test | Post-Test | U | p-Value | U | p-Value | |||||
| FRQ | 9 (2–11) | 9 (4–11) | −0.74 | 0.46 | 11 (9–12) | 11 (7–14) | 0 | 1 | 3.5 | 0.22 | 4 | 0.29 |
| Barthel index | 95 (85–100) | 90 (87.5–97.5) | −0.58 | 0.56 | 90 (90–90) | 85 (80–90) | −1.34 | 0.18 | 4.5 | 0.34 | 2.5 | 0.12 |
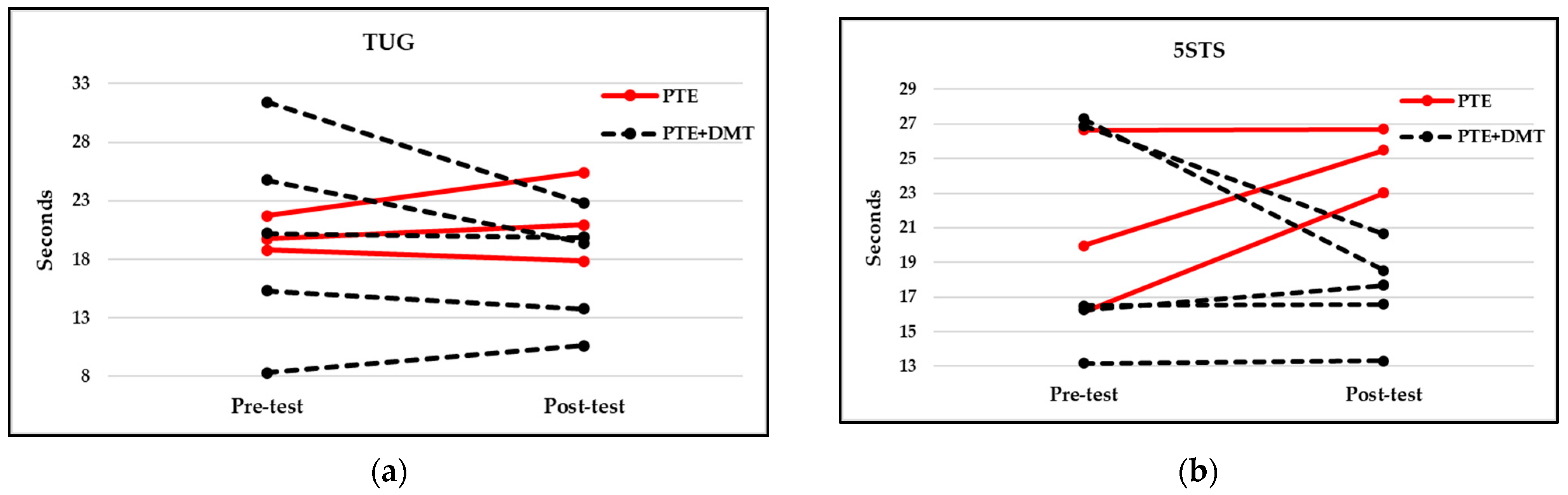
| TUG | 20.21 (11.81–28.09) | 19.21 (12.21–21.34) | −1.21 | 0.23 | 19.73 (18.81–21.73) | 20.96 (17.84–25.43) | −1.07 | 0.29 | 7 | 0.88 | 4 | 0.3 |
| 5STS | 16.51 (14.71–27.09) | 17.68 (14.95–19.59) | −0.41 | 0.69 | 19.95 (16.15–26.65) | 25.49 (23.02–26.71) | −1.6 | 0.11 | 7 | 0.88 | 0 | 0.025 * |
| FOF SIQ | 3 (1.5–4) | 3 (2–3.5) | −0.14 | 0.89 | 4 (3–4) | 4 (4–4) | −1 | 0.32 | 4 | 0.34 | 1.5 | 0.05 * |
| FFQ-R | 20 (14.5–22.5) | 19 (15–21.5) | −0.69 | 0.49 | 21 (20–22) | 21 (21–24) | −1.34 | 0.18 | 5.5 | 0.54 | 2 | 0.099 |
| Short FES-I | 15 (7.5–19.5) | 10 (7.5–20.5) | −0.67 | 0.5 | 17 (15–17) | 20 (18–20) | −1.6 | 0.11 | 6.5 | 0.76 | 3.5 | 0.23 |
| FFABQ | 27 (6.5–36.5) | 18 (3–25) | −0.94 | 0.35 | 29 (12–31) | 24 (11–33) | −0.54 | 0.59 | 5 | 0.45 | 4 | 0.3 |
| ABC | 42.81 (33.44–73.28) | 60 (46.72–63.91) | −0.73 | 0.47 | 45 (45–61.88) | 44.38 (40.63–54.38) | −0.54 | 0.59 | 5 | 0.72 | 2 | 0.16 |
| PCS-12 | 28.41 (22.06–46.73) | 48.24 (41.01–52.34) | −1.75 | 0.08 | 38.14 (26.38–46.26) | 30.58 (26.67–50.48) | 0 | 1 | 7 | 0.88 | 4 | 0.3 |
| MCS-12 | 47.66 (44.37–56.69) | 38.73 (33.35–49.18) | −1.75 | 0.08 | 44.57 (34.75–52.47) | 38.19 (30.38–42.67) | −1.6 | 0.11 | 4 | 0.3 | 7 | 0.88 |
| Therapeutic bond | 5 (4.46–5) | 4.42 (4.25–4.42) | 3 | 0.15 | ||||||||
| EARS | 16 (11–20) | 8 (6–8) | 2 | 0.095 | ||||||||
| Variable | PTE+DMT Group | PTE Group | PTE+DMT Group vs. PTE Group | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Participant 1 | Participant 2 | Participant 3 | Participant 4 | Participant 5 | Participant 1 | Participant 2 | Participant 3 | U | p-Value | |
| FRQ | 0 | −18.18% | 9.09% | 11.11% | 0 | −22.22% | 27.27% | −8.33% | 5 | 0.72 |
| Barthel index | 0 | 6.25% | 0 | −5.26% | −5% | −5.56% | −11.11% | 0 | 3 | 0.17 |
| TUG | 27.76% | −21.59% | −9.93% | −27.43% | −1.68% | 6.24% | −5.18% | 17.05% | 4 | 0.3 |
| 5STS | 1.06% | 0.48% | −23.17% | −32.13% | 8.73% | 42.54% | 0.23% | 27.77% | 3 | 0.18 |
| FOF SIQ | 300% | −66.67% | −25% | −25% | 50% | 0 | 33.33% | 0 | 6 | 0.65 |
| FFQ-R | 100% | −5% | −4.76% | −4.17% | −40% | 9.09% | 5% | 0 | 3 | 0.18 |
| Short FES-I | 228.57% | −57.9% | −10% | −33.33% | −12.5% | 17.65% | 33.33% | 5.88% | 3 | 0.18 |
| FFABQ | 275% | −60.87% | −25.93% | −77.78% | −100% | −8.33% | −22.58% | 13.79% | 3 | 0.18 |
| ABC | −20.77% | 92.31% | 18.97% | 16.46% | 0 | −1.39% | −34.34% | 20.83% | 4 | 0.48 |
| PCS-12 | −8.94% | 83.72% | 119.93% | 73.06% | 19.3% | 9.13% | −19.81% | 1.1% | 2 | 0.1 |
| MCS-12 | −27.24% | −35.16% | −9.13% | −22.81% | 0.28% | −14.3% | −18.68% | −12.58% | 8 | 0.66 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pitluk Barash, M.; Shuper Engelhard, E.; Elboim-Gabyzon, M. Feasibility and Effectiveness of a Novel Intervention Integrating Physical Therapy Exercise and Dance Movement Therapy on Fall Risk in Community-Dwelling Older Women: A Randomized Pilot Study. Healthcare 2023, 11, 1104. https://doi.org/10.3390/healthcare11081104
Pitluk Barash M, Shuper Engelhard E, Elboim-Gabyzon M. Feasibility and Effectiveness of a Novel Intervention Integrating Physical Therapy Exercise and Dance Movement Therapy on Fall Risk in Community-Dwelling Older Women: A Randomized Pilot Study. Healthcare. 2023; 11(8):1104. https://doi.org/10.3390/healthcare11081104
Chicago/Turabian StylePitluk Barash, Michal, Einat Shuper Engelhard, and Michal Elboim-Gabyzon. 2023. "Feasibility and Effectiveness of a Novel Intervention Integrating Physical Therapy Exercise and Dance Movement Therapy on Fall Risk in Community-Dwelling Older Women: A Randomized Pilot Study" Healthcare 11, no. 8: 1104. https://doi.org/10.3390/healthcare11081104
APA StylePitluk Barash, M., Shuper Engelhard, E., & Elboim-Gabyzon, M. (2023). Feasibility and Effectiveness of a Novel Intervention Integrating Physical Therapy Exercise and Dance Movement Therapy on Fall Risk in Community-Dwelling Older Women: A Randomized Pilot Study. Healthcare, 11(8), 1104. https://doi.org/10.3390/healthcare11081104






