Comparison of Secular Trends in Peptic Ulcer Diseases Mortality in China, Brazil and India during 1990–2019: An Age-Period-Cohort Analysis
Abstract
1. Introduction
2. Methods
2.1. Data Sources
2.2. Statistical Analysis
2.3. Ethics Consideration
3. Results
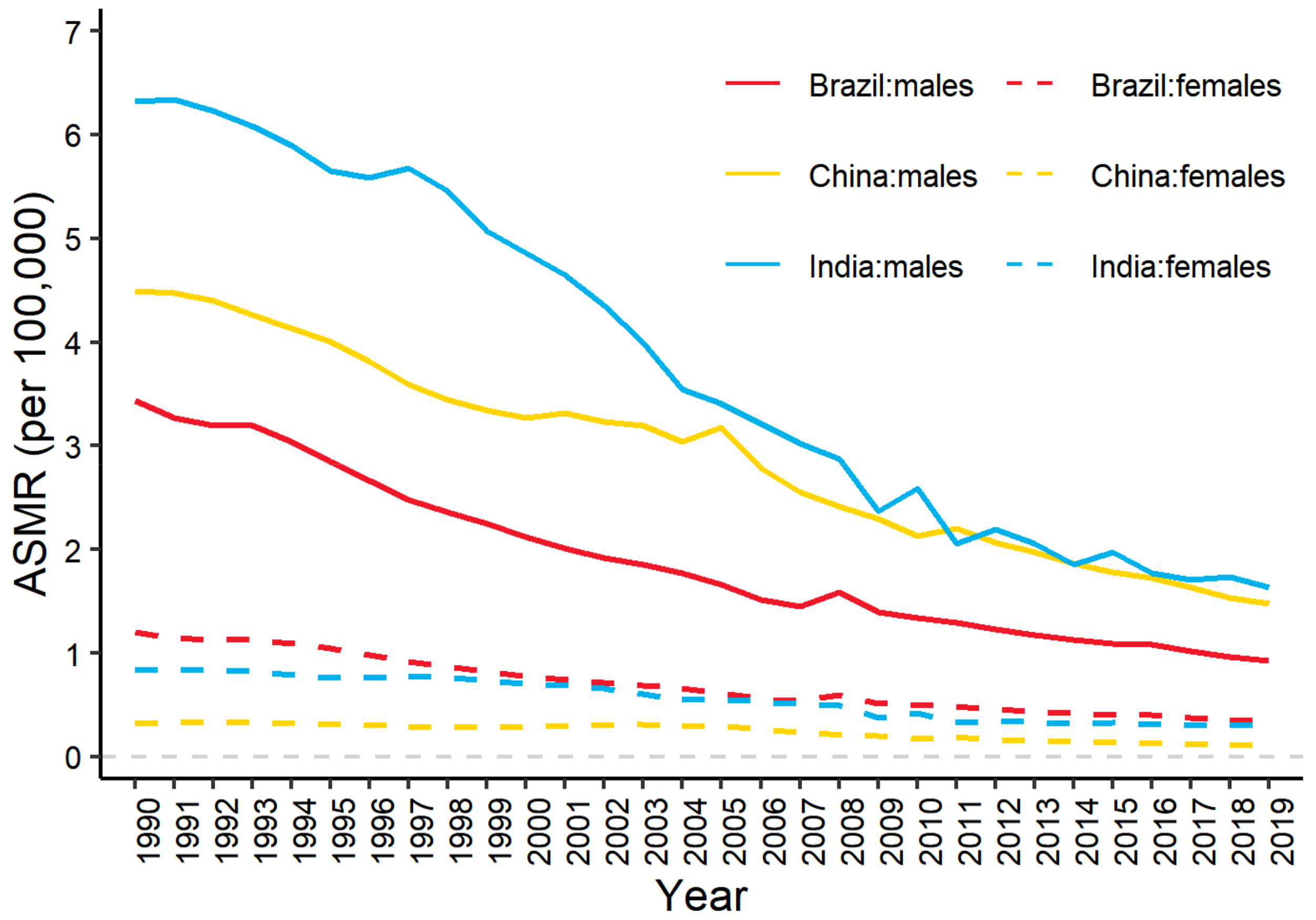
3.1. Trends in Deaths and Age-Standardized Mortality Rates of PUD
3.2. Age-Standardized Mortality Rates of PUD Attributable to Smoking
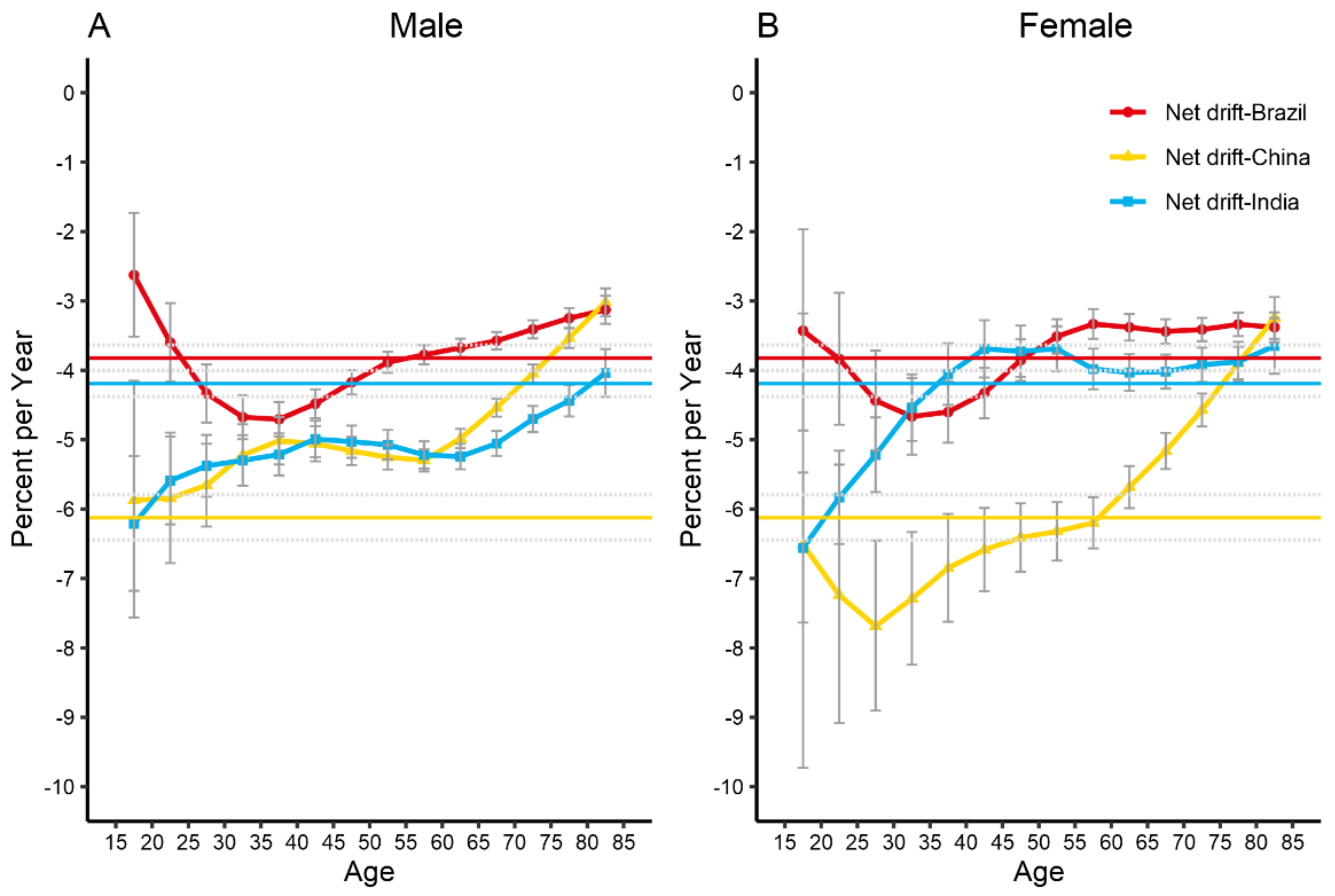
3.3. Net Drifts and Local Drifts for PUD Mortality
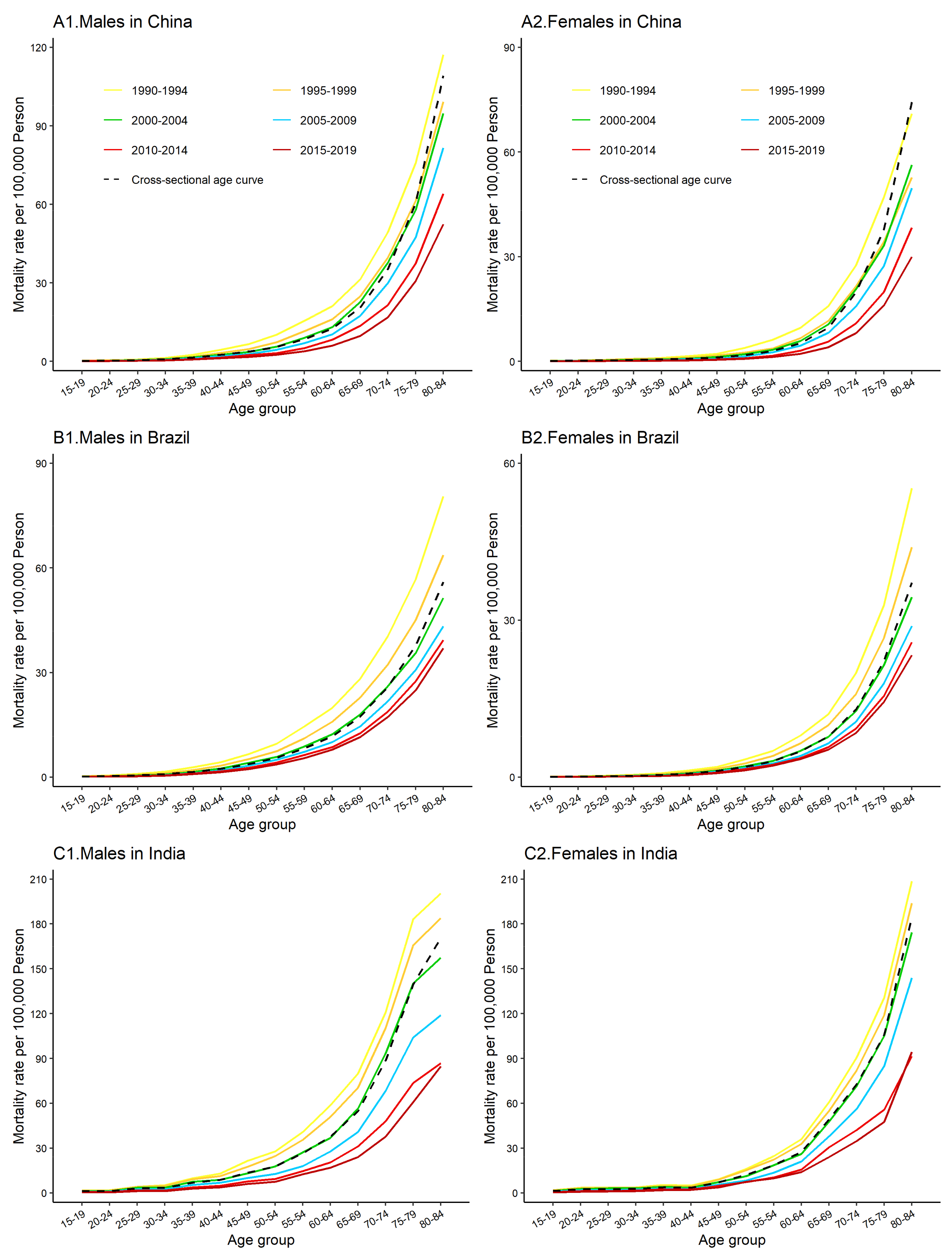
3.4. The Age, Period and Cohort Effects on PUD Mortality
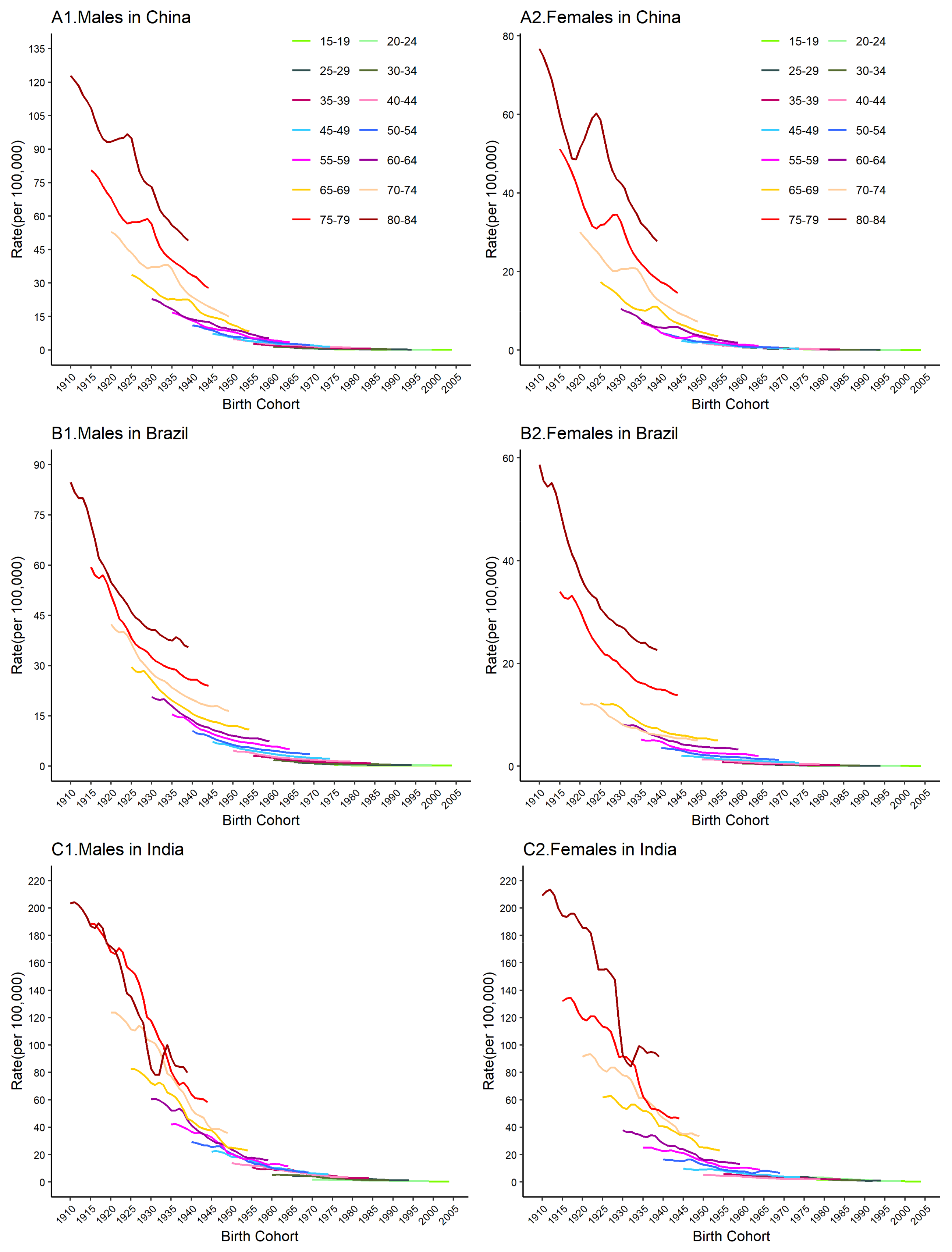
3.5. Age- and Cohort-Specific Mortality Rates for PUD
4. Discussion
4.1. Main Risk Factors for PUD
4.2. Comparative Analysis of the Reasons for the Decrease in PUD Mortality in China, Brazil and India
4.3. Limitations of Our Study
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| NCD | Non-communicable diseases |
| APC | Age-period-cohort |
| GBD | Global Burden of Disease study |
| PUD | Peptic ulcer diseases |
| HP | Helicobacter pylori |
| BRICS | Brazil, Russia, India, China, and South Africa |
| ASMR | Age-standardized mortality rates |
| RRs | Rate ratios |
| NSAIDs | Non-steroidal anti-inflammatory drugs |
| CODEm | Cause of death ensemble model |
| FHP | Family Health Program |
| FCTC | Framework Convention on Tobacco Control |
| PAF | Population attributable fraction |
References
- Rosenstock, S.J.; Jørgensen, T. Prevalence and incidence of peptic ulcer disease in a Danish County—A prospective cohort study. Gut 1995, 36, 819. [Google Scholar] [CrossRef] [PubMed]
- Jameson, J.L.; Fauci, A.; Kasper, D.; Hauser, S.; Longo, D.; Loscalzo, J. Harrison’s Principles of Internal Medicine, 19th ed.; McGraw Hill Education: New York, NY, USA, 2015. [Google Scholar]
- Sung, J.J.; Kuipers, E.J.; El-Serag, H.B. Systematic review: The global incidence and prevalence of peptic ulcer disease. Aliment. Pharmacol. Ther. 2009, 29, 938–946. [Google Scholar] [CrossRef]
- Kurata, J.H.; Nogawa, A.N.; Abbey, D.E.; Petersen, F. A prospective study of risk for peptic ulcer disease in Seventh-Day Adventists. Gastroenterology 1992, 102, 902–909. [Google Scholar] [CrossRef] [PubMed]
- Agréus, L.; Talley, N.J.; Jones, M. Value of the “Test & Treat” Strategy for Uninvestigated Dyspepsia at Low Prevalence Rates of Helicobacter pylori in the Population. Helicobacter 2016, 21, 186–191. [Google Scholar] [CrossRef] [PubMed]
- Lanas, A.; García-Rodríguez, L.A.; Polo-Tomás, M.; Ponce, M.; Quintero, E.; Perez-Aisa, M.A.; Gisbert, J.P.; Bujanda, L.; Castro, M.; Muñoz, M.; et al. The changing face of hospitalisation due to gastrointestinal bleeding and perforation. Aliment. Pharmacol. Ther. 2011, 33, 585–591. [Google Scholar] [CrossRef]
- Malmi, H.; Kautiainen, H.; Virta, L.J.; Färkkilä, N.; Koskenpato, J.; Färkkilä, M.A. Incidence and complications of peptic ulcer disease requiring hospitalisation have markedly decreased in Finland. Aliment. Pharmacol. Ther. 2014, 39, 496–506. [Google Scholar] [CrossRef]
- Levin, T.R.; Schmittdiel, J.A.; Kunz, K.; Henning, J.M.; Henke, C.J.; Colby, C.J.; Selby, J.V. Costs of acid-related disorders to a health maintenance organization. Am. J. Med. 1997, 103, 520–528. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.Q.; Sridhar, S.; Hunt, R.H. Role of Helicobacter pylori infection and non-steroidal anti-inflammatory drugs in peptic-ulcer disease: A meta-analysis. Lancet 2002, 359, 14–22. [Google Scholar] [CrossRef]
- Voutilainen, M.; Mäntynen, T.; Färkkilä, M.; Juhola, M.; Sipponen, P. Impact of non-steroidal anti-inflammatory drug and aspirin use on the prevalence of dyspepsia and uncomplicated peptic ulcer disease. Scand. J. Gastroenterol. 2001, 36, 817–821. [Google Scholar] [CrossRef]
- Axon, A.T. Helicobacter pylori infection. J. Antimicrob. Chemother. 1993, 32, 61–68. [Google Scholar] [CrossRef]
- Czinn, S.J. Helicobacter pylori infection: Detection, investigation, and management. J. Pediatr. 2005, 146, S21–S26. [Google Scholar] [CrossRef] [PubMed]
- Fagerström, K. The epidemiology of smoking: Health consequences and benefits of cessation. Drugs 2002, 62, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Masironi, R. Smoking control strategies in developing countries: Report of a WHO Expert Committee. World Smok. Health 1984, 9, 4–6. [Google Scholar]
- Li, Z.; Zou, D.; Ma, X.; Chen, J.; Shi, X.; Gong, Y.; Man, X.; Gao, L.; Zhao, Y.; Wang, R.; et al. Epidemiology of peptic ulcer disease: Endoscopic results of the systematic investigation of gastrointestinal disease in China. Am. J. Gastroenterol. 2010, 105, 2570–2577. [Google Scholar] [CrossRef] [PubMed]
- Marques, S.B.; Mattar, R.; Artifon, E.L.; Sakai, P.; Carrilho, F.J. High prevalence of duodenal ulcer in a tertiary care hospital in the city of São Paulo, SP, Brazil. Arq. Gastroenterol. 2011, 48, 171–174. [Google Scholar] [CrossRef]
- Khuroo, M.S.; Mahajan, R.; Zargar, S.A.; Javid, G.; Munshi, S. Prevalence of peptic ulcer in India: An endoscopic and epidemiological study in urban Kashmir. Gut 1989, 30, 930–934. [Google Scholar] [CrossRef]
- Singh, V.; Trikha, B.; Nain, C.K.; Singh, K.; Vaiphei, K. Epidemiology of Helicobacter pylori and peptic ulcer in India. J. Gastroenterol. Hepatol. 2002, 17, 659–665. [Google Scholar] [CrossRef] [PubMed]
- The World Bank. World Development Indicators Database. World Bank Publ. 2005, 8, 37–42. [Google Scholar]
- Boerma, J.T.; Fat, D.M.; Mathers, C.; Ebrary, I.; World Health Organization. The Global Burden of Disease: 2004 Update; World Health Organization: Geneva, Switzerland, 2008. [Google Scholar]
- McBride, B.; Hawkes, S.; Buse, K. Soft power and global health: The sustainable development goals (SDGs) era health agendas of the G7, G20 and BRICS. BMC Public Health 2019, 19, 815. [Google Scholar] [CrossRef] [PubMed]
- Barbosa da Silva Junior, J.; Desiraju, K.; Matsoso, P.; Minghui, R.; Salagay, O. BRICS cooperation in strategic health projects. Bull. World Health Organ. 2014, 92, 388. [Google Scholar] [CrossRef]
- Abbafati, C.; Machado, D.B.; Cislaghi, B.; Salman, O.M.; Karanikolos, M.; McKee, M.; Abbas, K.M.; Brady, O.J.; Larson, H.J.; Trias-Llimós, S.; et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef]
- Burnett, R.T.; Pope, C.A.; Ezzati, M.; Olives, C.; Lim, S.S.; Mehta, S.; Shin, H.H.; Singh, G.; Hubbell, B.; Brauer, M.; et al. An integrated risk function for estimating the global burden of disease attributable to ambient fine particulate matter exposure. Environ. Health Perspect. 2014, 122, 397–403. [Google Scholar] [CrossRef] [PubMed]
- Murray, C.J.; Aravkin, A.Y.; Zheng, P.; Abbafati, C.; Abbas, K.M.; Abbasi-Kangevari, M.; Abd-Allah, F.; Abdelalim, A.; Abdollahi, M.; Abdollahpour, I.; et al. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1223–1249. [Google Scholar] [CrossRef]
- Roth, G.A.; Abate, D.; Abate, K.H.; Abay, S.M.; Abbafati, C.; Abbasi, N.; Abbastabar, H.; Abd-Allah, F.; Abdela, J.; Abdelalim, A.; et al. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1736–1788. [Google Scholar] [CrossRef]
- Yang, Y.; Zhou, M.; Zeng, X.; Wang, C. The burden of oral cancer in China, 1990–2017: An analysis for the Global Burden of Disease, Injuries, and Risk Factors Study 2017. BMC Oral Health 2021, 21, 44. [Google Scholar] [CrossRef] [PubMed]
- Flaxman, A.D.; Vos, T.; Murray, C.J.L. An Integrative Metaregression Framework for Descriptive Epidemiology; University of Washington Press: Seattle, WA, USA, 2015. [Google Scholar]
- Bikbov, B.; Purcell, C.A.; Levey, A.S.; Smith, M.; Abdoli, A.; Abebe, M.; Adebayo, O.M.; Afarideh, M.; Agarwal, S.K.; Agudelo-Botero, M.; et al. Global, regional, and national burden of chronic kidney disease, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2020, 395, 709–733. [Google Scholar] [CrossRef] [PubMed]
- Owens, B. Kidney cancer. Nature 2016, 537, S97. [Google Scholar] [CrossRef]
- Zhou, M.; Wang, H.; Zhu, J.; Chen, W.; Wang, L.; Liu, S.; Li, Y.; Wang, L.; Liu, Y.; Yin, P.; et al. Cause-specific mortality for 240 causes in China during 1990–2013: A systematic subnational analysis for the Global Burden of Disease Study 2013. Lancet 2016, 387, 251–272. [Google Scholar] [CrossRef]
- Ribeiro, A.L.P.; Duncan, B.B.; Brant, L.C.C.; Lotufo, P.A.; Mill, J.G.; Barreto, S.M. Cardiovascular Health in Brazil: Trends and Perspectives. Circulation 2016, 133, 422–433. [Google Scholar] [CrossRef]
- Jha, P.; Gajalakshmi, V.; Gupta, P.C.; Kumar, R.; Mony, P.; Dhingra, N.; Peto, R. Prospective study of one million deaths in India: Rationale, design, and validation results. PLoS Med. 2006, 3, e18. [Google Scholar] [CrossRef]
- Yang, Y.; Schulhofer-Wohl, S.; Fu, W.J.; Land, K.C. The Intrinsic Estimator for Age-Period-Cohort Analysis: What It Is and How to Use It. Am. J. Sociol. 2008, 113, 1697–1736. [Google Scholar] [CrossRef]
- Wang, L.; Yu, C.; Liu, Y.; Wang, J.; Li, C.; Wang, Q.; Wang, P.; Wu, S.; Zhang, Z.-J. Lung Cancer Mortality Trends in China from 1988 to 2013: New Challenges and Opportunities for the Government. Int. J. Environ. Res. Public Health 2016, 13, 1052. [Google Scholar] [CrossRef]
- Konturek, S.J.; Bielański, W.; Płonka, M.; Pawlik, T.; Pepera, J.; Konturek, P.C.; Czarnecki, J.; Penar, A.; Jedrychowski, W. Helicobacter pylori, non-steroidal anti-inflammatory drugs and smoking in risk pattern of gastroduodenal ulcers. Scand. J. Gastroenterol. 2003, 38, 923–930. [Google Scholar] [PubMed]
- Sugimoto, M.; Yamaoka, Y. The association of vacA genotype and Helicobacter pylori-related disease in Latin American and African populations. Clin. Microbiol. Infect. 2009, 15, 835–842. [Google Scholar] [CrossRef]
- Zhang, B.-B.; Li, Y.; Liu, X.-Q.; Wang, P.-J.; Yang, B.; Bian, D.-L. Association between vacA genotypes and the risk of duodenal ulcer: A meta-analysis. Mol. Biol. Rep. 2014, 41, 7241–7254. [Google Scholar] [CrossRef]
- Lanas, A.; García-Rodríguez, L.A.; Arroyo, M.T.; Gomollón, F.; Feu, F.; González-Pérez, A.; Zapata, E.; Bástida, G.; Rodrigo, L.; Santolaria, S.; et al. Risk of upper gastrointestinal ulcer bleeding associated with selective cyclo-oxygenase-2 inhibitors, traditional non-aspirin non-steroidal anti-inflammatory drugs, aspirin and combinations. Gut 2006, 55, 1731–1738. [Google Scholar] [CrossRef] [PubMed]
- Palmer, R.H. Risk of Upper and Lower Gastrointestinal Bleeding in Patients Taking Nonsteroidal Anti-Inflammatory Drugs, Antiplatelet Agents, or Anticoagulants. Clin. Gastroenterol. Hepatol. 2015, 13, 2023–2024. [Google Scholar] [CrossRef] [PubMed]
- Chan, F.K.-L.; Goto, S.; Wu, M.-S.; Abola, M.T.B.; Yeoh, K.G.; Sutrisna, B.; Chua, S.S.; Mahachai, V.; Turajane, T.; Wu, B.; et al. Burden of nonsteroidal anti-inflammatory and antiplatelet drug use in Asia: A multidisciplinary working party report. Clin. Gastroenterol. Hepatol. 2012, 10, 753–760. [Google Scholar] [CrossRef]
- González-Pérez, A.; Sáez, M.E.; Johansson, S.; Nagy, P.; García Rodríguez, L.A. Risk factors associated with uncomplicated peptic ulcer and changes in medication use after diagnosis. PLoS ONE 2014, 9, e101768. [Google Scholar] [CrossRef]
- Masclee, G.M.C.; Valkhoff, V.E.; Coloma, P.M.; de Ridder, M.; Romio, S.; Schuemie, M.J.; Herings, R.; Gini, R.; Mazzaglia, G.; Picelli, G.; et al. Risk of upper gastrointestinal bleeding from different drug combinations. Gastroenterology 2014, 147, 784–792. [Google Scholar] [CrossRef]
- Eastwood, G.L. Is smoking still important in the pathogenesis of peptic ulcer disease? J. Clin. Gastroenterol. 1997, 25, S1–S7. [Google Scholar] [CrossRef]
- Endoh, K.; Leung, F.W. Effects of smoking and nicotine on the gastric mucosa: A review of clinical and experimental evidence. Gastroenterology 1994, 107, 864–878. [Google Scholar] [CrossRef]
- Ainley, C.C.; Forgacs, I.C.; Keeling, P.W.; Thompson, R.P. Outpatient endoscopic survey of smoking and peptic ulcer. Gut 1986, 27, 648–651. [Google Scholar] [CrossRef] [PubMed]
- Kurata, J.H.; Elashoff, J.D.; Nogawa, A.N.; Haile, B.M. Sex and smoking differences in duodenal ulcer mortality. Am. J. Public Health 1986, 76, 700–702. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Ma, L.; Li, Y.; Cho, C.H. Exposure to cigarette smoke increases apoptosis in the rat gastric mucosa through a reactive oxygen species-mediated and p53-independent pathway. Free Radic. Biol. Med. 2000, 28, 1125–1131. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, T.; Matsuo, K.; Ito, H.; Sawaki, A.; Hirose, K.; Wakai, K.; Sato, S.; Nakamura, T.; Yamao, K.; Ueda, R.; et al. Smoking increases the treatment failure for Helicobacter pylori eradication. Am. J. Med. 2006, 119, 217–224. [Google Scholar] [CrossRef]
- Yu, J.; Yang, P.; Qin, X.; Li, C.; Lv, Y.; Wang, X. Impact of smoking on the eradication of Helicobacter pylori. Helicobacter 2022, 27, e12860. [Google Scholar] [CrossRef] [PubMed]
- Dutta, A.K.; Chacko, A.; Balekuduru, A.; Sahu, M.K.; Gangadharan, S.K. Time trends in epidemiology of peptic ulcer disease in India over two decades. Indian J. Gastroenterol. 2012, 31, 111–115. [Google Scholar] [CrossRef]
- Sonnenberg, A. Causes underlying the birth-cohort phenomenon of peptic ulcer: Analysis of mortality data 1911–2000, England and Wales. Int. J. Epidemiol. 2006, 35, 1090–1097. [Google Scholar] [CrossRef]
- Charoenca, N.; Mock, J.; Kungskulniti, N.; Preechawong, S.; Kojetin, N.; Hamann, S.L. Success counteracting tobacco company interference in Thailand: An example of FCTC implementation for low- and middle-income countries. Int. J. Environ. Res. Public Health 2012, 9, 1111–1134. [Google Scholar] [CrossRef]
- Sussman, S.; Pokhrel, P.; Black, D.; Kohrman, M.; Hamann, S.; Vateesatokit, P.; Nsimba, S.E.D. Tobacco control in developing countries: Tanzania, Nepal, China, and Thailand as examples. Nicotine Tob. Res 2007, 9, S447–S457. [Google Scholar] [CrossRef] [PubMed]
- Leow, A.H.R.; Lim, Y.Y.; Liew, W.C.; Goh, K.L. Time trends in upper gastrointestinal diseases and Helicobacter pylori infection in a multiracial Asian population—A 20-year experience over three time periods. Aliment. Pharmacol. Ther. 2016, 43, 831–837. [Google Scholar] [CrossRef]
- Mehrotra, R.; Mehrotra, V.; Jandoo, T. Tobacco control legislation in India: Past and present. Indian J. Cancer 2010, 47, 75–80. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, R.L.; Wipfli, H.L.; Samet, J.M. World No Tobacco Day 2011: India’s progress in implementing the framework convention on tobacco control. Indian J. Med. Res. 2011, 133, 455–457. [Google Scholar] [PubMed]
- Suliankatchi Abdulkader, R.; Sinha, D.N.; Jeyashree, K.; Rath, R.; Gupta, P.C.; Kannan, S.; Agarwal, N.; Venugopal, D. Trends in tobacco consumption in India 1987-2016: Impact of the World Health Organization Framework Convention on Tobacco Control. Int. J. Public Health 2019, 64, 841–851. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Sun, Y.; Yang, J.; de Martel, C.; Charvat, H.; Clifford, G.M.; Vaccarella, S.; Wang, L. Time trends and other sources of variation in Helicobacter pylori infection in mainland China: A systematic review and meta-analysis. Helicobacter 2020, 25, e12729. [Google Scholar] [CrossRef]
- Ren, S.; Cai, P.; Liu, Y.; Wang, T.; Zhang, Y.; Li, Q.; Gu, Y.; Wei, L.; Yan, C.; Jin, G. Prevalence of Helicobacter pylori infection in China: A systematic review and meta-analysis. J. Gastroenterol. Hepatol. 2022, 37, 464–470. [Google Scholar] [CrossRef]
- Yang, G.; Wang, Y.; Wu, Y.; Yang, J.; Wan, X. The road to effective tobacco control in China. Lancet 2015, 385, 1019–1028. [Google Scholar] [CrossRef]
- Meng, W.; Zhong, Q.; Chen, Y.; Shen, H.; Yun, X.; Smith, K.R.; Li, B.; Liu, J.; Wang, X.; Ma, J.; et al. Energy and air pollution benefits of household fuel policies in northern China. Proc. Natl. Acad. Sci. USA 2019, 116, 16773–16780. [Google Scholar] [CrossRef]
- Grace, R.C.; Kivell, B.M.; Laugesen, M. Estimating cross-price elasticity of e-cigarettes using a simulated demand procedure. Nicotine Tob. Res. 2015, 17, 592–598. [Google Scholar] [CrossRef]
- Wang, Z.; Hu, S.; Sang, S.; Luo, L.; Yu, C. Age-Period-Cohort Analysis of Stroke Mortality in China: Data from the Global Burden of Disease Study 2013. Stroke 2017, 48, 271–275. [Google Scholar] [CrossRef] [PubMed]
- Hooi, J.K.Y.; Lai, W.Y.; Ng, W.K.; Suen, M.M.Y.; Underwood, F.E.; Tanyingoh, D.; Malfertheiner, P.; Graham, D.Y.; Wong, V.W.S.; Wu, J.C.Y.; et al. Global Prevalence of Helicobacter pylori Infection: Systematic Review and Meta-Analysis. Gastroenterology 2017, 153, 420–429. [Google Scholar] [CrossRef] [PubMed]
- Cesar, P.A.M.; Liberal, M.M.C.D.; Marvulle, V.; Zucchi, P. Analysis of the indicators of the Family Health Program in the Metropolitan Region of São Paulo. Einstein 2018, 16, eGS4174. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, M.I.; Duncan, B.B.; Azevedo e Silva, G.; Menezes, A.M.; Monteiro, C.A.; Barreto, S.M.; Chor, D.; Menezes, P.R. Chronic non-communicable diseases in Brazil: Burden and current challenges. Lancet 2011, 377, 1949–1961. [Google Scholar] [CrossRef]
- Malta, D.C.; Da Silva, A.G.; Machado, Í.E.; Sá, A.C.M.G.N.D.; Santos, F.M.D.; Prates, E.J.S.; Cristo, E.B. Trends in smoking prevalence in all Brazilian capitals between 2006 and 2017. J. Bras. Pneumol. 2019, 45, e20180384. [Google Scholar] [CrossRef] [PubMed]
- Goldacre, M.J.; Duncan, M.; Cook-Mozaffari, P.; Griffith, M.; Travis, S. Inflammatory bowel disease, peptic ulcer and diverticular disease as certified causes of death in an English population 1979-2003. Eur. J. Gastroenterol. Hepatol. 2008, 20, 96–103. [Google Scholar] [CrossRef] [PubMed]

| China | Brazil | India | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Both | Men | Women | Both | Men | Women | Both | Men | Women | |
| ASMR 1/100,000 | |||||||||
| 1990 | 7.53 | 10.02 | 5.47 | 6.07 | 8.23 | 4.19 | 20.17 | 22.78 | 17.37 |
| 2019 | 2.33 | 3.37 | 1.58 | 2.26 | 3.04 | 1.63 | 6.70 | 6.87 | 6.50 |
| Annual percentage change | −3.82 | −3.50 | −4.05 | −3.51 | −3.50 | −3.41 | −4.34 | −4.67 | −3.92 |
| p values | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 |
| Deaths n × 100 | |||||||||
| 1990 | 555 | 350 | 205 | 50 | 33 | 17 | 832 | 505 | 327 |
| 2019 | 401 | 253 | 148 | 52 | 31 | 21 | 691 | 349 | 342 |
| Relative proportion, % * | |||||||||
| 1990 | 0.66 | 0.76 | 0.54 | 0.51 | 0.56 | 0.43 | 1.01 | 1.15 | 0.84 |
| 2019 | 0.38 | 0.41 | 0.33 | 0.37 | 0.39 | 0.41 | 0.74 | 0.70 | 0.78 |
| Population n × 100,000 | |||||||||
| 1990 | 11837 | 6102 | 5735 | 1488 | 736 | 753 | 8556 | 4453 | 4102 |
| 2019 | 14224 | 7428 | 6975 | 2167 | 1058 | 1109 | 13907 | 7132 | 6775 |
| Percentage of global | |||||||||
| 1990 | 22.13 | 22.65 | 21.59 | 2.78 | 2.73 | 2.83 | 15.99 | 16.53 | 15.45 |
| 2019 | 18.38 | 18.68 | 18.09 | 2.80 | 2.73 | 2.87 | 17.97 | 18.38 | 17.57 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sun, J.; Huang, L.; Li, R.; Wang, T.; Wang, S.; Yu, C.; Gong, J. Comparison of Secular Trends in Peptic Ulcer Diseases Mortality in China, Brazil and India during 1990–2019: An Age-Period-Cohort Analysis. Healthcare 2023, 11, 1085. https://doi.org/10.3390/healthcare11081085
Sun J, Huang L, Li R, Wang T, Wang S, Yu C, Gong J. Comparison of Secular Trends in Peptic Ulcer Diseases Mortality in China, Brazil and India during 1990–2019: An Age-Period-Cohort Analysis. Healthcare. 2023; 11(8):1085. https://doi.org/10.3390/healthcare11081085
Chicago/Turabian StyleSun, Jinyi, Lihong Huang, Ruiqing Li, Tong Wang, Shuwen Wang, Chuanhua Yu, and Jie Gong. 2023. "Comparison of Secular Trends in Peptic Ulcer Diseases Mortality in China, Brazil and India during 1990–2019: An Age-Period-Cohort Analysis" Healthcare 11, no. 8: 1085. https://doi.org/10.3390/healthcare11081085
APA StyleSun, J., Huang, L., Li, R., Wang, T., Wang, S., Yu, C., & Gong, J. (2023). Comparison of Secular Trends in Peptic Ulcer Diseases Mortality in China, Brazil and India during 1990–2019: An Age-Period-Cohort Analysis. Healthcare, 11(8), 1085. https://doi.org/10.3390/healthcare11081085





