Analgesic Efficacy of COX-2 Inhibitors in Periodontal Surgery: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Material and Methods
2.1. Study Design
2.2. Selection Criteria (PICO) [33]
2.2.1. Inclusion Criteria
2.2.2. Exclusion Criteria
2.3. Electronic Search
2.4. Assessment of Bias
2.5. Data Extraction
2.6. Statistical Analysis
3. Results
3.1. Searching and Evaluation of Bias
3.2. Qualitative Assessment
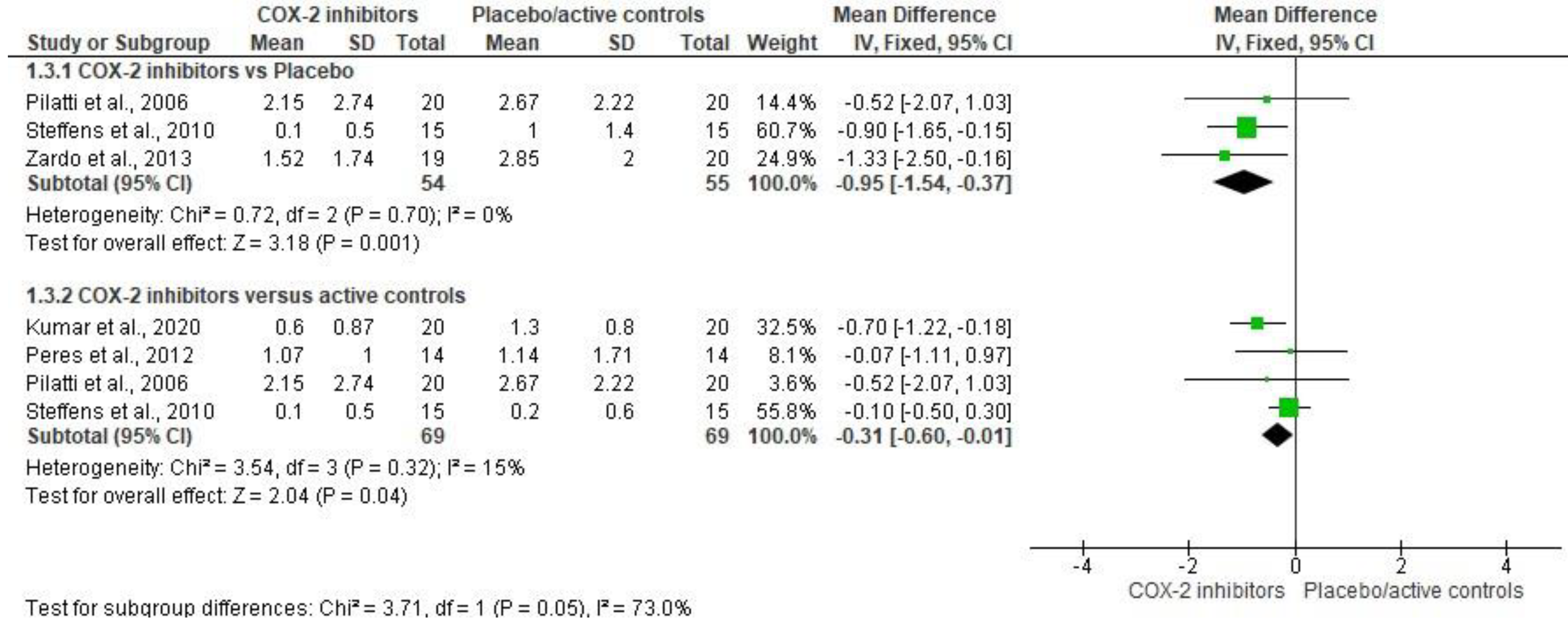
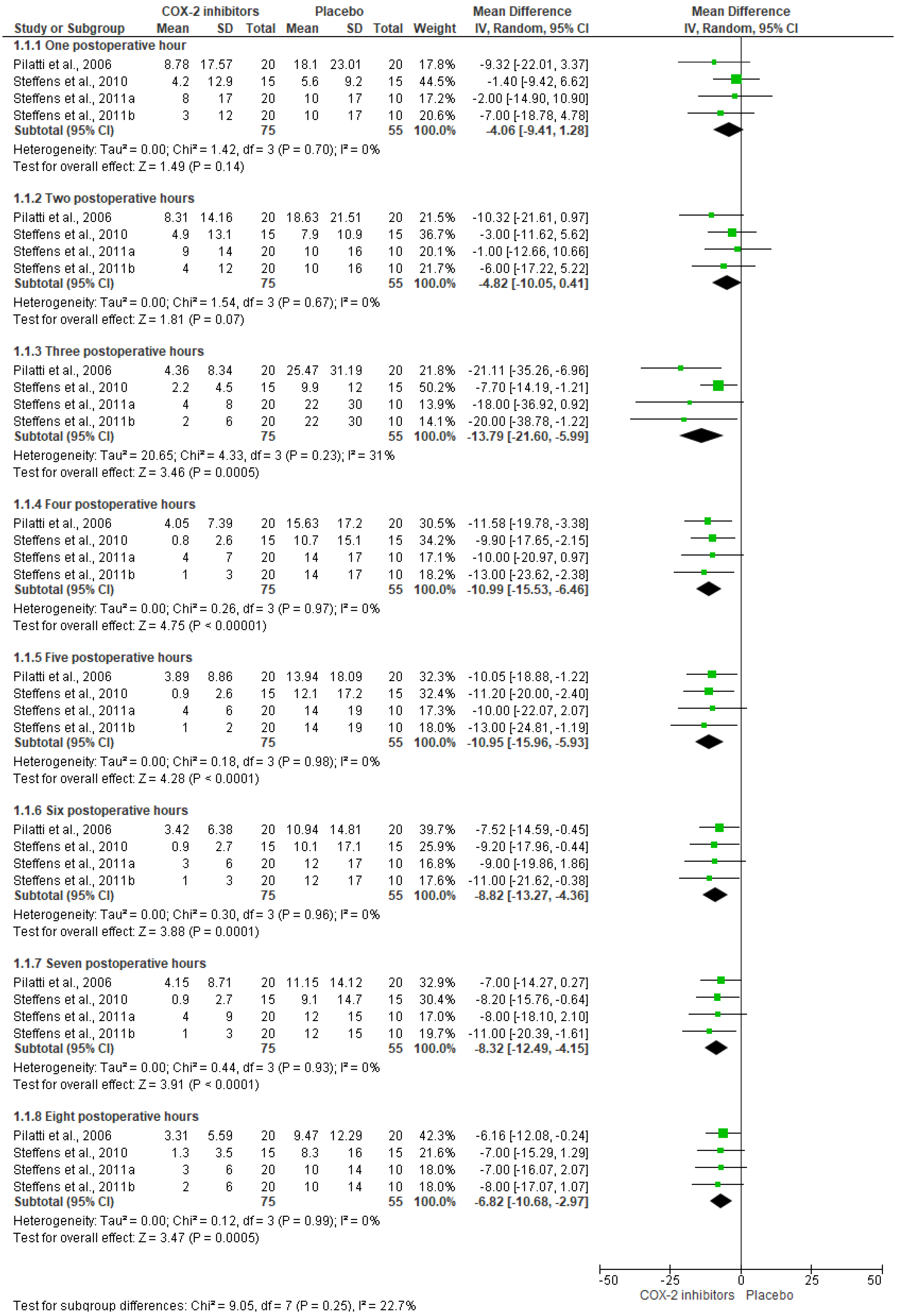
3.3. Quantitative Evaluation
3.4. Sensitivity Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lovich-Sapola, J.; Smith, C.E.; Brandt, C.P. Postoperative pain control. Surg. Clin. N. Am. 2015, 95, 301–318. [Google Scholar] [CrossRef] [PubMed]
- Godse, N.R.; Tarfa, R.A.; Perez, P.L.; Hirsch, B.E.; McCall, A.A. Pain and Pain Control with Opioid and Nonopioid Medications After Otologic Surgery. Otol. Neurotol. 2022, 43, 268–275. [Google Scholar] [CrossRef]
- Mundiya, J.; Woodbine, E. Updates on Topical and Local Anesthesia Agents. Oral Maxillofac. Surg. Clin. N. Am. 2022, 34, 147–155. [Google Scholar] [CrossRef]
- Giovannitti, J.A., Jr.; Rosenberg, M.B.; Phero, J.C. Pharmacology of local anesthetics used in oral surgery. Oral Maxillofac. Surg. Clin. N. Am. 2013, 25, 453–465. [Google Scholar] [CrossRef] [PubMed]
- Pergolizzi, J.V.; Magnusson, P.; LeQuang, J.A.; Gharibo, C.; Varrassi, G. The pharmacological management of dental pain. Expert Opin. Pharmacother. 2020, 21, 591–601. [Google Scholar] [CrossRef] [PubMed]
- Wagner, J.C.; Johnson, T.M.; Gilbert, W.A. Should periodontists prescribe postoperative oral corticosteroids to control pain and swelling? A systematic review. Clin. Adv. Periodontics 2022, 12, 134–142. [Google Scholar] [CrossRef] [PubMed]
- Pozos-Guillen, A.; Martinez-Rider, R.; Aguirre-Banuelos, P.; Pérez-Urizar, J. Pre-emptive analgesic effect of tramadol after mandibular third molar extraction: A pilot study. J. Oral Maxillofac. Surg. 2007, 65, 1315–1320. [Google Scholar] [CrossRef]
- Schoenbrunner, A.R.; Joshi, G.P.; Janis, J.E. Multimodal Analgesia in the Aesthetic Plastic Surgery: Concepts and Strategies. Plast. Reconstr. Surg. Glob. Open 2022, 10, e4310. [Google Scholar] [CrossRef]
- Aurilio, C.; Pace, M.C.; Sansone, P.; Giaccari, L.G.; Coppolino, F.; Pota, V.; Barbarisi, M. Multimodal analgesia in neurosurgery: A narrative review. Postgrad. Med. 2022, 134, 267–276. [Google Scholar] [CrossRef]
- Clarke, H.; Poon, M.; Weinrib, A.; Katznelson, R.; Wentlandt, K.; Katz, J. Preventive analgesia and novel strategies for the prevention of chronic post-surgical pain. Drugs 2015, 75, 339–351. [Google Scholar] [CrossRef]
- Nosotti, M.; Rosso, L.; Tosi, D.; Palleschi, A.; Mendogni, P.; Righi, I.; Marenghi, C.; Santambrogio, L. Preventive analgesia in thoracic surgery: Controlled, randomized, double-blinded study. Eur. J. Cardiothorac. Surg. 2015, 48, 428–433. [Google Scholar] [CrossRef] [PubMed]
- Kearsley, R.; Campbell, J.P. Regional analgesia following caesarean section: New kid and a block? Anaesthesia 2022, 77, 376–379. [Google Scholar] [CrossRef] [PubMed]
- Hedderson, M.; Lee, D.; Hunt, E.; Lee, K.; Xu, F.; Mustille, A.; Galin, J.; Campbell, C.; Quesenberry, C.; Reyes, V.; et al. Enhanced Recovery After Surgery to Change Process Measures and Reduce Opioid Use After Cesarean Delivery: A Quality Improvement Initiative. Obstet. Gynecol. 2019, 134, 511–519. [Google Scholar] [CrossRef] [PubMed]
- McLaughlin, D.C.; Cheah, J.W.; Aleshi, P.; Zhang, A.L.; Ma, C.B.; Feeley, B.T. Multimodal analgesia decreases opioid consumption after shoulder arthroplasty: A prospective cohort study. J. Shoulder Elb. Surg. 2018, 27, 686–691. [Google Scholar] [CrossRef] [PubMed]
- Shim, J.H. Multimodal analgesia or balanced analgesia: The better choice? Korean J. Anesthesiol. 2020, 73, 361–362. [Google Scholar] [CrossRef] [PubMed]
- Vadivelu, N.; Mitra, S.; Schermer, E.; Kodumudi, V.; Kaye, A.D.; Urman, R.D. Preventive analgesia for postoperative pain control: A broader concept. Local Reg. Anesth. 2014, 7, 17–22. [Google Scholar] [CrossRef]
- Caporossi, L.S.; Dos Santos, C.S.; Calcia, T.B.B.; Cenci, M.S.; Muniz, F.W.M.G.; da Silveira Lima, G. Pharmacological management of pain after periodontal surgery: A systematic review with meta-analysis. Clin. Oral Investig. 2020, 24, 2559–2578. [Google Scholar] [CrossRef]
- Blondell, R.D.; Azadfard, M.; Wisniewski, A.M. Pharmacologic therapy for acute pain. Am. Fam. Physician 2013, 87, 766–772. [Google Scholar] [PubMed]
- Esparza-Villalpando, V.; Chavarria-Bolaños, D.; Gordillo-Moscoso, A.; Masuoka-Ito, D.; Martinez-Rider, R.; Isiordia-Espinoza, M.; Pozos-Guillen, A. Comparison of the analgesic efficacy of preoperative/postoperative oral dexketoprofen trometamol in third molar surgery: A randomized clinical trial. J. Craniomaxillofac. Surg. 2016, 44, 1350–1355. [Google Scholar] [CrossRef]
- Cui, J.; Jia, J. Natural COX-2 Inhibitors as Promising Anti-inflammatory Agents: An Update. Curr. Med. Chem. 2021, 28, 3622–3646. [Google Scholar] [CrossRef]
- Jiang, M.; Deng, H.; Chen, X.; Lin, Y.; Xie, X.; Bo, Z. The efficacy and safety of selective COX-2 inhibitors for postoperative pain management in patients after total knee/hip arthroplasty: A meta-analysis. J. Orthop. Surg. Res. 2020, 15, 39. [Google Scholar] [CrossRef] [PubMed]
- Girano-Castaños, J.; Peña-Soto, C.; Girano-Castaños, J. Preemtive Etoricoxib and Ketorolac for Pain Prevention after Periodontal Surgery. Asoc. Peru. Periodoncia Y Oseointegración 2016, 1, 1–5. Available online: https://appo.com.pe/wp-content/uploads/2016/11/Efecto-Analg%C3%A9sico-del-etoricoxib-y-el-ketorolaco-v%C3%ADa-oral-en-cirug%C3%ADa-pl%C3%A1stica-periodontal.pdf (accessed on 20 April 2022).
- Konuganti, K.; Rangaraj, M.; Elizabeth, A. Pre-emptive 8 mg dexamethasone and 120 mg etoricoxib for pain prevention after periodontal surgery: A randomised controlled clinical trial. J. Indian Soc. Periodontol. 2015, 19, 474–476. [Google Scholar] [CrossRef] [PubMed]
- Kumar, S.; Sanghavi, P.K.; Patel, P.N.; Sonvane, P.H.; Dave, P.R.; Gor, V.U.; Mohammed, I. Efficacy of preemptive oral doses of acetaminophen and celecoxib for post-operative pain management after open-flap debridement: A randomised controlled study. Adv. Hum. Biol. 2020, 10, 188–192. [Google Scholar] [CrossRef]
- Peres, M.F.S.; Ribeiro, F.V.; Ruiz, K.G.S.; Nociti, F.H.J.; Sallum, E.A.; Casati, M.Z. Steroidal and Non-Steroidal Cyclooxygenase-2 Inhibitor Anti-Inflammatory Drugs as Pre-Emptive Medication in Patients Undergoing Periodontal Surgery. Braz. Dent. J. 2012, 23, 621–628. [Google Scholar] [CrossRef]
- Pilatti, G.L.; André dos Santos, F.; Bianchi, A.; Cavassim, R.; Tozetto, C.W. The use of celecoxib and dexamethasone for the prevention and control of postoperative pain after periodontal surgery. J. Periodontol. 2006, 77, 1809–1814. [Google Scholar] [CrossRef]
- Steffens, J.P.; Santos, F.A.; Sartori, R.; Pilatti, G.L. Preemptive dexamethasone and etoricoxib for pain and discomfort prevention after periodontal surgery: A double-masked, crossover, controlled clinical trial. J. Periodontol. 2010, 81, 1153–1160. [Google Scholar] [CrossRef]
- Steffens, J.P.; Santos, F.A.; Pilatti, G.L. The use of etoricoxib and celecoxib for pain prevention after periodontal surgery: A double-masked, parallel-group, placebo-controlled, randomized clinical trial. J. Periodontol. 2011, 82, 1238–1244. [Google Scholar] [CrossRef]
- Zardo, L.N.; dos Santos, F.A.; Pilatti, G.L. Use of etoricoxib and dexamethasone for postoperative pain prevention and control in mucogingival surgery—A randomized parallel double-blind clinical trial. Braz. J. Oral Sci. 2013, 12, 345–351. [Google Scholar] [CrossRef]
- Jenabian, N.; Moghadamnia, A.A.; Beyraghshamshir, R. Clinical Efficacy of Celecoxib with and without Caffeine versus Ibuprofen for Pain Control following Crown Lengthening Surgery. J. Dent. Sch. 2015, 33, 51–58. [Google Scholar]
- Shamseer, L.; Moher, D.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: Elaboration and explanation. BMJ 2015, 350, g7647. [Google Scholar] [CrossRef] [PubMed]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Leonardo, R. PICO: Model for Clinical Questions. Evid. Based Med. Pract. 2018, 3, 2. [Google Scholar] [CrossRef]
- Franco-de la Torre, L.; Figueroa-Fernández, N.P.; Franco-González, D.L.; Alonso-Castro, Á.J.; Rivera-Luna, F.; Isiordia-Espinoza, M.A. A Meta-Analysis of the Analgesic Efficacy of Single-Doses of Ibuprofen Compared to Traditional Non-Opioid Analgesics Following Third Molar Surgery. Pharmaceuticals 2021, 14, 360. [Google Scholar] [CrossRef] [PubMed]
- Isiordia-Espinoza, M.A.; Franco-González, M.A.; Alonso-Castro, J.; la Torre, L.F.-D. Analgesic effectiveness and safety of celecoxib versus non-opioid active controls after third molar surgery: A meta-analytical evaluation. J. Stomatol. Oral Maxillofac. Surg. 2022, 123, e1–e9. [Google Scholar] [CrossRef] [PubMed]
- Atkins, D.; Eccles, M.; Flottorp, S.; Guyatt, G.H.; Henry, D.; Hill, S.; Liberati, A.; O’Connell, D.; Oxman, A.D.; Phillips, B.; et al. Systems for grading the quality of evidence and the strength of recommendations I: Critical appraisal of existing approaches The GRADE Working Group. BMC Health Serv. Res. 2004, 4, 38. [Google Scholar] [CrossRef]
- Guyatt, G.H.; Oxman, A.D.; Vist, G.E.; Kunz, R.; Falck-Ytter, Y.; Alonso-Coello, P.; Schünemann, H.J.; GRADE Working Group. GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008, 336, 924–926. [Google Scholar] [CrossRef]
- Isiordia-Espinoza, M.A.; Aragon-Martinez, O.H.; Bollogna-Molina, R.E.; Alonso-Castro, A.J. Infection, alveolar osteitis, and adverse effects using metronidazole in healthy patients undergoing third molar surgery: A meta-analysis. J. Maxillofac. Oral Surg. 2018, 17, 142–149. [Google Scholar] [CrossRef]
- la Torre, L.F.-D.; Gómez-Sánchez, E.; Serafín-Higuera, N.A.; Alonso-Castro, J.; López-Verdín, S.; Molina-Frechero, N.; Granados-Soto, V.; Isiordia-Espinoza, M.A. Dexamethasone Increases the Anesthetic Success in Patients with Symptomatic Irreversible Pulpitis: A Meta-Analysis. Pharmaceuticals 2022, 15, 878. [Google Scholar] [CrossRef]
- Suchetha, A.; Tanwar, E.; Darshan, B.M.; Apoorva, S.M.; Bhat, D. Post-operative complications after periodontal surgery. Int. J. Appl. Dent Sci. 2018, 4, 152–156. Available online: https://www.oraljournal.com/pdf/2018/vol4issue4/PartC/4-4-18-598.pdf (accessed on 9 February 2023).
- Kirmani, M.; Trivedi, H.; Bey, A.; Sharma, V.K. Post–Operative Complications of Periodontal Surgery. Int. J. Contemp Med. Res. 2016, 3, 1285–1286. [Google Scholar]
- Diwan, V.; Srinivasa, T.S.; Ramreddy, K.Y.; Agrawal, V.; Nagdeve, S.; Parvez, H. A comparative evaluation of transdermal diclofenac patch with oral diclofenac sodium as an analgesic drug following periodontal flap surgery: A randomized controlled clinical study. Indian J. Dent. Res. 2019, 30, 57–60. [Google Scholar] [CrossRef] [PubMed]
- Isiordia-Espinoza, M.A.; Sánchez-Prieto, M.; Tobías-Azúa, F.; Reyes-García, J.G. Pre-emptive analgesic effectiveness of meloxicam versus tramadol after mandibular third molar surgery: A pilot study. J. Oral Maxillofac. Surg. 2012, 70, 31–36. [Google Scholar] [CrossRef] [PubMed]
- Isiordia-Espinoza, M.A.; Sánchez-Prieto, M.; Tobías-Azúa, F.; Reyes-García, J.G.; Granados-Soto, V. Pre-emptive analgesia with the combination of tramadol plus meloxicam for third molar surgery: A pilot study. Br. J. Oral Maxillofac. Surg. 2012, 50, 673–677. [Google Scholar] [CrossRef] [PubMed]
- O’Neill, A.; Lirk, P. Multimodal Analgesia. Anesthesiol. Clin. 2022, 40, 455–468. [Google Scholar] [CrossRef]
- Ma, K.; Bebawy, J.F.; Hemmer, L.B. Multimodal Analgesia and Intraoperative Neuromonitoring. J. Neurosurg. Anesthesiol. 2023; in press. [Google Scholar] [CrossRef]
- Itthipanichpong, C.; Chompootaweep, S.; Wittayalertpanya, S.; Kemsri, W.; Thaworn, N.; Lilitkarntrakul, P.; Parikamsil, S. Clinical pharmacokinetic of celecoxib in healthy Thai volunteers. J. Med. Assoc. Thai. 2005, 88, 632–638. [Google Scholar] [PubMed]
- Takemoto, J.K.; Reynolds, J.K.; Remsberg, C.M.; Vega-Villa, K.R.; Davies, N.M. Clinical pharmacokinetic and pharmacodynamic profile of etoricoxib. Clin. Pharmacokinet. 2008, 47, 703–720. [Google Scholar] [CrossRef]
- Renner, B.; Zacher, J.; Buvanendran, A.; Walter, G.; Strauss, J.; Brune, K. Absorption and distribution of etoricoxib in plasma, CSF, and wound tissue in patients following hip surgery--a pilot study. Naunyn Schmiedebergs Arch. Pharmacol. 2010, 381, 127–136. [Google Scholar] [CrossRef]
- Dallob, A.; Hawkey, C.J.; Greenberg, H.; Wight, N.; De Schepper, P.; Waldman, S.; Wong, P.; DeTora, L.; Gertz, B.; Agrawal, N.; et al. Characterization of etoricoxib, a novel, selective COX-2 inhibitor. J. Clin. Pharmacol. 2003, 43, 573–585. [Google Scholar] [CrossRef] [PubMed]
- Tan, L.; Taylor, E.; Hannam, J.A.; Salkeld, L.; Salman, S.; Anderson, B.J. Pharmacokinetics and analgesic effectiveness of intravenous parecoxib for tonsillectomy ± adenoidectomy. Paediatr. Anaesth. 2016, 26, 1126–1135. [Google Scholar] [CrossRef]
- Amabile, C.M.; Spencer, A.P. Parecoxib for parenteral analgesia in postsurgical patients. Ann. Pharmacother. 2004, 38, 882–886. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.K.; Boden, K.A.; Schreiber, K.L. The role of regional anaesthesia and multimodal analgesia in the prevention of chronic postoperative pain: A narrative review. Anaesthesia 2021, 76 (Suppl. 1), 8–17. [Google Scholar] [CrossRef] [PubMed]
- Chitnis, S.S.; Tang, R.; Mariano, E.R. The role of regional analgesia in personalized postoperative pain management. Korean J. Anesthesiol. 2020, 73, 363–371. [Google Scholar] [CrossRef] [PubMed]
- Sutton, C.D.; Carvalho, B. Optimal Pain Management After Cesarean Delivery. Anesthesiol. Clin. 2017, 35, 107–124. [Google Scholar] [CrossRef] [PubMed]
- Gelman, D.; Gelmanas, A.; Urbanaitė, D.; Tamošiūnas, R.; Sadauskas, S.; Bilskienė, D.; Naudžiūnas, A.; Širvinskas, E.; Benetis, R.; Macas, A. Role of Multimodal Analgesia in the Evolving Enhanced Recovery after Surgery Pathways. Medicina 2018, 54, 20. [Google Scholar] [CrossRef]
- González-Barnadas, A.; Camps-Font, O.; Martín-Fatás, P.; Figueiredo, R.; Gay-Escoda, C.; Valmaseda-Castellón, E. Efficacy and safety of selective COX-2 inhibitors for pain management after third molar removal: A meta-analysis of randomized clinical trials. Clin. Oral Investig. 2020, 24, 79–96. [Google Scholar] [CrossRef]
- la Torre, L.F.; Franco-González, D.L.; Brennan-Bourdon, L.M.; Molina-Frechero, N.; Alonso-Castro, Á.J.; Isiordia-Espinoza, M.A. Analgesic Efficacy of Etoricoxib following Third Molar Surgery: A Meta-analysis. Behav. Neurol. 2021, 2021, 9536054. [Google Scholar] [CrossRef]
- Higgins, J.P.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef]
- Brinck, E.C.V.; Tiippana, E.; Heesen, M.; Bell, R.F.; Straube, S.; Moore, R.A.; Kontinen, V. Perioperative intravenous ketamine for acute postoperative pain in adults. Cochrane Database Syst. Rev. 2018, 12, CD012033. [Google Scholar] [CrossRef]
- Argimon-Pallás, J.M.; Jiménez-Villa, J. Métodos de Investigación Clínica y Epidemiológica, 5th ed.; Elsevier: Barcelona, Spain, 2019. [Google Scholar]
- Ayeleke, R.O.; Mourad, S.; Marjoribanks, J.; Calis, K.A.; Jordan, V. Antibiotic prophylaxis for elective hysterectomy. Cochrane Database Syst. Rev. 2017, 6, CD004637. [Google Scholar] [CrossRef]
- Phua, Q.S.; Lu, L.; Harding, M.; Poonnoose, S.I.; Jukes, A.; To, M.S. Systematic Analysis of Publication Bias in Neurosurgery Meta-Analyses. Neurosurgery 2022, 90, 262–269. [Google Scholar] [CrossRef] [PubMed]
- Delgado-Rodríguez, M.; Sillero-Arenas, M. Systematic review and meta-analysis. Med. Intensiva (Engl. Ed.). 2018, 42, 444–453. [Google Scholar] [CrossRef] [PubMed]


| ID Study and Study Design | Treatments (n) | Details of Patients, Dental Procedure, and Evaluation | Important Results (Conclusions) |
|---|---|---|---|
| Kumar et al., 2020 [24] Randomized, double-blind, parallel clinical trial. Single-dose study. Preemptive analgesia. | Group A: Celecoxib 200 mg (n = 20). Group B: Acetaminophen 500 mg (n = 20). Drugs were given by oral route. | Healthy patients aged between 20 years to 50 years were included. Patients underwent open-flap debridement. The inferior alveolar nerve block was made with 2% lidocaine, and local infiltration with 4% articaine with 1:100,000 epinephrine. The rescue analgesic was not informed. The number of patients taking rescue analgesic medication, the time to first analgesic medication after surgery, and the pain intensity were recorded. | Celecoxib was more effective than acetaminophen for control of pain after periodontal surgery. |
| Peres et al., 2012 [25] Randomized, double-blind, parallel clinical trial. Single-dose study. Preemptive analgesia. | Group A: Lumiracoxib 400 mg (n = 14). Group B: Dexamethasone 4 mg (n = 14). Drugs were administered orally. | Patients needing to be submitted to periodontal surgery for crown lengthening were selected. Local infiltration was made using 2% lidocaine and 1:100,000 epinephrine. Dipyrone 500 mg rescued analgesic medication was employed. The anxiety level, the number of pills of dipyrone after surgery, edema, and pain intensity were assessed. | Lumiracoxib and dexamethasone had similar anti-inflammatory and analgesic effects. |
| Pilatti et al., 2006 [26] Randomized, triple-blind, crossover, clinical assay. Multiple-dose study. Preemptive analgesia. | Group A: Celecoxib 200 mg (n = 20). Group B: Dexamethasone 4 mg (n = 20). Group C: Placebo (n = 20). Drugs were given by oral route 1 h before surgery and placebo and dexamethasone were given 8 h after of first dose and celecoxib 12 h after of the first dose. | Patients aged 27 years and 52 years were included. Patients underwent mucoperiosteal flap surgery, scaling, and root planing on at least three quadrants were included. Local anesthesia was carried out with 2% lidocaine and 1:100,000 epinephrine. Acetaminophen 750 mg rescue analgesic medication was used. The stress, anxiety, and pain intensity were evaluated. | Celecoxib was better when compared to placebo. Dexamethasone was not more effective than a placebo. The authors concluded that celecoxib and dexamethasone were effective for pain control after periodontal surgery. |
| Steffens et al., 2010 [27] Randomized, triple-blind, crossover, clinical assay. Single-dose study. Preemptive analgesia. | Group A: Etoricoxib 120 mg (n = 15). Group B: Dexamethasone 8 mg (n = 15). Group C: Placebo (n = 15). Drugs were administered by oral route. | Patients aged 18 years to 56 years and needing open-flap debridement surgery were selected. Local anesthesia was given using 2% mepivacaine and 1:100,000 epinephrine. Acetaminophen 750 mg rescue analgesic medication was used. The stress, anxiety, total analgesic intake, and pain intensity were evaluated. | Both etoricoxib and dexamethasone are effective for pain control after periodontal surgery. |
| Steffens et al., 2011 [28] Randomized, double-blind, parallel clinical assay. Multiple-dose study. Preemptive analgesia. | Group A: Celecoxib 200 mg 1 h before surgery and another 200 mg dose 12 h after the first dose (n = 20). Group B: Etoricoxib 120 mg 1 h before surgery (n = 20). Group 3. Placebo 1 h before surgery (n = 20). | Patients aged 18 years to 56 years old with needing a mucoperiosteal flap. The anesthesia was completed using 2% mepivacaine with 1:100,000 epinephrine. Paracetamol 750 mg rescue analgesic medication was employed. Pain intensity by VAS, stress, anxiety, and analgesic intake were evaluated. | Similar analgesic effectiveness between celecoxib and etoricoxib was observed. Both drugs were better than the placebo. |
| Zardo et al., 2013 [29] Randomized, double-blind, parallel clinical trial. Single-dose study. Preemptive analgesia. | Group A: Etoricoxib 90 mg (n = 19). Group B: Dexamethasone 8 mg (n = 19). Group C: Placebo (n = 20). Drugs were given by oral route 1 h before surgery. | Patients aged 19 years to 67 years with indications of periodontal surgery were included. Anesthesia was made using 2% lidocaine—1:100,000 epinephrine. Paracetamol 750 mg rescue analgesic medication was utilized. Rescue analgesic intake, pain intensity, and adverse effects were measured. | Etoricoxib and dexamethasone are effective for the control of pain in periodontal surgery. |
| Jenabian et al., 2015 [30] Randomized, double-blind, parallel clinical trial. Multiple-dose study. Preemptive and postoperative analgesia. | Group A: Ibuprofen 400 mg (n = 15). Group B: Celecoxib 200 mg (n = 15). Group C: Celecoxib 200 mg plus caffeine 30 mg (n = 15). Drugs were given an hour before surgery and 1 h, 8 h, 16 h, and 24 h after crown lengthening surgery. | Patients aged 20 years to 60 years who needed crown lengthening surgery were included in this study. The local anesthetic used in the surgical procedures was not reported. Paracetamol-codeine rescue analgesia was used. Pain was evaluated by VAS | The celecoxib plus caffeine combination showed better analgesic efficacy when compared to other treatments in crown lengthening surgery. |
| ID Study and Study Design | Treatments (n) | Details of Patients, Dental Procedure, and Evaluation | Important Results (Conclusions) |
|---|---|---|---|
| Girano-Castaños et al., 2016 [22] Randomized, parallel clinical trial. Single-dose study. Preemptive analgesia. | Group A: Etoricoxib 120 mg (n = 15). Group B: Ketorolaco 10 mg (n = 15). Drugs were given by oral route 1 h prior surgery. | Patients who required periodontal plastic surgery due to periodontal recession were included. The anesthetic technique and the medication used for this purpose were not specified. Paracetamol 500 mg rescue analgesic was used. Pain intensity using the VAS and a verbal scale was recorded. | Similar analgesic efficacy between etoricoxib and ketorolac after periodontal surgery was observed. No adverse effects were reported. |
| Konuganti et al., 2015 [23] Randomized, parallel clinical trial. Single-dose study. Preemptive analgesia. | Group A: Etoricoxib 120 mg (n = 20). Group B: Dexamethasone 8 mg (n = 20). Group C: Placebo (n = 20). Drugs were administered orally 1 h before surgery. | Patients aged 18 years to 56 years who needing open flap debridement surgery. The anesthetic technique and the medication used for this purpose were not specified. Paracetamol 650 mg rescue analgesic was used. The the number of pills after surgery, and pain intensity were assessed. | Similar analgesic effectiveness between etoricoxib and dexamethasone was observed. No adverse effects were reported. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Isiordia-Espinoza, M.A.; Gómez-Sánchez, E.; Mora-Falcón, I.J.; Amador-Beas, I.A.; Hernández-Gómez, A.; Serafín-Higuera, N.A.; Franco-de la Torre, L. Analgesic Efficacy of COX-2 Inhibitors in Periodontal Surgery: A Systematic Review and Meta-Analysis. Healthcare 2023, 11, 1054. https://doi.org/10.3390/healthcare11071054
Isiordia-Espinoza MA, Gómez-Sánchez E, Mora-Falcón IJ, Amador-Beas IA, Hernández-Gómez A, Serafín-Higuera NA, Franco-de la Torre L. Analgesic Efficacy of COX-2 Inhibitors in Periodontal Surgery: A Systematic Review and Meta-Analysis. Healthcare. 2023; 11(7):1054. https://doi.org/10.3390/healthcare11071054
Chicago/Turabian StyleIsiordia-Espinoza, Mario Alberto, Eduardo Gómez-Sánchez, Itzel Joselyn Mora-Falcón, Iván Agustín Amador-Beas, Adriana Hernández-Gómez, Nicolás Addiel Serafín-Higuera, and Lorenzo Franco-de la Torre. 2023. "Analgesic Efficacy of COX-2 Inhibitors in Periodontal Surgery: A Systematic Review and Meta-Analysis" Healthcare 11, no. 7: 1054. https://doi.org/10.3390/healthcare11071054
APA StyleIsiordia-Espinoza, M. A., Gómez-Sánchez, E., Mora-Falcón, I. J., Amador-Beas, I. A., Hernández-Gómez, A., Serafín-Higuera, N. A., & Franco-de la Torre, L. (2023). Analgesic Efficacy of COX-2 Inhibitors in Periodontal Surgery: A Systematic Review and Meta-Analysis. Healthcare, 11(7), 1054. https://doi.org/10.3390/healthcare11071054