Diagnostic Yield of Neuroimaging for Headache in a Pediatric Emergency Department: A Single Tertiary Centre Experience
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Study Population
2.3. Study Variables
2.4. Ethical Approval
2.5. Data Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Munoz-Ceron, J.; Marin-Careaga, V.; Peña, L.; Mutis, J.; Ortiz, G. Headache at the emergency room: Etiologies, diagnostic usefulness of the ICHD 3 criteria, red and green flags. PLoS ONE 2019, 14, e0208728. [Google Scholar] [CrossRef] [PubMed]
- Lateef, T.M.; Merikangas, K.R.; He, J.; Kalaydjian, A.; Khoromi, S.; Knight, E.; Nelson, K.B. Headache in a national sample of American children: Prevalence and comorbidity. J. Child Neurol. 2009, 24, 536–543. [Google Scholar] [CrossRef] [PubMed]
- Rossi, R.; Versace, A.; Lauria, B.; Grasso, G.; Castagno, E.; Ricceri, F.; Pagliero, R.; Urbino, A.F. Headache in the pediatric emergency department: A 5-year retrospective study. Cephalalgia Int. J. Headache 2018, 38, 1765–1772. [Google Scholar] [CrossRef] [PubMed]
- Hershey, A.D.; Winner, P.; Kabbouche, M.A.; Powers, S.W. Headaches. Curr. Opin. Pediatr. 2007, 19, 663–669. [Google Scholar] [CrossRef] [PubMed]
- Lewis, D.W.; Ashwal, S.; Dahl, G.; Dorbad, D.; Hirtz, D.; Prensky, A.; Jarjour, I. Practice parameter: Evaluation of children and adolescents with recurrent headaches: Report of the Quality Standards Subcommittee of the American Academy of Neurology and the Practice Committee of the Child Neurology Society. Neurology 2002, 59, 490–498. [Google Scholar] [CrossRef]
- Babineau, S.E.; Green, M.W. Headaches in children. Continuum 2012, 18, 853–868. [Google Scholar] [CrossRef]
- Casucci, G.; Terlizzi, R.; Cevoli, S. Headache in school age. Neurol. Sci. 2014, 35, 31–35. [Google Scholar] [CrossRef]
- Conicella, E.; Raucci, U.; Vanacore, N.; Vigevano, F.; Reale, A.; Pirozzi, N.; Valeriani, M. The child with headache in a pediatric emergency department. Headache 2008, 48, 1005–1011. [Google Scholar] [CrossRef]
- Kan, L.; Nagelberg, J.; Maytal, J. Headaches in a pediatric emergency department: Etiology, imaging, and treatment. Headache 2000, 40, 25–29. [Google Scholar] [CrossRef]
- Lewis, D.W. Headache in the pediatric emergency department. Semin. Pediatr. Neurol. 2001, 8, 46–51. [Google Scholar] [CrossRef]
- Scagni, P.; Pagliero, R. Headache in an Italian pediatric emergency department. J. Headache Pain 2008, 9, 83–87. [Google Scholar] [CrossRef] [PubMed]
- Burton, L.J.; Quinn, B.; Pratt-Cheney, J.L.; Pourani, M. Headache etiology in a pediatric emergency department. Pediatr. Emerg. Care 1997, 13, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Gandhi, R.; Lewis, E.C.; Evans, J.W.; Sell, E. Investigating the necessity of computed tomographic scans in children with headaches: A retrospective review. CJEM 2015, 17, 148–153. [Google Scholar] [CrossRef] [PubMed]
- Hsiao, H.J.; Huang, J.L.; Hsia, S.H.; Lin, J.J.; Huang, I.A.; Wu, C.T. Headache in the pediatric emergency service: A medical center experience. Pediatr. Neonatol. 2014, 55, 208–212. [Google Scholar] [CrossRef]
- Al Jumah, M.; Awada, A.; Al Azzam, S. Headache syndromes amongst schoolchildren in Riyadh, Saudi Arabia. Headache 2002, 42, 281–286. [Google Scholar] [CrossRef]
- Alexiou, G.A.; Argyropoulou, M.I. Neuroimaging in childhood headache: A systematic review. Pediatr. Radiol. 2013, 43, 777–784. [Google Scholar] [CrossRef]
- Behzadmehr, R.; Arefi, S.; Behzadmehr, R. Brain Imaging Findings in Children with Headache. Acta Inform. Med. 2018, 26, 51–53. [Google Scholar] [CrossRef]
- DeVries, A.; Young, P.C.; Wall, E.; Getchius, T.S.; Li, C.H.; Whitney, J.; Rosenberg, A. CT scan utilization patterns in pediatric patients with recurrent headache. Pediatrics 2013, 132, e1–e8. [Google Scholar] [CrossRef]
- Gupta, V.; Khandelwal, N.; Prabhakar, A.; Satish Kumar, A.; Ahuja, C.K.; Singh, P. Prevalence of normal head CT and positive CT findings in a large cohort of patients with chronic headaches. Neuroradiol. J. 2015, 28, 421–425. [Google Scholar] [CrossRef]
- Robbins, M.S.; Starling, A.J.; Pringsheim, T.M.; Becker, W.J.; Schwedt, T.J. Treatment of Cluster Headache: The American Headache Society Evidence-Based Guidelines. Headache 2016, 56, 1093–1106. [Google Scholar] [CrossRef]
- Ali, A.H.A.; Al-Ghamdi, S.; Karrar, M.H.; Alajmi, S.A.; Almutairi, O.S.; Aldalbahi, A.M.; Alotaibi, Y.M.; Alruwaili, S.A.; Elamin, A.Y. Is there a misuse of computed tomography in the diagnostic workup of headache? A retrospective record-based study in secondary health-care facility in Saudi Arabia. J. Fam. Med. Prim. Care 2018, 7, 357–361. [Google Scholar] [CrossRef] [PubMed]
- Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition (beta version). Cephalalgia 2013, 33, 629–808. [Google Scholar] [CrossRef] [PubMed]
- Raucci, U.; Della Vecchia, N.; Ossella, C.; Paolino, M.C.; Villa, M.P.; Reale, A.; Parisi, P. Management of Childhood Headache in the Emergency Department. Review of the Literature. Front. Neurol. 2019, 10, 886. [Google Scholar] [CrossRef] [PubMed]
- Zhu, K.; Born, D.W.; Dilli, E. Secondary Headache: Current Update. Headache 2020, 60, 2654–2664. [Google Scholar] [CrossRef]
- Tsze, D.S.; Ochs, J.B.; Gonzalez, A.E.; Dayan, P.S. Red flag findings in children with headaches: Prevalence and association with emergency department neuroimaging. Cephalalgia 2019, 39, 185–196. [Google Scholar] [CrossRef]
- Thukral, B.B. Problems and preferences in pediatric imaging. Indian J. Radiol. Imaging 2015, 25, 359–364. [Google Scholar] [CrossRef] [PubMed]
- Hall, E.J. Lessons we have learned from our children: Cancer risks from diagnostic radiology. Pediatr. Radiol. 2002, 32, 700–706. [Google Scholar] [CrossRef]
- Little, R.D. Emergency Department Evaluation and Management of Children With Headaches. Clin. Pediatr. Emerg. Med. 2017, 18, 298–302. [Google Scholar] [CrossRef]
- Verma, R.K.; Kottke, R.; Andereggen, L.; Weisstanner, C.; Zubler, C.; Gralla, J.; Kiefer, C.; Slotboom, J.; Wiest, R.; Schroth, G.; et al. Detecting subarachnoid hemorrhage: Comparison of combined FLAIR/SWI versus CT. Eur. J. Radiol. 2013, 82, 1539–1545. [Google Scholar] [CrossRef]
- Meredith, J.T.; Wait, S.; Brewer, K.L. A prospective double-blind study of nasal sumatriptan versus IV ketorolac in migraine. Am. J. Emerg. Med. 2003, 21, 173–175. [Google Scholar] [CrossRef]
- Brousseau, D.C.; Duffy, S.J.; Anderson, A.C.; Linakis, J.G. Treatment of pediatric migraine headaches: A randomized, double-blind trial of prochlorperazine versus ketorolac. Ann. Emerg. Med. 2004, 43, 256–262. [Google Scholar] [CrossRef] [PubMed]
| Variables | Mean | SD |
|---|---|---|
| Age (years) | 11.7 | 3.3 |
| Age of onset (years) | 9.3 | 3.0 |
| Height (cm) | 139.1 | 19.0 |
| Weight (kg) | 42.4 | 19.0 |
| Frequency | Percentages | |
| Gender | ||
| Males | 152 | 58% |
| Females | 111 | 42% |
| Prior diagnosis of headache | 25 | 10% |
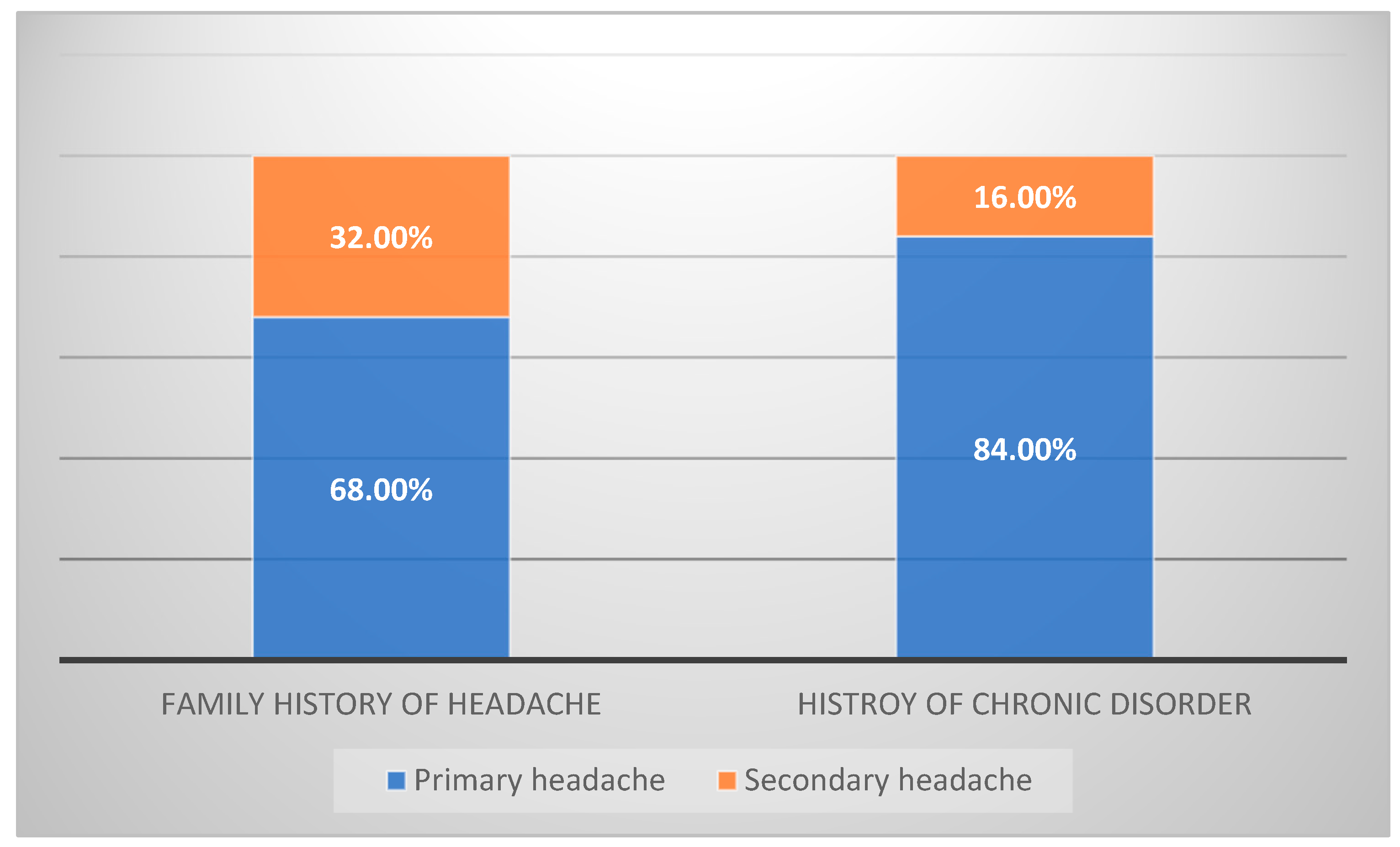
| Family history of headache | 31 | 12% |
| History of chronic disorder | 109 | 41% |
| Neurological disorders | 55 | 21% |
| Respiratory disorders | 32 | 12% |
| Genetic disorders | 18 | 7% |
| Malignancy | 16 | 6% |
| Metabolic disorder | 5 | 2% |
| Infectious disorders | 5 | 2% |
| Others | 60 | 23% |
| All Patients ** N = 260 | Primary N = 58 | Secondary N = 202 | p-Value * | ||||
|---|---|---|---|---|---|---|---|
| Abnormal Examination | Abnormal Examination | Abnormal Examination | |||||
| N | % | N | % | N | % | ||
| Neurological examination | 100 | 39% | 25 | 43% | 75 | 37% | 0.43 |
| Mental status changes | 14 | 5% | 5 | 9% | 9 | 5% | 0.27 |
| Language | 7 | 3% | 1 | 2% | 6 | 3% | 1.0 |
| Cranial nerve | 9 | 4% | 3 | 5% | 6 | 3% | 0.43 |
| Motor | 24 | 9% | 6 | 10% | 18 | 9% | 0.76 |
| Sensory | 2 | 1% | 1 | 2% | 1 | 1% | 0.42 |
| Cerebellar | 10 | 4% | 0 | 0% | 10 | 5% | 0.11 |
| Gait | 12 | 5% | 1 | 2% | 11 | 5% | 0.29 |
| Reflexes | 3 | 1% | 0 | 0% | 3 | 2% | 1.0 |
| CT Findings | All Patients ** N = 260 | Headache Type | p-Value * | ||||
|---|---|---|---|---|---|---|---|
| Primary N = 58 | Secondary N = 202 | ||||||
| N | % | N | % | N | % | ||
| Abnormal CT | 131 | 50% | 14 | 24% | 117 | 58% | <0.001 |
| Mass | 18 | 7% | 0 | 0% | 18 | 9% | 0.13 |
| Cyst | 14 | 5% | 0 | 0% | 14 | 7% | 0.21 |
| Ventricular dilation | 10 | 4% | 0 | 0% | 10 | 5% | 0.61 |
| Hydrocephalus | 17 | 7% | 0 | 0% | 17 | 8% | 0.13 |
| Calcification | 4 | 2% | 0 | 0% | 4 | 2% | 1.0 |
| VP shunt malfunction | 5 | 2% | 0 | 0% | 5 | 2% | 1.0 |
| Infarction | 2 | 1% | 0 | 0% | 2 | 1% | 1.0 |
| Edema | 6 | 2% | 0 | 0% | 6 | 3% | 1.0 |
| Sinusitis | 42 | 16% | 9 | 16% | 33 | 16% | 0.49 |
| Others | 85 | 33% | 14 | 24% | 71 | 35% | 0.33 |
| MRI findings | |||||||
| MRI abnormal | 68 | 26% | 2 | 3% | 66 | 33% | <0.001 |
| Mass A | 21 | 8% | 0 | 0% | 21 | 10% | 0.17 |
| Cyst A | 12 | 5% | 0 | 0% | 12 | 6% | 0.58 |
| Ventricular/dilation | 1 | 0% | 0 | 0% | 1 | 0% | 1.0 |
| Hydrocephalus | 8 | 3% | 0 | 0% | 8 | 4% | 1.0 |
| Hematoma | 3 | 1% | 0 | 0% | 3 | 1% | 1.0 |
| Sinusitis | 2 | 1% | 0 | 0% | 2 | 1% | 1.0 |
| Encephalomalacia | 1 | 0% | 0 | 0% | 1 | 0% | 1.0 |
| Hypoplasia of corpus callosum | 2 | 1% | 0 | 0% | 2 | 1% | 1.0 |
| Others B | 34 | 13% | 2 | 3% | 32 | 16% | 0.21 |
| Management Variable | All Patients ** N = 260 | Headache Type | p-Value * | ||||
|---|---|---|---|---|---|---|---|
| Primary N = 58 | Secondary N = 202 | ||||||
| Emergency department medications | |||||||
| N | % | N | % | N | % | ||
| Anesthetic in ER | 25 | 10% | 0 | 0% | 25 | 12% | 0.005 |
| Antiepileptic in ER | 8 | 3% | 0 | 0% | 8 | 4% | 0.12 |
| Antiemetic in ER | 39 | 15% | 10 | 17% | 29 | 14% | 0.58 |
| NSAID in ER | 76 | 29% | 24 | 41% | 52 | 26% | 0.021 |
| Acetaminophen in ER | 118 | 45% | 24 | 41% | 94 | 47% | 0.487 |
| Others in ER | 15 | 6% | 6 | 10% | 9 | 4% | 0.09 |
| Investigation | |||||||
| Basic screen tests | 218 | 84% | 44 | 76% | 174 | 86% | 0.061 |
| Blood culture | 84 | 32% | 11 | 19% | 73 | 36% | 0.014 |
| Urine culture | 53 | 20% | 6 | 10% | 47 | 23% | 0.031 |
| LP | 32 | 12% | 1 | 2% | 31 | 15% | 0.005 |
| VP shunt X-ray | 20 | 8% | 0 | 0% | 20 | 10% | 0.013 |
| Others | 49 | 19% | 12 | 21% | 37 | 18% | 0.684 |
| Outpatient medications | |||||||
| Acetaminophen in OP | 83 | 32% | 18 | 31% | 65 | 32% | 0.869 |
| Antiepileptic in OP | 8 | 3% | 2 | 3% | 6 | 3% | 0.853 |
| Antibiotics in OP | 24 | 9% | 1 | 2% | 23 | 11% | 0.025 |
| Vitamins supplements in OP | 16 | 6% | 5 | 9% | 11 | 5% | 0.375 |
| Antihistamine in OP | 12 | 5% | 2 | 3% | 10 | 5% | 0.631 |
| Corticosteroids in OP | 18 | 7% | 2 | 3% | 16 | 8% | 0.237 |
| NSAIDs in OP | 45 | 17% | 20 | 34% | 25 | 12% | <0.001 |
| Others in OP | 21 | 8% | 4 | 7% | 17 | 8% | 0.708 |
| Follow-up | |||||||
| Admission | 135 | 52% | 10 | 17% | 125 | 62% | <0.001 |
| Follow up | 163 | 63% | 41 | 71% | 122 | 60% | 0.153 |
| Persistent Headache | 29 | 11% | 12 | 21% | 17 | 8% | 0.009 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Almuqbil, M.; Alsayed, S.A.; Almutairi, A.M.; Aladhadh, K.M.; Alghannami, A.O.; Almutairi, M. Diagnostic Yield of Neuroimaging for Headache in a Pediatric Emergency Department: A Single Tertiary Centre Experience. Healthcare 2023, 11, 913. https://doi.org/10.3390/healthcare11060913
Almuqbil M, Alsayed SA, Almutairi AM, Aladhadh KM, Alghannami AO, Almutairi M. Diagnostic Yield of Neuroimaging for Headache in a Pediatric Emergency Department: A Single Tertiary Centre Experience. Healthcare. 2023; 11(6):913. https://doi.org/10.3390/healthcare11060913
Chicago/Turabian StyleAlmuqbil, Mohammed, Saud Abdulaziz Alsayed, Amer Mohammed Almutairi, Khalid Mohammed Aladhadh, Abdullah Omar Alghannami, and Mohammed Almutairi. 2023. "Diagnostic Yield of Neuroimaging for Headache in a Pediatric Emergency Department: A Single Tertiary Centre Experience" Healthcare 11, no. 6: 913. https://doi.org/10.3390/healthcare11060913
APA StyleAlmuqbil, M., Alsayed, S. A., Almutairi, A. M., Aladhadh, K. M., Alghannami, A. O., & Almutairi, M. (2023). Diagnostic Yield of Neuroimaging for Headache in a Pediatric Emergency Department: A Single Tertiary Centre Experience. Healthcare, 11(6), 913. https://doi.org/10.3390/healthcare11060913







