Risk Factors for Delayed-Onset Infection after Mandibular Wisdom Tooth Extractions
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Ethics Statement
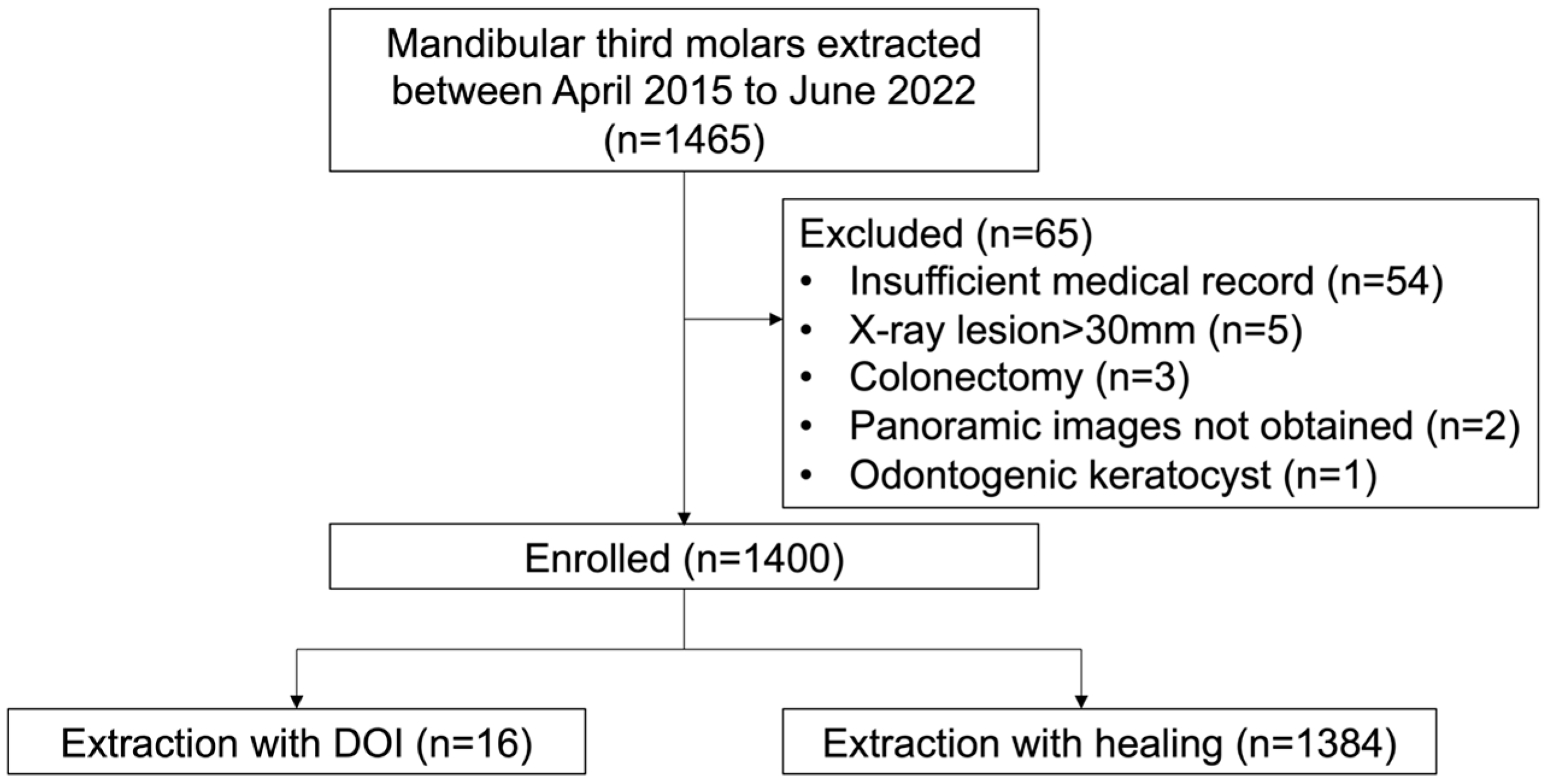
2.3. Patient Selection
2.4. Surgical Procedure and Postoperative Management
2.5. Outcome Variables
2.6. Predictive Variables
- Attributes (sex, age)
- Operative variables
- Anatomical variables
- Physical status
2.7. Statistical Analysis
3. Results
3.1. Univariate Analyses
3.2. Multivariate Logistic Regression Model Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sukegawa, S.; Yokota, K.; Kanno, T.; Manabe, Y.; Sukegawa-Takahashi, Y.; Masui, M.; Furuki, Y. What are the risk factors for postoperative infections of third molar extraction surgery: A retrospective clinical study? Med. Oral Patol. Oral Cir. Bucal. 2019, 24, e123–e129. [Google Scholar] [CrossRef] [PubMed]
- Bortoluzzi, M.C.; Manfro, R.; De Déa, B.E.; Dutra, T.C. Incidence of dry socket, alveolar infection, and postoperative pain following the extraction of erupted teeth. J. Contemp. Dent. Pr. 2010, 11, E033–E040. [Google Scholar] [CrossRef]
- Bouloux, G.F.; Steed, M.B.; Perciaccante, V.J. Complications of third molar surgery. Oral Maxillofac. Surg. Clin. N. Am. 2007, 19, 117–128. [Google Scholar] [CrossRef] [PubMed]
- Figueiredo, R.; Valmaseda-Castellón, E.; Berini-Aytés, L.; Gay-Escoda, C. Delayed-onset infections after lower third molar extraction: A case-control study. J. Oral Maxillofac. Surg. 2007, 65, 97–102. [Google Scholar] [CrossRef] [PubMed]
- Berge, T.I.; Bøe, O.E. Predictor evaluation of postoperative morbidity after surgical removal of mandibular third molars. Acta Odontol. Scand. 1994, 52, 162–169. [Google Scholar] [CrossRef]
- Goldberg, M.H.; Nemarich, A.N.; Marco, W.P., 2nd. Complications after mandibular third molar surgery: A statistical analysis of 500 consecutive procedures in private practice. J. Am. Dent. Assoc. 1985, 111, 277–279. [Google Scholar] [CrossRef]
- Piecuch, J.F.; Arzadon, J.; Lieblich, S.E. Prophylactic antibiotics for third molar surgery: A supportive opinion. J. Oral Maxillofac. Surg. 1995, 53, 53–60. [Google Scholar] [CrossRef]
- Bui, C.H.; Seldin, E.B.; Dodson, T.B. Types, frequencies, and risk factors for complications after third molar extraction. J. Oral Maxillofac. Surg. 2003, 61, 1379–1389. [Google Scholar] [CrossRef]
- Monaco, G.; Cecchini, S.; Gatto, M.R.; Pelliccioni, G.A. Delayed onset infections after lower third molar germectomy could be related to the space distal to the second molar. Int. J. Oral Maxillofac. Surg. 2017, 46, 373–378. [Google Scholar] [CrossRef]
- Figueiredo, R.; Valmaseda-Castellón, E.; Berini-Aytés, L.; Gay-Escoda, C. Incidence and clinical features of delayed-onset infections after extraction of lower third molars. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2005, 99, 265–269. [Google Scholar] [CrossRef]
- Kaposvári, I.; Körmöczi, K.; Csurgay, K.; Horváth, F.; Ashourioun, A.H.; Buglyó, A.; Turai, A.R.; Joób-Fancsaly, Á. Delayed-onset infections after lower third molar surgery: A Hungarian case-control study. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2021, 132, 641–647. [Google Scholar] [CrossRef] [PubMed]
- The International Expert Committee. International Expert Committee Report on the Role of the A1C Assay in the Diagnosis of Diabetes. Diabetes Care 2009, 32, 1327–1334. [Google Scholar] [CrossRef]
- Brunello, G.; De Biagi, M.; Crepaldi, G.; Rodrigues, F.I.; Sivolella, S. An observational cohort study on delayed-onset infections after mandibular third-molar extractions. Int. J. Dent. 2017, 2017, 1435348. [Google Scholar] [CrossRef] [PubMed]
- Blondeau, F.; Daniel, N.G. Extraction of impacted mandibular third molars: Postoperative complications and their risk factors. J. Can. Dent. Assoc. 2007, 73, 325. [Google Scholar] [PubMed]
- Osborn, T.P.; Frederickson, G., Jr.; Small, I.A.; Torgerson, T.S. A prospective study of complications related to mandibular third molar surgery. J. Oral Maxillofac. Surg. 1985, 43, 767–769. [Google Scholar] [CrossRef]
- Osunde, O.; Saheeb, B.; Bassey, G. Indications and risk factors for complications of lower third molar surgery in a Nigerian teaching hospital. Ann. Med. Health Sci. Res. 2014, 4, 938–942. [Google Scholar] [CrossRef]
- Waite, P.D.; Cherala, S. Surgical outcomes for suture-less surgery in 366 impacted third molar patients. J. Oral Maxillofac. Surg. 2006, 64, 669–673. [Google Scholar] [CrossRef]
- Lebendiger, A.; Gitlitz, G.F.; Hurwitt, E.S.; Lord, G.H.; Henderson, J. Laboratory and clinical evaluation of a new absorbable hemostatic material prepared from oxidized regenerated cellulose. Surg. Forum 1960, 10, 440–443. [Google Scholar]
- Al-Shammari, K.F.; Al-Khabbaz, A.K.; Al-Ansari, J.M.; Neiva, R.; Wang, H.L. Risk indicators for tooth loss due to periodontal disease. J. Periodontol. 2005, 76, 1910–1918. [Google Scholar] [CrossRef]
- Tada, A.; Tano, R.; Miura, H. The relationship between tooth loss and hypertension: A systematic review and meta-analysis. Sci. Rep. 2022, 12, 13311. [Google Scholar] [CrossRef]
- Epstein, J.B.; Chong, S.; Le, N.D. A survey of antibiotic use in dentistry. J. Am. Dent. Assoc. 2000, 131, 1600–1609. [Google Scholar] [CrossRef]
- Davies, S.C.; Fowler, T.; Watson, J.; Livermore, D.M.; Walker, D. Annual Report of the Chief Medical Officer: Infection and the Rise of Antimicrobial Resistance. Lancet 2013, 381, 1606–1609. [Google Scholar] [CrossRef] [PubMed]
- Chardin, H.; Yasukawa, K.; Nouacer, N.; Plainvert, C.; Aucouturier, P.; Ergani, A.; Descroix, V.; Toledo-Arenas, R.; Azerad, J.; Bouvet, A. Reduced susceptibility to amoxicillin of oral streptococci following amoxicillin exposure. J. Med. Microbiol. 2009, 58, 1092–1097. [Google Scholar] [CrossRef] [PubMed]
- Khalil, D.; Hultin, M.; Rashid, M.U.; Lund, B. Oral microflora and selection of resistance after a single dose of amoxicillin. Clin. Microbiol. Infect. 2016, 22, e941–e949. [Google Scholar] [CrossRef] [PubMed]
- Sifuentes-Cervantes, J.S.; Carrillo-Morales, F.; Castro-Núñez, J.; Cunningham, L.L.; Van Sickels, J.E. Third molar surgery: Past, present, and the future. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2021, 132, 523–531. [Google Scholar] [CrossRef]
- Lodi, G.; Azzi, L.; Varoni, E.M.; Pentenero, M.; Del Fabbro, M.; Carrassi, A.; Sardella, A.; Manfredi, M. Antibiotics to prevent complications following tooth extractions. Cochrane Database Syst. Rev. 2021, 2, Cd003811. [Google Scholar] [PubMed]
- Steel, B.J.; Surendran, K.S.B.; Braithwaite, C.; Mehta, D.; Keith, D.J.W. Current thinking in lower third molar surgery. Br. J. Oral Maxillofac. Surg. 2022, 60, 257–265. [Google Scholar] [CrossRef]
- Figueiredo, R.; Valmaseda-Castellón, E.; Formoso-Senande, M.F.; Berini-Aytés, L.; Gay-Escoda, C. Delayed-onset infections after impacted lower third molar extraction: Involved bacteria and sensitivity profiles to commonly used antibiotics. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2012, 114, 43–48. [Google Scholar] [CrossRef]
- Figueiredo, R.; Valmaseda-Castellón, E.; Laskin, D.M.; Berini-Aytés, L.; Gay-Escoda, C. Treatment of delayed-onset infections after impacted lower third molar extraction. J. Oral Maxillofac. Surg. 2008, 66, 943–947. [Google Scholar] [CrossRef]
- Azab, M.; Ibrahim, S.; Li, A.; Khosravirad, A.; Carrasco-Labra, A.; Zeng, L.; Brignardello-Petersen, R. Efficacy of secondary vs primary closure techniques for the prevention of postoperative complications after impacted mandibular third molar extractions: A systematic review update and meta-analysis. J. Am. Dent. Assoc. 2022, 153, 943–956.e948. [Google Scholar] [CrossRef]
| Healing | DOI | p-Value | ||
|---|---|---|---|---|
| Outcome (%) | 1384 (98.9%) | 16 (1.1%) | ||
| Attribute variables | ||||
| Age | 32.4 ± 14.1 | 37.7 ± 20.9 | 0.143 | |
| Sex | Male | 564 | 5 | 0.610 |
| Female | 820 | 11 | ||
| Operative variables | ||||
| Simultaneous left and right extraction | Yes | 440 | 3 | 0.417 |
| No | 944 | 13 | ||
| Simultaneous maxilla and mandible extraction | Yes | 344 | 6 | 0.251 |
| No | 1040 | 10 | ||
| Specialist | Yes | 175 | 4 | 0.137 |
| No | 1209 | 12 | ||
| Anatomical variables | ||||
| Class | Ⅰ | 482 | 3 | 0.003 |
| Ⅱ | 712 | 6 | ||
| Ⅲ | 190 | 7 | ||
| Position | A | 758 | 2 | 0.003 |
| B | 487 | 10 | ||
| C | 139 | 4 | ||
| Right or left | Left | 706 | 5 | 0.136 |
| Right | 678 | 11 | ||
| No. of wisdom tooth roots | Immature root | 100 | 4 | 0.058 |
| 1 | 492 | 4 | ||
| 2 | 778 | 8 | ||
| 3 | 14 | 0 | ||
| Wisdom tooth follicular cyst | Yes | 44 | 2 | 0.095 |
| No | 1340 | 14 | ||
| Wisdom tooth radicular cyst | Yes | 8 | 0 | 1.000 |
| No | 1376 | 16 | ||
| Wisdom tooth root canal filling | Yes | 7 | 0 | 1.000 |
| No | 1377 | 16 | ||
| Physical status | ||||
| Height | 162.2 ± 8.5 | 160.1 ± 9.7 | 0.319 | |
| Weight | 58.6 ± 12.3 | 59.9 ± 19.2 | 0.672 | |
| BMI | 22.1 ± 3.7 | 23.0 ± 4.6 | 0.343 | |
| Hypertension | Yes | 76 | 4 | 0.011 |
| No | 1308 | 12 | ||
| Diabetes | Yes | 34 | 0 | 1.000 |
| No | 1350 | 16 | ||
| Bisphosphonate | Yes | 10 | 1 | 0.119 |
| No | 1372 | 15 | ||
| Corticosteroid | Yes | 24 | 0 | 1.000 |
| No | 1360 | 16 | ||
| Contraceptives | Yes | 11 | 0 | 1.000 |
| No | 1373 | 16 | ||
| Smoking | Yes | 179 | 3 | 0.452 |
| No | 1205 | 13 | ||
| Alcohol consumption | Yes | 212 | 3 | 0.725 |
| No | 1172 | 13 | ||
| Hemostatic agent | Yes | 58 | 4 | 0.004 |
| No | 1326 | 12 | ||
| Preoperative SBP | 125.3 ± 17.0 | 133 ± 20.8 | 0.075 | |
| Preoperative DBP | 77.1 ± 24.3 | 77.0 ± 13.9 | 0.984 | |
| SBP after local anesthesia | 121.6 ± 18.3 | 121.4 ± 19.9 | 0.955 | |
| DBP after local anesthesia | 71.0 ± 13.9 | 71.9 ± 15.0 | 0.796 | |
| Postoperative SBP | 122.1 ± 17.4 | 121.8 ± 14.6 | 0.946 | |
| Postoperative DBP | 73.3 ± 14.6 | 70.0 ± 13.9 | 0.361 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Miyazaki, R.; Sukegawa, S.; Nakagawa, K.; Nakai, F.; Nakai, Y.; Ishihama, T.; Miyake, M. Risk Factors for Delayed-Onset Infection after Mandibular Wisdom Tooth Extractions. Healthcare 2023, 11, 871. https://doi.org/10.3390/healthcare11060871
Miyazaki R, Sukegawa S, Nakagawa K, Nakai F, Nakai Y, Ishihama T, Miyake M. Risk Factors for Delayed-Onset Infection after Mandibular Wisdom Tooth Extractions. Healthcare. 2023; 11(6):871. https://doi.org/10.3390/healthcare11060871
Chicago/Turabian StyleMiyazaki, Ryo, Shintaro Sukegawa, Ken Nakagawa, Fumi Nakai, Yasuhiro Nakai, Takanori Ishihama, and Minoru Miyake. 2023. "Risk Factors for Delayed-Onset Infection after Mandibular Wisdom Tooth Extractions" Healthcare 11, no. 6: 871. https://doi.org/10.3390/healthcare11060871
APA StyleMiyazaki, R., Sukegawa, S., Nakagawa, K., Nakai, F., Nakai, Y., Ishihama, T., & Miyake, M. (2023). Risk Factors for Delayed-Onset Infection after Mandibular Wisdom Tooth Extractions. Healthcare, 11(6), 871. https://doi.org/10.3390/healthcare11060871






