Impact of Disability Status on Mortality in Patients with Gastric Cancer: A Nationwide Study Focusing on Regional Disparities
Abstract
1. Introduction
2. Methods
2.1. Data and Study Population
2.2. Outcome Measures
2.3. Independent Variables
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Torre, L.A.; Bray, F.; Siegel, R.L.; Ferlay, J.; Lortet-Tieulent, J.; Jemal, A. Global cancer statistics, 2012. CA Cancer J. Clin. 2015, 65, 87–108. [Google Scholar] [CrossRef]
- Rawla, P.; Barsouk, A. Epidemiology of gastric cancer: Global trends, risk factors and prevention. Gastroenterol. Rev./Przegląd Gastroenterol. 2019, 14, 26–38. [Google Scholar] [CrossRef] [PubMed]
- Park, Y.; Ki, M. Population Attributable Fraction of Helicobacter pylori Infection–Related Gastric Cancer in Korea: A Meta-Analysis. Cancer Res. Treat. 2021, 53, 744–753. [Google Scholar] [CrossRef] [PubMed]
- Jung, K.-W.; Won, Y.-J.; Hong, S.; Kong, H.-J.; Im, J.-S.; Seo, H.G. Prediction of Cancer Incidence and Mortality in Korea, 2021. Cancer Res. Treat. 2021, 53, 316–322. [Google Scholar] [CrossRef]
- Hoang, T.; Woo, H.; Cho, S.; Lee, J.; Kazmi, S.Z.; Shin, A. Descriptive Analysis of Gastric Cancer Mortality in Korea, 2000–2020. Cancer Res. Treat. 2022, 6, 307. [Google Scholar] [CrossRef]
- Jung, K.-W.; Won, Y.-J.; Kong, H.-J.; Oh, C.-M.; Shin, A.; Lee, J.-S. Survival of Korean Adult Cancer Patients by Stage at Diagnosis, 2006–2010: National Cancer Registry Study. Cancer Res. Treat. 2013, 45, 162–171. [Google Scholar] [CrossRef]
- Kim, H.W.; Shin, D.W.; Yeob, K.E.; Cho, I.Y.; Kim, S.Y.; Park, S.M.; Park, J.H.; Kawachi, I. Disparities in the Diagnosis and Treatment of Gastric Cancer in Relation to Disabilities. Clin. Transl. Gastroenterol. 2020, 11, e00242. [Google Scholar] [CrossRef]
- Jeon, B.; Kwon, S.; Kim, H. Health care utilization by people with disabilities: A longitudinal analysis of the Korea Welfare Panel Study (KoWePS). Disabil. Health J. 2015, 8, 353–362. [Google Scholar] [CrossRef]
- Verlenden, J.V.; Zablotsky, B.; Yeargin-Allsopp, M.; Peacock, G. Healthcare Access and Utilization for Young Adults with Disability: U.S., 2014–2018. J. Adolesc. Health 2022, 70, 241–248. [Google Scholar] [CrossRef]
- Lee, J.-E.; Kim, H.-R.; Shin, H.-I. Accessibility of medical services for persons with disabilities: Comparison with the general population in Korea. Disabil. Rehabil. 2013, 36, 1728–1734. [Google Scholar] [CrossRef] [PubMed]
- Son, K.Y.; Kim, S.H.; Sunwoo, S.; Lee, J.-Y.; Lim, S.; Kim, Y.S. Association between disability and cardiovascular event and mortality: A nationwide representative longitudinal study in Korea. PLoS ONE 2020, 15, e0236665. [Google Scholar] [CrossRef] [PubMed]
- Shin, D.W.; Cho, J.H.; Noh, J.M.; Han, H.; Han, K.; Park, S.H.; Kim, S.Y.; Park, J.H.; Kawachi, I. Disparities in the Diagnosis and Treatment of Lung Cancer among People with Disabilities. J. Thorac. Oncol. 2019, 14, 163–175. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Shin, D.W.; Kim, H.W.; Jung, J.H.; Han, K.; Cho, I.Y.; Kim, S.Y.; Choi, K.S.; Park, J.H.; Kawachi, I. Disparities in gastric cancer screening among people with disabilities: A national registry-linkage study in South Korea. Gastric Cancer 2020, 23, 497–509. [Google Scholar] [CrossRef]
- Sharby, N.; Martire, K.; Iversen, M.D. Decreasing Health Disparities for People with Disabilities through Improved Communication Strategies and Awareness. Int. J. Environ. Res. Public Health 2015, 12, 3301–3316. [Google Scholar] [CrossRef] [PubMed]
- Cho, S.; Chang, Y.; Kim, Y. Cancer Patients’ Utilization of Tertiary Hospitals in Seoul Before and After the Benefit Expansion Policy. J. Prev. Med. Public Health 2019, 52, 41–50. [Google Scholar] [CrossRef]
- Ministry of Health and Welfare. Division Policy for People with Disabilities. 2022. Available online: http://www.mohw.go.kr/react/policy/index.jsp?PAR_MENU_ID=06&MENU_ID=06370111&PAGE=11&topTitle= (accessed on 24 November 2022).
- Jeon, B.; Noguchi, H.; Kwon, S.; Ito, T.; Tamiya, N. Disability, poverty, and role of the basic livelihood security system on health services utilization among the elderly in South Korea. Soc. Sci. Med. 2017, 178, 175–183. [Google Scholar] [CrossRef]
- Sundararajan, V.; Henderson, T.; Perry, C.; Muggivan, A.; Quan, H.; Ghali, W.A. New ICD-10 version of the Charlson comorbidity index predicted in-hospital mortality. J. Clin. Epidemiol. 2004, 57, 1288–1294. [Google Scholar] [CrossRef]
- Cuypers, M.; Schalk, B.W.M.; Boonman, A.J.N.; Naaldenberg, J.; Leusink, G.L. Cancer-related mortality among people with intellectual disabilities: A nationwide population-based cohort study. Cancer 2021, 128, 1267–1274. [Google Scholar] [CrossRef]
- Choi, J.Y.; Yeob, K.E.; Hong, S.H.; Kim, S.Y.; Jeong, E.-H.; Shin, D.W.; Park, J.H.; Kang, G.-W.; Kim, H.S.; Kawachi, I. Disparities in the Diagnosis, Treatment, and Survival Rate of Cervical Cancer among Women with and without Disabilities. Cancer Control 2021, 28, 10732748211055268. [Google Scholar] [CrossRef]
- Park, S.M.; Son, K.Y.; Park, J.-H.; Cho, B. Disparities in short-term and long-term all-cause mortality among Korean cancer patients with and without preexisting disabilities: A nationwide retrospective cohort study. Support. Care Cancer 2011, 20, 963–970. [Google Scholar] [CrossRef] [PubMed]
- Yoo, K.-Y. Cancer Control Activities in the Republic of Korea. Jpn. J. Clin. Oncol. 2008, 38, 327–333. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.S. Polarization of cancer patient management. J. Korean Med. Assoc. 2017, 60, 223. [Google Scholar] [CrossRef]
- Lee, S. Spatial and Socioeconomic Inequalities in Accessibility to Healthcare Services in South Korea. Healthcare 2022, 10, 2049. [Google Scholar] [CrossRef] [PubMed]
- Lezzoni, L.I.; Kileen, M.B.; O’Day, B.L. Rural Residents with Disabilities Confront Substantial Barriers to Obtaining Primary Care. Health Serv. Res. 2006, 41, 1258–1275. [Google Scholar]
- Dassah, E.; Aldersey, H.; McColl, M.A.; Davison, C. Factors affecting access to primary health care services for persons with disabilities in rural areas: A “best-fit” framework synthesis. Glob. Health Res. Policy 2018, 3, 36. [Google Scholar] [CrossRef]
- Lee, Y.J. A study on the spatial differences in cancer patients’ health care utilization and treatment of medical institutions. Korea Spat. Plan. Rev. 2009, 60, 97–114. [Google Scholar]
| Variables | Total | 1-Year Mortality | 5-Year Mortality | Overall Mortality | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | (%) | p-Value | N | (%) | p-Value | N | (%) | p-Value | ||
| Disability status | ||||||||||
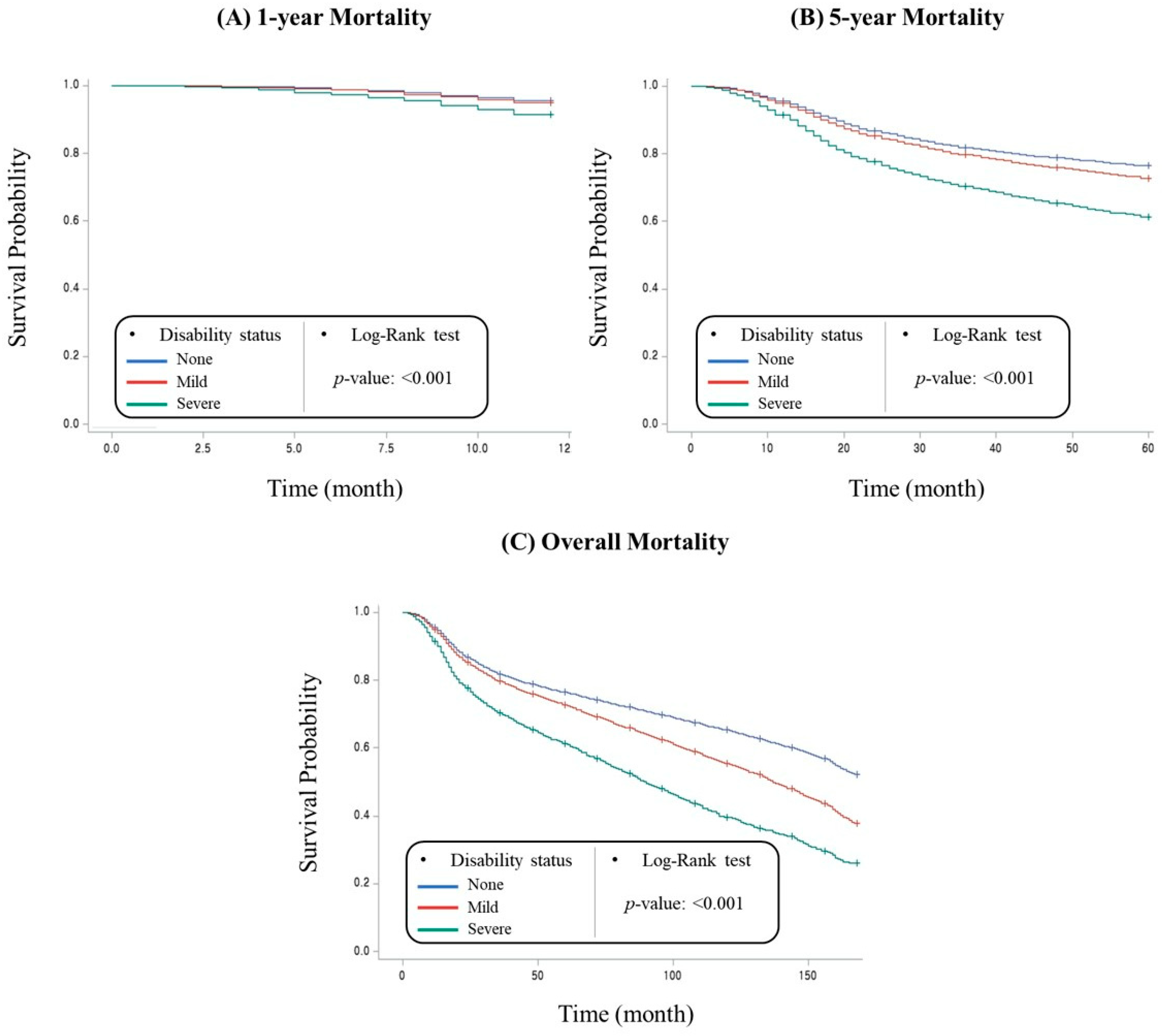
| No | 178,026 | 7786 | (4.4) | <0.001 | 41,333 | (23.2) | <0.001 | 60,707 | (34.1) | <0.001 |
| Mild | 19,297 | 989 | (5.1) | 5161 | (26.7) | 8316 | (43.1) | |||
| Severe | 3243 | 275 | (8.5) | 1224 | (37.7) | 1850 | (57.0) | |||
| Sex | ||||||||||
| Male | 136,611 | 6481 | (4.7) | <0.001 | 34,046 | (24.9) | <0.001 | 51,276 | (37.5) | <0.001 |
| Female | 63,955 | 2569 | (4.0) | 13,672 | (21.4) | 19,597 | (30.6) | |||
| Age | ||||||||||
| 19–49 | 34,217 | 1309 | (3.8) | <0.001 | 7415 | (21.7) | <0.001 | 8953 | (26.2) | <0.001 |
| 50–59 | 50,324 | 1710 | (3.4) | 9775 | (19.4) | 12,896 | (25.6) | |||
| 60–69 | 58,489 | 2189 | (3.7) | 12,342 | (21.1) | 18,965 | (32.4) | |||
| 70–79 | 48,402 | 2826 | (5.8) | 14,146 | (29.2) | 23,859 | (49.3) | |||
| ≥80 | 9134 | 1016 | (11.1) | 4040 | (44.2) | 6200 | (67.9) | |||
| Income | ||||||||||
| Low | 41,041 | 2210 | (5.4) | <0.001 | 11,050 | (26.9) | <0.001 | 16,379 | (39.9) | <0.001 |
| Low–middle | 41,223 | 1969 | (4.8) | 10,313 | (25.0) | 14,732 | (35.7) | |||
| Middle–high | 59,765 | 2532 | (4.2) | 13,772 | (23.0) | 20,295 | (34.0) | |||
| High | 58,537 | 2339 | (4.0) | 12,583 | (21.5) | 19,467 | (33.3) | |||
| Type of healthcare insurance | ||||||||||
| Medical Aid | 8470 | 651 | (7.7) | <0.001 | 2890 | (34.1) | <0.001 | 4551 | (53.7) | <0.001 |
| NHI * Self employed | 66,347 | 3269 | (4.9) | 16,888 | (25.5) | 24,242 | (36.5) | |||
| NHI * Employee | 125,749 | 5130 | (4.1) | 27,940 | (22.2) | 42,080 | (33.5) | |||
| Region | ||||||||||
| Capital city | 126,267 | 5577 | (4.4) | 0.007 | 29,645 | (23.5) | <0.001 | 43,247 | (34.3) | <0.001 |
| Other areas | 74,299 | 3473 | (4.7) | 18,073 | (24.3) | 27,626 | (37.2) | |||
| Charlson Comorbidity Index | ||||||||||
| 0 | 54,753 | 407 | (0.7) | <0.001 | 5633 | (10.3) | <0.001 | 10,702 | (19.5) | <0.001 |
| 1 | 24,806 | 339 | (1.4) | 3311 | (13.3) | 6843 | (27.6) | |||
| 2 | 33,826 | 500 | (1.5) | 4766 | (14.1) | 8696 | (25.7) | |||
| ≥3 | 87,181 | 7804 | (9.0) | 34,008 | (39.0) | 44,632 | (51.2) | |||
| Type of treatment | ||||||||||
| Surgery only | 147,392 | 3010 | (2.0) | <0.001 | 15,750 | (10.7) | <0.001 | 33,524 | (22.7) | <0.001 |
| Surgery and Chemo or radiotherapy | 39,705 | 2403 | (6.1) | 20,239 | (51.0) | 25,441 | (64.1) | |||
| Chemo or radiotherapy only | 13,469 | 3637 | (27.0) | 11,729 | (87.1) | 11,908 | (88.4) | |||
| Type of hospital | ||||||||||
| Tertiary hospital | 140,015 | 5585 | (4.0) | <0.001 | 31,038 | (22.2) | <0.001 | 46,407 | (33.1) | <0.001 |
| General hospital | 60,551 | 3465 | (5.7) | 16,680 | (27.5) | 24,466 | (40.4) | |||
| Total | 200,566 | 9050 | (4.5) | 47,718 | (23.8) | 70,873 | (35.3) | |||
| Variables | 1-Year Mortality | 5-Year Mortality | Overall Mortality | ||||||
|---|---|---|---|---|---|---|---|---|---|
| HR * | 95% CI * | HR * | 95% CI * | HR * | 95% CI * | ||||
| Disability status | |||||||||
| None | 1.00 | 1.00 | 1.00 | ||||||
| Mild | 1.04 | (0.97) | (1.11) | 1.07 | (1.04) | (1.11) | 1.12 | (1.09) | (1.14) |
| Severe | 1.61 | (1.42) | (1.81) | 1.62 | (1.53) | (1.71) | 1.64 | (1.57) | (1.72) |
| Sex | |||||||||
| Male | 1.00 | 1.00 | 1.00 | ||||||
| Female | 0.88 | (0.84) | (0.92) | 0.89 | (0.87) | (0.90) | 0.79 | (0.78) | (0.81) |
| Age | |||||||||
| 19–49 | 1.00 | 1.00 | 1.00 | ||||||
| 50–59 | 0.93 | (0.87) | (1.00) | 0.92 | (0.89) | (0.95) | 0.99 | (0.96) | (1.01) |
| 60–69 | 1.03 | (0.96) | (1.11) | 1.03 | (1.00) | (1.06) | 1.30 | (1.27) | (1.33) |
| 70–79 | 1.69 | (1.58) | (1.81) | 1.74 | (1.69) | (1.80) | 2.57 | (2.51) | (2.63) |
| ≥80 | 3.82 | (3.50) | (4.16) | 3.91 | (3.76) | (4.07) | 5.62 | (5.44) | (5.82) |
| Income | |||||||||
| Low | 1.00 | 1.00 | 1.00 | ||||||
| Low–middle | 0.98 | (0.91) | (1.05) | 0.97 | (0.95) | (1.00) | 0.99 | (0.96) | (1.01) |
| Middle–high | 0.91 | (0.85) | (0.96) | 0.92 | (0.90) | (0.95) | 0.92 | (0.89) | (0.94) |
| High | 0.85 | (0.80) | (0.91) | 0.86 | (0.84) | (0.89) | 0.85 | (0.83) | (0.87) |
| Type of healthcare insurance | |||||||||
| Medical Aid | 1.00 | 1.00 | 1.00 | ||||||
| NHI Self employed | 0.91 | (0.82) | (1.00) | 0.97 | (0.93) | (1.02) | 0.91 | (0.88) | (0.95) |
| NHI Employee | 0.80 | (0.73) | (0.88) | 0.88 | (0.85) | (0.92) | 0.84 | (0.81) | (0.87) |
| Region | |||||||||
| Capital city | 1.00 | 1.00 | 1.00 | ||||||
| Other areas | 1.00 | (0.96) | (1.05) | 1.01 | (0.99) | (1.03) | 1.02 | (1.00) | (1.03) |
| Charlson Comorbidity Index | |||||||||
| 0 | 1.00 | 1.00 | 1.00 | ||||||
| 1 | 1.67 | (1.44) | (1.93) | 1.25 | (1.19) | (1.30) | 1.29 | (1.25) | (1.33) |
| 2 | 1.75 | (1.53) | (1.99) | 1.23 | (1.18) | (1.28) | 1.24 | (1.20) | (1.27) |
| ≥3 | 6.08 | (5.49) | (6.73) | 2.51 | (2.43) | (2.58) | 2.12 | (2.07) | (2.17) |
| Type of treatment | |||||||||
| Surgery only | 1.00 | 1.00 | 1.00 | ||||||
| Surgery and Chemo or radiotherapy | 2.59 | (2.45) | (2.73) | 6.34 | (6.20) | (6.48) | 4.58 | (4.51) | (4.66) |
| Chemo or radiotherapy only | 9.44 | (8.97) | (9.94) | 22.03 | (21.45) | (22.63) | 17.37 | (16.96) | (17.78) |
| Type of hospital | |||||||||
| Tertiary hospital | 1.00 | 1.00 | 1.00 | ||||||
| General hospital | 1.21 | (1.16) | (1.26) | 1.12 | (1.10) | (1.14) | 1.08 | (1.07) | (1.10) |
| Subgroup | 1-Year Mortality | 5-Year Mortality | Overall Mortality | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| HR * | 95% CI * | HR * | 95% CI * | HR * | 95% CI * | |||||
| Region | Disability status | |||||||||
| Capital city | None | 1.00 | 1.00 | 1.00 | ||||||
| Mild | 0.96 | (0.81) | (1.14) | 1.04 | (0.96) | (1.12) | 1.12 | (1.06) | (1.19) | |
| Severe | 1.23 | (0.89) | (1.70) | 1.46 | (1.26) | (1.69) | 1.45 | (1.28) | (1.63) | |
| Other areas | None | 1.00 | 1.00 | 1.00 | ||||||
| Mild | 1.05 | (0.98) | (1.13) | 1.08 | (1.05) | (1.12) | 1.11 | (1.09) | (1.14) | |
| Severe | 1.69 | (1.48) | (1.92) | 1.65 | (1.55) | (1.76) | 1.68 | (1.60) | (1.77) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, W.-R.; Han, K.-T.; Choi, M.; Park, S.; Kim, W. Impact of Disability Status on Mortality in Patients with Gastric Cancer: A Nationwide Study Focusing on Regional Disparities. Healthcare 2023, 11, 641. https://doi.org/10.3390/healthcare11050641
Lee W-R, Han K-T, Choi M, Park S, Kim W. Impact of Disability Status on Mortality in Patients with Gastric Cancer: A Nationwide Study Focusing on Regional Disparities. Healthcare. 2023; 11(5):641. https://doi.org/10.3390/healthcare11050641
Chicago/Turabian StyleLee, Woo-Ri, Kyu-Tae Han, Mingee Choi, Seojin Park, and Woorim Kim. 2023. "Impact of Disability Status on Mortality in Patients with Gastric Cancer: A Nationwide Study Focusing on Regional Disparities" Healthcare 11, no. 5: 641. https://doi.org/10.3390/healthcare11050641
APA StyleLee, W.-R., Han, K.-T., Choi, M., Park, S., & Kim, W. (2023). Impact of Disability Status on Mortality in Patients with Gastric Cancer: A Nationwide Study Focusing on Regional Disparities. Healthcare, 11(5), 641. https://doi.org/10.3390/healthcare11050641






