Benzodiazepine-Receptor Agonist Utilization in Outpatients with Anxiety Disorder: A Retrospective Study Based on Electronic Healthcare Data from a Large General Tertiary Hospital
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Craske, M.G.; Stein, M.B. Anxiety. Lancet 2016, 388, 3048–3059. [Google Scholar] [CrossRef]
- Szuhany, K.L.; Simon, N.M. Anxiety Disorders: A Review. JAMA 2022, 328, 2431–2445. [Google Scholar] [CrossRef] [PubMed]
- Hendriks, S.M.; Spijker, J.; Licht, C.M.; Hardeveld, F.; de Graaf, R.; Batelaan, N.M.; Penninx, B.W.; Beekman, A.T. Long-term disability in anxiety disorders. BMC Psychiatry 2016, 16, 248. [Google Scholar] [CrossRef]
- McLean, C.P.; Asnaani, A.; Litz, B.T.; Hofmann, S.G. Gender differences in anxiety disorders: Prevalence, course of illness, comorbidity and burden of illness. J. Psychiatr. Res. 2011, 45, 1027–1035. [Google Scholar] [CrossRef] [PubMed]
- Konnopka, A.; König, H. Economic Burden of Anxiety Disorders: A Systematic Review and Meta-Analysis. Pharmacoeconomics 2020, 38, 25–37. [Google Scholar] [CrossRef] [PubMed]
- Baxter, A.J.; Scott, K.M.; Vos, T.; Whiteford, H.A. Global prevalence of anxiety disorders: A systematic review and meta-regression. Psychol. Med. 2013, 43, 897–910. [Google Scholar] [CrossRef]
- Olfson, M.; King, M.; Schoenbaum, M. Benzodiazepine use in the United States. JAMA Psychiatry 2015, 72, 136–142. [Google Scholar] [CrossRef]
- Davies, J.; Rae, T.C.; Montagu, L. Long-term benzodiazepine and Z-drugs use in England: A survey of general practice. Br. J. Gen. Pract. 2017, 67, e609–e613. [Google Scholar] [CrossRef] [PubMed]
- Lou, G.; Yu, Z.; Chen, L.; Zhou, Y.; Zhang, L. Trends in Prescriptions for Insomnia in a Province in China Between 2015 and 2019. Front. Psychiatry 2022, 13, 915823. [Google Scholar] [CrossRef]
- Guina, J.; Merrill, B. Benzodiazepines I: Upping the Care on Downers: The Evidence of Risks, Benefits and Alternatives. J. Clin. Med. 2018, 7, 17. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.; Xu, J.; Li, C.; Wang, G.; Wang, W.; Ye, Y.; Chen, Y.; Liu, T.; Zhao, M.; Wang, X.; et al. Hazardous use of benzodiazepine receptor agonists in psychiatric clinics in China: Electronic prescription database study. BJPsych Open 2022, 8, e188. [Google Scholar] [CrossRef] [PubMed]
- Brandt, J.; Alessi-Severini, S.; Singer, A.; Leong, C. Novel Measures of Benzodiazepine and Z-Drug Utilisation Trends in a Canadian Provincial Adult Population (2001–2016). J. Popul. Ther. Clin. Pharmacol. 2019, 26, e22–e38. [Google Scholar] [CrossRef]
- Jackson, G.; Gerard, C.; Minko, N.; Parsotam, N. Variation in benzodiazepine and antipsychotic use in people aged 65 years and over in New Zealand. N. Z. Med. J. 2014, 127, 67–78. [Google Scholar]
- Koyama, A.; Steinman, M.; Ensrud, K.; Hillier, T.; Yaffe, K. Ten-year trajectory of potentially inappropriate medications in very old women: Importance of cognitive status. J. Am. Geriatr. Soc. 2013, 61, 258–263. [Google Scholar] [CrossRef] [PubMed]
- Brandt, J.; Janzen, D.; Alessi-Severini, S.; Singer, A.; Chateau, D.; Enns, M.; Leong, C. Risk of long-term benzodiazepine and Z-drug use following the first prescription among community-dwelling adults with anxiety/mood and sleep disorders: A retrospective cohort study. BMJ Open 2021, 11, e046916. [Google Scholar] [CrossRef]
- Spanemberg, L.; Nogueira, E.L.; Silva, C.T.B.; Dargél, A.A.; Menezes, F.S.; Neto, A.C. High prevalence and prescription of benzodiazepines for elderly: Data from psychiatric consultation to patients from an emergency room of a general hospital. Gen. Hosp. Psychiatry 2011, 33, 45–50. [Google Scholar] [CrossRef]
- Zivković, K.; Zelić-Kerep, A.; Stimac, D.; Ozić, S.; Zivković, N. A study on the quality of outpatient prescription of psychopharmaceuticals in the City of Zagreb 2006-2009. Coll Antropol. 2014, 38, 717–724. [Google Scholar] [PubMed]
- Rosenbaum, J.F. The drug treatment of anxiety. N. Engl. J. Med. 1982, 306, 401–404. [Google Scholar] [CrossRef] [PubMed]
- Schutte-Rodin, S.; Broch, L.; Buysse, D.; Dorsey, C.; Sateia, M. Clinical guideline for the evaluation and management of chronic insomnia in adults. J. Clin. Sleep Med. 2008, 4, 487–504. [Google Scholar] [CrossRef]
- Wilson, S.; Anderson, K.; Baldwin, D.; Dijk, D.-J.; Espie, A.; Espie, C.; Gringras, P.; Krystal, A.; Nutt, D.; Selsick, H.; et al. British Association for Psychopharmacology consensus statement on evidence-based treatment of insomnia, parasomnias and circadian rhythm disorders: An update. J. Psychopharmacol. 2019, 33, 923–947. [Google Scholar] [CrossRef]
- Cook, B.; Creedon, T.; Wang, Y.; Lu, C.; Carson, N.; Jules, P.; Lee, E.; Alegría, M. Examining racial/ethnic differences in patterns of benzodiazepine prescription and misuse. Drug Alcohol Depend. 2018, 187, 29–34. [Google Scholar] [CrossRef] [PubMed]
- Giorno, R.D.; Schneiders, C.; Stefanelli, K.; Ceschi, A.; Gyoerik-Lora, S.; Aletto, I.; Gabutti, L. Unexpected Increase in Benzodiazepine Prescriptions Related to the Introduction of an Electronic Prescribing Tool: Evidence from Multicenter Hospital Data. Diagnostics 2019, 9, 190. [Google Scholar] [CrossRef]
- Chouinard, G. Issues in the clinical use of benzodiazepines: Potency, withdrawal, and rebound. J. Clin. Psychiatry 2004, 65, 7–12. [Google Scholar]
- Bandelow, B. Current and Novel Psychopharmacological Drugs for Anxiety Disorders. Adv. Exp. Med. Biol. 2020, 1191, 347–365. [Google Scholar] [CrossRef]
- Gomez, A.F.; Barthel, A.L.; Hofmann, S.G. Comparing the efficacy of benzodiazepines and serotonergic anti-depressants for adults with generalized anxiety disorder: A meta-analytic review. Expert Opin. Pharmacother. 2018, 19, 883–894. [Google Scholar] [CrossRef]
- Fava, G.A.; Benasi, G.; Lucente, M.; Offidani, E.; Cosci, F.; Guidi, J. Withdrawal Symptoms after Serotonin-Noradrenaline Reuptake Inhibitor Discontinuation: Systematic Review. Psychother. Psychosom. 2018, 87, 195–203. [Google Scholar] [CrossRef]
- Cosci, F.; Chouinard, G. Acute and Persistent Withdrawal Syndromes Following Discontinuation of Psychotropic Medications. Psychother. Psychosom. 2020, 89, 283–306. [Google Scholar] [CrossRef] [PubMed]
- Starcevic, V. The reappraisal of benzodiazepines in the treatment of anxiety and related disorders. Expert Rev. Neurother. 2014, 14, 1275–1286. [Google Scholar] [CrossRef]
- Bushnell, G.A.; Rynn, M.A.; Crystal, S.; Gerhard, T.; Olfson, M. Simultaneous Benzodiazepine and SSRI Initiation in Young People with Anxiety Disorders. J. Clin. Psychiatry 2021, 82, 13863. [Google Scholar] [CrossRef] [PubMed]
- Lader, M. Benzodiazepines revisited--will we ever learn? Addiction 2011, 106, 2086–2109. [Google Scholar] [CrossRef]
- Barker, M.J.; Greenwood, K.M.; Jackson, M.; Crowe, S.M. Persistence of cognitive effects after withdrawal from long-term benzodiazepine use: A meta-analysis. Arch. Clin. Neuropsychol. 2004, 19, 437–454. [Google Scholar] [CrossRef]
- Machado-Duque, M.E.; Castaño-Montoya, J.P.; Medina-Morales, D.A.; Castro-Rodríguez, A.; González-Montoya, A.; Machado-Alba, J.E. Association between the use of benzodiazepines and opioids with the risk of falls and hip fractures in older adults. Int. Psychogeriatr. 2018, 30, 941–946. [Google Scholar] [CrossRef]
- Carrier, H.; Cortaredona, S.; Philipps, V.; Jacqmin-Gadda, H.; Tournier, M.; Verdoux, H.; Verger, P. Long-term risk of hip or forearm fractures in older occasional users of benzodiazepines. Br. J. Clin. Pharmacol. 2020, 86, 2155–2164. [Google Scholar] [CrossRef] [PubMed]
- Joyce, G.; Ferido, P.; Thunell, J.; Tysinger, B.; Zissimopoulos, J. Benzodiazepine use and the risk of dementia. Alzheimers Dement 2022, 8, e12309. [Google Scholar] [CrossRef] [PubMed]
- Ettcheto, M.; Olloquequi, J.; Sánchez-López, E.; Busquets, O.; Cano, A.; Manzine, P.R.; Beas-Zarate, C.; Castro-Torres, R.D.; García, M.L.; Bulló, M.; et al. Benzodiazepines and Related Drugs as a Risk Factor in Alzheimer’s Disease Dementia. Front. Aging Neurosci. 2019, 11, 344. [Google Scholar] [CrossRef] [PubMed]
- Salkeld, G.; Cameron, I.D.; Cumming, R.G.; Easter, S.; Seymour, J.; Kurrle, S.E.; Quine, S. Quality of life related to fear of falling and hip fracture in older women: A time trade off study. BMJ 2000, 320, 341–346. [Google Scholar] [CrossRef] [PubMed]
- Panneman, M.J.M.; Goettsch, W.G.; Kramarz, P.; Herings, R.M.C. The costs of benzodiazepine-associated hospital-treated fall Injuries in the EU: A Pharmo study. Drugs Aging 2003, 20, 833–839. [Google Scholar] [CrossRef] [PubMed]
- Pek, E.A.; Remfry, A.; Pendrith, C.; Fan-Lun, C.; Bhatia, R.S.; Soong, C. High Prevalence of Inappropriate Benzodiazepine and Sedative Hypnotic Prescriptions among Hospitalized Older Adults. J. Hosp. Med. 2017, 12, 310–316. [Google Scholar] [CrossRef]
- Franchi, C.; Rossio, R.; Ardoino, I.; Mannucci, P.M.; Nobili, A. Inappropriate prescription of benzodiazepines in acutely hospitalized older patients. Eur. Neuropsychopharmacol. 2019, 29, 871–879. [Google Scholar] [CrossRef]
- Verhaeghe, M.; Bracke, P.; Bruynooghe, K. Stigmatization in different mental health services: A comparison of psychiatric and general hospitals. J. Behav. Health Serv. Res. 2007, 34, 186–197. [Google Scholar] [CrossRef]
- Chee, C.Y.I.; Ng, T.P.; Kua, E.H. Comparing the stigma of mental illness in a general hospital with a state mental hospital: A Singapore study. Soc. Psychiatry Psychiatr. Epidemiol. 2005, 40, 648–653. [Google Scholar] [CrossRef]
- Schomerus, G.; Matschinger, H.; Angermeyer, M.C. Do psychiatric units at general hospitals attract less stigmatizing attitudes compared with psychiatric hospitals? Epidemiol. Psychiatr. Sci. 2013, 22, 163–168. [Google Scholar] [CrossRef]
- World Health Organization. WHO Collaborating Centre for Drug Statistics Methodology; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Rouby, F.; Pradel, V.; Frauger, E.; Pauly, V.; Natali, F.; Reggio, P.; Thirion, X.; Micallef, J. Assessment of abuse of tianeptine from a reimbursement database using ‘doctor-shopping’ as an indicator. Fundam. Clin. Pharm. 2012, 26, 286–294. [Google Scholar] [CrossRef]
- Delaš Aždajić, M.; Likić, R.; Aždajić, S.; Šitum, M.; Lovrić, I.; Štimac Grbić, D.S. Outpatient benzodiazepine utilization in Croatia: Drug use or misuse. Int. J. Clin. Pharm. 2019, 41, 1526–1535. [Google Scholar] [CrossRef]
- Sonnenberg, C.M.; Bierman, E.J.M.; Deeg, D.J.H.; Comijs, H.C.; Tilburg, W.; Beekman, A.T.F. Ten-year trends in benzodiazepine use in the Dutch population. Soc. Psychiatry Psychiatr. Epidemiol. 2012, 47, 293–301. [Google Scholar] [CrossRef]
- Petitjean, S.; Ladewig, D.; Meier, C.R.; Amrein, R.; Wiesbeck, G.A. Benzodiazepine prescribing to the Swiss adult population: Results from a national survey of community pharmacies. Int. Clin. Psychopharmacol. 2007, 22, 292–298. [Google Scholar] [CrossRef] [PubMed]
- Lagnaoui, R.; Depont, F.; Fourrier, A.; Abouelfath, A.; Bégaud, B.; Verdoux, H.; Moore, N. Patterns and correlates of benzodiazepine use in the French general population. Eur. J. Clin. Pharmacol. 2004, 60, 523–529. [Google Scholar] [CrossRef] [PubMed]
- Terauchi, M.; Hiramitsu, S.; Akiyoshi, M.; Owa, Y.; Kato, K.; Obayashi, S.; Matsushima, E.; Kubota, T. Associations between anxiety, depression and insomnia in peri- and post-menopausal women. Maturitas 2012, 72, 61–65. [Google Scholar] [CrossRef] [PubMed]
- Breslau, N.; Roth, T.; Rosenthal, L.; Andreski, P. Sleep Disturbance and Psychiatric Disorders: A Longitudinal Epedemiological Study of Young Adults. Biol. Psychiatry 1996, 39, 411–418. [Google Scholar] [CrossRef] [PubMed]
- Johnson, E.O.; Roth, T.; Breslau, N. The association of insomnia with anxiety disorders and depression: Exploration of the direction of risk. J. Psychiatr. Res. 2006, 40, 700–708. [Google Scholar] [CrossRef] [PubMed]
- Chellappa, S.L.; Aeschbach, D. Sleep and anxiety: From mechanisms to interventions. Sleep Med. Rev. 2022, 61, 101583. [Google Scholar] [CrossRef]
- Johnson, H.M. Anxiety and Hypertension: Is There a Link? A Literature Review of the Comorbidity Relationship Between Anxiety and Hypertension. Curr. Hypertens. Rep. 2019, 21, 66. [Google Scholar] [CrossRef]
- da Silva Barbosa, C.; das Merces, M.C.; Costa Santana, A.I.; de Souza E Silva, D.; Pimentel, R.F.W.; Coelho, J.M.F.; E Almeida, A.A.; Damasceno, K.S.M.; Rossi, T.R.A.; D’Oliveira Júnior, A. Anxiety and dyslipidemia among primary health care professionals: A Cross-sectional study. Work 2022, 71, 739–748. [Google Scholar] [CrossRef] [PubMed]
- van Reedt Dortland, A.; Vreeburg, S.; Giltay, E.; Licht, C.; Vogelzangs, N.; van Veen, T.; de Geus, E.; Penninx, B.; Zitman, F.J.P. The impact of stress systems and lifestyle on dyslipidemia and obesity in anxiety and depression. Psychoneuroendocrinology 2013, 38, 209–218. [Google Scholar] [CrossRef] [PubMed]
- Georgieva, I.; Lepping, P.; Bozev, V.; Lickiewicz, J.; Pekara, J.; Wikman, S.; Losevica, M.; Raveesh, B.N.; Mihai, A.; Lantta, T. Prevalence, New Incidence, Course, and Risk Factors of PTSD, Depression, Anxiety, and Panic Disorder during the Covid-19 Pandemic in 11 Countries. Healthcare 2021, 9, 664. [Google Scholar] [CrossRef]
- Martinsson, G.; Fagerberg, I.; Wiklund-Gustin, L.; Lindholm, C. Specialist prescribing of psychotropic drugs to older persons in Sweden--a register-based study of 188,024 older persons. BMC Psychiatry 2012, 12, 197. [Google Scholar] [CrossRef] [PubMed]
- Cook, J.M.; Biyanova, T.; Masci, C.; Coyne, J.C. Older patient perspectives on long-term anxiolytic benzodiazepine use and discontinuation: A qualitative study. J. Gen. Intern. Med. 2007, 22, 1094–1100. [Google Scholar] [CrossRef]
- Donoghue, J.; Lader, M. Usage of benzodiazepines: A review. Int. J. Psychiatry Clin. Pract. 2010, 14, 78–87. [Google Scholar] [CrossRef]
- Park, H.; Satoh, H.; Miki, A.; Urushihara, H.; Sawada, Y. Medications associated with falls in older people: Systematic review of publications from a recent 5-year period. Eur. J. Clin. Pharmacol. 2015, 71, 1429–1440. [Google Scholar] [CrossRef]
- Cimolai, N. Zopiclone: Is it a pharmacologic agent for abuse? Can. Fam. Physician 2007, 53, 2124–2129. [Google Scholar]
- Ng, B.J.; Couteur, D.G.L.; Hilmer, S.N. Deprescribing Benzodiazepines in Older Patients: Impact of Interventions Targeting Physicians, Pharmacists, and Patients. Drugs Aging 2018, 35, 493–521. [Google Scholar] [CrossRef]
- Brett, J.; Murnion, B. Management of benzodiazepine misuse and dependence. Aust. Prescr. 2015, 38, 152–155. [Google Scholar] [CrossRef] [PubMed]
- Neutel, C.I. The epidemiology of long-term benzodiazepine use. Int. Rev. Psychiatry 2005, 17, 189–197. [Google Scholar] [CrossRef] [PubMed]
- Johnson, C.F.; Nassr, O.A.; Harpur, C.; Kenicer, D.; Thom, A.; Akram, G. Benzodiazepine and z-hypnotic prescribing from acute psychiatric inpatient discharge to long-term care in the community. Pharm. Pract. 2018, 16, 1256. [Google Scholar] [CrossRef]
- Milani, S.A.; Raji, M.A.; Chen, L.; Kuo, Y.F. Trends in the Use of Benzodiazepines, Z-Hypnotics, and Serotonergic Drugs Among US Women and Men Before and During the COVID-19 Pandemic. JAMA Netw. Open. 2021, 4, e2131012. [Google Scholar] [CrossRef] [PubMed]
- Collaborators, C.-M.D. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet 2021, 398, 1700–1712. [Google Scholar] [CrossRef]
- Daly, M.; Robinson, E. Depression and anxiety during COVID-19. Lancet 2022, 399, 518. [Google Scholar] [CrossRef]
- Conn, D.K.; Hogan, D.B.; Amdam, L.; Cassidy, K.L.; Cordell, P.; Frank, C.; Gardner, D.; Goldhar, M.; Ho, J.M.W.; Kitamura, C.; et al. Canadian Guidelines on Benzodiazepine Receptor Agonist Use Disorder Among Older Adults Title. Can. Geriatr. J. 2020, 23, 116–122. [Google Scholar] [CrossRef]
- Markota, M.; Rummans, T.A.; Bostwick, J.M.; Lapid, M.I. Benzodiazepine Use in Older Adults: Dangers, Management, and Alternative Therapies. Mayo Clin. Proc. 2016, 91, 1632–1639. [Google Scholar] [CrossRef]
- Riemann, D.; Baglioni, C.; Bassetti, C.; Bjorvatn, B.; Dolenc Groselj, L.; Ellis, J.G.; Espie, C.A.; Garcia-Borreguero, D.; Gjerstad, M.; Gonçalves, M.; et al. European guideline for the diagnosis and treatment of insomnia. J. Sleep Res. 2017, 26, 675–700. [Google Scholar] [CrossRef]
- Khatri, D.K.; Choudhary, M.; Sood, A.; Singh, S.B. Anxiety: An ignored aspect of Parkinson’s disease lacking attention. Biomed Pharmacother 2020, 131, 110776. [Google Scholar] [CrossRef] [PubMed]
- Pontone, G.M.; Mills, K.A. Optimal Treatment of Depression and Anxiety in Parkinson’s Disease. Am. J. Geriatr. Psychiatry 2021, 29, 530–540. [Google Scholar] [CrossRef]
- Bach, J.P.; Riedel, O.; Klotsche, J.; Spottke, A.; Dodel, R.; Wittchen, H.U. Impact of complications and comorbidities on treatment costs and health-related quality of life of patients with Parkinson’s disease. J. Neurol. Sci. 2012, 314, 41–47. [Google Scholar] [CrossRef]
- Jones, J.D.; Butterfield, L.C.; Song, W.; Lafo, J.; Mangal, P.; Okun, M.S.; Bowers, D. Anxiety and Depression Are Better Correlates of Parkinson’s Disease Quality of Life Than Apathy. J. Neuropsychiatry Clin. Neurosci. 2015, 27, 213–218. [Google Scholar] [CrossRef]
- Torres-Bondia, F.; Dakterzada, F.; Galván, L.; Buti, M.; Besanson, G.; Grill, E.; Buil, R.; Batlle, J.; Piñol-Ripoll, G. Benzodiazepine and Z-Drug Use and the Risk of Developing Dementia. Int. J. Neuropsychopharmacol. 2022, 25, 261–268. [Google Scholar] [CrossRef]
- Tsunoda, K.; Uchida, H.; Suzuki, T.; Watanabe, K.; Yamashima, T.; Kashima, H. Effects of discontinuing benzodiazepine-derivative hypnotics on postural sway and cognitive functions in the elderly. Int. J. Geriatr. Psychiatry 2010, 25, 1259–1265. [Google Scholar] [CrossRef] [PubMed]
- Huang, H.C.; Tsai, C.H.; Muo, C.H.; Lin, K.H.; Lu, M.K.; Sung, F.C.; Kao, C.H. Risk of Parkinson’s disease following zolpidem use: A retrospective, population-based cohort study. J. Clin. Psychiatry 2015, 76, e104–e110. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.W.; Hsieh, T.F.; Yu, C.H.; Huang, Y.S.; Lee, C.C.; Tsai, T.H. Zolpidem and the risk of Parkinson’s disease: A nationwide population-based study. J. Psychiatr. Res. 2014, 58, 84–88. [Google Scholar] [CrossRef]
- Cosci, F.; Mansueto, G.; Faccini, M.; Casari, R.; Lugoboni, F. Socio-demographic and clinical characteristics of benzodiazepine long-term users: Results from a tertiary care center. Compr. Psychiatry 2016, 69, 211–215. [Google Scholar] [CrossRef]
| Classification | Population n (%) | Prescription n (%) |
|---|---|---|
| Sex | ||
| Men | 2895 (36.9%) | 14,803 (34.6%) |
| Women | 4941 (63.1%) | 28,039 (65.4%) |
| Age | ||
| <16 | 86 (1.1%) | 213 (0.5%) |
| 16–24 | 577 (7.4%) | 1905 (4.5%) |
| 25–44 | 2625 (33.5%) | 11,882 (27.7%) |
| 45–64 | 3144 (40.1%) | 18,768 (43.8%) |
| >64 | 1404 (17.9%) | 10,074 (23.5%) |
| Other accompanying diseases | ||
| Sleep disorders | 3611 (46.1%) | 16,404 (38.2%) |
| Depression | 870 (11.1%) | 3218 (7.5%) |
| PD | 709 (9.1%) | 445 (1.0%) |
| AD | 54 (0.7%) | 156 (0.4%) |
| Bipolar disorder | 9 (0.1%) | 45 (0.1%) |
| HTA | 321 (4.1%) | 1782 (4.2%) |
| Dyslipidemia | 129 (1.7%) | 803 (1.9%) |
| Diabetes | 78 (1.0%) | 538 (1.3%) |
| CHD | 75 (1.0%) | 220 (0.5%) |
| Tumors | 20 (0.3%) | 122 (0.3%) |
| Other | 2573 (32.8%) | 20,565 (48.0%) |
| No | 2663 (34.0%) | 18,230 (42.6%) |
| Types of BZRAs on prescription | ||
| 1 | 7530 (96.1%) | 35,647 (83.2%) |
| 2 | 806 (10.3%) | 6546 (15.3%) |
| ≥3 | 78 (1.0%) | 649 (1.5%) |
| The number of prescriptions obtained by patients during the study period | ||
| 1 | 4376 (55.9%) | 4376 (10.2%) |
| ≥2 | 3460 (44.1%) | 38,466 (89.8%) |
| Age | 2018 | 2019 | 2020 | 2021 | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Men | Women | Total | Average of Total Number of BZRA Prescriptions | Men | Women | Total | Average of Total Number of BZR Prescriptions | Men | Women | Total | Average of Total Number of BZRA Prescriptions | Men | Women | Total | Average of Total Number of BZRA Prescriptions | |
| <16 (%) | 8 (0.32) | 11 (0.25) | 19 (0.28) | 1.46 | 11 (0.28) | 31 (0.42) | 42 (0.37) | 3.50 | 15 (0.35) | 61 (0.75) | 76 (0.62) | 3.30 | 12 (0.30) | 64 (0.78) | 76 (0.62) | 1.69 |
| 16–24 (%) | 84 (3.34) | 149 (3.44) | 233 (3.40) | 3.24 | 157 (3.93) | 291 (3.94) | 448 (3.94) | 3.00 | 199 (4.70) | 287 (3.55) | 486 (3.94) | 2.98 | 271 (6.67) | 467 (5.68) | 738 (6.00) | 2.19 |
| 25–44 (%) | 758 (30.16) | 1173 (27.07) | 1931 (28.21) | 4.44 | 1251 (31.35) | 1920 (25.97) | 3171 (27.85) | 4.93 | 1272 (30.03) | 2080 (25.73) | 3352 (27.21) | 4.73 | 1175 (28.92) | 2253 (27.39) | 3428 (27.89) | 3.37 |
| 45–64 (%) | 998 (39.71) | 2088 (48.19) | 3086 (45.08) | 5.00 | 1507 (37.76) | 3410 (46.12) | 4917 (43.19) | 5.59 | 1650 (38.95) | 3916 (48.44) | 5566 (45.17) | 5.74 | 1519 (37.39) | 3680 (44.73) | 5199 (42.30) | 3.94 |
| ≥65 (%) | 665 (26.46) | 912 (21.05) | 1577 (23.04) | 5.40 | 1065 (26.69) | 1742 (23.56) | 2807 (24.66) | 6.78 | 1100 (25.97) | 1741 (21.53) | 2841 (23.06) | 6.41 | 1086 (26.73) | 1763 (21.43) | 2849 (23.18) | 4.12 |
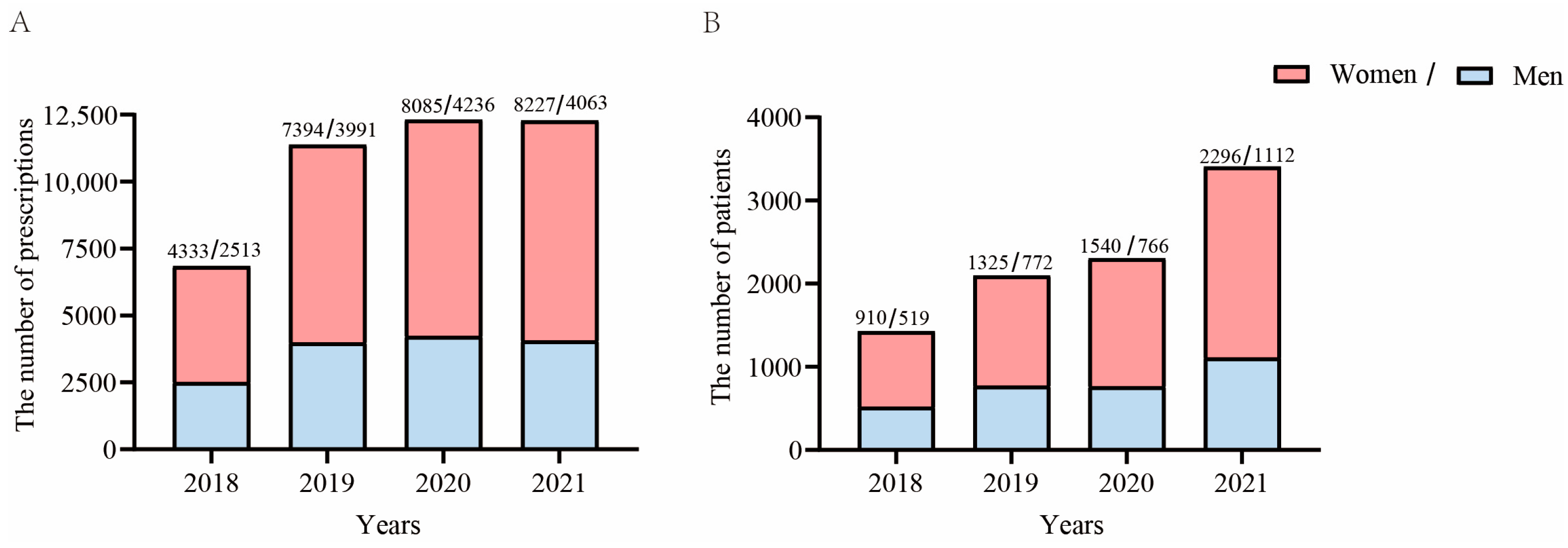
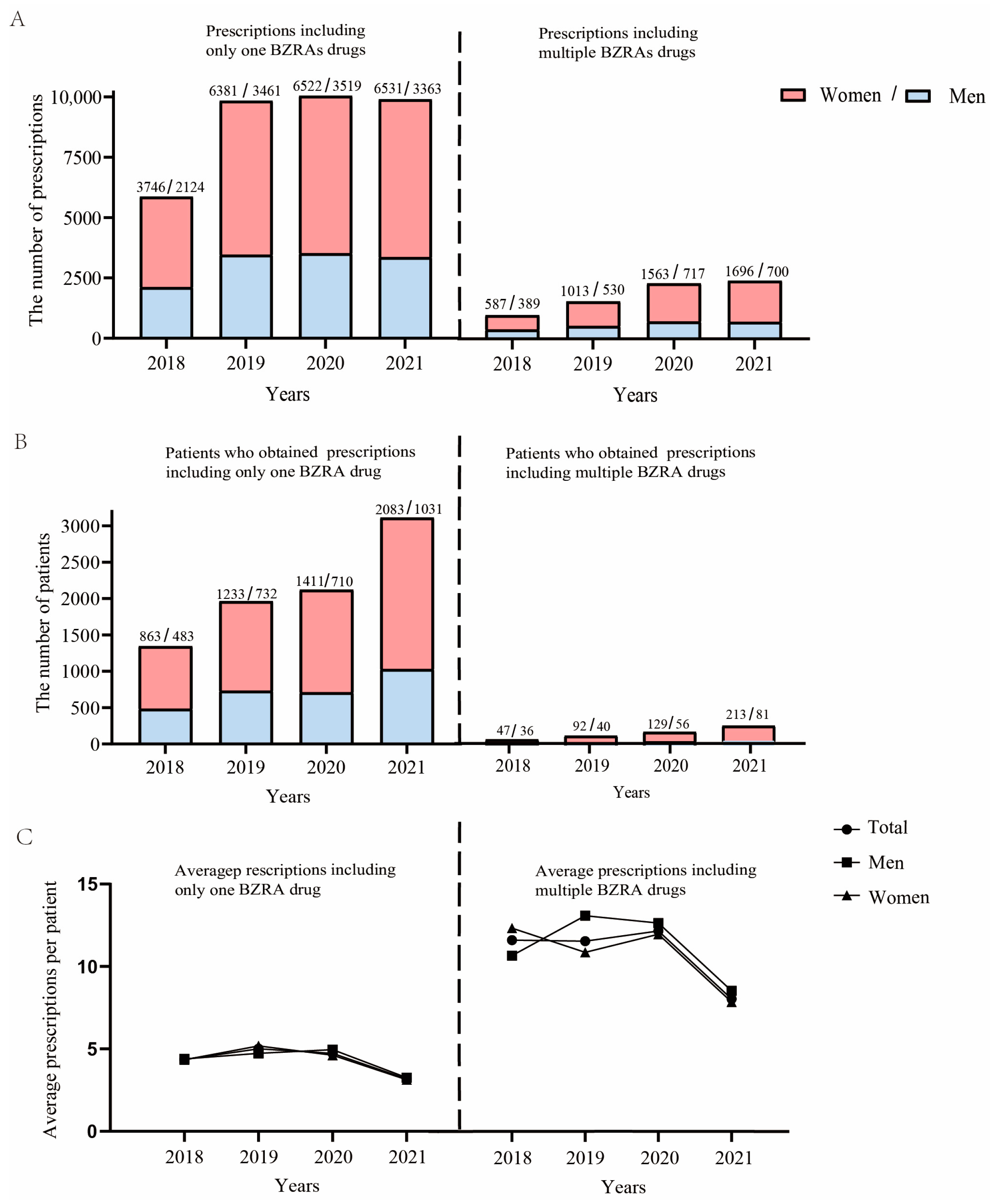
| Total number of BZRAs Prescriptions % | 2513 36.71 | 4333 63.29 | 6846 | 4.79 | 3991 35.05 | 7394 64.95 | 11,385 | 5.43 | 4236 34.38 | 8085 65.62 | 12,321 | 5.34 | 4063 33.06 | 8227 66.94 | 12,290 | 3.61 |
| Average of prescriptions by sex | 4.84 | 4.76 | 5.17 | 5.58 | 5.53 | 5.25 | 3.65 | 3.58 |
| Sex | ||||||
|---|---|---|---|---|---|---|
| Anxiety | Male | Female | Statistics | |||
| ATC Code | BZRAs | N | Total% | N (%) | N (%) | p |
| BZDs | ||||||
| N03AE01 | Clonazepam | 1702 | 10.87 | 670 (12.10) | 1032 (10.20) | <0.001 |
| N05BA01 | Diazepam | 104 | 0.66 | 43 (0.78) | 61 (0.60) | 0.239 |
| N05BA06 | Lorazepam | 6009 | 38.38 | 2218 (40.06) | 3791 (37.46) | 0.001 |
| N05BA12 | Alprazolam | 1315 | 8.40 | 458 (8.27) | 857 (8.47) | 0.695 |
| N05CD04 | Estazolam | 1898 | 12.12 | 633 (11.43) | 1265 (12.50) | 0.054 |
| Z-drugs | ||||||
| N05CF01 | Zopiclone | 1400 | 8.94 | 540 (9.75) | 860 (8.50) | 0.009 |
| N05CF02 | Zolpidem | 3230 | 20.63 | 975 (17.61) | 2255 (22.28) | <0.001 |
| <16 | 16–24 | 24–44 | 45–64 | >64 | Total | |
|---|---|---|---|---|---|---|
| Men | ||||||
| Prescriptions | 43 | 654 | 3956 | 4684 | 3130 | 12,467 |
| Individuals | 23 | 214 | 943 | 956 | 581 | 2717 |
| Average prescription | 1.87 | 3.06 | 4.20 | 4.90 | 5.38 | 4.59 |
| Women | ||||||
| Prescriptions | 164 | 1104 | 6347 | 10,536 | 5029 | 23,180 |
| Individuals | 61 | 338 | 1529 | 1894 | 710 | 4532 |
| Average prescription | 2.69 | 3.27 | 4.15 | 5.56 | 7.08 | 5.11 |
| All | ||||||
| Prescriptions | 207 | 1758 | 10,303 | 15,220 | 8159 | 35,647 |
| Individuals | 84 | 552 | 2472 | 2850 | 1291 | 7249 |
| Average prescription | 2.46 | 3.18 | 4.17 | 5.34 | 6.32 | 4.92 |
| <16 | 16–24 | 24–44 | 45–64 | >64 | Total | |
|---|---|---|---|---|---|---|
| Men | ||||||
| Prescriptions | 3 | 57 | 500 | 990 | 786 | 2336 |
| Individuals | 1 | 10 | 51 | 79 | 37 | 178 |
| Average prescription | 3.0 | 5.7 | 9.8 | 12.53 | 21.2 | 13.1 |
| Women | ||||||
| Prescriptions | 3 | 90 | 1079 | 2558 | 1129 | 4859 |
| Individuals | 1 | 15 | 102 | 215 | 76 | 409 |
| Average prescription | 3.0 | 6.0 | 10.6 | 11.9 | 14.9 | 11.9 |
| All | ||||||
| Prescriptions | 6 | 147 | 1579 | 3548 | 1915 | 7195 |
| Individuals | 2 | 25 | 153 | 294 | 113 | 587 |
| Average prescription | 3.0 | 5.9 | 10.3 | 12.1 | 17.0 | 12.3 |
| Univariate Analysis | Multivariate Analysis | |||
|---|---|---|---|---|
| Variables | OR (95% CI) | p Value | OR (95 %CI) | p Value |
| Age | 1.016 (1.014–1.017) | <0.001 | 1.018 (1.016–1.019) | <0.001 |
| Men | 0.894 (0.847–0.943) | <0.001 | 0.882 (0.835–0.932) | <0.001 |
| Insomnia | 0.612 (0.581–0.644) | <0.001 | 0.617 (0.586–0.649) | <0.001 |
| Depression | 0.676 (0.620–0.738) | 0.004 | 0.614 (0.562–0.672) | <0.001 |
| PD | 22.519 (8.412–60.286) | <0.001 | 27.161 (10.134–72.796) | <0.001 |
| AD | 10.334 (3.295–32.406) | <0.001 | 15.414 (4.893–48.556) | <0.001 |
| Bipolar disorder | 1.312 (0.556–3.101) | 0.536 | —— | —— |
| HTA | 0.709 (0.632–0.796) | <0.001 | 0.783 (0.693–0.885) | <0.001 |
| Dyslipidemia | 2.071 (1.624–2.642) | <0.001 | 2.566 (2.002–3.289) | <0.001 |
| Diabetes | 0.558 (0.460–0.677) | <0.001 | 0.638 (0.521–0.780) | <0.001 |
| CHD | 1.067 (0.743–1.533) | 0.725 | —— | —— |
| Tumors | 1.383 (0.263–0.557) | <0.001 | 0.445 (0.303–0.652) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, D.; Zhang, Q.; Zhao, Z.; Chen, M.; Hou, Y.; Wang, G.; Shen, H.; Zhu, H.; Ji, Y.; Ruan, L.; et al. Benzodiazepine-Receptor Agonist Utilization in Outpatients with Anxiety Disorder: A Retrospective Study Based on Electronic Healthcare Data from a Large General Tertiary Hospital. Healthcare 2023, 11, 554. https://doi.org/10.3390/healthcare11040554
Liu D, Zhang Q, Zhao Z, Chen M, Hou Y, Wang G, Shen H, Zhu H, Ji Y, Ruan L, et al. Benzodiazepine-Receptor Agonist Utilization in Outpatients with Anxiety Disorder: A Retrospective Study Based on Electronic Healthcare Data from a Large General Tertiary Hospital. Healthcare. 2023; 11(4):554. https://doi.org/10.3390/healthcare11040554
Chicago/Turabian StyleLiu, Denong, Qingyu Zhang, Zhijia Zhao, Mengjia Chen, Yanbin Hou, Guanjun Wang, Haowei Shen, Huaqiang Zhu, Yunxin Ji, Liemin Ruan, and et al. 2023. "Benzodiazepine-Receptor Agonist Utilization in Outpatients with Anxiety Disorder: A Retrospective Study Based on Electronic Healthcare Data from a Large General Tertiary Hospital" Healthcare 11, no. 4: 554. https://doi.org/10.3390/healthcare11040554
APA StyleLiu, D., Zhang, Q., Zhao, Z., Chen, M., Hou, Y., Wang, G., Shen, H., Zhu, H., Ji, Y., Ruan, L., & Lou, Z. (2023). Benzodiazepine-Receptor Agonist Utilization in Outpatients with Anxiety Disorder: A Retrospective Study Based on Electronic Healthcare Data from a Large General Tertiary Hospital. Healthcare, 11(4), 554. https://doi.org/10.3390/healthcare11040554






