Behavioral and Metabolic Risk Factors for Noncommunicable Diseases among Population in the Republic of Srpska (Bosnia and Herzegovina)
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Data
2.2. Statistical Analysis
3. Results
- Gender and alcohol consumption;
- Age and hypertension, cholesterol and diabetes;
- Education level and hypertension;
- Employment and hypertension, cholesterol and diabetes.
3.1. Gender and Risk Factors
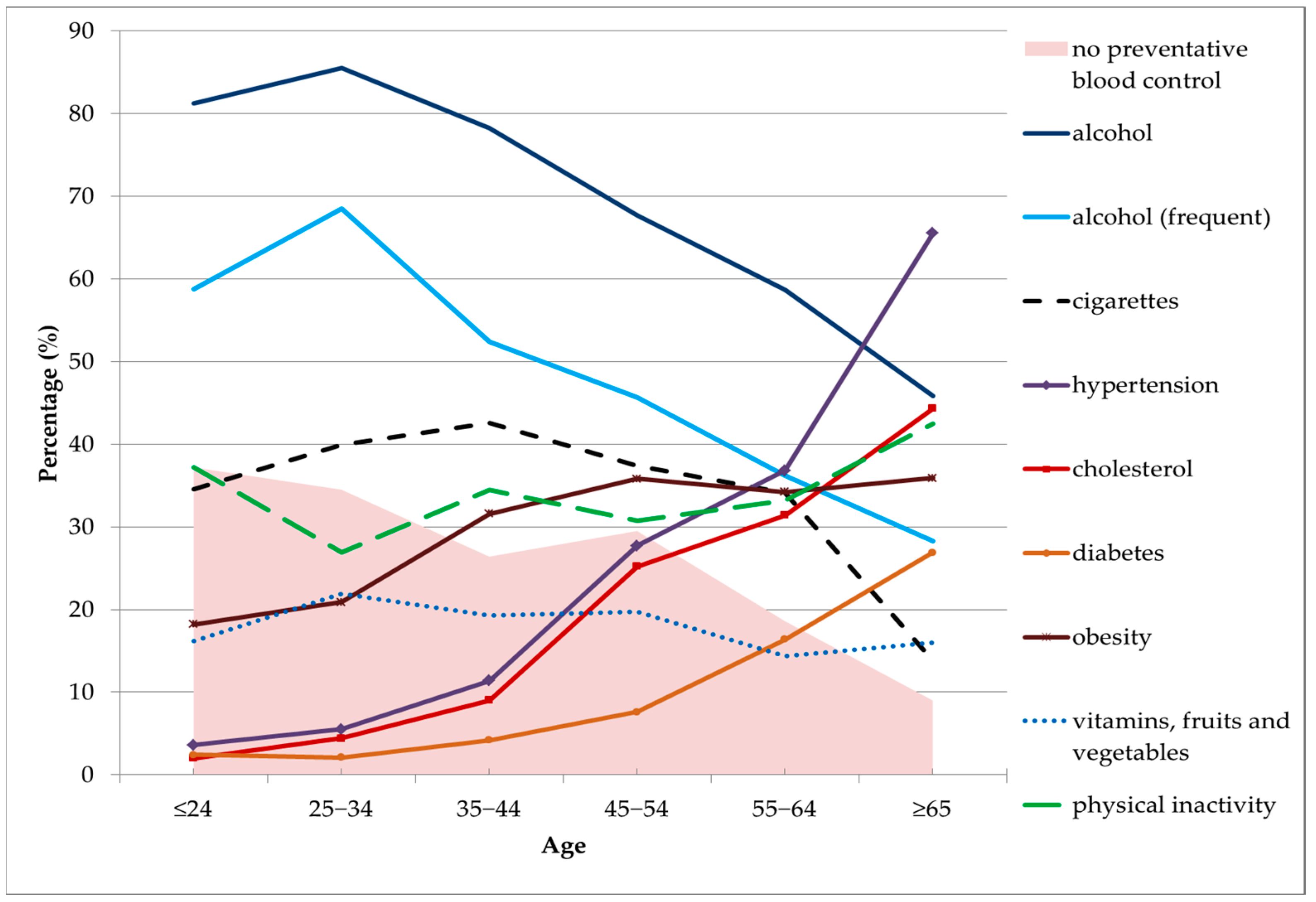
3.2. Age and Risk Factors
3.3. Type of Settlement and Risk Factors
3.4. Education and Risk Factors
3.5. Working Status of Population and Risk Factors
3.6. Income and Risk Factors
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Licher, S.; Heshmatollah, A.; Van Der Willik, K.D.; Stricker, B.H.C.; Ruiter, R.; De Roos, E.W.; LaHousse, L.; Koudstaal, P.J.; Hofman, A.; Fani, L.; et al. Lifetime risk and multimorbidity of non-communicable diseases and disease-free life expectancy in the general population: A population-based cohort study. PLoS Med. 2019, 16, e1002741. [Google Scholar] [CrossRef] [PubMed]
- Coates, M.M.; Kintu, A.; Gupta, N.; Wroe, E.B.; Adler, A.J.; Kwan, G.F.; Park, P.H.; Rajbhandari, R.; Byrne, A.L.; Casey, D.C.; et al. Burden of non-communicable diseases from infectious causes in 2017: A modelling study. Lancet Glob. Health 2020, 8, e1489–e1498. [Google Scholar] [CrossRef]
- Allen, L.; Williams, J.; Townsend, N.; Mikkelsen, B.; Roberts, N.; Foster, C.; Wickramasinghe, K. Socioeconomic status and non-communicable disease behavioural risk factors in low-income and lower-middle-income countries: A systematic review. Lancet Glob. Health 2017, 5, e277–e289. [Google Scholar] [CrossRef]
- World Health Organization. Noncommunicable Diseases Progress Monitor 2022. Available online: https://www.who.int/publications-detail-redirect/9789240047761 (accessed on 11 April 2022).
- Kumar, S.; Pillai, R.R.; Dwarakamai, V.; Reddy, N.S.; Joseph, N. Study on surveillance of risk factors for noncommunicable diseases in local population. Med. J. Dr. D.Y. Patil Vidyapeeth 2019, 12, 387. [Google Scholar] [CrossRef]
- GBD 2015 Risk Factors Collaborators. Global, Regional, and National Comparative Risk Assessment of 79 Behavioural, Environmental and Occupational, and Metabolic Risks or Clusters of Risks, 1990–2015: A Systematic Analysis for the Global Burden of Disease Study 2015. Lancet 2016, 388, 1659–1724. Available online: https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(16)31679-8/fulltext (accessed on 18 August 2022). [CrossRef]
- Budreviciute, A.; Damiati, S.; Sabir, D.K.; Onder, K.; Schuller-Goetzburg, P.; Plakys, G.; Katileviciute, A.; Khoja, S.; Kodzius, R. Management and Prevention Strategies for Non-communicable Diseases (NCDs) and Their Risk Factors. Front. Public Health 2020, 8, 574111. [Google Scholar] [CrossRef]
- Bigna, J.J.; Noubiap, J.J. The rising burden of non-communicable diseases in sub-Saharan Africa. Lancet Glob. Health 2019, 7, e1295–e1296. [Google Scholar] [CrossRef]
- Ezzati, M.; Lopez, A.D.; Rodgers, A.; Van der Hoorn, S.; Murray, C.J.L.; Comparative Risk Assessment Collaborating Group. Selected major risk factors and global and regional burden of disease. Lancet 2002, 360, 1347–1360. [Google Scholar] [CrossRef]
- Di Cesare, M.; Khang, Y.-H.; Asaria, P.; Blakely, T.; Cowan, M.J.; Farzadfar, F.; Guerrero, R.; Ikeda, N.; Kyobutungi, C.; Msyamboza, K.P.; et al. Inequalities in non-communicable diseases and effective responses. Lancet 2013, 381, 585–597. [Google Scholar] [CrossRef] [PubMed]
- Wolf-Maier, K.; Cooper, R.S.; Banegas, J.R.; Giampaoli, S.; Hense, H.-W.; Joffres, M.; Kastarinen, M.; Poulter, N.; Primatesta, P.; Rodríguez-Artalejo, F.; et al. Hypertension Prevalence and Blood Pressure Levels in 6 European Countries, Canada, and the United States. JAMA 2003, 289, 2363–2369. [Google Scholar] [CrossRef]
- Grotto, I.; Huerta, M.; Sharabi, Y. Hypertension and socioeconomic status. Curr. Opin. Cardiol. 2008, 23, 335–339. [Google Scholar] [CrossRef] [PubMed]
- Leng, B.; Jin, Y.; Li, G.; Chen, L.; Jin, N. Socioeconomic status and hypertension. J. Hypertens. 2015, 33, 221–229. [Google Scholar] [CrossRef] [PubMed]
- Radevic, S.; Radovanovic, S.; Djonovic, N.; Simic-Vukomanovic, I.; Mihailovic, N.; Janicijevic, K.; Kocic, S. Socioeconomic inequalities and non-communicable diseases in Serbia: National health survey. Vojn. Pregl. 2018, 75, 926–934. [Google Scholar] [CrossRef]
- Leung, A.; Bushnik, T.; Hennessy, D.; McAlister, F.; Manuel, D.G. Risk factors for hypertension in Canada. Public Health Rep. (1896-1970) 2019, 30, 3–13. [Google Scholar]
- Mills, K.T.; Stefanescu, A.; He, J. The global epidemiology of hypertension. Nat. Rev. Nephrol. 2020, 16, 223–237. [Google Scholar] [CrossRef] [PubMed]
- Walekhwa, S.; Kisa, A. Tobacco Use and Risk Factors for Hypertensive Individuals in Kenya. Healthcare 2021, 9, 591. [Google Scholar] [CrossRef] [PubMed]
- Benetou, V.; Chloptsios, Y.; Zavitsanos, X.; Karalis, D.; Naska, A.; Trichopoulou, A. Total cholesterol and HDL-cholesterol in relation to socioeconomic status in a sample of 11,645 Greek adults: The EPIC study in Greece. Scand. J. Public Health 2000, 28, 260–265. [Google Scholar] [CrossRef] [PubMed]
- Capewell, S.; Ford, E.S. Why have total cholesterol levels declined in most developed countries? BMC Public Health 2011, 11, 641. [Google Scholar] [CrossRef]
- Farzadfar, F.; Finucane, M.M.; Danaei, G.; Pelizzari, P.M.; Cowan, M.J.; Paciorek, C.J.; Singh, G.M.; Lin, J.K.; Stevens, G.A.; Riley, L.M.; et al. National, regional, and global trends in serum total cholesterol since 1980: Systematic analysis of health examination surveys and epidemiological studies with 321 country-years and 3·0 million participants. Lancet 2011, 377, 578–586. [Google Scholar] [CrossRef] [PubMed]
- Mattiuzzi, C.; Sanchis-Gomar, F.; Lippi, G. Worldwide burden of LDL cholesterol: Implications in cardiovascular disease. Nutr. Metab. Cardiovasc. Dis. 2020, 30, 241–244. [Google Scholar] [CrossRef]
- McNamara, C.L.; Balaj, M.; Thomson, K.H.; Eikemo, T.A.; Solheim, E.F.; Bambra, C. The socioeconomic distribution of non-communicable diseases in Europe: Findings from the European Social Survey (2014) special module on the social determinants of health. Eur. J. Public Health 2017, 27, 22–26. [Google Scholar] [CrossRef] [PubMed]
- Kalkhoran, S.; Benowitz, N.L.; Rigotti, N.A. Prevention and Treatment of Tobacco Use. J. Am. Coll. Cardiol. 2018, 72, 1030–1045. [Google Scholar] [CrossRef] [PubMed]
- Machado, E.; Parajára, M.D.C.; Guedes, L.F.F.; Meireles, A.L.; de Menezes, M.C.; Felisbino-Mendes, M.S.; Verly-Junior, E.; Malta, D.C. Burden of non-communicable diseases attributable to dietary risks in Brazil, 1990-2019: An analysis of the Global Burden of Disease Study 2019. Rev. Soc. Bras. Med. Trop. 2022, 55, e0282-2021. [Google Scholar] [CrossRef]
- Rehm, J.; Gmel, G.E., Sr.; Gmel, G.; Hasan, O.S.M.; Imtiaz, S.; Popova, S.; Probst, C.; Roerecke, M.; Room, R.; Samokhvalov, A.V.; et al. The relationship between different dimensions of alcohol use and the burden of disease—An update. Addiction 2017, 112, 968–1001. [Google Scholar] [CrossRef] [PubMed]
- Horvat, P.; Stefler, D.; Murphy, M.; King, L.; McKee, M.; Bobak, M. Alcohol, pattern of drinking and all-cause mortality in Russia, Belarus and Hungary: A retrospective indirect cohort study based on mortality of relatives. Addiction 2018, 113, 1252–1263. [Google Scholar] [CrossRef] [PubMed]
- Pedroni, C.; Dujeu, M.; Lebacq, T.; Desnouck, V.; Holmberg, E.; Castetbon, K. Alcohol consumption in early adolescence: Associations with sociodemographic and psychosocial factors according to gender. PLoS ONE 2021, 16, e0245597. [Google Scholar] [CrossRef] [PubMed]
- Wilson, T.; Temple, N.J. Alcohol consumption and health. In Nutrition Guide for Physicians and Related Healthcare Professions; Wilson, T., Temple, N.J., Bray, G.A., Eds.; Nutrition and Health; Springer International Publishing: Cham, Switzerland, 2022; pp. 337–344. [Google Scholar] [CrossRef]
- Lacombe, J.; Armstrong, M.E.G.; Wright, F.L.; Foster, C. The impact of physical activity and an additional behavioural risk factor on cardiovascular disease, cancer and all-cause mortality: A systematic review. BMC Public Health 2019, 19, 900. [Google Scholar] [CrossRef] [PubMed]
- Krawcyk, R.S.; Vinther, A.; Petersen, N.C.; Faber, J.; Iversen, H.K.; Christensen, T.; Lambertsen, K.L.; Rehman, S.; Klausen, T.W.; Rostrup, E.; et al. Effect of Home-Based High-Intensity Interval Training in Patients With Lacunar Stroke: A Randomized Controlled Trial. Front. Neurol. 2019, 10, 664. [Google Scholar] [CrossRef]
- Katzmarzyk, P.T.; Friedenreich, C.; Shiroma, E.J.; Lee, I.-M. Physical inactivity and non-communicable disease burden in low-income, middle-income and high-income countries. Br. J. Sports Med. 2021, 56, 101–106. [Google Scholar] [CrossRef]
- Ciumărnean, L.; Milaciu, M.V.; Negrean, V.; Orășan, O.H.; Vesa, S.C.; Sălăgean, O.; Iluţ, S.; Vlaicu, S.I. Cardiovascular Risk Factors and Physical Activity for the Prevention of Cardiovascular Diseases in the Elderly. Int. J. Environ. Res. Public Health 2021, 19, 207. [Google Scholar] [CrossRef]
- Bazzano, L.A.; Serdula, M.K.; Liu, S. Dietary intake of fruits and vegetables and risk of cardiovascular disease. Curr. Atheroscler. Rep. 2003, 5, 492–499. [Google Scholar] [CrossRef] [PubMed]
- Woodside, J.V.; Young, I.; McKinley, M.C. Fruits and vegetables: Measuring intake and encouraging increased consumption. Proc. Nutr. Soc. 2013, 72, 236–245. [Google Scholar] [CrossRef]
- Alissa, E.M.; Ferns, G.A. Dietary Fruits and Vegetables and Cardiovascular Diseases Risk. Crit. Rev. Food Sci. Nutr. 2017, 57, 1950–1962. [Google Scholar] [CrossRef] [PubMed]
- Nyberg, S.T.; Batty, G.D.; Pentti, J.; Virtanen, M.; Alfredsson, L.; Fransson, E.I.; Goldberg, M.; Heikkilä, K.; Jokela, M.; Knutsson, A.; et al. Obesity and loss of disease-free years owing to major non-communicable diseases: A multicohort study. Lancet Public Health 2018, 3, e490–e497. [Google Scholar] [CrossRef] [PubMed]
- Heath, L.; Jebb, S.A.; Aveyard, P.; Piernas, C. Obesity, metabolic risk and adherence to healthy lifestyle behaviours: Prospective cohort study in the UK Biobank. BMC Med. 2022, 20, 65. [Google Scholar] [CrossRef] [PubMed]
- Peng, W.; Li, K.; Yan, A.F.; Shi, Z.; Zhang, J.; Cheskin, L.J.; Hussain, A.; Wang, Y. Prevalence, Management, and Associated Factors of Obesity, Hypertension, and Diabetes in Tibetan Population Compared with China Overall. Int. J. Environ. Res. Public Health 2022, 19, 8787. [Google Scholar] [CrossRef] [PubMed]
- Robbins, J.M.; Vaccarino, V.; Zhang, H.; Kasl, S.V. Socioeconomic status and diagnosed diabetes incidence. Diabetes Res. Clin. Pr. 2005, 68, 230–236. [Google Scholar] [CrossRef] [PubMed]
- Saydah, S.; Lochner, K. Socioeconomic Status and Risk of Diabetes-Related Mortality in the U.S. Public Health Rep. 2010, 125, 377–388. [Google Scholar] [CrossRef] [PubMed]
- Saeedi, P.; Petersohn, I.; Salpea, P.; Malanda, B.; Karuranga, S.; Unwin, N.; Colagiuri, S.; Guariguata, L.; Motala, A.A.; Ogurtsova, K.; et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res. Clin. Pract. 2019, 157, 107843. [Google Scholar] [CrossRef]
- Rawshani, A.; Rawshani, A.; Rawshani, A.; Franzén, S.; Sattar, N.; Eliasson, B.; Svensson, A.-M.; Zethelius, B.; Miftaraj, M.; McGuire, D.K.; et al. Risk Factors, Mortality, and Cardiovascular Outcomes in Patients with Type 2 Diabetes. N. Engl. J. Med. 2018, 379, 633–644. [Google Scholar] [CrossRef]
- Milani, S.A.; Lopez, D.S.; Downer, B.; Samper-Ternent, R.; Wong, R. Effects of diabetes and obesity on cognitive impairment and mortality in older mexicans. Arch. Gerontol. Geriatr. 2021, 99, 104581. [Google Scholar] [CrossRef] [PubMed]
- Divajeva, D.; Marsh, T.; Logstrup, S.; Kestens, M.; Vemer, P.; Kriaucioniene, V.; Peresson, S.; O’Kelly, S.; Rito, A.; Webber, L. Economics of chronic diseases protocol: Cost-effectiveness modelling and the future burden of non-communicable disease in Europe. BMC Public Health 2014, 14, 456. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Noncommunicable Diseases. 2022. Available online: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases (accessed on 14 October 2022).
- Mackenbach, J.P.; Stirbu, I.; Roskam, A.-J.R.; Schaap, M.M.; Menvielle, G.; Leinsalu, M.; Kunst, A.E. Socioeconomic Inequalities in Health in 22 European Countries. N. Engl. J. Med. 2008, 358, 2468–2481. [Google Scholar] [CrossRef] [PubMed]
- Head, J.; Chungkham, H.S.; Hyde, M.; Zaninotto, P.; Alexanderson, K.; Stenholm, S.; Salo, P.; Kivimaki, M.; Goldberg, M.; Zins, M.; et al. Socioeconomic differences in healthy and disease-free life expectancy between ages 50 and 75: A multi-cohort study. Eur. J. Public Health 2018, 29, 267–272. [Google Scholar] [CrossRef]
- Zaninotto, P.; Batty, G.D.; Stenholm, S.; Kawachi, I.; Hyde, M.; Goldberg, M.; Westerlund, H.; Vahtera, J.; Head, J. Socioeconomic Inequalities in Disability-free Life Expectancy in Older People from England and the United States: A Cross-national Population-Based Study. J. Gerontol. Ser. A 2020, 75, 906–913. [Google Scholar] [CrossRef] [PubMed]
- Mäki, N.; Martikainen, P.; Eikemo, T.; Menvielle, G.; Lundberg, O.; Östergren, O.; Jasilionis, D.; Mackenbach, J.P. Educational differences in disability-free life expectancy: A comparative study of long-standing activity limitation in eight European countries. Soc. Sci. Med. 2013, 94, 1–8. [Google Scholar] [CrossRef]
- Gillman, M.W. Primordial Prevention of Cardiovascular Disease. Circulation 2015, 131, 599–601. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Noncommunicable Diseases Country Profiles 2018; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- NCD Risk Factor Collaboration (NCD-RisC). Worldwide Trends in Blood Pressure from 1975 to 2015: A Pooled Analysis of 1479 Population-Based Measurement Studies with 19·1 Million Participants. Lancet 2017, 389, 37–55. Available online: https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(16)31919-5/fulltext (accessed on 21 August 2022). [CrossRef] [PubMed]
- Statistical Yearbook 2020. Available online: https://www.rzs.rs.ba/front/article/4582/?left_mi=None&add=None (accessed on 18 June 2022).
- European Health Interview Survey (EHIS wave 3)—Methodological Manual. Available online: https://ec.europa.eu/eurostat/web/products-manuals-and-guidelines/-/KS-02-18-240 (accessed on 18 June 2022).
- World Health Organization. Global Status Report on Noncommunicable Diseases 2014; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- Bush, K.; Kivlahan, D.R.; McDonell, M.B.; Fihn, S.D.; Bradley, K.A. The AUDIT Alcohol Consumption Questions (AUDIT-C). An Effective Brief Screening Test for Problem Drinking. Arch. Intern. Med. 1998, 158, 1789–1795. [Google Scholar] [CrossRef] [PubMed]
- Pandas-dev/pandas: Pandas. Available online: https://zenodo.org/record/7344967#.Y-FkUj3MIdU (accessed on 11 November 2022).
- Seabold, S.; Perktold, J. Statsmodels: Econometric and Statistical Modeling with Python. In Proceedings of the 9th Python in Science Conference, Austin, TX, USA, 28 June–3 July 2010; pp. 92–96. [Google Scholar] [CrossRef]
- Pedregosa, F.; Varoquaux, G.; Gramfort, A.; Michel, V.; Thirion, B.; Grisel, O.; Blondel, M.; Prettenhofer, P.; Weiss, R.; Dubourg, V.; et al. Scikit-Learn: Machine Learning in Python. J. Mach. Learn. Res. 2011, 12, 2825–2830. [Google Scholar]
- de Vos, N. Nicodv/Kmodes. 2022. Available online: https://github.com/nicodv/kmodes (accessed on 12 November 2022).
- Hunter, J.D. Matplotlib: A 2D graphics environment. Comput. Sci. Eng. 2007, 9, 90–95. [Google Scholar] [CrossRef]
- Waskom, M.L. Seaborn: Statistical data visualization. J. Open Source Softw. 2021, 6, 3021. [Google Scholar] [CrossRef]
- Cao, F.; Liang, J.; Bai, L. A new initialization method for categorical data clustering. Expert Syst. Appl. 2009, 36, 10223–10228. [Google Scholar] [CrossRef]
- 18.4% of EU Population Smoked Daily in 2019. Available online: https://ec.europa.eu/eurostat/web/products-eurostat-news/-/edn-20211112-1 (accessed on 17 August 2022).
- Siahpush, M. Socioeconomic status and tobacco expenditure among Australian households: Results from the 1998-99 Household Expenditure Survey. J. Epidemiol. Community Health 2003, 57, 798–801. [Google Scholar] [CrossRef]
- Kaleta, D.; Makowiec-Dąbrowska, T.; Dziankowska-Zaborszczyk, E.; Fronczak, A. Prevalence and socio-demographic correlates of daily cigarette smoking in Poland: Results from the Global Adult Tobacco Survey (2009–2010). Int. J. Occup. Med. Environ. Health 2012, 25, 126–136. [Google Scholar] [CrossRef]
- Nagelhout, G.E.; Boer, D.D.K.-D.; Kunst, A.E.; Van Der Meer, R.M.; De Vries, H.; Van Gelder, B.M.; Willemsen, M.C. Trends in socioeconomic inequalities in smoking prevalence, consumption, initiation, and cessation between 2001 and 2008 in the Netherlands. Findings from a national population survey. BMC Public Health 2012, 12, 303. [Google Scholar] [CrossRef]
- Singh, A.; Ladusingh, L. Prevalence and Determinants of Tobacco Use in India: Evidence from Recent Global Adult Tobacco Survey Data. PLoS ONE 2014, 9, e114073. [Google Scholar] [CrossRef]
- Islami, F.; Stoklosa, M.; Drope, J.; Jemal, A. Global and Regional Patterns of Tobacco Smoking and Tobacco Control Policies. Eur. Urol. Focus 2015, 1, 3–16. [Google Scholar] [CrossRef]
- Alcohol. Available online: https://www.who.int/news-room/fact-sheets/detail/alcohol (accessed on 21 August 2022).
- Mravčík, V.; Chomynová, P.; Nechanská, B.; Černíková, T.; Csémy, L. Alcohol use and its consequences in the Czech Republic. Central Eur. J. Public Health 2019, 27, S15–S28. [Google Scholar] [CrossRef]
- Lourdes, T.G.R.; Hamid, H.A.A.; Riyadzi, M.R.; Hasani, W.S.R.; Mutalip, M.H.A.; Jabbar, N.A.; Rifin, H.M.; Saminathan, T.A.; Ismail, H.; Yusoff, M.F.M. Findings from a Nationwide Study on Alcohol Consumption Patterns in an Upper Middle-Income Country. Int. J. Environ. Res. Public Health 2022, 19, 8851. [Google Scholar] [CrossRef]
- Cooper, M.L.; Frone, M.R.; Russell, M.; Peirce, R.S. Gender, stress, coping, and alcohol use. In Gender and Alcohol: Individual and Social Perspectives; Rutgers Center of Alcohol Studies: Piscataway, NJ, USA, 1997; pp. 199–224. [Google Scholar]
- Wilsnack, R.W.; Vogeltanz, N.D.; Wilsnack, S.C.; Harris, T.R.; Ahlström, S.; Bondy, S.; Csémy, L.; Ferrence, R.; Ferris, J.; Fleming, J.; et al. Gender differences in alcohol consumption and adverse drinking consequences: Cross-cultural patterns. Addiction 2000, 95, 251–265. [Google Scholar] [CrossRef] [PubMed]
- Molgaard, C.A.; Nakamura, C.M.; Stanford, E.P.; Peddecord, K.M.; Morton, D.J. Prevalence of alcohol consumption among older persons. J. Community Health 1990, 15, 239–251. [Google Scholar] [CrossRef] [PubMed]
- Nikitara, K.; Odani, S.; Demenagas, N.; Rachiotis, G.; Symvoulakis, E.; Vardavas, C. Prevalence and correlates of physical inactivity in adults across 28 European countries. Eur. J. Public Health 2021, 31, 840–845. [Google Scholar] [CrossRef]
- Drygas, W.; Kwaśniewska, M.; Kaleta, D.; Pikala, M.; Bielecki, W.; Głuszek, J.; Zdrojewski, T.; Pająk, A.; Kozakiewicz, K.; Broda, G. Epidemiology of physical inactivity in Poland: Prevalence and determinants in a former communist country in socioeconomic transition. Public Health 2009, 123, 592–597. [Google Scholar] [CrossRef] [PubMed]
- Milošević, M.; Golubić, R.; Mustajbegović, J.; Doko Jelinić, J.; Janev Holcer, N.; Kern, J. Regional Pattrn of Physical Inactivity in Croatia. Coll. Antropol. 2009, 33, 35–38. [Google Scholar] [PubMed]
- Kruger, J.; Ham, S.A.; Kohl, H.W. Trends in Leisure-Time Physical Inactivity by Age, Sex, and Race/Ethnicity—United States, 1994–2004. Morb. Mortal. Wkly. Rep. 2005, 54, 991–994. [Google Scholar]
- Guthold, R.; Ono, T.; Strong, K.L.; Chatterji, S.; Morabia, A. Worldwide Variability in Physical Inactivity: A 51-Country Survey. Am. J. Prev. Med. 2008, 34, 486–494. [Google Scholar] [CrossRef] [PubMed]
- Giskes, K.; Turrell, G.; Patterson, C.; Newman, B. Socioeconomic differences among Australian adults in consumption of fruit and vegetables and intakes of vitamins A, C and folate. J. Hum. Nutr. Diet. 2002, 15, 375–385. [Google Scholar] [CrossRef]
- Wardle, J.; Haase, A.M.; Steptoe, A.; Nillapun, M.; Jonwutiwes, K.; Bellisie, F. Gender Differences in Food Choice: The Con-tribution of Health Beliefs and Dieting. Ann. Behav. Med. 2004, 27, 107. [Google Scholar] [CrossRef]
- World Health Organization; Regional Office for Europe. WHO European Regional Obesity: Report 2022; World Health Organization: Geneva, Switzerland, 2022. [Google Scholar]
- World Health Organization. Obesity and Overweight. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 18 October 2022).
- Marija, S.; Dragan, V.; Svetlana, R.; Nela, D. Socioeconomic Inequalities in Overweight and Obesity in Serbia: Data from 2013 National Health Survey. Front. Pharmacol. 2018, 8, 967. [Google Scholar] [CrossRef]
- Zatońska, K.; Psikus, P.; Basiak-Rasała, A.; Stępnicka, Z.; Gaweł-Dąbrowska, D.; Wołyniec, M.; Gibka, J.; Szuba, A.; Połtyn-Zaradna, K. Obesity and Chosen Non-Communicable Diseases in PURE Poland Cohort Study. Int. J. Environ. Res. Public Health 2021, 18, 2701. [Google Scholar] [CrossRef] [PubMed]
- 22% of People in the EU Have High Blood Pressure. Available online: https://ec.europa.eu/eurostat/web/products-eurostat-news/-/edn-20210929-1 (accessed on 17 August 2022).
- Li, Y.-C.; Wang, L.-M.; Jiang, Y.; Li, X.-Y.; Zhang, M.; Hu, N. [Prevalence of hypertension among Chinese adults in 2010]. Zhonghua Yu Fang Yi Xue Za Zhi 2012, 46, 409–413. [Google Scholar] [PubMed]
- Ninios, I.; Ninios, V.; Lazaridou, F.; Dimitriadis, K.; Kerasidou, O.; Louridas, G. Gender-Specific Differences in Hypertension Prevalence, Treatment, Control, and Associated Conditions among the Elderly: Data from a Greek Population. Clin. Exp. Hypertens. 2008, 30, 327–337. [Google Scholar] [CrossRef] [PubMed]
- Diabetes: Key Facts—World Health Organization. Available online: http://www.who.int/news-room/fact-sheets/detail/diabetes (accessed on 15 October 2018).
- Chronic Diabetes Affects Millions of People in the EU. Available online: https://ec.europa.eu/eurostat/web/products-eurostat-news/-/edn-20171113-1 (accessed on 20 August 2022).
- Wild, S.; Roglic, G.; Green, A.; Sicree, R.; King, H. Global Prevalence of Diabetes. Diabetes Care 2004, 27, 1047–1053. [Google Scholar] [CrossRef] [PubMed]
- Carlsson, A.C.; Wändell, P.; Hedlund, E.; Walldius, G.; Nordqvist, T.; Jungner, I.; Hammar, N. Country of birth-specific and gender differences in prevalence of diabetes in Sweden. Diabetes Res. Clin. Pract. 2013, 100, 404–408. [Google Scholar] [CrossRef] [PubMed]
- Gardete-Correia, L.; Boavida, J.; Raposo, J.; Mesquita, A.C.; Fona, C.; Carvalho, R.; Cardoso, S. First diabetes prevalence study in Portugal: PREVADIAB study. Diabet. Med. 2010, 27, 879–881. [Google Scholar] [CrossRef] [PubMed]
- Alnakhi, W.K.; Mamdouh, H.; Hussain, H.Y.; Ibrahim, G.M.; Ahmad, A.S.; Ali, R.; Abdulle, A. The Socio-Demographic Characteristics Associated with Non-Communicable Diseases among the Adult Population of Dubai: Results from Dubai Household Survey 2019. Healthcare 2021, 9, 1139. [Google Scholar] [CrossRef] [PubMed]
- Ongosi, A.; Wilunda, C.; Musumari, P.; Techasrivichien, T.; Wang, C.-W.; Ono-Kihara, M.; Serrem, C.; Kihara, M.; Nakayama, T. Prevalence and Risk Factors of Elevated Blood Pressure and Elevated Blood Glucose among Residents of Kajiado County, Kenya: A Population-Based Cross-Sectional Survey. Int. J. Environ. Res. Public Health 2020, 17, 6957. [Google Scholar] [CrossRef]
| Variables | Type | Men | Women | Total | |||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Gender | 1062 | 46.0 | 1249 | 54.0 | 2311 | 100 | |
| Age | ≤24 year | 228 | 21.5 | 388 | 31.1 | 616 | 26.7 |
| 25–34 year | 271 | 25.5 | 253 | 20.3 | 524 | 22.7 | |
| 35–44 year | 223 | 21.0 | 232 | 18.6 | 455 | 19.7 | |
| 45–54 year | 168 | 15.8 | 161 | 12.9 | 329 | 14.2 | |
| 55–64 year | 97 | 9.1 | 123 | 9.8 | 220 | 9.5 | |
| 65+ | 75 | 7.1 | 92 | 7.4 | 167 | 7.2 | |
| Type of settlement | Rural | 164 | 15.5 | 202 | 16.2 | 366 | 15.8 |
| Suburban | 195 | 18.4 | 264 | 21.1 | 459 | 19.9 | |
| Urban | 702 | 66.2 | 783 | 62.7 | 1485 | 64.3 | |
| Education level | Primary | 44 | 4.1 | 74 | 5.9 | 118 | 5.1 |
| Secondary | 638 | 60.1 | 693 | 55.5 | 1331 | 57.6 | |
| High | 380 | 35.8 | 481 | 38.5 | 861 | 37.3 | |
| Working status | Employed | 655 | 61.7 | 630 | 50.5 | 1285 | 55.7 |
| Unemployed | 156 | 14.7 | 182 | 14.6 | 338 | 14.6 | |
| Students | 157 | 14.8 | 327 | 26.2 | 484 | 21.0 | |
| Pensioners | 94 | 8.9 | 108 | 8.7 | 202 | 8.7 | |
| Income | Low | 154 | 14.5 | 134 | 10.8 | 288 | 12.5 |
| Middle | 525 | 49.5 | 644 | 51.8 | 1169 | 50.7 | |
| High | 381 | 35.9 | 466 | 37.5 | 847 | 36.8 | |
| Variables | Answer | Men | Woman | Total | |||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Smoking and Tobacco Use | Daily smoker | 319 | 48.9 | 333 | 51.1 | 652 | 28.8 |
| Non-daily smoker | 71 | 38.4 | 114 | 61.6 | 185 | 8.0 | |
| Never/ex-smoker | 672 | 63.3 | 802 | 64.2 | 1474 | 63.8 | |
| Alcohol consumption | Yes | 898 | 84.6 | 836 | 66.9 | 577 | 75.0 |
| No | 164 | 15.4 | 413 | 33.1 | 1734 | 25.0 | |
| Frequent alcohol | Yes | 727 | 68.5 | 507 | 40.8 | 1234 | 53.5 |
| consumption | No | 334 | 31.5 | 737 | 59.2 | 1071 | 46.5 |
| Blood pressure level (≥140/90 mmHg) | Yes | 193 | 18.2 | 193 | 15.5 | 386 | 16.7 |
| No | 681 | 64.1 | 887 | 71.0 | 1568 | 67.8 | |
| I do not know | 188 | 17.7 | 169 | 13.5 | 357 | 15.4 | |
| Cholesterol level (≥5.0 mmol/L) | Yes | 136 | 12.8 | 166 | 13.3 | 302 | 13.1 |
| No | 658 | 62.0 | 817 | 65.4 | 1475 | 63.9 | |
| I do not know | 268 | 25.2 | 265 | 21.2 | 533 | 23.1 | |
| Blood sugar level (≥7.0 mmol/L) | Yes | 77 | 7.3 | 74 | 5.9 | 151 | 6.5 |
| No | 811 | 76.4 | 1011 | 80.9 | 1822 | 78.8 | |
| I do not know | 174 | 16.4 | 164 | 13.1 | 338 | 14.6 | |
| Overweight and obesity | BMI < 25.0 | 506 | 46.2 | 647 | 53.6 | 1153 | 50.1 |
| BMI 25.0–29.9 | 408 | 37.3 | 388 | 32.2 | 796 | 34.6 | |
| BMI ≥ 30.0 | 181 | 16.5 | 171 | 14.2 | 352 | 15.3 | |
| Physical activity (>150 min/week) | Yes | 774 | 72.9 | 765 | 61.2 | 1539 | 66.6 |
| No | 288 | 27.1 | 484 | 38.8 | 772 | 33.4 | |
| Intake of vitamins, fruits and vegetables | Low | 253 | 24.0 | 170 | 13.7 | 423 | 18.4 |
| Middle | 422 | 40.0 | 470 | 37.8 | 892 | 38.9 | |
| High | 379 | 36.0 | 602 | 48.5 | 981 | 42.7 | |
| Health control (per year) | By no means | 383 | 36.1 | 300 | 24.0 | 683 | 29.6 |
| Once | 443 | 41.8 | 616 | 49.4 | 1059 | 45.9 | |
| Twice | 129 | 12.2 | 185 | 14.8 | 314 | 13.6 | |
| Repeatedly | 105 | 9.9 | 147 | 11.8 | 252 | 10.9 | |
| Variables | Test | Gender | Age | Type of Settlement | Education Level | Working Status | Income |
|---|---|---|---|---|---|---|---|
| Smoking and Tobacco Use | χ2 | 0.217 | 170.970 * | 10.953 | 15.464 | 42.902 | 10.516 |
| p | 0.641 | <0.001 | 0.004 | <0.001 | <0.001 | 0.005 | |
| Alcohol consumption | χ2 | 95.162 | 524.182 * | 28.817 | 79.321 | 110.020 | 16.472 |
| p | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | |
| Frequent alcohol | χ2 | 177.454 | 95.066 * | 42.460 | 42.878 | 61.897 | 1.710 |
| consumption | p | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | 0.425 |
| Blood pressure level | χ2 | 13.029 | 482.641 ** | 12.626 | 180.250 | 393.122 | 50.258 |
| p | 0.001 | <0.001 | 0.013 | <0.001 | <0.001 | <0.001 | |
| Cholesterol level | χ2 | 5.194 | 333.214 ** | 2.275 | 65.610 | 209.685 | 40.996 |
| p | 0.075 | <0.001 | 0.685 | <0.001 | <0.001 | <0.001 | |
| Blood sugar level | χ2 | 7.225 | 157.654 ** | 1.638 | 55.778 | 136.777 | 29.522 |
| p | 0.027 | <0.001 | 0.802 | <0.001 | <0.001 | <0.001 | |
| Overweight and obesity | χ2 | 9.972 | 58.026 | 0.294 | 6.883 | 46.422 | 6.000 |
| p | 0.007 | <0.001 | 0.990 | 0.142 | <0.001 | 0.199 | |
| Physical inactivity | χ2 | 34.991 | 244.699 * | 5.654 | 16.753 | 10.642 | 4.363 |
| p | <0.001 | <0.001 | 0.059 | <0.001 | 0.014 | 0.113 | |
| Intake of vitam., fruits and veget. | χ2 | 54.533 | 0.18 | 5.933 | 19.886 | 27.022 | 107.594 |
| p | <0.001 | 0.894 | 0.204 | <0.001 | <0.001 | <0.001 | |
| Health control | χ2 | 40.289 | 141.606 | 15.225 | 132.584 | 243.840 | 29.905 |
| p | <0.001 | <0.001 | 0.019 | <0.001 | <0.001 | <0.001 |
| Variables | Test | Gender | Age | Type of Settlement | Education Level | Working Status | Income |
|---|---|---|---|---|---|---|---|
| Male/ Female | 18–44/45+ | Urban/ Suburb and Rural | Tertiary/ Primary and Secondary | Employment/Unemployment | High and Middle/Low | ||
| Smoking and Tobacco Use | OR | 1.041 | 1.409 | 1.324 | 0.811 | 1.204 | 0.696 |
| 95% CI | 0.878–1.234 | 1.168–1.701 | 1.106–1.585 | 0.679–0.968 | 0.939–1.542 | 0.542–0.894 | |
| Alcohol consumption | OR | 2.705 | 2.980 | 1.622 | 1.300 | 1.709 | 1.704 |
| 95% CI | 2.206–3.317 | 2.449–3.627 | 1.338–1.967 | 1.066–1.586 | 1.311–2.228 | 1.309–2.219 | |
| Frequent alcohol consumption | OR | 3.164 | 2.383 | 1.721 | 1.204 | 1.298 | 1.171 |
| 95% CI | 2.664–3.758 | 1.989–2.856 | 1.449–2.044 | 1.016–1.427 | 1.021–1.651 | 0.914–1.499 | |
| Blood pressure level | OR | 1.302 | 0.114 | 0.732 | 0.597 | 0.839 | 0.553 |
| 95% CI | 1.042–1.628 | 0.088–0.146 | 0.583–0.920 | 0.470–0.759 | 0.600–1.174 | 0.413–0.742 | |
| Cholesterol level | OR | 1.017 | 0.114 | 0.882 | 0.981 | 1.217 | 0.532 |
| 95% CI | 0.793–1.305 | 0.086–0.152 | 0.682–1.140 | 0.761–1.264 | 0.821–1.805 | 0.388–0.730 | |
| Blood sugar level | OR | 1.297 | 0.175 | 0.945 | 0.657 | 0.926 | 0.480 |
| 95% CI | 0.931–1.808 | 0.122–0.252 | 0.669–1.335 | 0.458–0.943 | 0.548–1.565 | 0.320–0.722 | |
| Overw. and obesity (BMI ≥ 25/<25) | OR | 1.3473 | 0.544 | 0.996 | 0.938 | 0.909 | 0.678 |
| 95% CI | 1.143–1.588 | 0.448–0.659 | 0.822–1.207 | 0.775–1.136 | 0.700–1.181 | 0.520–0.883 | |
| Physical inactivity | OR | 0.588 | 0.949 | 0.879 | 0.714 | 0.960 | 0.763 |
| 95% CI | 0.493–0.702 | 0.787–1.143 | 0.735–1.052 | 0.595–0.857 | 0.743–1.241 | 0.592–0.984 | |
| Vitam., frui. and veg. (Low/mid. and high) | OR | 1.992 | 1.128 | 0.893 | 0.630 | 0.688 | 0.370 |
| 95% CI | 1.607–2.469 | 0.894–1.423 | 0.718–1.111 | 0.500–0.793 | 0.518–0.914 | 0.282–0.486 | |
| Health control | OR | 0.560 | 0.546 | 1.197 | 1.729 | 1.628 | 1.761 |
| 95% CI | 0.468–0.671 | 0.444–0.672 | 0.995–1.440 | 1.425–2.098 | 1.268–2.090 | 1.366–2.272 |
| Grouping | Variables | Accuracy Score | Gender | Age | Type of Settlement | Education Level | Working Status | Income |
|---|---|---|---|---|---|---|---|---|
| All ages | Smoking and Tobacco Use (bin) | 64.85% | 0.879 | 1.141 | 1.271 | 1.676 * | 1.592 ** | 1.187 |
| Alcohol consumption (bin) | 77.40% | 0.333 | 0.715 | 0.709 | 1.310 * | 0.926 ** | 1.097 | |
| Physical inactivity (bin) | 66.06% | 1.554 * | 1.023 | 1.016 | 0.678 | 1.017 ** | 0.993 | |
| Blood pressure level (bin) | 85.27% | 1.191 ** | 0.464 | 0.909 | 1.573 * | 1.003 | 1.182 | |
| Cholesterol level (bin) | 86.73% | 1.025 | 0.467 | 1.002 | 0.957 | 1.075 ** | 1.225 * | |
| Blood sugar level (bin) | 93.59% | 1.295 * | 0.539 | 1.067 | 1.210 ** | 0.951 | 1.136 | |
| Overweight and obesity (bin) | 73.11% | 0.782 | 1.278 * | 1.076 ** | 0.917 | 0.852 | 0.828 | |
| Vitamins, fruits and veg. (bin) | 81.49% | 0.527 | 0.910 ** | 0.983 * | 0.622 | 0.780 | 0.526 | |
| Health control (bin) | 70.67% | 0.595 | 0.733 | 1.029 * | 0.675 | 0.841 ** | 0.693 | |
| <35 age | Smoking and Tobacco Use (bin) | 63.44% | 1.015 | 1.192 | 1.438 | 1.558 * | 1.467 ** | 1.321 |
| Alcohol consumption (bin) | 83.22% | 0.715 | 0.994 | 0.798 | 1.119 * | 0.855 | 1.108 ** | |
| Physical inactivity (bin) | 67.64% | 2.262 * | 0.730 | 1.047 ** | 0.601 | 0.858 | 0.874 | |
| Blood pressure level (bin) | 95.42% | 1.190 | 0.836 | 0.893 | 1.966 * | 1.652 ** | 1.403 | |
| Cholesterol level (bin) | 96.82% | 1.078 * | 0.523 | 0.928 ** | 0.798 | 0.865 | 0.662 | |
| Blood sugar level (bin) | 97.81% | 0.557 | 0.882 | 1.338 ** | 1.622 * | 0.979 | 1.154 | |
| Overweight and obesity (bin) | 80.47% | 0.732 | 0.917 ** | 1.028 * | 0.744 | 0.747 | 0.829 | |
| Vitamins, fruits and veg. (bin) | 80.81% | 0.617 | 0.978 * | 0.876 ** | 0.684 | 0.766 | 0.699 | |
| Health control (bin) | 64.14% | 0.475 | 0.820 | 1.169 * | 0.819 | 0.942 ** | 0.893 | |
| 35≤ age <55 | Smoking and Tobacco Use (bin) | 58.69% | 0.831 | 1.186 | 1.092 | 1.664 * | 1.328 ** | 1.217 |
| Alcohol consumption (bin) | 75.8% | 0.208 | 0.655 | 0.755 | 1.435 ** | 0.826 | 0.909 ** | |
| Physical inactivity (bin) | 67.18% | 1.297 * | 0.675 | 1.011 | 0.765 | 0.850 | 1.032 ** | |
| Blood pressure level (bin) | 81.77% | 1.496 * | 0.436 | 0.824 | 1.131 ** | 0.888 | 1.063 | |
| Cholesterol level (bin) | 84.26% | 1.313 * | 0.334 | 0.811 | 0.833 | 1.176 ** | 1.164 | |
| Blood sugar level (bin) | 94.42% | 1.405 ** | 0.596 | 1.094 | 1.954 * | 1.178 | 0.889 | |
| Overweight and obesity (bin) | 66.14% | 0.736 | 1.143 ** | 0.881 | 0.903 | 1.171 * | 1.101 | |
| Vitamins, fruits and veg. (bin) | 80.26% | 0.682 | 0.913 | 0.970 ** | 0.699 | 1.148 * | 0.597 | |
| Health control (bin) | 71.91% | 0.715 | 1.076 * | 1.009 ** | 0.557 | 0.902 | 0.609 | |
| ≥55 age | Smoking and Tobacco Use (bin) | 75.21% | 1.166 | 2.803 * | 1.103 | 1.345 | 1.158 | 1.706 ** |
| Alcohol consumption (bin) | 66.94% | 0.174 | 0.950 | 0.827 | 1.183 ** | 0.885 | 1.579 * | |
| Physical inactivity (bin) | 61.63% | 1.025 ** | 1.002 | 0.938 | 0.810 | 1.095 * | 0.995 | |
| Blood pressure level (bin) | 63.37% | 0.770 | 0.467 | 0.856 | 1.659 * | 0.889 | 1.053 ** | |
| Cholesterol level (bin) | 61.90% | 0.642 | 0.924 | 1.046 ** | 0.877 | 0.874 | 1.333 * | |
| Blood sugar level (bin) | 79.07% | 0.853 | 0.724 | 1.261 * | 0.887 | 1.015 ** | 0.569 | |
| Overweight and obesity (bin) | 63.72% | 0.782 | 1.278 * | 1.076 ** | 0.917 | 0.852 | 0.828 | |
| Vitamins, fruits and veg. (bin) | 84.17% | 0.264 | 1.230 * | 1.096 ** | 0.388 | 0.707 | 0.277 | |
| Health control (bin) | 85.16% | 0.501 | 0.503 | 0.599 | 0.735 ** | 0.841 * | 0.609 |
| Grouping | Variables | Accuracy Score | Gender | Age | Type of Settlement | Education Level | Working Status | Income |
|---|---|---|---|---|---|---|---|---|
| All ages | Blood pressure level | 70.04% | 0.859 | 1.717 * | 1.187 ** | 0.847 | 0.924 | 1.029 |
| Cholesterol level | 63.92% | 1.040 | 1.744 * | 1.119 | 1.171 ** | 0.917 | 1.018 | |
| Blood sugar level | 78.75% | 0.911 | 1.505 * | 0.987 | 0.978 | 1.106 ** | 0.947 | |
| <35 age | Blood pressure level | 74.79% | 0.772 | 1.062 * | 1.008 ** | 0.619 | 0.689 | 0.917 |
| Cholesterol level | 69.34% | 1.039 | 1.896 * | 1.067 ** | 1.048 | 0.975 | 0.921 | |
| Blood sugar level | 81.14% | 1.187 * | 0.749 | 0.987 ** | 0.697 | 0.911 | 0.975 | |
| 35≤ age <55 | Blood pressure level | 69.01% | 0.916 | 1.667 * | 1.291 ** | 0.908 | 0.966 | 1.017 |
| Cholesterol level | 63.92% | 0.859 | 2.168 * | 1.157 | 1.164 ** | 0.937 | 0.934 | |
| Blood sugar level | 79.89% | 0.876 | 1.419 * | 1.018 ** | 0.892 | 0.971 | 0.965 | |
| ≥55 age | Blood pressure level | 57.5% | 1.194 | 1.811 * | 1.096 | 1.080 | 1.264 ** | 1.247 |
| Cholesterol level | 49.48% | 1.572 * | 1.372 ** | 1.121 | 1.082 | 1.017 | 0.938 | |
| Blood sugar level | 69.91% | 0.740 | 1.409 * | 1.109 ** | 0.866 | 1.047 | 0.744 |
| Grouping | Variables | Gender | Age | Type of Settlement | Education Level | Working Status | Income |
|---|---|---|---|---|---|---|---|
| All ages | Overweight and obesity | 0.806 | 1.248 * | 1.007 | 0.824 | 0.841 | 0.837 |
| Vitamins, fruits and veg. | 1.689 | 1.040 | 0.953 | 1.405 * | 1.237 | 1.804 | |
| Health control | 1.528 | 1.374 * | 0.974 | 1.108 | 1.296 | 1.387 | |
| <35 age | Overweight and obesity | 0.769 | 0.947 ** | 1.051 * | 0.727 | 0.743 | 0.872 |
| Vitamins, fruits and veg. | 1.606 * | 1.025 | 0.978 | 1.518 ** | 1.353 | 1.487 | |
| Health control | 1.804 * | 0.967 | 0.874 | 1.259 ** | 1.036 | 1.214 | |
| 35≤ age <55 | Overweight and obesity | 0.752 | 1.210 * | 0.868 | 0.948 | 1.190 ** | 1.023 |
| Vitamins, fruits and veg. | 1.807 ** | 1.261 | 0.925 | 1.209 | 1.036 | 1.985 * | |
| Health control | 1.431 ** | 1.205 | 0.933 | 1.294 | 1.185 | 1.530 * | |
| ≥55 age | Overweight and obesity | 1.034 ** | 0.911 | 1.120 * | 0.857 | 0.947 | 0.574 |
| Vitamins, fruits and veg. | 1.596 ** | 1.476 | 0.896 | 1.541 | 1.111 | 2.586 * | |
| Health control | 1.160 | 2.486 * | 1.317 | 0.775 | 1.200 | 1.716 ** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Majić, A.; Arsenović, D.; Čvokić, D.D. Behavioral and Metabolic Risk Factors for Noncommunicable Diseases among Population in the Republic of Srpska (Bosnia and Herzegovina). Healthcare 2023, 11, 483. https://doi.org/10.3390/healthcare11040483
Majić A, Arsenović D, Čvokić DD. Behavioral and Metabolic Risk Factors for Noncommunicable Diseases among Population in the Republic of Srpska (Bosnia and Herzegovina). Healthcare. 2023; 11(4):483. https://doi.org/10.3390/healthcare11040483
Chicago/Turabian StyleMajić, Aleksandar, Daniela Arsenović, and Dimitrije D. Čvokić. 2023. "Behavioral and Metabolic Risk Factors for Noncommunicable Diseases among Population in the Republic of Srpska (Bosnia and Herzegovina)" Healthcare 11, no. 4: 483. https://doi.org/10.3390/healthcare11040483
APA StyleMajić, A., Arsenović, D., & Čvokić, D. D. (2023). Behavioral and Metabolic Risk Factors for Noncommunicable Diseases among Population in the Republic of Srpska (Bosnia and Herzegovina). Healthcare, 11(4), 483. https://doi.org/10.3390/healthcare11040483





