Is a Maximal Strength-Training Program Effective on Physical Fitness, Injury Incidence, and Injury Burden in Semi-Professional Soccer Players? A Randomized Controlled Trial
Abstract
:1. Introduction
2. Materials and Methods
2.1. Experimental Design
2.2. Participants
2.3. Procedures
2.4. Intervention Program
2.5. Perceived Exertion Load (RPEL)
2.6. Wellbeing State
2.7. Physical Fitness Attributes
2.7.1. Vertical Jump Performance
2.7.2. Change in Direction Ability (CODA)
2.7.3. Linear Test Sprints
2.7.4. Repeated Sprint Ability (RSA 5 × 30 m)
2.7.5. Isometric Strength
2.8. Injuries
2.9. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bangsbo, J.; Mohr, M.; Krustrup, P. Physical and Metabolic Demands of Training and Match-Play in the Elite Football Player. J. Sports Sci. 2006, 24, 665–674. [Google Scholar] [CrossRef] [PubMed]
- Ekstrand, J.; Hägglund, M.; Waldén, M. Injury Incidence and Injury Patterns in Professional Football: The UEFA Injury Study. Br. J. Sports Med. 2011, 45, 553–558. [Google Scholar] [CrossRef]
- López-Valenciano, A.; Ruiz-Pérez, I.; Garcia-Gómez, A.; Vera-Garcia, F.J.; De Ste Croix, M.; Myer, G.D.; Ayala, F. Epidemiology of Injuries in Professional Football: A Systematic Review and Meta-Analysis. Br. J. Sports Med. 2020, 54, 711–718. [Google Scholar] [CrossRef] [PubMed]
- Bahr, R.; Clarsen, B.; Ekstrand, J. Why We Should Focus on the Burden of Injuries and Illnesses, Not Just Their Incidence. Br. J. Sports Med. 2018, 52, 1018–1021. [Google Scholar] [CrossRef] [PubMed]
- Gouttebarge, V.; Aoki, H.; Ekstrand, J.; Verhagen, E.A.; Kerkhoffs, G.M. Are Severe Musculoskeletal Injuries Associated with Symptoms of Common Mental Disorders among Male European Professional Footballers? Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 3934–3942. [Google Scholar] [CrossRef] [PubMed]
- Gebert, A.; Gerber, M.; Pühse, U.; Gassmann, P.; Stamm, H.; Lamprecht, M. Costs Resulting from Nonprofessional Soccer Injuries in Switzerland: A Detailed Analysis. J. Sport Health Sci. 2020, 9, 240–247. [Google Scholar] [CrossRef] [PubMed]
- Ekstrand, J. Keeping Your Top Players on the Pitch: The Key to Football Medicine at a Professional Level. Br. J. Sports Med. 2013, 47, 723–724. [Google Scholar] [CrossRef]
- Hägglund, M.; Waldén, M.; Magnusson, H.; Kristenson, K.; Bengtsson, H.; Ekstrand, J. Injuries Affect Team Performance Negatively in Professional Football: An 11-Year Follow-up of the UEFA Champions League Injury Study. Br. J. Sports Med. 2013, 47, 738–742. [Google Scholar] [CrossRef]
- Nilstad, A.; Andersen, T.E.; Bahr, R.; Holme, I.; Steffen, K. Risk Factors for Lower Extremity Injuries in Elite Female Soccer Players. Am. J. Sports Med. 2014, 42, 940–948. [Google Scholar] [CrossRef]
- Silvers-Granelli, H.J.; Bizzini, M.; Arundale, A.; Mandelbaum, B.R.; Snyder-Mackler, L. Does the FIFA 11+ Injury Prevention Program Reduce the Incidence of ACL Injury in Male Soccer Players? Clin. Orthop. Relat. Res. 2017, 475, 2447–2455. [Google Scholar] [CrossRef]
- Hägglund, M.; Waldén, M.; Ekstrand, J. Injury Incidence and Distribution in Elite Football—A Prospective Study of the Danish and the Swedish Top Divisions. Scand. J. Med. Sci. Sports 2005, 15, 21–28. [Google Scholar] [CrossRef] [PubMed]
- Mallo, J.; González, P.; Veiga, S.; Navarro, E. Injury Incidence in a Spanish Sub-Elite Professional Football Team: A Prospective Study during Four Consecutive Seasons. J. Sports Sci. Med. 2011, 10, 731–736. [Google Scholar] [PubMed]
- Noya-Salces, J.; Gómez-Carmona, P.M.; Gracia-Marco, L.; Moliner-Urdiales, D.; Sillero-Quintana, M. Epidemiology of Injuries in First Division Spanish Football. J. Sports Sci. 2014, 32, 1263–1270. [Google Scholar] [CrossRef] [PubMed]
- Bowen, L.; Gross, A.S.; Gimpel, M.; Li, F.X. Accumulated Workloads and the Acute: Chronic Workload Ratio Relate to Injury Risk in Elite Youth Football Players. Br. J. Sports Med. 2017, 51, 452–459. [Google Scholar] [CrossRef]
- Baldjian, A.; Mohrenberger, H.; Ciladi, M. Epidemiology of Injuries in a Professional Soccer Team in Argentina: A 2-Year Retrospective Observational. Arg. Jour Resp. Phys. Ther. 2022, 4, 23–31. [Google Scholar] [CrossRef]
- Owoeye, O.B.A.; Aiyegbusi, A.I.; Fapojuwo, O.A.; Badru, O.A.; Babalola, A.R. Injuries in Male and Female Semi-Professional Football (Soccer) Players in Nigeria: Prospective Study of a National Tournament. BMC Res. Notes 2017, 10, 133. [Google Scholar] [CrossRef]
- Croisier, J.L.; Ganteaume, S.; Binet, J.; Genty, M.; Ferret, J.M. Strength Imbalances and Prevention of Hamstring Injury in Professional Soccer Players: A Prospective Study. Am. J. Sports Med. 2008, 36, 1469–1475. [Google Scholar] [CrossRef]
- Hewett, T.E.; Lindenfeld, T.N.; Riccobene, J.V.; Noyes, F.R. The Effect of Neuromuscular Training on the Incidence of Knee Injury in Female Athletes: A Prospective Study. Am. J. Sports Med. 1999, 27, 699–706. [Google Scholar] [CrossRef]
- Impellizzeri, F.M.; McCall, A.; Ward, P.; Bornn, L.; Coutts, A.J. Training Load and Its Role in Injury Prevention, Part 2: Conceptual and Methodologic Pitfalls. J. Athl. Train. 2020, 55, 893–901. [Google Scholar] [CrossRef]
- Raya-González, J.; Torres-Martin, L.; Beato, M.; Rodríguez-Fernández, A.; Sanchez-Sanchez, J. The Effects of Training Based on Nordic Hamstring and Sprint Exercises on Measures of Physical Fitness and Hamstring Injury Prevention in U19 Male Soccer Players. Res. Sports Med. 2023, 31, 588–603. [Google Scholar] [CrossRef]
- Timmins, R.G.; Bourne, M.N.; Shield, A.J.; Williams, M.D.; Lorenzen, C.; Opar, D.A. Short Biceps Femoris Fascicles and Eccentric Knee Flexor Weakness Increase the Risk of Hamstring Injury in Elite Football (Soccer): A Prospective Cohort Study. Br. J. Sports Med. 2016, 50, 1524–1535. [Google Scholar] [CrossRef] [PubMed]
- Verstappen, S.; Van Rijn, R.M.; Cost, R.; Stubbe, J.H. The Association Between Training Load and Injury Risk in Elite Youth Soccer Players: A Systematic Review and Best Evidence Synthesis. Sports Med. Open 2021, 7, 6. [Google Scholar] [CrossRef] [PubMed]
- De Hoyo, M.; Pozzo, M.; Sañudo, B.; Carrasco, L.; Gonzalo-Skok, O.; Domínguez-Cobo, S.; Morán-Camacho, E. Effects of a 10-Week in-Season Eccentric-Overload Training Program on Muscle-Injury Prevention and Performance in Junior Elite Soccer Players. Int. J. Sports Physiol. Perform. 2015, 10, 46–52. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Sánchez, J.; Torres Martín, L.; Ramirez-Campillo, R.; Castillo, D.; Raya-González, J. The Effects of Jump Training on Measures of Physical Performance, Lower Extremities Injury Incidence and Burden in Highly Trained Male Soccer Players. Res. Sports Med. 2022, 26, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Thacker, S.B.; Stroup, F.; Branche, C.M.; Gilchrist, J. Prevention of Knee Injuries in Sports: A Systemic Review of the Literature. J. Sports Med. Phys. Fit. 2003, 43, 165–179. [Google Scholar]
- Franettovich-Smith, M.M.; Bonacci, J.; Mendis, M.D.; Christie, C.; Rotstein, A.; Hides, J.A. Gluteus Medius Activation during Running Is a Risk Factor for Season Hamstring Injuries in Elite Footballers. J. Sci. Med. Sport 2017, 20, 159–163. [Google Scholar] [CrossRef]
- Pietraszewski, P.; Gołaś, A.; Matusiński, A.; Mrzygłód, S.; Mostowik, A.; Maszczyk, A. Muscle Activity Asymmetry of the Lower Limbs during Sprinting in Elite Soccer Players. J. Hum. Kinet 2020, 75, 239–245. [Google Scholar] [CrossRef]
- Bogdanis, G.C.; Papaspyrou, A.; Souglis, A.G.; Theos, A.; Sotiropoulos, A.; Maridaki, M. Effects of Two Different Half-squat Training Programs on Fatigue during Repeated Cycling Sprints in Soccer Players. J. Strength Cond. Res. 2011, 25, 1849–1856. [Google Scholar] [CrossRef]
- Helgerud, J.; Rodas, G.; Kemi, O.J.; Hoff, J. Strength and Endurance in Elite Football Players. Int. J. Sports Med. 2011, 32, 677–682. [Google Scholar] [CrossRef]
- Timmins, R.G.; Filopoulos, D.; Nguyen, V.; Giannakis, J.; Ruddy, J.D.; Hickey, J.T.; Maniar, N.; Opar, D.A. Sprinting, Strength, and Architectural Adaptations Following Hamstring Training in Australian Footballers. Scand. J. Med. Sci. Sports 2021, 31, 1276–1289. [Google Scholar] [CrossRef]
- Wisløff, U.; Castagna, C.; Helgerud, J.; Jones, R.; Hoff, J. Strong Correlation of Maximal Squat Strength with Sprint Performance and Vertical Jump Height in Elite Soccer Players. Br. J. Sports Med. 2004, 38, 285–288. [Google Scholar] [CrossRef]
- Soligard, T.; Schwellnus, M.; Alonso, J.M.; Bahr, R.; Clarsen, B.; Dijkstra, H.P.; Gabbett, T.; Gleeson, M.; Hägglund, M.; Hutchinson, M.R.; et al. How Much Is Too Much? (Part 1) International Olympic Committee Consensus Statement on Load in Sport and Risk of Injury. Br. J. Sports Med. 2016, 50, 1030–1041. [Google Scholar] [CrossRef] [PubMed]
- Windt, J.; Gabbett, T.J. How Do Training and Competition Workloads Relate to Injury? The Workload-Injury Aetiology Model. Br. J. Sports Med. 2017, 51, 428–435. [Google Scholar] [CrossRef] [PubMed]
- Gabbett, T.J. The Training-Injury Prevention Paradox: Should Athletes Be Training Smarter and Harder? Br. J. Sports Med. 2016, 50, 273–280. [Google Scholar] [CrossRef] [PubMed]
- Malone, S.; Owen, A.; Newton, M.; Mendes, B.; Collins, K.D.; Gabbett, T.J. The Acute:Chonic Workload Ratio in Relation to Injury Risk in Professional Soccer. J. Sci. Med. Sport 2017, 20, 561–565. [Google Scholar] [CrossRef] [PubMed]
- Raya-González, J.; Nakamura, F.Y.; Castillo, D.; Yanci, J.; Fanchini, M. Determining the Relationship Between Internal Load Markers and Noncontact Injuries in Young Elite Soccer Players. Int. J. Sports Physiol. Perform. 2019, 14, 421–425. [Google Scholar] [CrossRef] [PubMed]
- Zouita, S.; Zouita, A.B.M.; Kebsi, W.; Dupont, G.; Ben-Abderrahman, A.; Ben-Salah, F.Z.; Zouhal, H. Strength Training Reduces Injury Rate in Elite Young Soccer Players during One Season. J. Strength Cond. Res. 2016, 30, 1295–1307. [Google Scholar] [CrossRef]
- Miyazaki, T.; Fujii, N. Effects of Changes in Optimal Muscle Fibre Length in the Biceps Femoris Long Head on Muscle Force during the Late Swing Phase of Maximal Speed Sprinting: A Simulation Study. Sports Biomech. 2022, 8, 1–16. [Google Scholar] [CrossRef]
- Olivares-Jabalera, J.; Fílter-Ruger, A.; Dos’Santos, T.; Afonso, J.; Della Villa, F.; Morente-Sánchez, J.; Soto-Hermoso, V.M.; Requena, B. Exercise-Based Training Strategies to Reduce the Incidence or Mitigate the Risk Factors of Anterior Cruciate Ligament Injury in Adult Football (Soccer) Players: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 13351. [Google Scholar] [CrossRef]
- Pérez-Gómez, J.; Carmelo, J.; Alcaraz, P.; Carlos-Vivas, J. Physical Exercises for Preventing Injuries Among Adult Male Football Players: A Systematic Review. J. Sport. Health Sci. 2022, 11, 115–122. [Google Scholar] [CrossRef]
- Brull-Muria, E.; Beltran-Garrido, J.V. Effects of a Specific Core Stability Program on the Sprint and Change-of-Direction Maneuverability Performance in Youth, Male Soccer Players. Int. J. Environ. Res. Public Health 2021, 18, 10116. [Google Scholar] [CrossRef] [PubMed]
- Hung, K.C.; Chung, H.W.; Yu, C.C.W.; Lai, H.C.; Sun, F.H. Effects of 8-Week Core Training on Core Endurance and Running Economy. PLoS ONE 2019, 14, e0213158. [Google Scholar] [CrossRef] [PubMed]
- Lovell, R.; Siegler, J.C.; Knox, M.; Brennan, S.; Marshall, P.W.M. Acute Neuromuscular and Performance Responses to Nordic Hamstring Exercises Completed before or after Football Training. J. Sports Sci. 2016, 34, 2286–2294. [Google Scholar] [CrossRef] [PubMed]
- Marshall, P.W.; Lovell, R.; Knox, M.F.; Brennan, S.L.; Siegler, J.C. Hamstring Fatigue and Muscle Activation Changes During Six Sets of Nordic Hamstring Exercise in Amateur Soccer Players. J. Strength Cond. Res. 2015, 29, 3124–3133. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, B.; Simmons, J.; O’Shea, P. Weight Training Today; West Publishing: St. Paul, MN, USA, 1989; pp. 201–204. [Google Scholar]
- Foster, C.; Florhaug, J.A.; Franklin, J.; Gottschall, L.; Hrovatin, L.A.; Parker, S.; Doleshal, P.; Dodge, C.A. New Approach to Monitoring Exercise Training. J. Strength Cond. Res. 2001, 15, 109–115. [Google Scholar] [PubMed]
- Los Arcos, A.; Mendez-Villanueva, A.; Martínez-Santos, R. In-Season Training Periodization of Professional Soccer Players. Biol. Sport 2017, 34, 149–155. [Google Scholar] [CrossRef] [PubMed]
- Hooper, S.L.; Mackinnon, L.T. Monitoring Overtraining in Athletes. Recommendations. Sports Med. 1995, 20, 321–327. [Google Scholar] [CrossRef]
- Impellizzeri, F.M.; Rampinini, E.; Maffiuletti, N.; Marcora, S.M. A Vertical Jump Force Test for Assessing Bilateral Strength Asymmetry in Athletes. Med. Sci. Sports Exerc. 2007, 39, 2044–2050. [Google Scholar] [CrossRef]
- Yanci, J.; Los Arcos, A.; Camara, J.; Castillo, D.; García, A.; Castagna, C. Effects of Horizontal Plyometric Training Volume on Soccer Players’ Performance. Res. Sports Med. 2016, 24, 308–319. [Google Scholar] [CrossRef]
- Bosco, C.; Luhtanen, P.; Komi, P.V. A Simple Method for Measurement of Mechanical Power in Jumping. Eur. J. Appl. Physiol. Occup. Physiol. 1983, 50, 273–282. [Google Scholar] [CrossRef]
- González-Montesinos, J.L.; Díaz Romero, N.; García Rodríguez, L.; Mora Vicente, J.; Castro Piñero, J.; Facio Silva, M. Jumping Ability and Elasticity Index in Primary Education. Rev. Int. Med. Cienc. Act Fís Deporte 2007, 7, 359–373. [Google Scholar]
- Sheppard, J.M.; Young, W.B. Agility Literature Review: Classifications, Training and Testing. J. Sports Sci. 2006, 24, 919–932. [Google Scholar] [CrossRef] [PubMed]
- Mendiguchia, J.; Edouard, P.; Samozino, P.; Brughelli, M.; Cross, M.; Ross, A.; Gill, N.; Morin, J.B. Field Monitoring of Sprinting Power–Force–Velocity Profile before, during and after Hamstring Injury: Two Case Reports. J. Sports Sci. 2016, 34, 535–541. [Google Scholar] [CrossRef] [PubMed]
- Spencer, M.; Pyne, D.; Santisteban, J.; Mujika, I. Fitness Determinants of Repeated-Sprint Ability in Highly Trained Youth Football Players. Int. J. Sports Physiol. Perform. 2011, 6, 497–508. [Google Scholar] [CrossRef] [PubMed]
- Spencer, M.; Bishop, D.; Dawson, B.; Goodman, C. Physiological and Metabolic Responses of Repeated-Sprint Activities: Specific to Field-Based Team Sports. Sports Med. 2005, 35, 1025–1044. [Google Scholar] [CrossRef] [PubMed]
- Romero-Franco, N.; Jiménez-Reyes, P.; Montaño-Munuera, J.A. Validity and Reliability of a Low-Cost Digital Dynamometer for Measuring Isometric Strength of Lower Limb. J. Sports Sci. 2017, 35, 2179–2184. [Google Scholar] [CrossRef] [PubMed]
- Newton, R.U.; Gerber, A.; Nimphius, S.; Shim, J.K.; Doan, B.K.; Robertson, M.; Pearson, D.R.; Craig, B.W.; Häkkinen, K.; Kraemer, W.J. Determination of Functional Strength Imbalance of the Lower Extremities. J. Strength Cond. Res. 2006, 20, 971–977. [Google Scholar] [CrossRef]
- Impellizzeri, F.M.; McCall, A.; Meyer, T.; Van Smeden, M. Measures of (Injury and Illness) Occurrence: A Primer on Epidemiological Concepts and Terminology for Authors. Sci. Med. Footb. 2022, 6, 137–140. [Google Scholar] [CrossRef]
- Raya-González, J. Strength Training for Injury Prevention in Soccer: A Systematic Review. J. Phys. Educ. Sports 2017, 49, 23–35. [Google Scholar]
- Kirkwood, B.R. and S.J.A. Essential Medical Statistics; Blackwell Science, Ed.: Oxford, UK, 2003. [Google Scholar]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Lawrence Erlbaum Associates: Hillsdale, MI, USA, 1998. [Google Scholar]
- Mujika, I.; Halson, S.; Burke, L.M.; Balagué, G.; Farrow, D. An Integrated, Multifactorial Approach to Periodization for Optimal Performance in Individual and Team Sports. Int. J. Sports Physiol. Perform. 2018, 13, 538–561. [Google Scholar] [CrossRef]
- West, S.W.; Clubb, J.; Torres-Ronda, L.; Howells, D.; Leng, E.; Vescovi, J.D.; Carmody, S.; Posthumus, M.; Dalen-Lorentsen, T.; Windt, J. More than a Metric: How Training Load Is Used in Elite Sport for Athlete Management. Int. J. Sports Med. 2021, 42, 300–306. [Google Scholar] [CrossRef] [PubMed]
- Semmler, J.G. Motor Unit Synchronization and Neuromuscular Performance. Exerc. Sport Sci. Rev. 2002, 30, 8–14. [Google Scholar] [CrossRef] [PubMed]
- Blazevich, A.J.; Gill, N.D.; Bronks, R.; Newton, R.U. Training-Specific Muscle Architecture Adaptation after 5-Wk Training in Athletes. Med. Sci. Sports Exerc. 2003, 35, 2013–2022. [Google Scholar] [CrossRef]
- Blazevich, A.J.; Cannavan, D.; Coleman, D.R.; Horne, S. Influence of Concentric and Eccentric Resistance Training on Architectural Adaptation in Human Quadriceps Muscles. J. Appl. Physiol. 2007, 103, 1565–1575. [Google Scholar] [CrossRef] [PubMed]
- Walker, S.; Trezise, J.; Haff, G.G.; Newton, R.U.; Häkkinen, K.; Blazevich, A.J. Increased Fascicle Length but Not Patellar Tendon Stiffness after Accentuated Eccentric-Load Strength Training in Already-Trained Men. Eur. J. Appl. Physiol. 2020, 120, 2371–2382. [Google Scholar] [CrossRef] [PubMed]
- Ludwig, O.; Kelm, J. Groin Pain and Muscular Imbalance of Quadriceps and Hamstrings in an Elite Soccer Player—A Case Study. Sportverletz.-Sportschaden 2016, 30, 163–167. [Google Scholar] [CrossRef] [PubMed]
- Rædergård, H.G.; Falch, H.N.; Tillaar, R. Van Den Effects of Strength vs. Plyometric Training on Change of Direction Performance in Experienced Soccer Players. Sports 2020, 8, 144. [Google Scholar] [CrossRef] [PubMed]
- Blazevich, A.J.; Sharp, N.C. Understanding Muscle Architectural Adaptation: Macro- and Micro-Level Research. Cells Tissues Organs 2005, 181, 1–10. [Google Scholar] [CrossRef]
- Pearson, S.J.; McMahon, J. Lower Limb Mechanical Properties: Determining Factors and Implications for Performance. Sports Med. 2012, 42, 929–940. [Google Scholar] [CrossRef]
- Brughelli, M.; Cronin, J.; Levin, G.; Chaouachi, A. Understanding Change of Direction Ability in Sport: A Review of Resistance Training Studies. Sports Med. 2008, 38, 1045–1063. [Google Scholar] [CrossRef]
- Young, W.B.; James, R.; Montgomery, I. Is Muscle Power Related to Running Speed with Changes of Direction? J. Sports Med. Phys. Fitness 2002, 42, 282–288. [Google Scholar] [PubMed]
- Bourgeois, F.; McGuigan, M.; Gill, N.; Gamble, P. Physical Characteristics and Performance in Change of Direction Tasks: A Brief Review and Training Considerations. J. Aust. Strength Cond. 2017, 25, 104–117. [Google Scholar]
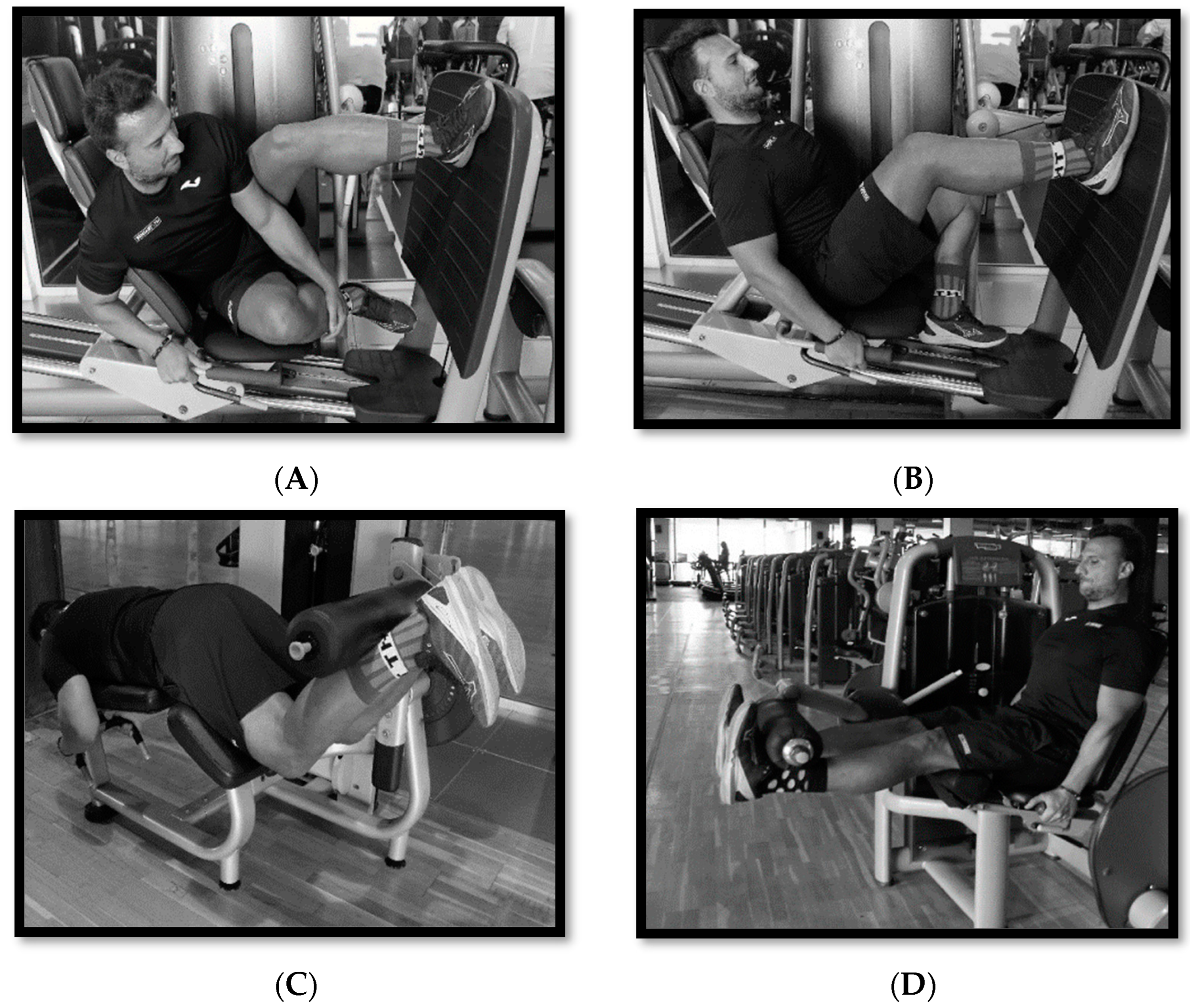


| Exercise | Temporal Sequence of Training Program | Series | Repetitions | Rest between Sets |
|---|---|---|---|---|
| Unilateral horizontal leg Press | W1–2: 85% 1 RM W3–4: 90% 1 RM W5–12: 95% 1 RM | 3 | W1–2: 4 Rep. W3–4: 4 Rep. W5–12: 3 Rep. | 3 min |
| Lateral leg press with 45° support | W1–2: 85% 1 RM W3–4: 90% 1 RM W5–12: 95% 1 RM | 3 | W1–2: 4 Rep. W3–4: 4 Rep. W5–12: 3 Rep. | 3 min |
| Knee extension | W1–2: 85% 1 RM W3–4: 90% 1 RM W5–12: 95% 1 RM | 3 | W1–2: 4 Rep. W3–4: 4 Rep. W5–12: 3 Rep. | 3 min |
| Knee flexion | W1–2: 85% 1 RM W3–4: 90% 1 RM W5–12: 95% 1 RM | 3 | W1–2: 4 Rep. W3–4: 4 Rep. W5–12: 3 Rep. | 3 min |
| RPEL (AU) | Hooper Total (AU) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| CG | EG | %Diff | p | ES | CG | EG | %Diff | p | ES | |
| W1 | 3032.5 ± 417.9 | 3144.0 ± 415.2 | 3.55 | 0.557 | −0.27 | 61.3 ± 10.6 | 64.9 ± 11.2 | 5.55 | 0.468 | −0.33 |
| W2 | 2952.0 ± 427.7 | 2978.5 ± 927.7 | 0.89 | 0.936 | −0.04 | 58.8 ± 9.2 | 57.6 ± 19.4 | −2.08 | 0.862 | 0.08 |
| W3 | 2703.3 ± 538.3 | 3362.8 ± 361.0 | 19.61 | 0.008 ** | −1.44 | 53.4 ± 22.7 | 59.9 ± 23.0 | 10.85 | 0.533 | −0.29 |
| W4 | 3015.0 ± 406.2 | 3310.0 ± 299.3 | 8.91 | 0.095 | −0.84 | 47.9 ± 26.4 | 64.4 ± 10.4 | 25.62 | 0.082 | −0.82 |
| W5 | 2647.2 ±1025.3 | 3247.5 ± 465.7 | 18.48 | 0.113 | −0.77 | 51.7 ± 26.0 | 64.6 ± 8.0 | 19.97 | 0.150 | −0.67 |
| W6 | 3010.0 ± 497.8 | 3216.7 ± 291.5 | 6.42 | 0.298 | −0.51 | 54.9 ± 21.8 | 62.1 ± 17.7 | 11.59 | 0.428 | −0.36 |
| W7 | 2851.1 ± 383.2 | 3256.1 ± 318.1 | 12.44 | 0.027 * | −1.15 | 55.3 ± 20.9 | 57 ± 21.3 | 2.98 | 0.859 | −0.08 |
| W8 | 2744.3 ±1083.0 | 3017.7 ± 416.2 | 9.06 | 0.490 | −0.33 | 51.6 ± 27.8 | 54.7 ± 20.1 | 5.67 | 0.778 | −0.13 |
| W9 | 2583.9 ±1064.1 | 2989.0 ± 337.0 | 13.55 | 0.268 | −0.53 | 49.4 ± 27.7 | 57.6 ± 4.0 | 14.24 | 0.366 | −0.42 |
| W10 | 2671.5 ± 804.0 | 3061.0 ± 360.7 | 12.72 | 0.188 | −0.65 | 45.3 ± 23.5 | 69.7 ± 9.8 | 35.01 | 0.007 ** | −1.36 |
| W11 | 2585.4 ± 926.9 | 2999.4 ± 410.0 | 13.80 | 0.213 | −0.58 | 58.3 ± 23.3 | 60.1 ± 12.1 | 3.00 | 0.831 | −0.10 |
| W12 | 2621.0 ± 431.3 | 3214.0 ± 317.1 | 18.45 | 0.003 ** | −1.57 | 57.5 ± 18.7 | 63.1 ± 8.0 | 8.87 | 0.394 | −0.39 |
| W1–6 | 15,921.0 ± 4142.2 | 18,601.5 ± 2523.4 | 14.41 | 0.098 | −0.78 | 328 ± 89.2 | 373.5 ± 64.3 | 12.18 | 0.207 | −0.59 |
| W7–12 | 14,705.0 ± 5200.0 | 17,909.8 ± 2504.6 | 17.89 | 0.096 | −0.79 | 317.4 ± 115.1 | 362.2 ± 55.8 | 12.37 | 0.283 | −0.50 |
| W1–12 | 30,626.0 ± 7966.5 | 36,511.3 ± 4302.4 | 16.12 | 0.055 | −0.92 | 645.4 ± 174.0 | 735.7 ± 114.3 | 12.27 | 0.187 | −0.61 |
| Total | CG | EG | |
|---|---|---|---|
| Injuries (n) | 6 (100%) | 5(83.3%) | 1(16.7%) |
| Type of injury | |||
| Muscular | 3 (50%) | 3 (50%) | 0 |
| Ligament | 2 (33.3%) | 1 (16.7%) | 1 (16.7%) |
| Tendon | 1 (100% | 1 (100%) | 0 |
| Mechanism of injury | |||
| Direct | 0 | 0 | 0 |
| Indirect | 6 (100%) | 5(83.3%) | 1(16.7%) |
| Overuse | 0 | 0 | 0 |
| Body region | |||
| Thigh | 3 (50%) | 3 (50%) | 0 |
| Knee | 2 (33.3%) | 2 (33.3%) | 0 |
| Ankle | 1 (16.7%) | 0 | 1 (16.7%) |
| Musculoskeletal structure | |||
| Hamstrings | 3 (50%) | 3 (50%) | 0 |
| Knee ligament | 1 (16.7%) | 1 (16.7%) | 0 |
| Patellar tendon | 1 (16.7%) | 1 (16.7%) | 0 |
| Ankle ligament | 1 (16.7%) | 0 | 1 (16.7%) |
| Time and epoch | |||
| Training session | 3 (50%) | 2 (33.3%) | 1 (16.7%) |
| Competition session | 3 (50%) | 3 (50%) | 0 |
| W1–6 | 4 (66.6%) | 3 (50%) | 1 (16.7%) |
| W7–12 | 2 (33.3%) | 2 (33.3%) | 0 |
| Time of absence (days) | |||
| Total | 138 (100%) | 113 (81.9%) | 25(18.1%) |
| Mean ± SD | 34.5 ± 16.6 | 37.7 ± 18.8 |
| CG | EG | Between-Group Differences | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variables | Baseline | Post | %Diff | p | ES | Baseline | Post | %Diff | p | ES | p | F |
| CMJ (cm) | 37.93 ± 3.76 | 38.02 ± 3.90 | 0.24 | 0.468 | −0.24 | 36.69 ± 4.58 | 39.98 ± 4.63 | 8.23 | <0.001 *** | −7.51 | <0.001 *** | 294.93 |
| CMJd (cm) | 22.27 ± 2.79 | 22.20 ± 2.88 | −0.32 | 0.572 | 0.19 | 19.79 ± 4.19 | 21.36 ± 4.03 | 7.35 | <0.001 *** | −5.26 | <0.001 *** | 95.19 |
| CMJnd (cm) | 22.73 ± 3.50 | 22.78 ± 3.41 | 0.22 | 0.630 | −0.16 | 21.20 ± 4.13 | 22.67 ± 4.22 | 6.48 | <0.001 *** | −3.60 | <0.001 *** | 67.90 |
| CMJLA (%) | −1.85 ± 5.75 | −0.28 ± 1.41 | −556.38 | 0.452 | −0.25 | −7.85 ± 9.21 | −7.09 ± 1.82 | −10.69 | 0.812 | −0.08 | <0.001 *** | 81.48 |
| SJ (cm) | 31.04 ± 3.97 | 30.97 ± 3.86 | −0.23 | 0.563 | 0.19 | 29.52 ± 3.61 | 31.48 ± 3.35 | 6.23 | <0.001 *** | −3.96 | <0.001 *** | 114.50 |
| EI (%) | 23.55 ± 15.55 | 24.06 ± 15.85 | −0.25 | 0.452 | 0.09 | 24.59 ± 9.85 | 27.16 ± 8.91 | −0.93 | 0.016 * | −0.30 | 0.075 | 3.58 |
| 505-CODAd (s) | 2.26 ± 0.07 | 2.26 ± 0.09 | −0.09 | 0.785 | 0.09 | 2.31 ± 0.06 | 2.21 ± 0.05 | −4.80 | <0.001 *** | 5.77 | <0.001 *** | 108.68 |
| 505-CODnd (s) | 2.26 ± 0.08 | 2.26 ± 0.07 | −0.09 | 0.764 | 0.10 | 2.29 ± 0.07 | 2.18 ± 0.06 | −4.99 | <0.001 *** | 3.83 | <0.001 *** | 115.22 |
| 505-CODALA (%) | −0.18 ± 1.80 | −0.23 ± 2.48 | 19.91 | 0.931 | 0.03 | 0.95 ± 1.89 | 1.12 ± 1.68 | 15.76 | 0.715 | −0.12 | 0.555 | 0.36 |
| SPR10 (s) | 1.70 ± 0.07 | 1.69 ± 0.06 | −0.77 | 0.018 * | 0.92 | 1.74 ± 0.07 | 1.65 ± 0.07 | −5.21 | <0.001 *** | 1.94 | <0.001 *** | 20.10 |
| SPR20 (s) | 2.93 ± 0,10 | 2.91 ± 0.10 | −0.55 | 0.168 | 0.47 | 2.99 ± 0.11 | 2.87 ± 0.13 | −4.11 | <0.001 *** | 1.64 | 0.002 ** | 13.74 |
| SPR40 (s) | 5.31 ± 0.16 | 5.29 ± 0.15 | −0.30 | 0.112 | 0.56 | 5.40 ± 0.19 | 5.25 ± 0.20 | −2.84 | <0.001 *** | 1.64 | <0.001 *** | 16.23 |
| RSAtotal (s) | 21.85 ± 0.43 | 21.71 ± 0.45 | −0.64 | 0.010 * | 1.02 | 22.34 ± 0.70 | 21.50 ± 0.66 | −3.92 | <0.001 *** | 5.34 | <0.001 *** | 87.34 |
| RSASdec (s) | 3.11 ± 0.95 | 3.04 ± 0.68 | −2.33 | 0.775 | 0.09 | 4.15 ± 1.24 | 3.10 ± 0.76 | −33.94 | 0.003 ** | 1.25 | 0.141 | 2.38 |
| ISOQUAd (kg) | 40.87 ± 5.19 | 41.09 ± 5.04 | 0.54 | 0.073 | −0.64 | 40.30 ± 4.06 | 44.24 ± 3.84 | 8.91 | <0.001 *** | −10.96 | <0.001 *** | 741.72 |
| ISOQUAnd (kg) | 39.20 ± 4.77 | 39.51 ± 4.76 | 0.78 | 0.003 ** | −1.28 | 39.25 ± 4.48 | 43.29 ± 4.48 | 9.33 | <0.001 *** | −11.86 | <0.001 *** | 753.38 |
| ISOQUALA (%) | 3.77 ± 7.92 | 3.59 ± 7.49 | −5.10 | 0.462 | 0.24 | 2.45 ± 8.55 | 2.04 ± 7.91 | −19.84 | 0.374 | 0.30 | 0.471 | 0.54 |
| ISOHAMSd (kg) | 22.57 ± 3.05 | 22.68 ± 2.91 | 0.49 | 0.281 | −0.36 | 22.01 ± 2.55 | 26.22 ± 2.58 | 16.06 | <0.001 *** | −9.96 | <0.001 *** | 608.11 |
| ISOHAMSnd (kg) | 22.33 ± 2.82 | 22.55 ± 3.01 | 0.98 | 0.051 | −0.71 | 22.00 ± 2.93 | 26.27 ± 3.04 | 16.25 | <0.001 *** | −6.97 | <0.001 *** | 349.22 |
| ISOHAMSLA (%) | 0.83 ± 6.23 | 0.51 ± 6.14 | −61.76 | 0.648 | 0.15 | 0.06 ± 7.16 | −0.21 ± 7.15 | 130.19 | 0.711 | 0.12 | 0.994 | 5.93 |
| Imb.Q-H Right (%) | 44.79 ± 2.33 | 44.81 ± 2.15 | 0.04 | 0.901 | −0.04 | 45.41 ± 2.60 | 40.75 ± 2.18 | −11.43 | <0.001 *** | 3.71 | <0.001 *** | 139.39 |
| Imb.Q-H Left (%) | 43.05 ± 1.94 | 42.99 ± 2.19 | −0.13 | 0.839 | 0.07 | 44.00 ± 3.23 | 39.36 ± 2.08 | −11.78 | <0.001 *** | 2.37 | <0.001 *** | 56.70 |
| ISOABDd (kg) | 29.81 ± 5.59 | 30.16 ± 5.58 | 1.16 | <0.001 *** | −1.79 | 27.93 ± 4.65 | 32.36 ± 4.66 | 13.69 | <0.001 *** | −8.00 | <0.001 *** | 438.81 |
| ISOABDnd (kg) | 28.75 ± 4.54 | 28.83 ± 4.45 | 0.28 | 0.380 | −0.29 | 27.87 ± 4.24 | 31.51 ± 4.02 | 11.55 | <0.001 *** | −9.22 | <0.001 *** | 651.64 |
| ISOABDLA (%) | 2.86 ± 7.38 | 3.69 ± 7.75 | 22.47 | 0.011 * | −1.02 | −0.34 ± 9.46 | 2.12 ± 8.58 | 116.25 | 0.009 ** | −1.05 | 0.086 | 3.32 |
| ISOADDd (kg) | 24.61 ± 4.00 | 25.89 ± 4.78 | 4.94 | 0.234 | −0.40 | 23.97 ± 2.91 | 24.57 ± 2.79 | 2.44 | <0.001 *** | −1.78 | 0.489 | 0.50 |
| ISOADDnd (kg) | 24.41 ± 3.65 | 24.67 ± 3.74 | 1.05 | 0.011 * | −1.00 | 24.18 ± 2.89 | 24.62 ± 2.84 | 1.79 | <0.001 *** | −1.86 | 0.130 | 2.53 |
| ISOADDLA (%) | 0.51 ± 5.91 | 3.48 ± 11.98 | 85.25 | 0.338 | −0.32 | −1.02 ± 5.61 | −0.29 ± 5.08 | −254.36 | 0.201 | −0.44 | 0.510 | 0.45 |
| Imb.Abd-Add Right (%) | 16.83 ± 6.51 | 13.76 ± 8.33 | −22.29 | 0.340 | 0.32 | 13.19 ± 9.46 | 23.53 ± 6.67 | 43.94 | <0.001 *** | −3.27 | <0.001 *** | 16.45 |
| Imb.Abd-Add Left (%) | 14.76 ± 6.09 | 14.11 ± 6.76 | −4.67 | 0.142 | 0.51 | 12.56 ± 7.53 | 21.56 ± 5.46 | 41.76 | <0.001 *** | −3.16 | <0.001 *** | 103.93 |
| CG | EG | All | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variables | Injured (n = 6) | Not Injured (n = 4) | %Diff | p; ES | Injured (n = 1) | Not Injured (n = 9) | %Diff | ES | Injured (n = 7) | Not Injured (n = 13) | %Diff | p; ES |
| RPEL | ||||||||||||
| W1–6 | 13,763.0 ± 5153.0 | 18,079.0 ± 639.3 | −31.36 | 0.134; 1.18 | 15,990.0 | 18,891.7 ± 2493.3 | −18.15 | 1.16 | 14,134.2 ± 4697.8 | 18,601.4 ± 2028.5 | −31.61 | 0.009 **; 0.74 |
| W7–12 | 12,242.0 ± 6415.7 | 17,168.0 ± 2123.9 | −40.24 | 0.166; 1.03 | 10,931.0 | 18,685.2 ± 541.1 | −70.94 | 14.33 | 12,023.5 ± 5763.3 | 18,143.4 ± 1462.0 | −50.90 | 0.006 **; 0.76 |
| W1–12 | 26,005.0 ± 9263.6 | 35,247.0 ± 1897.0 | −35.54 | 0.089; 1.38 | 26,921.0 | 37,576.9 ± 2837.3 | −39.58 | 3.76 | 26,157.7 ± 8294.1 | 36,744.8 ± 2720.9 | −40.47 | <0.001 ***; 2.14 |
| Hooper total | ||||||||||||
| W1–6 | 279.0 ± 101.6 | 377.0 ± 39.6 | −35.13 | 0.099; 1.27 | 293.0 | 382.4 ± 61.3 | −30.53 | 1.46 | 281.3 ± 91.1 | 380.5 ± 53.0 | −35.25 | 0.006 **; 1.51 |
| W7–12 | 253.6 ± 133.8 | 381.2 ± 41.8 | −50.32 | 0.100; 1.29 | 231.0 | 376.8 ± 33.3 | −63.11 | 4.38 | 249.8 ± 120.1 | 378.4 ± 35.0 | −51.44 | 0.001 **; 1.84 |
| W1–12 | 532.6 ± 183.8 | 758.2 ± 50.3 | −42.36 | 0.050; 1.67 | 524.0 | 759.2 ± 92.1 | −44.90 | 2.55 | 531.2 ± 164.5 | 758.9 ± 77.4 | −42.87 | <0.001 ***; 2.10 |
| Hooper Sleep | ||||||||||||
| W1–6 | 44.40 ± 18.53 | 66.20 ± 10.3 | −49.10 | 0.051; 1.45 | 51.0 | 67.6 ± 9.6 | −32.55 | 1.73 | 45.5 ± 16.8 | 67.1 ± 9.5 | −47.47 | 0.002 **; 1.80 |
| W7–12 | 39.6 ± 24.8 | 64.0 ± 13.0 | −61.62 | 0.087; 1.23 | 43.0 | 62.3 ± 8.8 | −44.88 | 2.20 | 40.2 ± 22.2 | 62.9 ± 10.0 | −56.47 | 0.054; 1.32 |
| W1–12 | 84.0 ± 35.1 | 130.2 ± 16.9 | −55.00 | 0.029 *; 1.68 | 94.0 | 129.9 ± 17.0 | −66.48 | 2.11 | 85.7 ± 31.7 | 130.0 ± 16.3 | −51.69 | <0.001 ***; 2.04 |
| Hooper Stress | ||||||||||||
| W1–6 | 53.2 ± 16.3 | 81.4 ± 20.2 | −53.01 | 0.041 *; 1.54 | 43.0 | 68.0 ± 12.2 | −58.14 | 2.04 | 51.5 ± 15.1 | 72.8 ± 16.2 | −41.36 | 0.013 *; 1.34 |
| W7–12 | 43.0 ± 18.8 | 66.0 ± 9.4 | −53.49 | 0.040 *; 1.55 | 48.0 | 66.6 ± 10.7 | −38.75 | 1.74 | 43.8 ± 16.9 | 66.4 ± 9.9 | −51.60 | 0.001 **; 1.84 |
| W1–12 | 105.2 ± 41.0 | 164.6 ± 36.1 | −56.46 | 0.041 *; 1.54 | 87.0 | 135.3 ± 20.6 | −55.52 | 2.35 | 102.2 ± 37.4 | 145.8 ± 29.5 | −42.66 | 0.012 *; 1.37 |
| Hooper Fatigue | ||||||||||||
| W1–6 | 82.8 ± 32.8 | 107.4 ± 10.7 | −29.71 | 0.173; 1.01 | 95.0 | 121.0 ± 21.8 | −27.37 | 1.19 | 84.8 ± 29.7 | 116.1 ± 19.3 | −36.91 | 0.011 *; 1.38 |
| W7–12 | 53.2 ± 17.5 | 80.8 ± 20.2 | −51.88 | 0.049 *; 1.46 | 40.0 | 68.2 ± 12.4 | −70.50 | 2.28 | 51.0 ± 16.5 | 72.7 ± 16.1 | −42.55 | 0.013 *; 1.34 |
| W1–12 | 160.4 ± 54.0 | 217.4 ± 8.8 | −35.54 | 0.077; 1.48 | 167.0 | 239.8 ± 32.4 | −43.59 | 2.25 | 161.5 ± 48.3 | 231.8 ± 28.2 | −43.53 | <0.001 ***; 2.01 |
| Hooper Muscle soreness | ||||||||||||
| W1–6 | 98.6 ± 36.1 | 122.0 ± 7.9 | −23.73 | 0.224; 0.90 | 104.0 | 125.9 ± 20.0 | −21.06 | 1.10 | 99.5 ± 32.4 | 124.5 ± 16.4 | −25.13 | 0.122; 0.97 |
| W7–12 | 82.8 ± 33.4 | 107.0 ± 9.4 | −29.23 | 0.184; 0.99 | 92.0 | 120.0 ± 21.9 | −30.43 | 1.28 | 84.3 ± 30.1 | 115.4 ± 19.1 | −36.89 | 0.012 *; 1.37 |
| W1–12 | 183.0 ± 60.6 | 246.0 ± 13.9 | −34.43 | 0.080; 1.43 | 176.0 | 254.2 ± 26.8 | −44.43 | 2.92 | 181.8 ± 54.3 | 251.3 ± 22.8 | −38.23 | 0.024 *; 1.67 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Durán-Custodio, R.; Castillo, D.; Raya-González, J.; Yanci, J. Is a Maximal Strength-Training Program Effective on Physical Fitness, Injury Incidence, and Injury Burden in Semi-Professional Soccer Players? A Randomized Controlled Trial. Healthcare 2023, 11, 3195. https://doi.org/10.3390/healthcare11243195
Durán-Custodio R, Castillo D, Raya-González J, Yanci J. Is a Maximal Strength-Training Program Effective on Physical Fitness, Injury Incidence, and Injury Burden in Semi-Professional Soccer Players? A Randomized Controlled Trial. Healthcare. 2023; 11(24):3195. https://doi.org/10.3390/healthcare11243195
Chicago/Turabian StyleDurán-Custodio, Roberto, Daniel Castillo, Javier Raya-González, and Javier Yanci. 2023. "Is a Maximal Strength-Training Program Effective on Physical Fitness, Injury Incidence, and Injury Burden in Semi-Professional Soccer Players? A Randomized Controlled Trial" Healthcare 11, no. 24: 3195. https://doi.org/10.3390/healthcare11243195
APA StyleDurán-Custodio, R., Castillo, D., Raya-González, J., & Yanci, J. (2023). Is a Maximal Strength-Training Program Effective on Physical Fitness, Injury Incidence, and Injury Burden in Semi-Professional Soccer Players? A Randomized Controlled Trial. Healthcare, 11(24), 3195. https://doi.org/10.3390/healthcare11243195









