Towards the Future of Public Health: Roadmapping Trends and Scenarios in the Post-COVID Healthcare Era
Abstract
1. Introduction
2. Materials and Methods
- RQ1: What are the possible long-term consequences of the COVID-19 pandemic?
- RQ2: How can we improve global public healthcare to achieve the population’s needs?
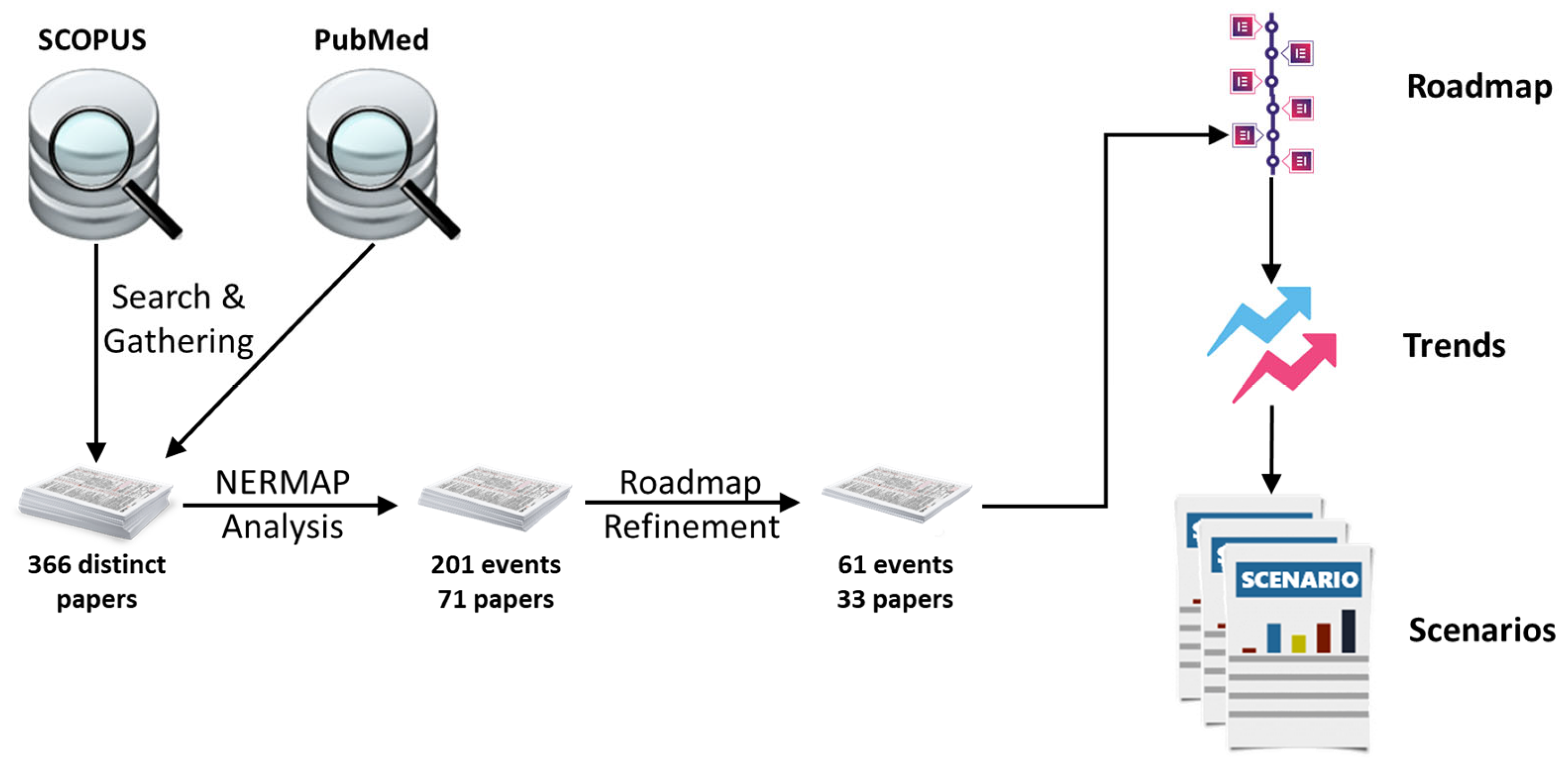
- Collect relevant literature on public Hhealth by systematically searching scientific databases: SCOPUS and PubMed—science databases relevant to understanding this work’s technological and medical aspects. We removed duplicate documents.
- The NERMAP tool extracts candidate future events and builds an initial roadmap.
- We analyze and refine the pre-built roadmap, producing a final roadmap.
- We use the roadmap to develop future scenarios for public health.
3. Results
3.1. Roadmap
3.2. Trends
- The population is aging, leading to a rise in the number of individuals with multiple disabilities and long-term care requirements.
- Mental disorders will increase in incidence and prevalence, particularly depressive disorders and dementia associated with aging, in addition to anxiety conditions, reflecting the effect of the COVID-19 pandemic on the younger population.
- The incorporation of new technologies will allow the availability of new vaccines.
- The locus of health action will shifted from medical facilities to households, thanks to the growing popularity of “virtual health”, which includes introducing more home diagnostic tools (self-tests) and telemedicine.
- There will be a growing need to adopt a more decisive approach toward addressing the causes and risk factors that lead to individual or population health problems. This approach should prioritize primary prevention measures that aim to prevent the development of clinical conditions and early diagnosis and treatment measures for secondary prevention.
- Information and Communication Technologies (ICTs) will play a leading role in transforming healthcare systems and their care models, enabling the adoption of new technologies that allow for flexible formats of care delivery. This shift will lead to a greater emphasis on value-based care, as opposed to traditional volume-based care, which has helped to improve the overall quality of healthcare services.
- Regardless of the stage of development of each nation’s search for the best model of care to achieve its ideal health system, the patient will always be considered a central figure.
- There will be an increase in large tech companies (Big Tech) in the health sector.
- There will be a significant increase in the utilization of nanotechnology within the healthcare industry.
- Technological and industrial developments will be made with a significant innovative capacity for public health. Changes in technologies will favor early diagnosis, information and communication technologies, equipment equipped with connectivity, portability, and security, and less invasive equipment.
- The large-scale use of health data and other data from various diverse, relevant sources will create a multifaceted and highly personalized picture of each user’s health profile and consumption/use of health services.
- The progression of chronic diseases to more advanced stages, coupled with the failure of healthcare systems to prioritize preventive measures, will increase health costs.
- Public spending on health will lead to essential changes in the capacity of health systems, especially in the volume and quality of health services.
- The maintenance of social and economic inequalities between countries. There will be difficulties in establishing more effective sanitary controls. Example: difficulty implementing preventive measures, such as immunization, which are more “homogeneous” between countries.
- Developing countries will persist in facing endemic diseases, including but not limited to syphilis and other sexually transmitted diseases, malaria, tuberculosis, leptospirosis, leishmaniasis, hospital infections, and arboviruses. New viruses occurring in other countries could result in new pandemics.
- Governments will broaden their vision beyond their political-administrative limits by strengthening intergovernmental partnerships at the regional level.
- There will be challenges with complementarity between the public and private sectors, which should ideally function as partners to achieve the best outcomes for universal health coverage. However, finding the balance point for avoiding accentuating social inequalities will still be challenging.
3.3. Scenarios
3.3.1. The Possible and Optimistic Scenario
3.3.2. The Likely and Neutral Scenario
3.3.3. The Plausible and Pessimistic Scenario
4. Discussion
4.1. Population Aging with an Increase in the Number of People with Multiple Disabilities and Need for Long-Term Care and an Increase in Mental Disorders
4.2. The Migration of the Locus of Health Action from the Health Care Units to the Homes with an Increase in the Use of “Virtual Health” (Development of More Home Diagnostic Tools (Self-Tests) and Telemedicine)
4.3. The Large-Scale Use of Health Data Together with Others from a Variety of Different Relevant Sources to Create a Multifaceted and Highly Personalized Health Profile and Profile of the Use of Health Services of Each User
4.4. The Growth in the Use of Nanotechnology in the Healthcare Field
4.5. The Performance of Big Tech in Health
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tulchinsky, T.H.; Varavikova, E.A. A History of Public Health. New Public Health 2014, 1–42. [Google Scholar] [CrossRef]
- Fülöp, M.T.; Breaz, T.O.; He, X.; Ionescu, C.A.; Cordoş, G.S.; Stanescu, S.G. The Role of Universities’ Sustainability, Teachers’ Wellbeing, and Attitudes toward e-Learning during COVID-19. Front. Public Health 2022, 10, 981593. [Google Scholar] [CrossRef] [PubMed]
- Koutroukis, T.; Chatzinikolaou, D.; Vlados, C.; Pistikou, V. The Post-COVID-19 Era, Fourth Industrial Revolution, and New Globalization: Restructured Labor Relations and Organizational Adaptation. Societies 2022, 12, 187. [Google Scholar] [CrossRef]
- Gukasyan, Z.O.; Tavbulatova, Z.K.; Aksenova, Z.A.; Gasanova, N.M.; Karpunina, E.K. Strategies for Adapting Companies to the Turbulence Caused by the COVID-19 Pandemic. In Business 4.0 as a Subject of the Digital Economy; Popkova, E.G., Ed.; Advances in Science, Technology & Innovation; Springer International Publishing: Cham, Switzerland, 2022; pp. 639–645. ISBN 978-3-030-90324-4. [Google Scholar]
- Fülöp, M.T.; Breaz, T.O.; Topor, I.D.; Ionescu, C.A.; Dragolea, L.-L. Challenges and Perceptions of E-Learning for Educational Sustainability in the “New Normality Era”. Front. Psychol. 2023, 14, 1104633. [Google Scholar] [CrossRef] [PubMed]
- Legge, D.G. COVID-19 Response Exposes Deep Flaws in Global Health Governance. Global Social Policy 2020, 20, 383–387. [Google Scholar] [CrossRef]
- Wang, Z.; Duan, Y.; Jin, Y.; Zheng, Z.-J. Coronavirus Disease 2019 (COVID-19) Pandemic: How Countries Should Build More Resilient Health Systems for Preparedness and Response. Glob. Health J. 2020, 4, 139–145. [Google Scholar] [CrossRef] [PubMed]
- Gostin, L.O.; Moon, S.; Meier, B.M. Reimagining Global Health Governance in the Age of COVID-19. Am. J. Public Health 2020, 110, 1615–1619. [Google Scholar] [CrossRef]
- Yglesias-González, M.; Palmeiro-Silva, Y.; Sergeeva, M.; Cortés, S.; Hurtado-Epstein, A.; Buss, D.F.; Hartinger, S.M. Code Red for Health Response in Latin America and the Caribbean: Enhancing Peoples’ Health through Climate Action. Lancet Reg. Health-Am. 2022, 11, 100248. [Google Scholar] [CrossRef]
- Rehfuess, E.A.; Burns, J.B.; Pfadenhauer, L.M.; Krishnaratne, S.; Littlecott, H.; Meerpohl, J.J.; Movsisyan, A. Lessons Learnt: Undertaking Rapid Reviews on Public Health and Social Measures during a Global Pandemic. Res. Synth. Methods 2022, 13, 558–572. [Google Scholar] [CrossRef]
- Cameron, A.; Esiovwa, R.; Connolly, J.; Hursthouse, A.; Henriquez, F. Antimicrobial Resistance as a Global Health Threat: The Need to Learn Lessons from the COVID-19 Pandemic. Glob. Policy 2022, 13, 179–192. [Google Scholar] [CrossRef]
- Sachs, J.D.; Karim, S.S.A.; Aknin, L.; Allen, J.; Brosbøl, K.; Colombo, F.; Barron, G.C.; Espinosa, M.F.; Gaspar, V.; Gaviria, A.; et al. The Lancet Commission on Lessons for the Future from the COVID-19 Pandemic. Lancet 2022, 400, 1224–1280. [Google Scholar] [CrossRef] [PubMed]
- de Lyra, A.O.; Barbosa, C.E.; de Lima, Y.O.; dos Santos, H.S.; Argôlo, M.; de Souza, J.M. Toward Computer-Supported Semi-Automated Timelines of Future Events. Eur. J. Futures Res. 2023, 11, 4. [Google Scholar] [CrossRef]
- de Lyra, A.O. NERMAP: Apoiando o Processo de Roadmapping Tecnológico a Partir da Técnica de Reconhecimento de Entidades Nomeadas; Universidade Federal do Rio de Janeiro: Rio de Janeiro, Brazil, 2021. [Google Scholar]
- Lyra, A.; Barbosa, C.E.; Lima, Y.; Salazar, H.; Souza, J. NERMAP: Collaborative Building of Technological Roadmaps Using Named Entity Recognition. In Proceedings of the 2022 IEEE 25th International Conference on Computer Supported Cooperative Work in Design (CSCWD), Hangzhou, China, 4 May 2022; pp. 986–991. [Google Scholar]
- OpenAI, R. GPT-4 Technical Report. arXiv 2023, arXiv:2303.08774. [Google Scholar]
- Manyika, J.; Hsiao, S. An Overview of Bard: An Early Experiment with Generative AI; Google: Mouyntain View, CA, USA, 2023. [Google Scholar]
- Touvron, H.; Martin, L.; Stone, K. Llama 2: Open Foundation and Fine-Tuned Chat Models; Meta: Menlo Park, CA, USA, 2023. [Google Scholar]
- xAI xAI Grok. Available online: https://grok.x.ai/ (accessed on 13 November 2023).
- Oliveira, M.G.; Freitas, J.S.; Fleury, A.L.; Rozenfeld, H.; Phaal, R.; Probert, D.; Cheng, L.C. Roadmapping: Uma Abordagem Estratégica Para o Gerenciamento da Inovação em Produtos, Serviços e Tecnologias; Elsevier: Rio de Janeiro, Brazil, 2012. [Google Scholar]
- Phaal, R.; Farrukh, C.J.P.; Probert, D.R. Technology Roadmapping—A Planning Framework for Evolution and Revolution. Technol. Forecast. Soc. Change 2004, 71, 5–26. [Google Scholar] [CrossRef]
- Cartaxo, B.; Pinto, G.; Soares, S. The Role of Rapid Reviews in Supporting Decision-Making in Software Engineering Practice; ACM: Christchurch, New Zealand, 2018; pp. 24–34. [Google Scholar]
- Motta, R.C.; de Oliveira, K.M.; Travassos, G.H. A Conceptual Perspective on Interoperability in Context-Aware Software Systems. Inf. Softw. Technol. 2019, 114, 231–257. [Google Scholar] [CrossRef]
- El-Warrak, L.; Nunes, M.; Lyra, A.; Barbosa, C.E.; Lima, Y.; Salazar, H.; Argôlo, M.; de Souza, J.M. Analyzing Industry 4.0 Trends through the Technology Roadmapping Method. Procedia Comput. Sci. 2022, 201, 511–518. [Google Scholar] [CrossRef]
- Simões, R.V.; Parreiras, M.V.C.; da Silva, A.C.C.; Barbosa, C.E.; de Lima, Y.O.; de Souza, J.M. Artificial Intelligence and Digital Transformation: Analyzing Future Trends. In Proceedings of the 2022 IEEE International Conference on Systems, Man, and Cybernetics (SMC), Prague, Czech Republic, 9–12 October 2022; p. 6. [Google Scholar]
- Paes, V.; Pessoa, C.; Pagliusi, R.; Barbosa, C.E.; Margarido Argôlo, M.; Lima, Y.; Santos, H.; Lyra, A.; Souza, J. Analyzing the Challenges for Future Smart and Sustainable Cities. Sustainability 2023, 15, 7996. [Google Scholar] [CrossRef]
- Kentikelenis, A.; Stubbs, T. Austerity Redux: The Post-Pandemic Wave of Budget Cuts and the Future of Global Public Health. Glob. Policy 2021, 13, 5–17. [Google Scholar] [CrossRef]
- Ariyamuthu, V.K.; Sandikci, B.; AbdulRahim, N.; Hwang, C.; MacConmara, M.P.; Parasuraman, R.; Atis, A.; Tanriover, B. Trends in Utilization of Deceased Donor Kidneys Based on Hepatitis C Virus Status and Impact of Public Health Service Labeling on Discard. Transpl. Infect. Dis. 2020, 22, e13204. [Google Scholar] [CrossRef]
- Nundoochan, A. Improving Equity in the Distribution and Financing of Health Services in Mauritius, a Small Island State with Deeply Rooted Welfare State Standards. BMJ Glob. Health 2021, 6, e006757. [Google Scholar] [CrossRef]
- Gaille, M.; Horn, R. UK-FR GENE (Genetics and Ethics Network) Consortia The Ethics of Genomic Medicine: Redefining Values and Norms in the UK and France. Eur. J. Hum. Genet. 2021, 29, 780–788. [Google Scholar] [CrossRef]
- Erzse, A.; Stacey, N.; Chola, L.; Tugendhaft, A.; Freeman, M.; Hofman, K. The Direct Medical Cost of Type 2 Diabetes Mellitus in South Africa: A Cost of Illness Study. Glob. Health Action 2019, 12, 1636611. [Google Scholar] [CrossRef] [PubMed]
- Baker, P.R.A.; Dingle, K.; Dunne, M.P. Future of Public Health Training: What Are the Challenges? What Might the Solutions Look Like? Asia-Pac. J. Public Health 2018, 30, 691–698. [Google Scholar] [CrossRef] [PubMed]
- Serebrisky, D.; Wiznia, A. Pediatric Asthma: A Global Epidemic. Ann. Glob. Health 2019, 85, 6. [Google Scholar] [CrossRef] [PubMed]
- Bisht, R.; Saharia, R.; Sarma, J. COVID-19 and the Burden of Ill-Health: A Double Crisis of Disruptions and Inequalities. J. Soc. Econ. Dev. 2021, 23, 342–356. [Google Scholar] [CrossRef] [PubMed]
- Beyer, T.; Bidaut, L.; Dickson, J.; Kachelriess, M.; Kiessling, F.; Leitgeb, R.; Ma, J.; Shiyam Sundar, L.K.; Theek, B.; Mawlawi, O. What Scans We Will Read: Imaging Instrumentation Trends in Clinical Oncology. Cancer Imaging 2020, 20, 38. [Google Scholar] [CrossRef] [PubMed]
- Walicka, M.; Raczyńska, M.; Marcinkowska, K.; Lisicka, I.; Czaicki, A.; Wierzba, W.; Franek, E. Amputations of Lower Limb in Subjects with Diabetes Mellitus: Reasons and 30-Day Mortality. J. Diabetes Res. 2021, 2021, 8866126. [Google Scholar] [CrossRef] [PubMed]
- Godman, B.; Haque, M.; Islam, S.; Iqbal, S.; Urmi, U.L.; Kamal, Z.M.; Shuvo, S.A.; Rahman, A.; Kamal, M.; Haque, M.; et al. Rapid Assessment of Price Instability and Paucity of Medicines and Protection for COVID-19 Across Asia: Findings and Public Health Implications for the Future. Front. Public Health 2020, 8, 585832. [Google Scholar] [CrossRef]
- Kalla, I.S.; Miri, A.; Seedat, F. Occult Pulmonary Arterial Hypertension in Patients with Previous Pulmonary Tuberculosis. Afr Afr. J. Thorac. Crit. Care Med. 2020, 26, 133–137. [Google Scholar] [CrossRef]
- Yadav, P.R.; Munni, M.N.; Campbell, L.; Mostofa, G.; Dobson, L.; Shittu, M.; Pattanayek, S.K.; Uddin, M.J.; Das, D.B. Translation of Polymeric Microneedles for Treatment of Human Diseases: Recent Trends, Progress, and Challenges. Pharmaceutics 2021, 13, 1132. [Google Scholar] [CrossRef]
- England, K.; Azzopardi-Muscat, N. Demographic Trends and Public Health in Europe. Eur. J. Public Health 2017, 27, 9–13. [Google Scholar] [CrossRef] [PubMed]
- Amador, M.; Matias-Guiu, X.; Sancho-Pardo, G.; Contreras Martinez, J.; de la Torre-Montero, J.C.; Peñuelas Saiz, A.; Garrido, P.; García-Sanz, R.; Rodríguez-Lescure, Á.; Paz-Ares, L. Impact of the COVID-19 Pandemic on the Care of Cancer Patients in Spain. ESMO Open 2021, 6, 100157. [Google Scholar] [CrossRef] [PubMed]
- Mager, N.D.; Moore, T.S. Healthy People 2030: Roadmap for Public Health for the next Decade. Am. J. Pharm. Educ. 2020, 84, 1541–1544. [Google Scholar] [CrossRef] [PubMed]
- Mcinerney, T.F. The WHO FCTC and Global Governance: Effects and Implications for Future Global Public Health Instruments. Tob. Control. 2019, 28, S89–S93. [Google Scholar] [CrossRef] [PubMed]
- Lindström, B. Workshop Salutogenesis and the Future of Health Promotion and Public Health. Scand. J. Public Health 2018, 46, 94–98. [Google Scholar] [CrossRef] [PubMed]
- Crayton, T.J.; Meier, B.M. Autonomous Vehicles: Developing a Public Health Research Agenda to Frame the Future of Transportation Policy. J. Transp. Health 2017, 6, 245–252. [Google Scholar] [CrossRef]
- Tesfaye, G.; Loxton, D.; Chojenta, C.; Assefa, N.; Smith, R. Magnitude, Trends and Causes of Maternal Mortality among Reproductive Aged Women in Kersa Health and Demographic Surveillance System, Eastern Ethiopia 11 Medical and Health Sciences 1117 Public Health and Health Services 11 Medical and Health Sciences 1114 Paediatrics and Reproductive Medicine. BMC Womens Health 2018, 18, 198. [Google Scholar] [CrossRef]
- Makhele, L.; Matlala, M.; Sibanda, M.; Martin, A.P.; Godman, B. A Cost Analysis of Haemodialysis and Peritoneal Dialysis for the Management of End-Stage Renal Failure At an Academic Hospital in Pretoria, South Africa. Pharm. Open 2019, 3, 631–641. [Google Scholar] [CrossRef]
- Catalanotti, J.S.; Popiel, D.K.; Barbour, A. Retaining Interest in Caring for Underserved Patients among Future Medicine Subspecialists: Underserved Medicine and Public Health (UMPH) Program. BMC Med. Educ. 2021, 21, 589. [Google Scholar] [CrossRef]
- Little, N.R.G.; Welsh, P.; Sholar, A. Developing Future Public Health Leaders Trained in Long-Term Care Administration. J. Public Health Manag. Pract. 2021, 27, E79–E86. [Google Scholar] [CrossRef]
- Lim, G.X.D. Special Care Dentistry in a Charity Clinic: Demographic Analysis and Barriers to Care in Singapore. Ci Ji Yi Xue Za Zhi 2019, 31, 232–239. [Google Scholar] [CrossRef] [PubMed]
- Obón-Santacana, M.; Vilardell, M.; Carreras, A.; Duran, X.; Velasco, J.; Galván-Femenía, I.; Alonso, T.; Puig, L.; Sumoy, L.; Duell, E.J.; et al. GCAT|Genomes for Life: A Prospective Cohort Study of the Genomes of Catalonia. BMJ Open 2018, 8, e018324. [Google Scholar] [CrossRef] [PubMed]
- Walbaum, M.; Scholes, S.; Rojas, R.; Mindell, J.S.; Pizzo, E. Projection of the Health and Economic Impacts of Chronic Kidney Disease in the Chilean Population. PLoS ONE 2021, 16, e0256680. [Google Scholar] [CrossRef] [PubMed]
- Ackerman, I.N.; Zomer, E.; Gilmartin-Thomas, J.F.-M.; Liew, D. Forecasting the Future Burden of Opioids for Osteoarthritis. Osteoarthr. Cartil. 2018, 26, 350–355. [Google Scholar] [CrossRef] [PubMed]
- Ethgen, O.; Beaudart, C.; Buckinx, F.; Bruyère, O.; Reginster, J.Y. The Future Prevalence of Sarcopenia in Europe: A Claim for Public Health Action. Calcif. Tissue Int. 2017, 100, 229–234. [Google Scholar] [CrossRef] [PubMed]
- Fang, E.F.; Xie, C.; Schenkel, J.A.; Wu, C.; Long, Q.; Cui, H.; Aman, Y.; Frank, J.; Liao, J.; Zou, H.; et al. A Research Agenda for Ageing in China in the 21st Century (2nd Edition): Focusing on Basic and Translational Research, Long-Term Care, Policy and Social Networks. Ageing Res. Rev. 2020, 64, 101174. [Google Scholar] [CrossRef] [PubMed]
- Ritter, P.L.; Dal Pai, D.; Belmonte-de-Abreu, P.; Camozzato, A. Trends in Elderly Psychiatric Admissions to the Brazilian Public Health Care System. Rev. Bras. Psiquiatr. 2016, 38, 314–317. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Yin, J.; Wu, C.; Wei, X.; Sun, Q. Antibiotic Expenditure by Public Healthcare Institutions in Shandong Province in China, 2012–2016. Front. Pharmacol. 2018, 9, 1396. [Google Scholar] [CrossRef] [PubMed]
- Gulis, G.; Aringazina, A.; Sangilbayeva, Z.; Zhan, K.; de Leeuw, E.; Allegrante, J.P. Population Health Status of the Republic of Kazakhstan: Trends and Implications for Public Health Policy. Int. J. Environ. Res. Public Health 2021, 18, 12235. [Google Scholar] [CrossRef]
- Bose, M.; Banerjee, S. Equity in Distribution of Public Subsidy for Noncommunicable Diseases among the Elderly in India: An Application of Benefit Incidence Analysis. BMC Public Health 2019, 19, 1735. [Google Scholar] [CrossRef]
- Manteaw, B.O. Sanitation Dilemmas and Africa’s Urban Futures: Foregrounding Environmental Public Health in Contemporary Urban Planning. Acad. J. Interdiscip. Stud. 2020, 9, 177–187. [Google Scholar] [CrossRef]
- Skott, M.; Durbeej, N.; Smitmanis-Lyle, M.; Hellner, C.; Allenius, E.; Salomonsson, S.; Lundgren, T.; Jayaram-Lindström, N.; Rozental, A. Patient-Controlled Admissions to Inpatient Care: A Twelve-Month Naturalistic Study of Patients with Schizophrenia Spectrum Diagnoses and the Effects on Admissions to and Days in Inpatient Care. BMC Health Serv. Res. 2021, 21, 598. [Google Scholar] [CrossRef] [PubMed]
- Dash, S.; Shakyawar, S.K.; Sharma, M.; Kaushik, S. Big Data in Healthcare: Management, Analysis and Future Prospects. J. Big Data 2019, 6, 54. [Google Scholar] [CrossRef]
- Leider, J.P.; Shah, G.H.; Williams, K.S.; Gupta, A.; Castrucci, B.C. Data, Staff, and Money: Leadership Reflections on the Future of Public Health Informatics. J. Public Health Manag. Pract. 2017, 23, 302–310. [Google Scholar] [CrossRef] [PubMed]
- Arora, V.S.; McKee, M.; Stuckler, D. Google Trends: Opportunities and Limitations in Health and Health Policy Research. Health Policy 2019, 123, 338–341. [Google Scholar] [CrossRef] [PubMed]
- Ajbar, A.; Shepherd, T.A.; Robinson, M.; Mallen, C.D.; Prior, J.A. Using Google Trends to Assess the Impact of Global Public Health Days on Online Health Information-Seeking Behaviour in Arabian Peninsula. J. Egypt. Public Health Assoc. 2021, 96, 4. [Google Scholar] [CrossRef] [PubMed]
- Thomason, J. Big Tech, Big Data and the New World of Digital Health. Glob. Health J. 2021, 5, 165–168. [Google Scholar] [CrossRef]
- Schuhmacher, A.; Gatto, A.; Kuss, M.; Gassmann, O.; Hinder, M. Big Techs and Startups in Pharmaceutical R&D—A 2020 Perspective on Artificial Intelligence. Drug Discov. Today 2021, 26, 2226–2231. [Google Scholar] [CrossRef]
| Database | Search String |
|---|---|
| SCOPUS | TITLE (“public health*” AND (“future*” OR “roadmap” OR “research avenue*” OR “research agenda” OR “trend*”) AND NOT “review”) AND (PUBYEAR > 2015) AND (LIMIT-TO (DOCTYPE, “ar”) OR LIMIT-TO (DOCTYPE, “cp”)) AND (LIMIT-TO (LANGUAGE, “English”)) |
| PubMed | (((“public health*”[Title] AND (“future*”[Title] OR “research avenue*”[Title] OR “research agenda”[Title] OR “trend*”[Title])) NOT “review”[Title]) AND 1 January 2015:31 December 3000 [Date - Publication] AND “english”[Language]) AND ((booksdocs[Filter] OR congress[Filter] OR editorial[Filter] OR historicalarticle[Filter] OR letter[Filter] OR news[Filter] OR researchsupportnonusgovt[Filter] OR researchsupportusgovtnon-phs[Filter] OR researchsupportusgovtphs[Filter] OR researchsupportusgovernment[Filter] OR review[Filter])) |
| Year | Event | Source |
|---|---|---|
| 2023 | Public expenditure projections reveal that by 2023, 83 out of 189 countries will face contractions in government spending compared to their 2010s average, thereby exposing a cumulative total of 2.3 billion people to the socio-economic consequences of budget cuts. | [27] |
| 2023 | Most high-income countries are expected to increase their spending compared to the 2010s. Over half of these countries will have higher government expenditures than pre-COVID averages. Eight countries are projected to experience moderate spending reductions, while the remaining 20 will face aggressive austerity measures. | [27] |
| 2023 | Increase in the number of kidney patients affected by the Hepatitis C Virus (HCV) in the US. | [28] |
| 2024 | A central objective of Mauritius’s current national health sector strategic plan for 2024 is to review health-financing strategies. | [29] |
| 2025 | Increase in the development of genomic medicine, offering a unique opportunity to study the ethical and social issues arising from integrating genomics into routine clinical care in the UK and France. | [30] |
| 2025 | As South Africa aims to fully implement National Health Insurance (NHI), and given the pressure on the health sector coupled with limited resources, it will be crucial to define priorities and service packages that address equity. | [31] |
| 2025 | In Japan, 30% of the population will be elderly. | [32] |
| 2025 | The World Health Organization estimates that approximately 300 million people currently have asthma worldwide, and with current trends rising, it is expected to reach 400 million. | [33] |
| 2025 | The TB strategy aims at adopting concrete preventive, diagnostic, and treatment measures to eliminate the disease. | [34] |
| 2025 | The surge in government spending due to the pandemic is anticipated to be gradually withdrawn, with countries reverting to their typical expenditure levels as seen in the 2010s. | [27] |
| 2025 | Improvments to the optimization process of imaging technologies to increase specificity will be made, thus offering a non-invasive approach to evaluate tumor phenotypes. | [35] |
| 2025 | The global prevalence of diabetes is to increase to 570.9 million. | [36] |
| 2025 | China will achieve its highest excess growth rate of 2% and increase its GDP% spent on health care from 5.4% in 2012 to 6.6% in 2025. | [37] |
| 2025 | The BRICS nations will continue to strive to improve universal and comprehensive health coverage in the upcoming year. | [38] |
| 2025 | The transdermal drug delivery (TDD) market is estimated to be worth approximately USD 95.57 billion. | [39] |
| 2027 | Many European countries will have rising health inequalities, causing a stall or slightly declining life expectancy. A public health perspective of healthy aging is to remain a priority for European public health in the years to come. | [40] |
| 2027 | Racial and ethnic composition and how these affect health and well-being is likely to be one of the critical challenges facing public health leaders in the coming decades in Europe. | [40] |
| 2030 | Cancer incidence is expected to increase by aproximately 45% when compared to 2020 numbers, making it the world’s leading cause of death. | [41] |
| 2030 | One of the US government’s Healthy People 2030 goals focuses on increasing disease monitoring and prevention efforts, and improving the global capacity to prevent, detect, and respond to public health threats. | [42] |
| 2030 | In Mauritius, the 2030 Agenda for Sustainable Development is committed to ensuring universal health coverage, where all individuals and communities, regardless of their circumstances, will receive the health services they need without the risk of suffering financial difficulties. | [29] |
| 2030 | Reducing tobacco consumption is essential to reducing noncommunicable diseases in the coming years. | [43] |
| 2030 | Health promotion is on the 2030 agenda as a priority goal for sustainable development in Shanghai. | [44] |
| 2030 | Results of the projection for 2030 show a significant increase in the costs of treating all “Type 2 diabetes mellitus (T2DM)” and related complications. Accounting for an estimated incidence rate of 55,000 new diabetes cases, the burden of T2DM is projected to cost the South African public healthcare system over USD 2.5 bn by 2030. | [31] |
| 2030 | The Sustainable Development Goal is to provide access by 2030 to safe, affordable, and sustainable transport systems for all. An autonomous vehicle policy can seek to address the needs of populations with reduced mobility through targeted subsidies and technical assistance, using transport to make cities inclusive for all. | [45] |
| 2030 | A challenge to progress towards “universal health coverage (UHC)” by 2030 is the decrease in OOP spending on pharmaceuticals from the private sector, as there is a general misperception that generic drugs in the public sector are below the norm. | [29] |
| 2030 | Indicators such as “noncommunicable diseases (NCDs)”, childhood obesity, the harmful use of alcohol, and mortality from self-harm and interpersonal violence, which suggest that more interventions are still needed to improve patient care in the public health system, are still below the target of 100%. | [38] |
| 2030 | SDG targets seek to realize a one-third reduction in premature mortality from NCDs to ensure healthy lives and promote well-being at all ages. | [45] |
| 2030 | The target is to reduce global maternal mortality to less than 70 per 100,000 live births, with no country having an MMR above 140 per 100,000 live births. | [46] |
| 2030 | It is predicted that 4.5 million South Africans in the public sector will have Type 2 diabetes. | [31] |
| 2030 | It is estimated that by 2030 > 70% of patients worldwide with end-stage renal disease will be in developing countries. | [47] |
| 2030 | The Association of American Medical Colleges projects a potential national shortage of up to 49,300 primary care physicians and 9600 medicine subspecialty physicians. | [48] |
| 2030 | The United States aims to reduce new HIV infections by 75% by 2025 and 90% by 2030. | [49] |
| 2030 | Countries seek to double the global energy efficiency improvement rate to mitigate and adapt to climate change. | [45] |
| 2030 | Ending the HIV Epidemic. | [49] |
| 2030 | Individuals aged 65 and older will constitute 20% of the US population. | [49] |
| 2030 | Singaporean seniors aged 65 and above are expected to reach one million. | [50] |
| 2030 | The elimination of malaria cases and deaths across Southeast Asia. | [51] |
| 2030 | NCDs will be the leading cause of morbidity and mortality, accounting for 80% of deaths worldwide. Cancer affected around 3.45 million Europeans in 2012 and caused 1.75 million deaths. The morbidity and mortality rates of these conditions and other chronic disorders are responsible for the significant burden on public healthcare system expenses. | [51] |
| 2030 | About 30,00 seniors will use Long-term Care Facilities (LTCF) or home care services in Singapore. | [50] |
| 2030 | An increase in the prevalence of Chronic Kidney Disease (CKD) stages 3a to “end-stage kidney disease” (ESKD) in the United States from 13.2% in 2010 to 16.7% in 2030. | [52] |
| 2030 | Tobacco control elements are prioritized in the UN 2030 Sustainable Development Agenda and Sustainable Development Goals. | [43] |
| 2030 | The cost of opioid prescriptions for osteoarthritis (OA) is expected to rise to USD 72.4M. The estimated cost per person will grow from USD 62.28 in 2015 to USD 128.68 in 2030. | [53] |
| 2035 | For the first time in the history of the United States, people 65 years and older will constitute a greater percentage of the total US population than those 18 years and younger. There will be an expected 78 million people 65 years and older compared with the 76.7 million of those who are younger than 18 years. | [49] |
| 2041 | Due to the substantial increase in the Chilean population with chronic kidney disease (CKD), the direct costs of treating CKD are expected to triple. | [52] |
| 2041 | The number of people with end-stage renal disease (ESKD), and thus the number of people in need of Renal Replacement Therapy (RRT), is projected to increase from 24,601 in 2021 to 83,885 in 2041. | [52] |
| 2045 | The number of individuals with sarcopenia is projected to increase from 19,740,527 in 2016 to 32,338,990. In 2016, the overall prevalence rate among the elderly was 20.2%, and in 2045 it is expected to be 22.3%. | [54] |
| 2045 | The proportion of women aged 65 years or older is estimated to increase by 31.4%, from 21.1% in 2016 to 30.0%. The proportion of men in the same age group is projected to increase by 37.0%, from 16.5% in 2016 to 25.2%. | [54] |
| 2050 | There are expected to be 1.4 billion Chinese people, with 365 million aged 65+, representing 26.1% of the country’s population. | [55] |
| 2050 | The Chinese population statistics taken between 1950 and 2050 show a reduction in the crude death rate and total fertility rate, accompanied by an increase in life expectancy at birth and an expansion of the population aged 65 and above. | [55] |
| 2050 | The number of people affected by dementia will reach 135.5 million. | [56] |
| 2050 | Dementia diagnoses will rise to 152 million by 2050. | [55] |
| 2050 | Without an effective strategy to control antimicrobial resistance (AMR), there will be approximately 10 million deaths each year and a cumulative USD 100 trillion economic burden caused by resistant infections. | [57] |
| 2050 | A full implementation of the network, anticipating that digital and mHealth technologies and other smart services will improve prevention, diagnosis, treatment, and management in rural areas in Kazakhstan. | [58] |
| 2050 | While the world population has surpassed 7 billion and is expected to continue to increase and reach around 10 billion by 2050, Europe is the only world region expected to experience a population decline by 2050. This decline in population growth is attributed to the low fertility rates experienced in most European countries. | [40] |
| 2050 | Nearly 25% of the population in Singapore would have CKD. | [52] |
| 2050 | The number of elderly people in India will surpass the population of children below 14 years. | [59] |
| 2050 | In India, the proportion of the population aged 60 years and above is projected to increase from 9% to 20%. | [59] |
| 2050 | Almost all areas except Africa will have nearly 25% of their people aged 60 or older. | [59] |
| 2050 | Over a quarter of the global oldest-old population will live in China. | [55] |
| 2050 | Current projections suggest that the population growth rate in African urban regions could swell from 395 million in 2010 to around 1.339 billion. | [60] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
El-Warrak, L.; Nunes, M.; Luna, G.; Barbosa, C.E.; Lyra, A.; Argôlo, M.; Lima, Y.; Salazar, H.; de Souza, J.M. Towards the Future of Public Health: Roadmapping Trends and Scenarios in the Post-COVID Healthcare Era. Healthcare 2023, 11, 3118. https://doi.org/10.3390/healthcare11243118
El-Warrak L, Nunes M, Luna G, Barbosa CE, Lyra A, Argôlo M, Lima Y, Salazar H, de Souza JM. Towards the Future of Public Health: Roadmapping Trends and Scenarios in the Post-COVID Healthcare Era. Healthcare. 2023; 11(24):3118. https://doi.org/10.3390/healthcare11243118
Chicago/Turabian StyleEl-Warrak, Leonardo, Mariano Nunes, Gabriel Luna, Carlos Eduardo Barbosa, Alan Lyra, Matheus Argôlo, Yuri Lima, Herbert Salazar, and Jano Moreira de Souza. 2023. "Towards the Future of Public Health: Roadmapping Trends and Scenarios in the Post-COVID Healthcare Era" Healthcare 11, no. 24: 3118. https://doi.org/10.3390/healthcare11243118
APA StyleEl-Warrak, L., Nunes, M., Luna, G., Barbosa, C. E., Lyra, A., Argôlo, M., Lima, Y., Salazar, H., & de Souza, J. M. (2023). Towards the Future of Public Health: Roadmapping Trends and Scenarios in the Post-COVID Healthcare Era. Healthcare, 11(24), 3118. https://doi.org/10.3390/healthcare11243118







