Mandibular Cortical Bone Evaluation in a Healthy Paediatric Population
Abstract
1. Introduction
2. Material and Methods
2.1. Sample Selection
- Patients with chronic diseases/conditions/treatments affecting bone, e.g., eating disorders, musculoskeletal disorders, etc.;
- Patients born prematurely or during early puberty;
- Patients undergoing/having undergone orthodontic treatment;
- Poor quality.
2.2. Sample Size
2.3. Study Procedure
2.4. Qualitative Bone Assessment (Mandibular Cortical Index, MCI)
2.5. Quantitative Bone Assessment (Mandibular Cortical Width, MCW)
- Antegonion—the deepest point of the antegonial notch concavity (A, H);
- The mesial cementoenamel junction of the first molar perpendicular to the mandibular base (B, G);
- The most superior cusp tip of the second premolar perpendicular to the mandibular base (C, F);
- The most superior cusp tip of the first premolar perpendicular to the mandibular base (D, E).
2.6. Statistical Analysis
3. Results
3.1. Demographic Characteristics
3.2. Observer Reliability
3.3. Qualitative Cortical Bone Assessment
3.4. Quantitative Cortical Bone Assessment
3.5. Correlation of Cortical Bone with Dental Status
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bachrach, L.K. Acquisition of optimal bone mass in childhood and adolescence. Trends Endocrinol. Metab. 2001, 12, 22–28. [Google Scholar] [CrossRef]
- Guerri, S.; Mercatelli, D.; Gómez, M.P.A.; Napoli, A.; Battista, G.; Guglielmi, G.; Bazzocchi, A. Quantitative imaging techniques for the assessment of osteoporosis and sarcopenia. Quant. Imaging Med. Surg. 2018, 8, 60–85. [Google Scholar] [CrossRef] [PubMed]
- International Atomic Energy Agency. Radiation Protection in Dental Radiology; Safety Reports Series No. 108; IAEA: Vienna, Austria, 2022. [Google Scholar]
- Taguchi, A.; Suei, Y.; Ohtsuka, M.; Otani, K.; Tanimoto, K.; Ohtaki, M. Usefulness of panoramic radiography in the diagnosis of postmenopausal osteoporosis in women. Width and morphology of inferior cortex of the mandible. Dentomaxillofac. Radiol. 1996, 25, 263–267. [Google Scholar] [CrossRef] [PubMed]
- Alonso, M.B.C.C.; Cortes, A.R.G.; Camargo, A.J.; Arita, E.S.; Haiter-Neto, F.; Watanabe, P.C.A. Assessment of Panoramic Radiomorphometric Indices of the Mandible in a Brazilian Population. ISRN Rheumatol. 2011, 2011, 854287. [Google Scholar] [CrossRef] [PubMed]
- Karayianni, K.; Horner, K.; Mitsea, A.; Berkas, L.; Mastoris, M.; Jacobs, R.; Lindh, C.; van der Stelt, P.F.; Harrison, E.; Adams, J.E.; et al. Accuracy in osteoporosis diagnosis of a combination of mandibular cortical width measurement on dental panoramic radiographs and a clinical risk index (OSIRIS): The OSTE-ODENT project. Bone 2007, 40, 223–229. [Google Scholar] [CrossRef]
- Paulsson-Björnsson, L.; Adams, J.; Bondemark, L.; Devlin, H.; Horner, K.; Lindh, C. The impact of premature birth on the mandibular cortical bone of children. Osteoporos. Int. 2014, 26, 637–644. [Google Scholar] [CrossRef] [PubMed]
- Apolinário, A.; Figueiredo, P.; Guimarães, A.; Acevedo, A.; Castro, L.; Paula, A.; Paula, L.; Melo, N.; Leite, A. Pamidronate Affects the Mandibular Cortex of Children with Osteogenesis Imperfecta. J. Dent. Res. 2015, 94 (Suppl. S3), 95S–102S. [Google Scholar] [CrossRef] [PubMed]
- Frascino, A.V.; Costa, C.; Salgado, D.M.R.A.; Coracin, F.L.; Fava, M.; Odone-Filho, V. Mandibular radiomorphometric assessment of bone mineral density in survivors of paediatric hematopoietic stem-cell transplantation. Clinics Sao Paulo 2019, 74, e929. [Google Scholar] [CrossRef] [PubMed]
- Seremidi, K.; Mitsea, A.; Papaioannou, W.; Petroleka, K.; Gizani, S. Correction: Assessing quality and quantity of cortical bone in childhood cancer survivors using anthropometric indices. Oral Radiol. 2023, 39, 821. [Google Scholar] [CrossRef]
- Yasa, Y.; Buyuk, S.K.; Genc, E. Comparison of mandibular cortical bone among obese, overweight, and normal weight adolescents using panoramic mandibular index and mental index. Clin. Oral Investig. 2020, 24, 2919–2924. [Google Scholar] [CrossRef]
- Gkastaris, K.; Goulis, D.G.; Potoupnis, M.; Anastasilakis, A.D.; Kapetanos, G. Obesity, osteoporosis and bone metabolism. J. Musculoskelet. Neuronal Interact. 2020, 20, 372–381. [Google Scholar] [PubMed]
- WMA. Declaration of Helsinki: Ethical Principles for Medical Research Involving Human Subjects. World Medical Association Fortaleza, Brazil Amendment. 2013. Available online: https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/ (accessed on 20 December 2018).
- Bartlett, J.E. Introduction to Power Analysis: A Guide to G*Power, Jamovi, and Superpower. 2022. Available online: https://osf.io/zqphw/ (accessed on 20 December 2018). [CrossRef]
- Madjarova, S.J.; Pareek, A.; Eckhardt, C.M.; Khorana, A.; Kunze, K.N.; Ollivier, M.; Karlsson, J.; Williams, R.J.; Nwachukwu, B.U. Fragility Part I: A guide to understanding statistical power. Knee Surg. Sports Traumatol. Arthrosc. 2022, 30, 3924–3928. [Google Scholar] [CrossRef] [PubMed]
- Serdar, C.C.; Cihan, M.; Yücel, D.; Serdar, M.A. Sample size, power and effect size revisited: Simplifed and practical ap-proaches in pre-clinical, clinical and laboratory studies. Biochem. Med. 2021, 31, 27–53. [Google Scholar] [CrossRef]
- Uttley, J. Power analysis, sample size, and assessment of statistical assumptions—Improving the evidential value of lighting research. Leukos 2019, 15, 143–162. [Google Scholar] [CrossRef]
- Klemetti, E.; Kolmakov, S.; Kröger, H. Pantomography in assessment of the osteoporosis risk group. Scand. J. Dent. Res. 1994, 102, 68–72. [Google Scholar] [CrossRef] [PubMed]
- Lindh, C.; Horner, K.; Jonasson, G.; Olsson, P.; Rohlin, M.; Jacobs, R.; Karayianni, K.; Van der Stelt, P.; Adams, J.; Marjanovic, E.; et al. The use of visual assessment of dental radiographs for identifying women at risk of having osteoporosis: The OS-TEODENT project. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2008, 106, 285–293. [Google Scholar] [CrossRef]
- Parfitt, A.; Travers, R.; Rauch, F.; Glorieux, F. Structural and cellular changes during bone growth in healthy children. Bone 2000, 27, 487–494. [Google Scholar] [CrossRef] [PubMed]
- Seeman, E. The structural and biomechanical basis of the gain and loss of bone strength in women and men. Endocrinol. Metab. Clin. N. Am. 2003, 32, 25–38. [Google Scholar] [CrossRef]
- Eimar, H.; Al-Saleh, M.; Cortes, A.; Gozal, D.; Graf, D.; Flores-Mir, C. Sleep-Disordered Breathing Is Associated with Reduced Mandibular Cortical Width in Children. JDR Clin. Transl. Res. 2019, 4, 58–67. [Google Scholar] [CrossRef]
- Mellion, Z.J.; Behrents, R.G.; Johnston, L.E. The pattern of facial skeletal growth and its relationship to various common indexes of maturation. Am. J. Orthod. Dentofac. Orthop. 2013, 143, 845–854. [Google Scholar] [CrossRef]
- Verma, D.; Peltomaki, T.; Jager, A. Reliability of growth prediction with hand-wrist radiographs. Eur. J. Orthod. 2009, 31, 438–442. [Google Scholar] [CrossRef]
- Zemel, B. Bone mineral accretion and its relationship to growth, sexual maturation and body composition during childhood and adolescence. World Rev. Nutr. Diet. 2013, 106, 39–45. [Google Scholar] [PubMed]
- Schoenau, E. Bone mass increase in puberty: What makes it happen? Horm. Res. 2006, 65 (Suppl. S2), 2–10. [Google Scholar] [CrossRef] [PubMed]
- Hernandez, R.A.M.; Ohtani, J.; Fujita, T.; Sunagawa, H.; Kawata, T.; Kaku, M.; Motokawa, M.; Tanne, K. Sex hormones receptors play a crucial role in the control of femoral and mandibular growth in newborn mice. Eur. J. Orthod. 2011, 33, 564–569. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Fujita, K.; Roforth, M.M.; Demaray, S.; McGregor, U.; Kirmani, S.; McCready, L.K.; Peterson, J.M.; Drake, M.T.; Monroe, D.G.; Khosla, S. Effects of Estrogen on Bone mRNA Levels of Sclerostin and Other Genes Relevant to Bone Metabolism in Postmenopausal Women. J. Clin. Endocrinol. Metab. 2014, 99, E81–E88. [Google Scholar] [CrossRef]
- Küchler, E.C.; de Lara, R.M.; Omori, M.A.; Marañón-Vásquez, G.; Baratto-Filho, F.; Nelson-Filho, P.; Stuani, M.B.S.; Blanck-Lubarsch, M.; Schroeder, A.; Proff, P.; et al. Effects of estrogen deficiency during puberty on maxillary and mandibular growth and associated gene expression—An μCT study on rats. Head Face Med. 2021, 17, 14. [Google Scholar] [CrossRef]
- Miranda, F.; Massaro, C.; Janson, G.; de Freitas, M.R.; Henriques, J.F.C.; Lauris, J.R.P.; Garib, D. Aging of the normal occlusion. Eur. J. Orthod. 2019, 41, 196–203. [Google Scholar] [CrossRef]
- Gunacar, D.N.; Erbek, S.M.; Aydınoglu, S.; Kose, T.E. Evaluation of the relationship between tooth decay and trabecular bone structure in paediatric patients using fractal analysis: A retrospective study. Eur. Oral Res. 2022, 56, 67–73. [Google Scholar]
- Bimstein, E. Frequency of alveolar bone loss adjacent to proximal caries in the primary molars and healing due to restoration of the teeth. Pediatr. Dent. 1992, 14, 30–33. [Google Scholar]
- Guealmann, M.; Matsson, L.; Bimstein, E. Periodontal health at first permanent molars adjacent to primary molar stainless steel crowns. J. Clin. Periodontol. 1983, 15, 531–533. [Google Scholar] [CrossRef]
- Sharaf, A.A.; Farsi, N.M. A clinical and radiographic evaluation of stainless steel crowns for primary molars. J. Dent. 2004, 32, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Bimstein, E.; Zaidenberg, R.; Soskolne, A.W. Alveolar bone loss and restorative dentistry in the primary molars. J. Clin. Pediatr. Dent. 1996, 21, 51–54. [Google Scholar]
- Protecting Patients in Dentistry|IAEA 2019. International Atomic Energy Agency. Vienna International Centre. Available online: https://www.iaea.org/newscenter/multimedia/videos/protecting-patients-in-dentistry (accessed on 28 November 2023).

| Stages | Right N (%) | Left N (%) | Total N (%) | |||
|---|---|---|---|---|---|---|
| Boys | Girls | Boys | Girls | Boys | Girls | |
| C1 | 276 (84.7) | 304 (91.0) | 265 (81.3) | 293 (87.7) | 250 (76.9) | 280 (84.1) |
| C2 | 49 (15.0) | 30 (9.0) | 60 (18.4) | 41 (12.3) | 74 (22.8) | 53 (15.9) |
| C3 | 1 (0.3) | 0 (0.0) | 1 (0.3) | 0 (0.0) | 1 (0.3) | 0 (0.0) |
| p-value 1 | 0.017 | 0.027 | 0.026 | |||
| Boys | Age Groups | |||||||
| 6–7 yrs | 8–9 yrs | 10–11 yrs | 12–13 yrs | 14–15 yrs | 16–17 yrs | 18 yrs | ||
| N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | ||
| Stages | C1 | 23 (63.9) | 64 (90.1) | 50 (92.6) | 45 (77.8) | 27 (55.1) | 31 (70.5) | 13 (76.5) |
| C2 | 13 (36.1) | 6 (8.5) | 4 (7.4) | 12 (22.2) | 22 (44.9) | 13 (29.5) | 4 (23.5) | |
| C3 | 0 (0.0) | 1 (1.4) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| p-value 1 < 0.001 | ||||||||
| Girls | Age Groups | |||||||
| 6–7 yrs | 8–9 yrs | 10–11 yrs | 12–13 yrs | 14–15 yrs | 16–17 yrs | 18 yrs | ||
| N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | ||
| Stages | C1 | 23 (71.0) | 60 (84.5) | 66 (85.7) | 48 (80.0) | 38 (92.7) | 30 (88.2) | 16 (84.2) |
| C2 | 9 (29.0) | 11 (15.5) | 11 (14.3) | 12 (20.0) | 3 (7.3) | 4 (11.8) | 3 (15.8) | |
| C3 | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| p-value 1 = 0.291 | ||||||||
| Bone Morphology n (%) | ||||
|---|---|---|---|---|
| Characteristics | C1 | C2 | Total | p-Value |
| Caries | ||||
| 0 | 476 (80.5) | 115 (19.5) | 591 | 0.074 1 |
| 1 | 18 (100.0) | 0 (0.0) | 18 | |
| 2 | 13 (81.3) | 3 (18.8) | 16 | |
| 3+ | 23 (71.9) | 9 (28.1) | 32 | |
| Composites | ||||
| 0 | 427 (82.0) | 94 (18.0) | 521 | |
| 1 | 32 (78.0) | 9 (22.0) | 41 | |
| 2 | 29 (74.4) | 10 (25.6) | 39 | 0.252 2 |
| 3 | 18 (85.7) | 3 (14.3) | 21 | |
| 4+ | 24 (68.6) | 11 (31.4) | 35 | |
| SCC | ||||
| 0 | 503 (80.5) | 122 (19.5) | 625 | 0.915 1 |
| 1 | 15 (88.2) | 2 (11.8) | 17 | |
| 2 | 8 (80.0) | 2 (20.0) | 10 | |
| 3 | 4 (80.0) | 1 (20.0) | 5 | |
| Missing teeth | ||||
| 0 | 477 (80.7) | 114 (19.3) | 591 | |
| 1 | 33 (89.2) | 4 (10.8) | 37 | |
| 2 | 15 (65.2) | 8 (34.8) | 23 | 0.194 1 |
| 3 | 3 (75.0) | 1 (25.0) | 4 | |
| 4 | 2 (100.0) | 0 (0.0) | 2 | |
| Dentition | ||||
| Early mixed | 166 (83.4) | 33 (16.6) | 199 | |
| Late mixed | 130 (84.4) | 24 (15.6) | 154 | 0.082 2 |
| Permanent | 234 (77.0) | 70 (23.0) | 304 | |
| Characteristics | Total Cortical Bone Thickness Mean | p-Value 1 |
|---|---|---|
| Caries | ||
| 0 | 3.6311 | |
| 1 | 3.0969 | 0.083 |
| 2 | 2.6996 | |
| 3+ | 3.0482 | |
| Composites | ||
| 0 | 3.5458 | |
| 1 | 3.3291 | |
| 2 | 3.8376 | 0.791 |
| 3 | 3.7524 | |
| 4+ | 3.7178 | |
| SCC | ||
| 0 | 3.5878 | |
| 1 | 2.7611 | |
| 2 | 3.7000 | 0.398 |
| 3 | 3.2364 | |
| Missing teeth | ||
| 0 | 3.5944 | |
| 1 | 3.2060 | |
| 2 | 3.6282 | 0.575 |
| 3 | 3.0624 | |
| 4 | 1.9198 | |
| Dentition | ||
| Early mixed | 3.2142 | |
| Late mixed | 3.4024 | <0.001 |
| Permanent | 3.8778 | |
| Bonferroni | ||
| Early–late mixed | 0.999 | |
| Early mixed–permanent | <0.001 | |
| Late mixed–permanent | 0.049 |
| Bone Quality | C1 | C2 | C3 | ||||
|---|---|---|---|---|---|---|---|
| Gender | Boys | Girls | Boys | Girls | Boys | Girls | |
| Age | |||||||
| 6 years | 76% | 71% | 24% | 29% | 0% | 0% | |
| 7 years | 65% | 75% | 35% | 25% | 0% | 0% | |
| 8 years | 59% | 69% | 41% | 31% | 0% | 0% | |
| 9 years | 84% | 75% | 16% | 25% | 0% | 0% | |
| 10 years | 82% | 90% | 18% | 10% | 0% | 0% | |
| 11 years | 88% | 94% | 8% | 6% | 4% | 0% | |
| 12 years | 91% | 91% | 9% | 9% | 0% | 0% | |
| 13 years | 86% | 85% | 14% | 15% | 0% | 0% | |
| 14 years | 88% | 84% | 12% | 16% | 0% | 0% | |
| 15 years | 77% | 50% | 23% | 50% | 0% | 0% | |
| 16 years | 76% | 88% | 24% | 12% | 0% | 0% | |
| 17 years | 65% | 89% | 35% | 11% | 0% | 0% | |
| 18 years | 94% | 77% | 6% | 24% | 0% | 0% | |
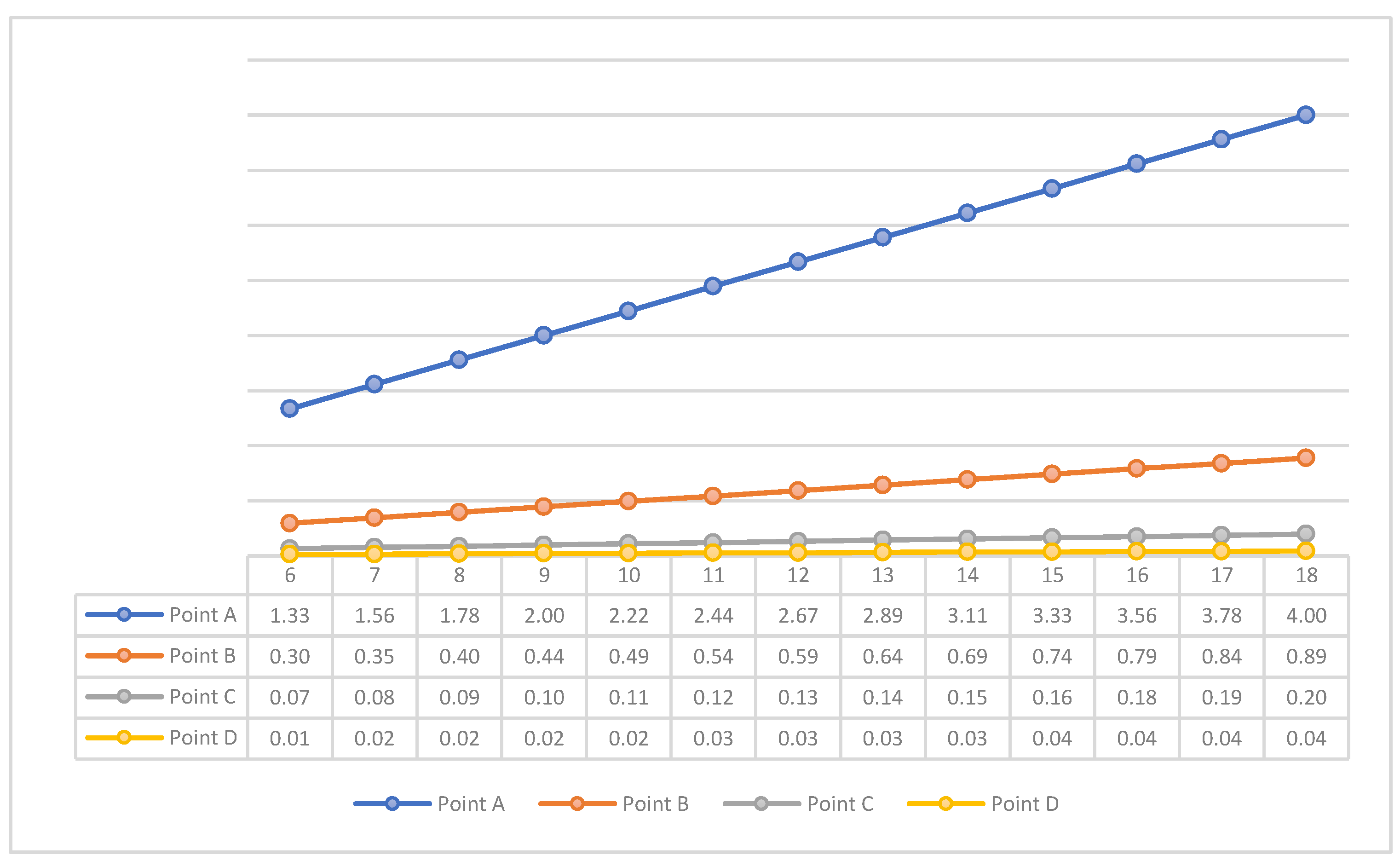
| Bone Quantity | Point A | Point B | Point C | Point D | Total | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Gender | Boys | Girls | Boys | Girls | Boys | Girls | Boys | Girls | Boys | Girls | |
| Age | |||||||||||
| 6 years | 2.02 | 2.16 | 3.49 | 4.04 | 3.62 | 4.13 | 3.84 | 4.40 | 3.42 | 3.91 | |
| 7 years | 3.51 | 2.38 | 4.20 | 3.20 | 4.29 | 3.18 | 4.84 | 3.49 | 4.31 | 3.16 | |
| 8 years | 3.22 | 2.84 | 4.16 | 2.84 | 4.51 | 3.93 | 4.78 | 4.42 | 3.13 | 2.00 | |
| 9 years | 3.16 | 2.82 | 3.84 | 3.51 | 4.13 | 3.58 | 4.60 | 4.24 | 2.27 | 2.02 | |
| 10 years | 2.93 | 2.76 | 3.96 | 3.51 | 4.09 | 3.53 | 4.44 | 3.87 | 2.20 | 1.96 | |
| 11 years | 3.04 | 2.84 | 3.58 | 3.53 | 3.58 | 3.44 | 3.82 | 3.64 | 2.00 | 1.93 | |
| 12 years | 3.20 | 2.60 | 3.91 | 3.33 | 3.87 | 3.36 | 4.13 | 3.58 | 2.27 | 1.84 | |
| 13 years | 2.82 | 2.42 | 3.44 | 3.20 | 3.62 | 3.00 | 4.02 | 3.16 | 2.00 | 1.69 | |
| 14 years | 2.78 | 2.20 | 3.40 | 2.80 | 3.53 | 2.73 | 3.51 | 2.96 | 1.89 | 1.53 | |
| 15 years | 2.36 | 3.58 | 2.91 | 4.51 | 2.84 | 4.58 | 2.78 | 4.71 | 1.56 | 2.49 | |
| 16 years | 3.18 | 2.56 | 4.11 | 3.47 | 4.16 | 3.71 | 4.27 | 3.87 | 2.24 | 1.96 | |
| 17 years | 2.36 | 3.20 | 3.07 | 4.64 | 3.16 | 4.76 | 3.18 | 4.82 | 1.69 | 2.49 | |
| 18 years | 3.87 | 3.62 | 5.31 | 4.58 | 5.11 | 4.62 | 5.20 | 4.76 | 2.78 | 2.76 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kotsanti, M.; Mitsea, A.; Christoloukas, N.; Seremidi, K.; Gizani, S. Mandibular Cortical Bone Evaluation in a Healthy Paediatric Population. Healthcare 2023, 11, 3105. https://doi.org/10.3390/healthcare11243105
Kotsanti M, Mitsea A, Christoloukas N, Seremidi K, Gizani S. Mandibular Cortical Bone Evaluation in a Healthy Paediatric Population. Healthcare. 2023; 11(24):3105. https://doi.org/10.3390/healthcare11243105
Chicago/Turabian StyleKotsanti, Marilena, Anastasia Mitsea, Nikolaos Christoloukas, Kyriaki Seremidi, and Sotiria Gizani. 2023. "Mandibular Cortical Bone Evaluation in a Healthy Paediatric Population" Healthcare 11, no. 24: 3105. https://doi.org/10.3390/healthcare11243105
APA StyleKotsanti, M., Mitsea, A., Christoloukas, N., Seremidi, K., & Gizani, S. (2023). Mandibular Cortical Bone Evaluation in a Healthy Paediatric Population. Healthcare, 11(24), 3105. https://doi.org/10.3390/healthcare11243105






