Self-Care Ability and Life Quality of Cured Leprosy Patients: The Mediating Effects of Social Support
Abstract
:1. Introduction
2. Methods
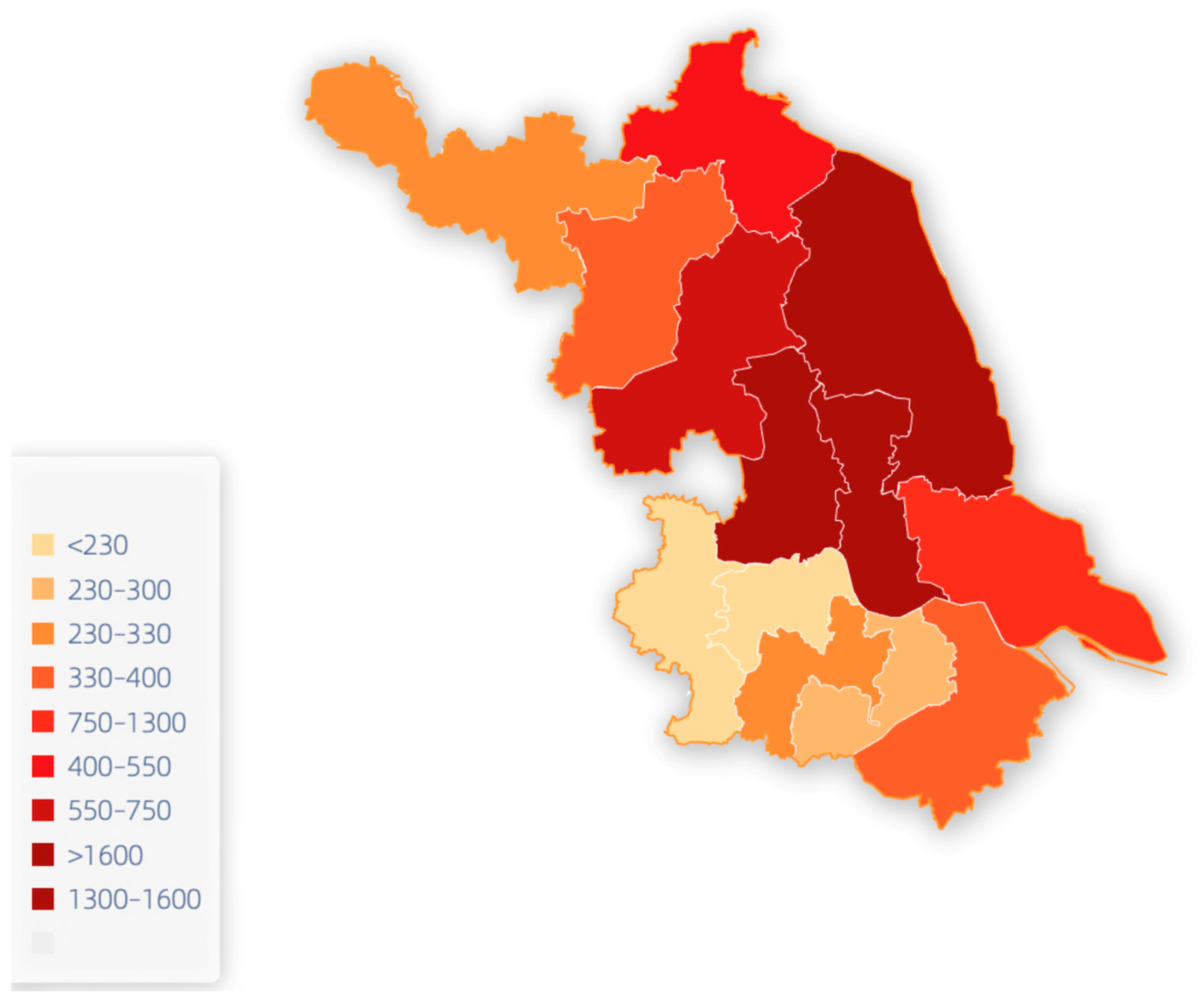
2.1. Research Context
2.2. Study Population
2.3. Recruitment Process
2.4. Study Tools
2.5. Data Collection Process
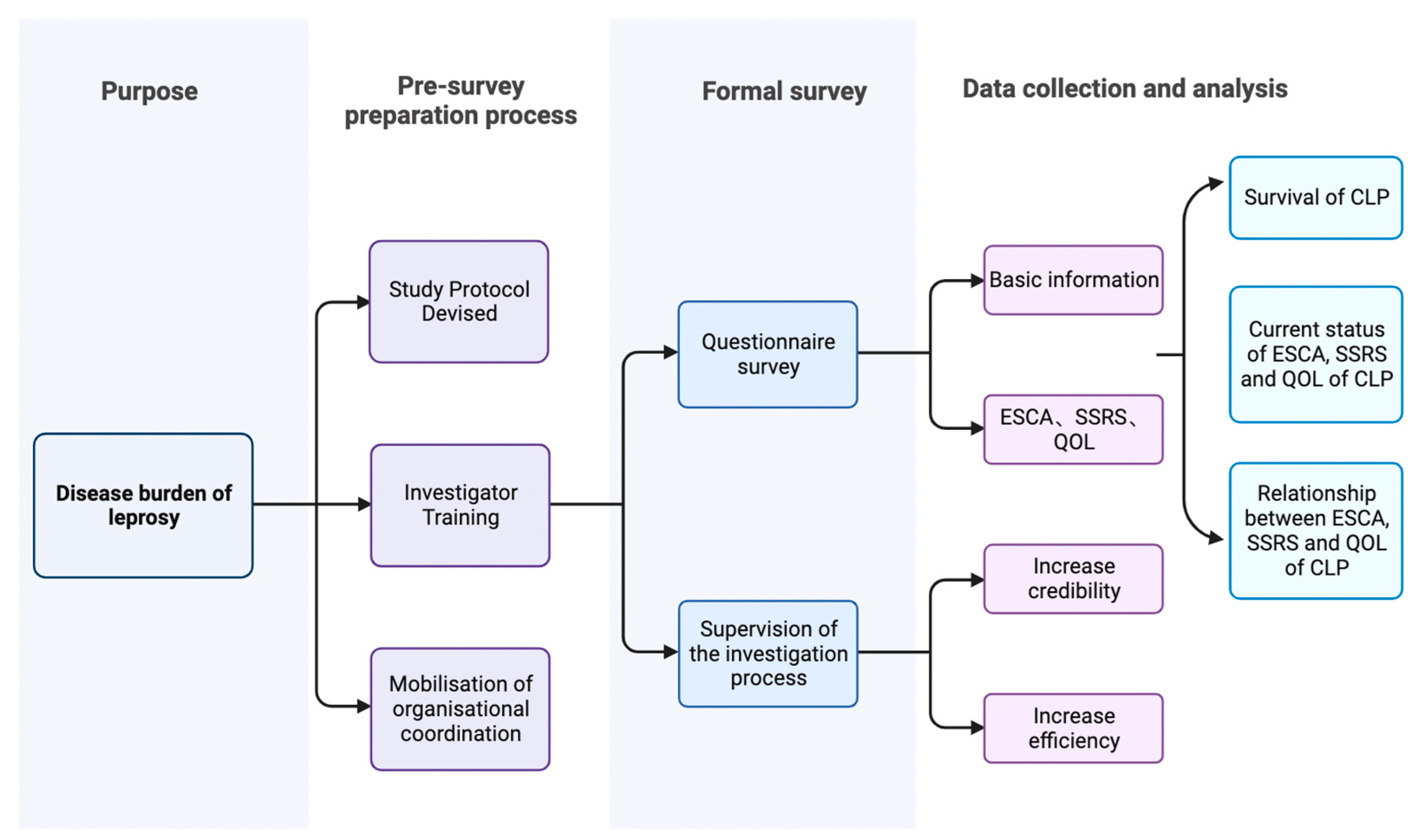
2.6. Survey Flow Chart
2.7. Statistical Methods
2.8. Ethics Approval
3. Results
3.1. Demographic Characteristics
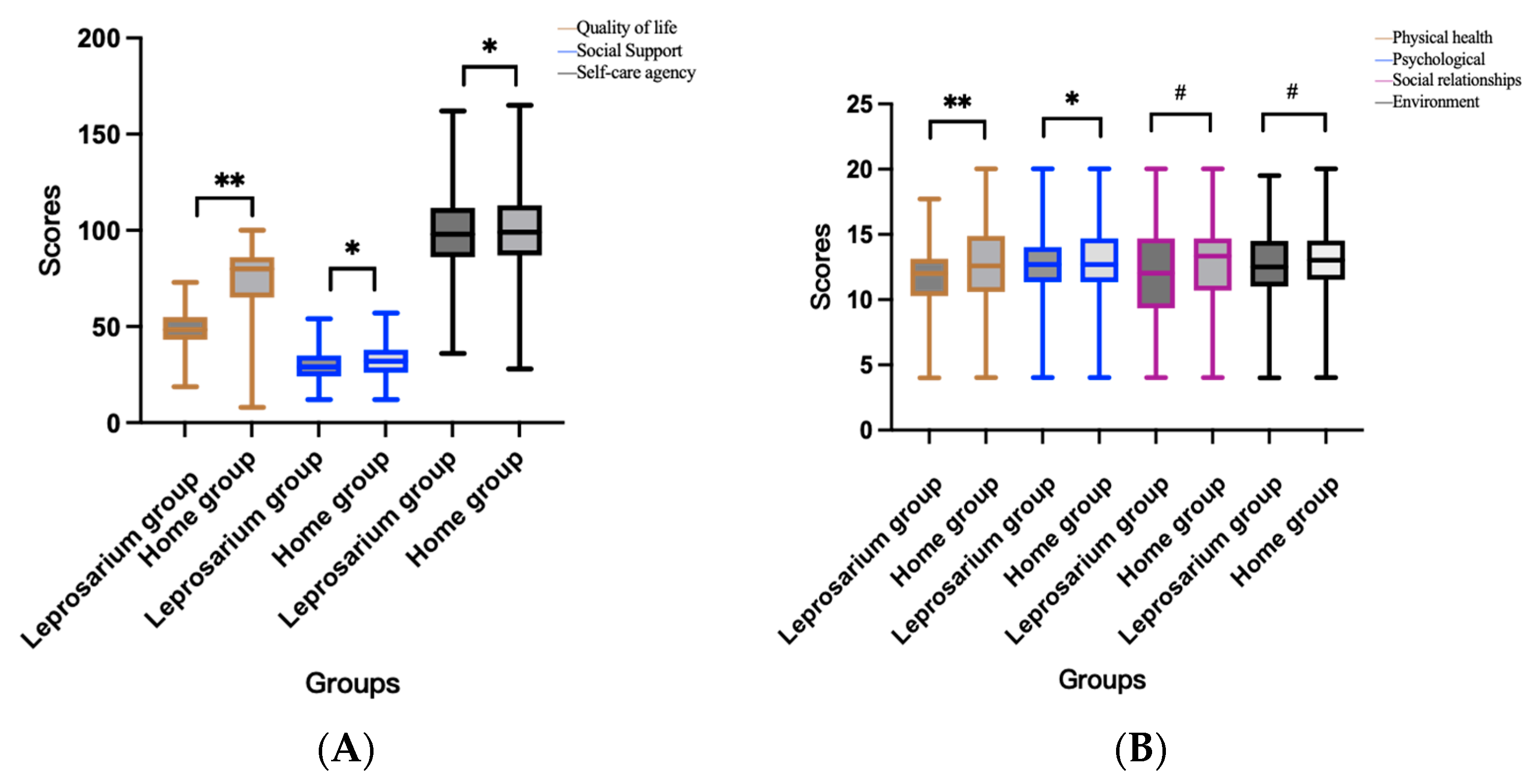
3.2. Scores on the CLP Scale
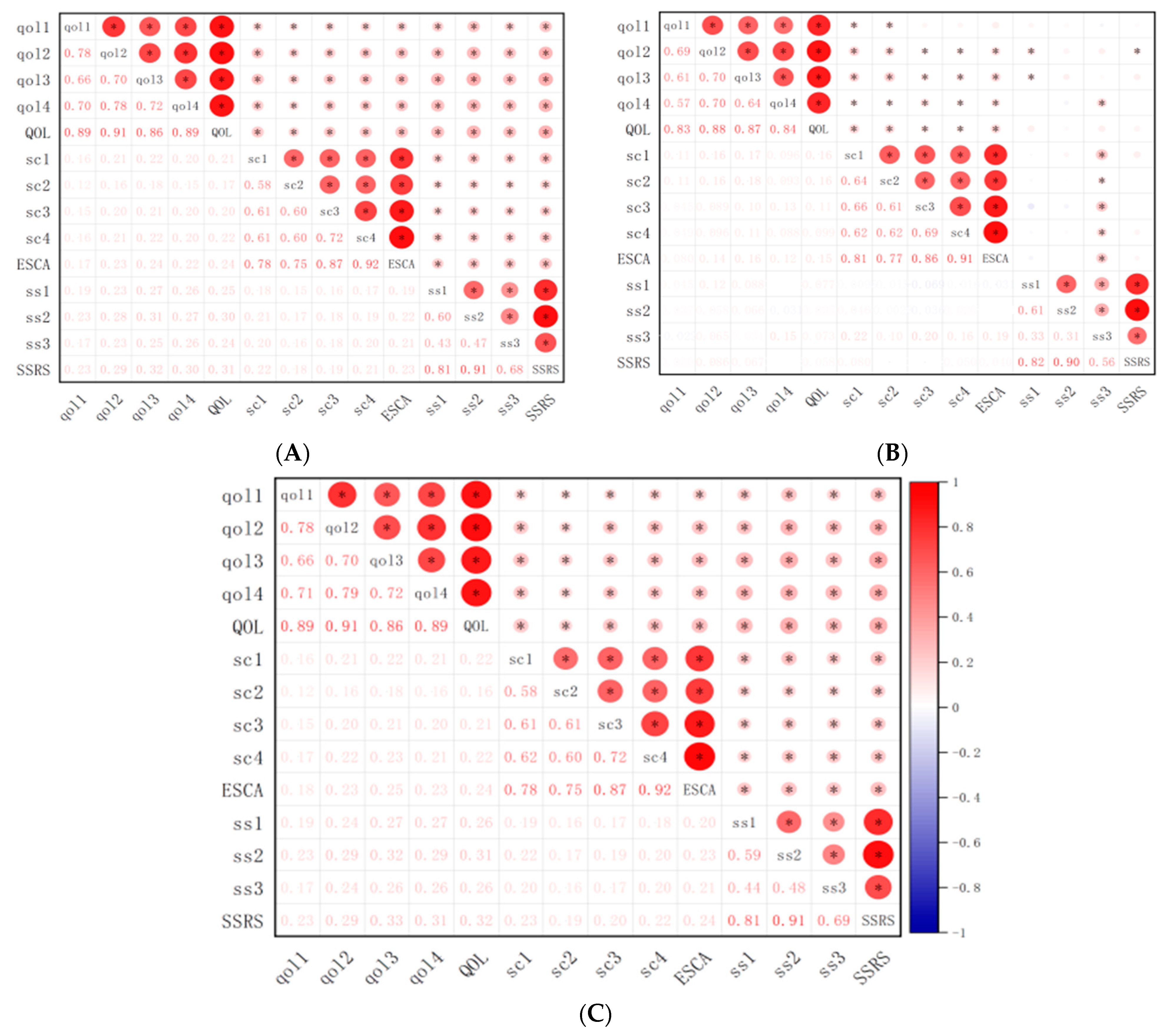
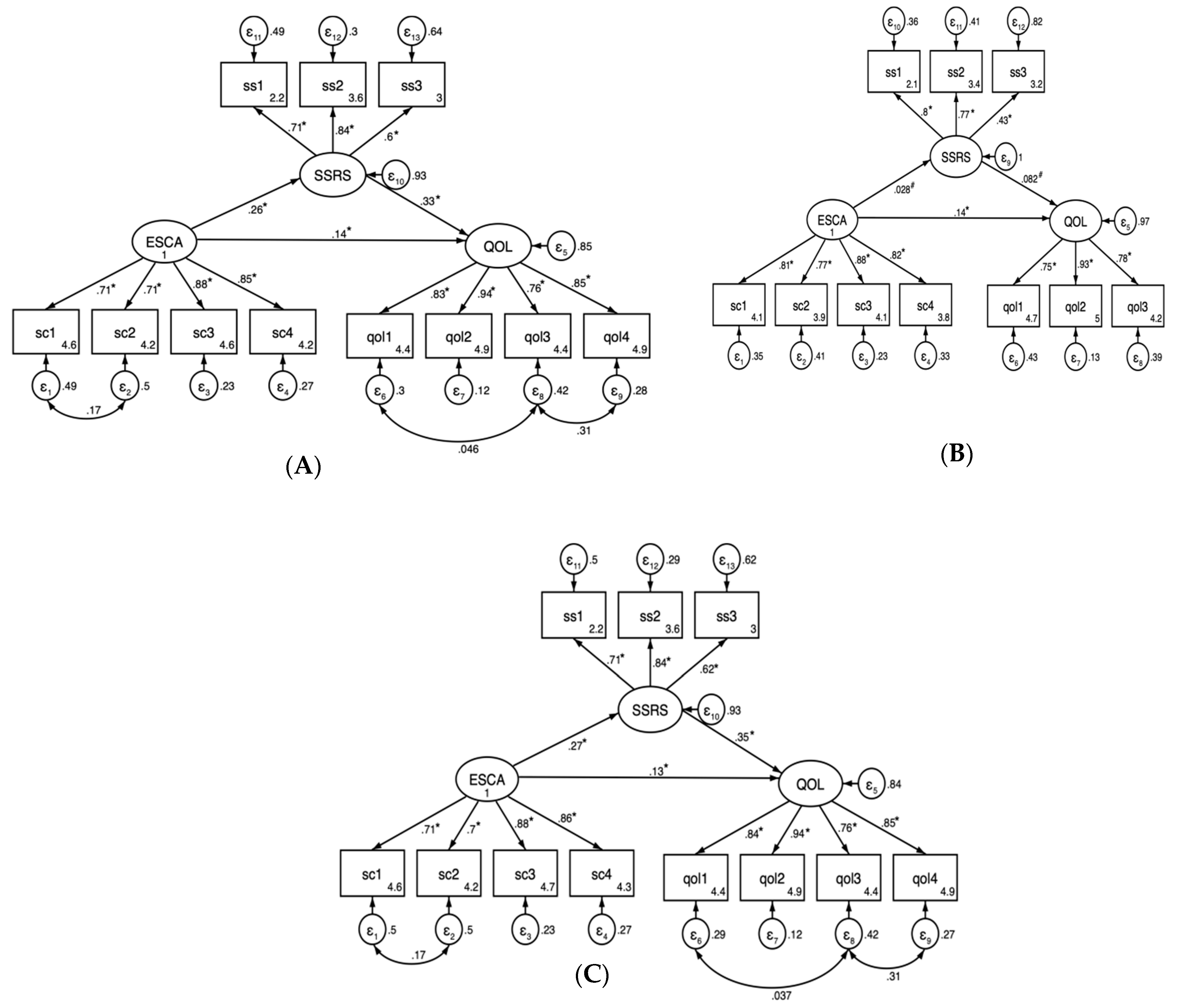
3.3. Structural Estimation Modeling Analysis
4. Discussion
5. Limitations and Prospects
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Britton, W.J.; Lockwood, D.N. Leprosy. Lancet 2004, 363, 1209–1219. [Google Scholar] [CrossRef] [PubMed]
- Hockings, K.J.; Mubemba, B.; Avanzi, C.; Pleh, K.; Düx, A.; Bersacola, E.; Bessa, J.; Ramon, M.; Metzger, S.; Patrono, L.V.; et al. Leprosy in wild chimpanzees. Nature 2021, 598, 652–656. [Google Scholar] [CrossRef]
- Santos, V.S.; Santos, L.C.; Lôbo, L.V.; Lemos, L.M.; Gurgel, R.Q.; Cuevas, L.E. Leprosy and disability in children younger than 15 years in an endemic area of northeast Brazil. Pediatr. Infect. Dis. J. 2015, 34, e44–e47. [Google Scholar] [CrossRef] [PubMed]
- de Paula, H.L.; de Souza, C.D.F.; Silva, S.R.; Martins-Filho, P.R.S.; Barreto, J.G.; Gurgel, R.Q.; Cuevas, L.E.; Santos, V.S. Risk Factors for Physical Disability in Patients with Leprosy: A Systematic Review and Meta-analysis. JAMA Dermatol. 2019, 155, 1120–1128. [Google Scholar] [CrossRef] [PubMed]
- Global Leprosy (Hansen Disease) Update, 2022: New Paradigm—Control to Elimination. Available online: https://www.who.int/publications/i/item/who-wer9837-409-430 (accessed on 14 September 2023).
- Richardus, J.H.; Nicholls, P.G.; Croft, R.P.; Withington, S.G.; Smith, W.C. Incidence of acute nerve function impairment and reactions in leprosy: A prospective cohort analysis after 5 years of follow-up. Int. J. Epidemiol. 2004, 33, 337–343. [Google Scholar] [CrossRef] [PubMed]
- Stolk, W.A.; Kulik, M.C.; le Rutte, E.A.; Jacobson, J.; Richardus, J.H.; de Vlas, S.J.; Houweling, T.A. Between-Country Inequalities in the Neglected Tropical Disease Burden in 1990 and 2010, with Projections for 2020. PLoS Negl. Trop. Dis. 2016, 10, e0004560. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Jin, G.; Yang, J.; Li, Y.; Wei, P.; Zhang, L. Epidemiological characteristics of leprosy during the period 2005–2020: A retrospective study based on the Chinese surveillance system. Front. Public Health 2023, 10, 991828. [Google Scholar] [CrossRef]
- Tabah, E.N.; Nsagha, D.S.; Bissek, A.Z.; Njamnshi, T.N.; Njih, I.N.; Pluschke, G.; Njamnshi, A.K. Community knowledge, perceptions and attitudes regarding leprosy in rural Cameroon: The case of Ekondotiti and Mbonge health districts in the south-west region. PLoS Negl. Trop. Dis. 2018, 12, e0006233. [Google Scholar] [CrossRef]
- Dako-Gyeke, M. Courtesy stigma: A concealed consternation among caregivers of people affected by leprosy. Soc. Sci. Med. 2018, 196, 190–196. [Google Scholar] [CrossRef]
- Liying, Y.; Meier, P.; Jingquan, W. Study on leprosy-related discrimination and knowledge in medical staff of leprosy control agency. Chin. Prev. Med. 2009, 10, 1098–1100. [Google Scholar]
- The WHOQOL Group. Development of the World Health Organization WHOQOL-BREF quality of life assessment. Psychol. Med. 1998, 28, 551–558. [Google Scholar] [CrossRef] [PubMed]
- Xiao, S. Theoretical basis and research application of the Social Support Rating Scale. J. Clin. Psychiatry 1994, 4, 98–100. [Google Scholar]
- Li, D. Reliability analysis of the Applied Social Support Rating Scale for firefighters. Chin. J. Health Psychol. 2017, 25, 1342–1345. [Google Scholar]
- Wang, H.H.; Laffrey, S.C. Preliminary development and testing of instruments to measure self-care agency and social support of women in Taiwan. Kaohsiung J. Med. Sci. 2000, 16, 459–467. [Google Scholar] [PubMed]
- Liu, Y.; Guo, Y. Correlation between health behaviors and self-care ability of community-based stroke patients. Chin. J. Nurs. 2011, 46, 279–281. [Google Scholar]
- Wang, C.; Yu, W.; Shui, T. Translation and validation of the Chinese-Cantonese version of the Exercise of Self-Care Ability Scale. Int. J. Nurs. Stud. 2012, 49, 1122–1137. [Google Scholar] [CrossRef]
- Deng, Q.; Wang, L.M.; Zhang, M. Quality of life and related influencing factors in Chinese adults. Zhonghua Liu Xing Bing Xue Za Zhi 2016, 37, 243–247. [Google Scholar]
- Chen, G. Optimizing the Terms of Mental Health Check About Adults in City of Our Country Study on the Degree of Social Support. J. Xi’an Inst. Phys. Educ. 2001, 1, 99–101. [Google Scholar]
- Kong, W.; Yan, L.; Shen, Y.; Fei, L.; Wu, L.; Xie, B. A survey on the health status and the influencing factors among the cured leprosy patients in Zhejiang province. Chin. J. Lepr. Ski. Dis. 2014, 30, 338–340. [Google Scholar]
- Martoreli Júnior, J.F.; Ramos, A.C.V.; Alves, J.D.; de Almeida Crispim, J.; Alves, L.S. Inequality of gender, age and disabilities due to leprosy and trends in a hyperendemic metropolis: Evidence from an eleven-year time series study in Central-West Brazil. PLoS Negl. Trop. Dis. 2021, 15, e0009941. [Google Scholar] [CrossRef]
- Zhang, L.; Zheng, S.; Jin, G. Epidemiological analysis on newly registered leprosy cases in Jiangsu Province from 1994 to 2013. Jiangsu Prev. Med. 2015, 26, 4–6. [Google Scholar]
- Wang, Y.; Xiao, D.; Wu, M.; Qing, L.; Yang, T.; Xiao, P.; Deng, D. Epidemiological Characteristics and Factors Associated with Cure of Leprosy in Chongqing, China, from 1949 to 2019. Am. J. Trop. Med. Hyg. 2022, 108, 165–173. [Google Scholar] [CrossRef]
- Hatzenbuehler, M.L.; Phelan, J.C.; Link, B.G. Stigma as a fundamental cause of population health inequalities. Am. J. Public Health 2013, 103, 813–821. [Google Scholar] [CrossRef]
- Zhao, X.; Lu, H. Survival status of leprosy convalescent in leprosy hospital village in Taizhou, Jiangsu Province. China Trop. Med. 2020, 20, 569–571. [Google Scholar]
- Wu, L.L.; Cheng, S.P.; Lee, N.S.; Chen, I.J. Activity of daily living and life quality of patients with Hansen’s disease in Taiwan. Hu Li Za Zhi Chin. 2010, 57, 57–69. [Google Scholar]
- Wei, C. A Study of Combined Chemotherapy on Accelerating the Return of Leprosy Patients to Society; Guangxi Zhuang Autonomous Region, Hezhou Dermatological Disease Control Hospital: Hezhou, China, 31 March 2016. [Google Scholar]
- Tsutsumi, A.; Izutsu, T.; Akramul Islam, M.D.; Amed, J.U.; Nakahara, S.; Takagi, F.; Wakai, S. Depressive status of leprosy patients in Bangladesh: Association with self-perception of stigma. Lepr. Rev. 2004, 75, 57–66, Erratum in Lepr. Rev. 2004, 75, 205. [Google Scholar] [CrossRef]
- Fei, L.; Shen, Y.; Wu, L.; Kong, W.; Xie, B. Survey on the survival status of leprosarium and home cuerd leprosy patients. Zhejiang Prev. Med. 2015, 27, 1029–1030, 1033. [Google Scholar]
- Chen, W.; Xiong, M.; Li, M.; Wang, X.; Yu, M.; Su, T.; Zheng, D.; Yang, B. Status of social support, self care and quality of life among leprosyconvalescents. South China Prev. Med. 2017, 43, 327–331. [Google Scholar]
- Wu, L.; Shen, Y.; Yu, M. Current status of self-care research for leprosy patients in China. Zhejiang Prev. Med. 2015, 27, 477–479, 485. [Google Scholar]
- Deps, P.; Cruz, A. Why we should stop using the word leprosy. Lancet Infect. Dis. 2020, 20, e75–e78. [Google Scholar] [CrossRef]
- Sarode, G.; Sarode, S.; Anand, R.; Patil, S.; Jafer, M.; Baeshen, H.; Awan, K.H. Epidemiological aspects of leprosy. Disease-a-Month 2020, 66, 100899. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.; Ye, Q.; Xu, K.; Sun, P. Analysis of the current status and influencing factors of anxiety and depression in leprosy patients. Nurs. Res. 2022, 36, 2239–2242. [Google Scholar]
- Heijnders, M.; Van Der Meij, S. The fight against stigma: An overview of stigma-reduction strategies and interventions. Psychol. Health Med. 2006, 11, 353–363. [Google Scholar] [CrossRef]
| Leprosarium Group N (%) | Home Group N (%) | χ2 | p | |
|---|---|---|---|---|
| Sex | ||||
| Male | 409 (73.04) | 5936 (68.35) | 5.37 | 0.02 |
| Female | 151 (26.96) | 2749 (31.65) | ||
| Age | ||||
| <40 | 1 (0.18) | 25 (0.29) | 0.58 | 0.90 |
| 40–60 | 35 (6.25) | 490 (5.64) | ||
| 60–80 | 367 (65.54) | 5712 (65.77) | ||
| ≥80 | 157 (28.04) | 2458 (28.30) | ||
| Marriage | ||||
| Single | 374 (66.79) | 948 (10.92) | 916.741 | <0.001 |
| Married | 119 (21.25) | 5687 (65.48) | ||
| Divorced | 16 (2.86) | 127 (1.46) | ||
| Widowed | 50 (8.93) | 1907 (21.96) | ||
| Separated | 1 (0.18) | 16 (0.18) | ||
| Education level | ||||
| Illiterate | 429 (76.61) | 4237 (48.79) | 164.767 | <0.001 |
| Primary school | 108 (19.29) | 3334 (38.39) | ||
| High school/above | 23 (4.11) | 1114 (12.83) | ||
| Occupation | ||||
| Farmers | 512 (91.43) | 8274 (95.27) | 23.085 | <0.001 |
| Fishermen | 0 (0.00) | 40 (0.46) | ||
| Other | 48 (8.57) | 371 (4.27) | ||
| Account | ||||
| Agricultural | 515 (91.96) | 8128 (93.59) | 2.275 | 0.132 |
| Non-agricultural | 45 (8.04) | 557 (6.41) | ||
| Living capacity | ||||
| Fully self-care | 75 (13.39) | 4970 (57.23) | 769.335 | <0.001 |
| Partially self-care | 290 (51.79) | 3184 (36.66) | ||
| Not self-care | 195 (34.82) | 531 (6.11) | ||
| Work capacity | ||||
| Total loss | 287 (51.25) | 1349 (15.53) | 556.49 | <0.001 |
| Partial loss | 243 (43.39) | 3695 (42.54) | ||
| No loss | 30 (5.36) | 3641 (41.92) | ||
| Deformity | ||||
| No | 58 (10.36) | 4893 (56.34) | 447.171 | <0.001 |
| Yes | 502 (89.64) | 3792 (43.66) | ||
| Living expenses | ||||
| No | 384 (68.57) | 7800 (89.81) | 233.58 | <0.001 |
| Yes | 176 (31.43) | 885 (10.19) | ||
| Insurance | ||||
| No | 405 (72.32) | 8087 (93.11) | 304.018 | <0.001 |
| Yes | 155 (27.68) | 598 (6.89) |
| Domain | CLP (Mean ± SD) | General Population (Mean ± SD) | t | p |
|---|---|---|---|---|
| Physical health * | 12.69 ± 2.90 | 15.10 ± 2.30 | −27.43 | 0.000 |
| Psychological * | 12.17 ± 2.60 | 13.89 ± 1.89 | −23.56 | 0.000 |
| Social relationships * | 12.85 ± 2.92 | 13.93 ± 2.06 | −13.52 | 0.000 |
| Environment * | 12.86 ± 2.61 | 12.14 ± 2.08 | 9.07 | 0.000 |
| Subjective support # | 17.71 ± 4.92 | 23.34 ± 4.28 | −49.61 | 0.000 |
| Objective support # | 7.02 ± 3.18 | 8.94 ± 2.83 | −25.70 | 0.000 |
| Support utilization # | 6.98 ± 2.32 | 7.99 ± 1.81 | −20.54 | 0.000 |
| Variables | Leprosarium Group (Mean ± SD) | Home Group (Mean ± SD) | Statistics | p |
|---|---|---|---|---|
| Quality of life | 48.99 ± 9.04 | 51.39 ± 9.89 | 9.61 | <0.01 |
| Physical health | 11.66 ± 2.47 | 12.76 ± 2.91 | 29.36 | <0.01 |
| 1. Pain and discomfort | 3.09 ± 0.97 | 2.69 ± 1.07 | 48.93 | <0.01 |
| 2. Dependence on medicinal substances and medical aids | 2.96 ± 1.00 | 2.50 ± 1.08 | 47.548 | <0.01 |
| 3. Energy and fatigue | 2.75 ± 0.79 | 2.94 ± 0.91 | 0.881 | 0.348 |
| 4. Mobility | 2.76 ± 0.96 | 3.08 ± 1.02 | 0.251 | 0.617 |
| 5. Sleep and rest | 3.12 ± 0.86 | 3.25 ± 0.90 | 17.926 | <0.01 |
| 6. Activities of daily living | 3.02 ± 0.89 | 3.19 ± 0.94 | 28.569 | <0.01 |
| 7. Work capacity | 2.83 ± 0.97 | 3.04 ± 0.98 | 0.339 | 0.56 |
| Psychological | 12.44 ± 2.51 | 12.87 ± 2.61 | 4.158 | 0.041 |
| 1. Self-esteem | 3.01 ± 0.86 | 3.05 ± 0.85 | 5.359 | 0.021 |
| 2. Positive feelings | 3.03 ± 0.84 | 3.09 ± 0.80 | 0.354 | 0.552 |
| 3. Thinking, learning, memory, and concentration | 3.01 ± 0.76 | 3.07 ± 0.81 | 13.078 | <0.01 |
| 4. Bodily image and appearance | 2.88 ± 0.93 | 3.13 ± 0.98 | 4.383 | 0.036 |
| 5. Spirituality/religion/personal beliefs | 3.12 ± 0.92 | 3.26 ± 0.93 | 11.98 | <0.01 |
| 6. Negative feelings | 2.37 ± 0.94 | 2.30 ± 0.95 | 0.001 | 0.977 |
| Social relationships | 12.10 ± 2.87 | 12.90 ± 2.92 | 2.767 | 0.096 |
| 1. Personal relationships | 3.32 ± 0.85 | 3.44 ± 0.85 | 0.493 | 0.483 |
| 2. Sexual activity | 2.57 ± 1.01 | 2.92 ± 0.96 | 24.093 | <0.01 |
| 3. Social support | 3.21 ± 0.81 | 3.34 ± 0.83 | 15.249 | <0.01 |
| Environment | 12.79 ± 2.62 | 12.86 ± 2.61 | 0.358 | 0.549 |
| 1. Freedom, physical safety, and security | 3.34 ± 0.84 | 3.32 ± 0.81 | 0.627 | 0.429 |
| 2. Home environment | 3.34 ± 0.86 | 3.28 ± 0.81 | 2.087 | 0.149 |
| 3. Financial resources | 2.85 ± 0.86 | 2.89 ± 0.97 | 7.082 | <0.01 |
| 4. Opportunities for acquiring new information and skills | 2.91 ± 0.85 | 2.95 ± 0.88 | 0.185 | 0.668 |
| 5. Participation in and opportunities for recreation/leisure activity | 2.82 ± 0.98 | 2.83 ± 1.00 | 1.574 | 0.21 |
| 6. Physical environment (pollution/noise/traffic/climate) | 3.56 ± 0.93 | 3.48 ± 0.87 | 2.065 | 0.151 |
| 7. Health- and social care: accessibility and quality | 3.60 ± 0.86 | 3.65 ± 0.82 | 6.856 | <0.01 |
| 8. Transport | 3.18 ± 0.98 | 3.35 ± 0.93 | 0.087 | 0.769 |
| Social Support | 29.31 ± 8.02 | 31.87 ± 8.76 | 5.81 | 0.016 |
| Subjective support | 16.09 ± 4.68 | 17.81 ± 4.91 | 3.115 | 0.078 |
| Objective support | 6.18 ± 3.00 | 7.07 ± 3.19 | 3.622 | 0.057 |
| Support utilization | 7.03 ± 2.21 | 6.98 ± 2.33 | 1.903 | 0.168 |
| Self-care agency | 98.75 ± 21.90 | 100.95 ± 19.75 | 4.577 | 0.032 |
| Self-concept | 18.74 ± 4.62 | 19.01 ± 4.09 | 18.995 | <0.01 |
| Self-responsibility | 13.60 ± 3.45 | 13.83 ± 3.27 | 3.334 | 0.068 |
| Self-care skills | 27.47 ± 6.72 | 27.97 ± 5.97 | 10.597 | <0.01 |
| Level of health literacy | 38.94 ± 10.16 | 40.15 ± 9.41 | 2.446 | 0.118 |
| Group | Index | x2/df | SREM | RMSEA | GFI | AGFI | TLI | CFI |
|---|---|---|---|---|---|---|---|---|
| Criteria | <4 | <0.1 | <0.08 | >0.90 | >0.90 | >0.90 | >0.90 | |
| Total | Initial Model | 33.9 | 0.029 | 0.060 | 0.971 | 0.954 | 0.967 | 0.976 |
| Modified model | 3.55 | 0.02 | 0.043 | 0.987 | 0.977 | 0.988 | 0.992 | |
| Leprosarium group | Initial Model | 4.52 | 0.031 | 0.079 | 0.944 | 0.910 | 0.936 | 0.952 |
| Modified model | 3.04 | 0.055 | 0.060 | 0.967 | 0.942 | 0.963 | 0.974 | |
| Home group | Initial Model | 33.54 | 0.03 | 0.061 | 0.969 | 0.951 | 0.966 | 0.975 |
| Modified model | 3.67 | 0.032 | 0.046 | 0.985 | 0.973 | 0.981 | 0.987 |
| Group | Relationship | β (95%CI) | σ | Z | p |
|---|---|---|---|---|---|
| Total | ESCA→SSRS | 0.26 (0.23, 0.28) | 0.01 | 21.81 | <0.01 |
| ESCA→QOL | 0.14 (0.11, 0.16) | 0.01 | 12.16 | <0.01 | |
| SSRS→QOL | 0.33 (0.31, 0.35) | 0.01 | 29.2 | <0.01 | |
| The mediating role of SSRS in ESCA and QOL | 0.07 | <0.01 | |||
| Leprosarium group | ESCA→QOL | 0.14 (0.04, 0.22) | 0.05 | 2.84 | <0.01 |
| Home group | ESCA→SSRS | 0.27 (0.24, 0.29) | 0.01 | 22.57 | <0.01 |
| ESCA→QOL | 0.13 (0.11, 0.16) | 0.01 | 11.67 | <0.01 | |
| SSRS→QOL | 0.35 (0.32, 0.37) | 0.01 | 32.07 | <0.01 | |
| The mediating role of SSRS in ESCA and QOL | 0.08 | <0.01 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Xu, L.; Jin, G.; Li, X.; Shao, Y.; Li, Y.; Zhang, L. Self-Care Ability and Life Quality of Cured Leprosy Patients: The Mediating Effects of Social Support. Healthcare 2023, 11, 3059. https://doi.org/10.3390/healthcare11233059
Xu L, Jin G, Li X, Shao Y, Li Y, Zhang L. Self-Care Ability and Life Quality of Cured Leprosy Patients: The Mediating Effects of Social Support. Healthcare. 2023; 11(23):3059. https://doi.org/10.3390/healthcare11233059
Chicago/Turabian StyleXu, Li, Guangjie Jin, Xiang Li, Yuting Shao, Yunhui Li, and Lianhua Zhang. 2023. "Self-Care Ability and Life Quality of Cured Leprosy Patients: The Mediating Effects of Social Support" Healthcare 11, no. 23: 3059. https://doi.org/10.3390/healthcare11233059
APA StyleXu, L., Jin, G., Li, X., Shao, Y., Li, Y., & Zhang, L. (2023). Self-Care Ability and Life Quality of Cured Leprosy Patients: The Mediating Effects of Social Support. Healthcare, 11(23), 3059. https://doi.org/10.3390/healthcare11233059







