Improving Antimicrobial Stewardship Program Using the Lean Six Sigma Methodology: A Descriptive Study from Mediclinic Welcare Hospital in Dubai, the UAE
Abstract
:1. Introduction
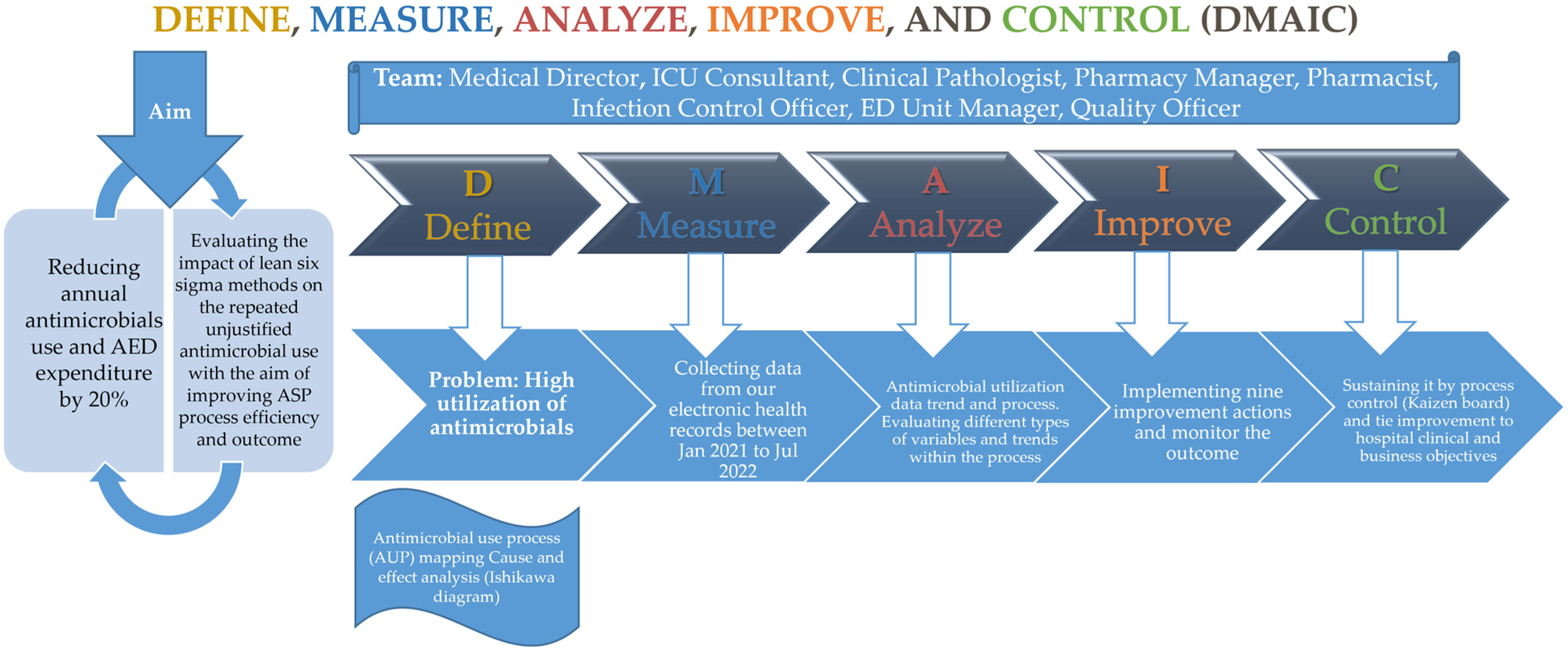
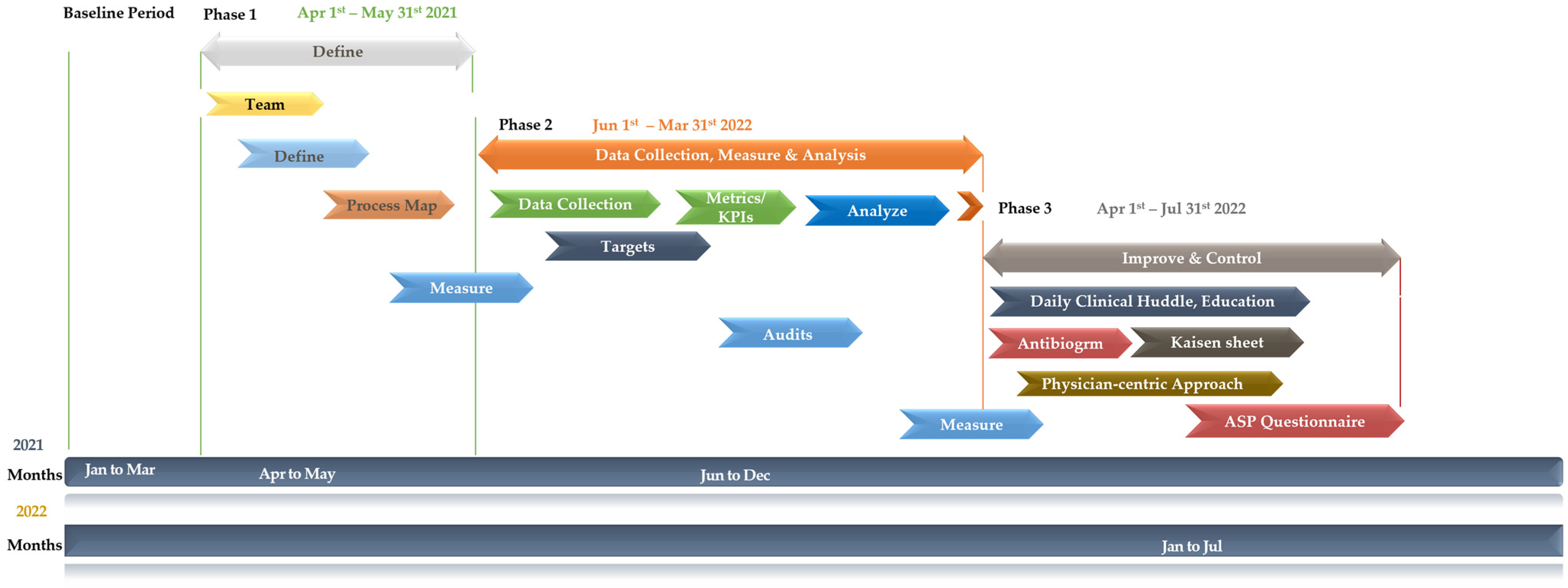
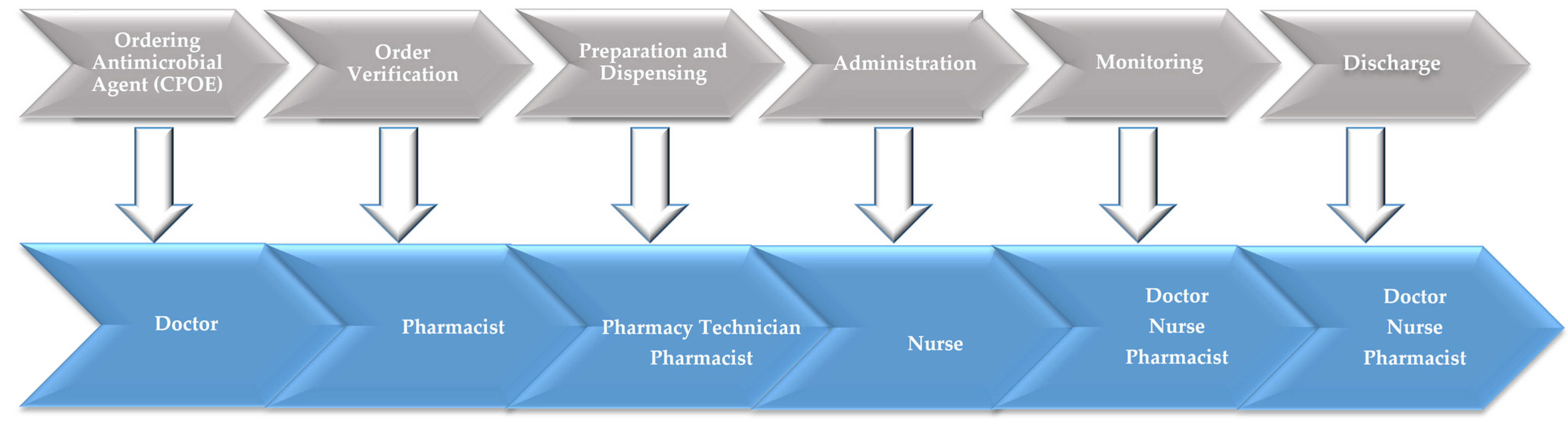
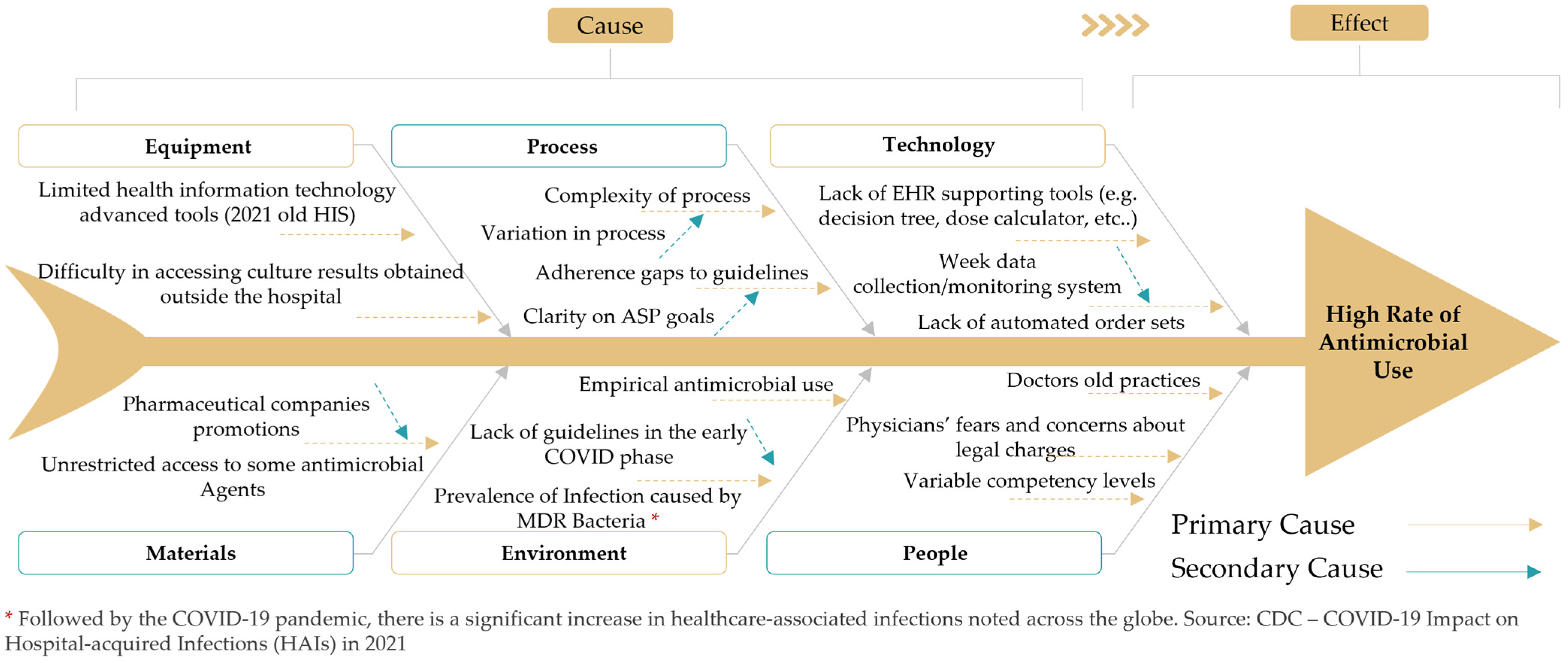
2. Materials and Methods
2.1. Study Setting and Design
2.2. Ethics Statement
2.3. Descriptive Analysis of the Nine ASP Interventions
- Leadership support: descriptive assessment of the involvement of leadership personnel to advocate prudent antimicrobial use practices.
- Guidelines for antimicrobial use: descriptive assessment of the guidelines established to outline proper and prudent antimicrobial drug usage.
- Formulary restriction with prior authorization: assessment of the imposed restrictions on the availability of specific antimicrobials through formulary control, requiring prior authorization for prescription.
- Utilization audits: descriptive assessment of antimicrobial prescribing patterns and practices.
- Utilization of local antibiogram and adherence to culture and susceptibility results: descriptive assessment of local antibiograms and adherence to culture and susceptibility data to guide antimicrobial selection.
- Conversion from IV to PO antimicrobials: assessment following the patients transitioning from IV to PO antimicrobial administration when clinically appropriate.
- Assessment of antimicrobial use (selection, dosage, route, and duration): assessed through evaluation of antimicrobial therapy, considering appropriateness in terms of drug selection, dosage, route of administration, and duration of treatment.
- Feedback/education: assessment of the constructive feedback and educational resources provided for healthcare practitioners to enhance their understanding of optimal antimicrobial prescribing practices.
- Proper cleaning and hand hygiene: assessment of effective cleaning practices and proper hand hygiene adherence.
2.4. Assessment of the CTQs
2.5. Data Analysis
3. Results
3.1. Description of the Study Phases
3.2. Descriptive Assessment of ASP Interventions over the Intervention Phases
3.3. Critical-to-Quality Improvement following Interventions
4. Discussion
4.1. Study Strengths and Recommendations Based on the Study Findings
4.2. Study Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AED | The United Arab Emirates Dirham |
| AMR | Antimicrobial resistance |
| ASP | Antimicrobial stewardship program |
| AUP | Antimicrobial use process |
| CDC | The Centers for Disease Control and Prevention |
| CHG | Chlorhexidine gluconate |
| CTQ | Critical-to-quality |
| DDD | Defined daily dose |
| DMAIC | Define, Measure, Analyze, Improve, Control |
| ED | Emergency department |
| ESBL | Extended spectrum beta-lactamase |
| ICU | Intensive care unit |
| ID | Infectious disease |
| IV | Intravenous |
| JCI | Joint Commission International |
| KPI | Key performance indicator |
| K-W | Kruskal–Wallis |
| LBL | Linear-by-linear test for association |
| LSS | Lean Six Sigma |
| MDR | Multidrug resistant |
| MRSA | Methicillin-resistant Staphylococcus aureus |
| M-W | Mann–Whitney U test |
| MWEL | Mediclinic Welcare Hospital |
| PO | Oral |
| UAE | The United Arab Emirates |
| VRE | Vancomycin-resistant Enterococcus |
References
- UAE Vision 2021 National Agenda. World-Class Healthcare. Available online: https://www.vision2021.ae/en/national-agenda-2021/list/world-class-circle (accessed on 25 July 2023).
- Rotteau, L.; Goldman, J.; Shojania, K.; Vogus, T.; Christianson, M.; Baker, G.; Rowland, P.; Coffey, M. Striving for high reliability in healthcare: A qualitative study of the implementation of a hospital safety programme. BMJ Qual. Saf. 2022, 31, 867–877. [Google Scholar] [CrossRef] [PubMed]
- Zimmermann, G.; Siqueira, L.; Bohomol, E. Lean Six Sigma methodology application in health care settings: An integrative review. Rev. Bras. De Enferm. 2020, 73, e20190861. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, S.; Hawarna, S.; Alqasmi, I.; Mohiuddin, M.; Rahman, M.; Mehrab Ashrafi, D. Role of Lean Six Sigma approach for enhancing the patient safety and quality improvement in the hospitals. Int. J. Healthc. Manag. 2022, 1–11. [Google Scholar] [CrossRef]
- Ahmed, S.; Manaf, N.; Islam, R. Effects of Lean Six Sigma application in healthcare services: A literature review. Rev. Environ. Health 2013, 28, 189–194. [Google Scholar] [CrossRef] [PubMed]
- Monday, L. Define, Measure, Analyze, Improve, Control (DMAIC) Methodology as a Roadmap in Quality Improvement. Glob. J. Qual. Saf. Healthc. 2022, 5, 44–46. [Google Scholar] [CrossRef] [PubMed]
- Prestinaci, F.; Pezzotti, P.; Pantosti, A. Antimicrobial resistance: A global multifaceted phenomenon. Pathog. Glob. Health 2015, 109, 309–318. [Google Scholar] [CrossRef]
- Cunha, C.B. An Overview of Antimicrobial Stewardship Programs: Imperatives, Interventions, and Innovations. Med. Clin. 2018, 102, xxi–xxiii. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Core Elements of Hospital Antibiotic Stewardship Programs. 2019. Available online: https://www.cdc.gov/antibiotic-use/core-elements/hospital.html (accessed on 29 August 2023).
- Joint Commission on Hospital Accreditation. APPROVED: New Antimicrobial Stewardship Standard. Jt. Comm. Perspect. 2016, 36, 1, 3–4, 8. [Google Scholar]
- Singh, S.; Menon, V.P.; Mohamed, Z.U.; Kumar, V.A.; Nampoothiri, V.; Sudhir, S.; Moni, M.; Dipu, T.; Dutt, A.; Edathadathil, F. Implementation and impact of an antimicrobial stewardship program at a tertiary care center in South India. Open Forum Infect. Dis. 2019, 6, ofy290. [Google Scholar] [CrossRef]
- Baroudi, R.; Flaugher, M.; Grace, E.; Zakria, D. The Importance of an Antimicrobial Stewardship Program. Fed. Pract. 2015, 32, 20–24. [Google Scholar]
- Majumder, M.A.A.; Rahman, S.; Cohall, D.; Bharatha, A.; Singh, K.; Haque, M.; Gittens-St Hilaire, M. Antimicrobial Stewardship: Fighting Antimicrobial Resistance and Protecting Global Public Health. Infect. Drug Resist. 2020, 13, 4713–4738. [Google Scholar] [CrossRef] [PubMed]
- Ha, D.R.; Haste, N.M.; Gluckstein, D.P. The Role of Antibiotic Stewardship in Promoting Appropriate Antibiotic Use. Am. J. Lifestyle Med. 2019, 13, 376–383. [Google Scholar] [CrossRef] [PubMed]
- Bauer, K.A.; Kullar, R.; Gilchrist, M.; File, T.M., Jr. Antibiotics and adverse events: The role of antimicrobial stewardship programs in ‘doing no harm’. Curr. Opin. Infect. Dis. 2019, 32, 553–558. [Google Scholar] [CrossRef] [PubMed]
- Doron, S.; Davidson, L.E. Antimicrobial stewardship. Mayo Clin. Proc. 2011, 86, 1113–1123. [Google Scholar] [CrossRef] [PubMed]
- Jamaati, H.; Dastan, F.; Mirshafiei Langari, Z.; Haghgoo, R.; Eskandari, R.; Marjani, M.; Moniri, A.; Hashemian, S.M.; Farzanegan, B.; Abedini, A.; et al. Study Protocol on Antimicrobial Stewardship in a Tertiary Respiratory Referral Hospital. Tanaffos 2018, 17, 183–187. [Google Scholar] [PubMed]
- Zay Ya, K.; Win, P.T.N.; Bielicki, J.; Lambiris, M.; Fink, G. Association between Antimicrobial Stewardship Programs and Antibiotic Use Globally: A Systematic Review and Meta-Analysis. JAMA Netw. Open 2023, 6, e2253806. [Google Scholar] [CrossRef]
- Mediclinic Middle East. About Mediclinic Middle East. Available online: https://www.mediclinic.ae/en/corporate/about-mediclinic-middle-east.html (accessed on 1 September 2023).
- Mediclinic Middle East. Vision and Values. Available online: https://www.mediclinic.ae/en/corporate/about-mediclinic-middle-east/vision-and-values.html (accessed on 1 September 2023).
- Monday, L.M.; Yazdanpaneh, O.; Sokolowski, C.; Chi, J.; Kuhn, R.; Bazzy, K.; Dhar, S. A Physician-Driven Quality Improvement Stewardship Intervention Using Lean Six Sigma Improves Patient Care for Community-Acquired Pneumonia. Glob. J. Qual. Saf. Healthc. 2021, 4, 109–116. [Google Scholar] [CrossRef]
- Rathi, R.; Vakharia, A.; Shadab, M. Lean six sigma in the healthcare sector: A systematic literature review. Mater. Today Proc. 2022, 50, 773–781. [Google Scholar] [CrossRef]
- McDermott, O.; Antony, J.; Bhat, S.; Jayaraman, R.; Rosa, A.; Marolla, G.; Parida, R. Lean Six Sigma in Healthcare: A Systematic Literature Review on Challenges, Organisational Readiness and Critical Success Factors. Processes 2022, 10, 1945. [Google Scholar] [CrossRef]
- Satapathy, S.; Sahu, Y.P.; Panigrahi, A.K.; Rath, B.; Patra, A.N. Drug utilization pattern of antimicrobials in intensive care unit of a tertiary care teaching hospital. Int. J. Basic Clin. Pharmacol. 2020, 9, 1594. [Google Scholar] [CrossRef]
- Black, B.; Beadle, K.; Harding, S.J. Out of sight, out of mind: Impact of an antimicrobial stewardship initiative to reduce fluoroquinolone utilization. J. Am. Coll. Clin. Pharm. 2022, 5, 668–673. [Google Scholar] [CrossRef]
- Hopkins, T.L.; Yang, L.; Douglass, D.; Sanchez, C.; Morneau, K.; Cadena-Zuluaga, J.; Walter, E. 890. Bundled Antimicrobial Stewardship Intervention Reduces Inpatient Third Generation Cephalosporin Use without Restriction. Open Forum Infect. Dis. 2022, 9, ofac492–ofac735. [Google Scholar] [CrossRef]
- Jose, J.E.; Reji, S.C.; Sunny, A.; Upendran, B.; Lakshmi, R. A Study on Prescribing Pattern, Indications and Rationality of Restricted Antibiotic Use in a Tertiary Care Hospital. Saudi J. Med. Pharm. Sci. 2022, 8, 86–91. [Google Scholar] [CrossRef]
- Kumar, S.; Kumar, A. Evaluation of Restricted Antibiotics Utilisation in a Tertiary Care Teaching Hospital. Indian J. Pharm. Pract. 2021, 14, 199. [Google Scholar] [CrossRef]
- So, J.P.; Aleem, I.S.; Tsang, D.S.; Matlow, A.G.; Wright, J.G. Increasing Compliance with an Antibiotic Prophylaxis Guideline to Prevent Pediatric Surgical Site Infection: Before and after Study. Ann. Surg. 2015, 262, 403–408. [Google Scholar] [CrossRef]
- Moehring, R.W.; Davis, A.; Ashley, E.D.; Dyer, A.P.; Drew, R.H.; Loknyghina, Y.; Johnson, M.D.; Jones, T.M.; Spires, S.S.; Sexton, D.J. Harvesting the low-hanging fruit? Comparative assessment of intravenous to oral route antimicrobial conversion policy implementation. Infect. Control Hosp. Epidemiol. 2023, 44, 954–958. [Google Scholar] [CrossRef]
- Hoffmann, M.; Sendlhofer, G.; Gombotz, V.; Pregartner, G.; Zierler, R.; Schwarz, C.; Tax, C.; Brunner, G. Hand hygiene compliance in intensive care units: An observational study. Int. J. Nurs. Pract. 2020, 26, e12789. [Google Scholar] [CrossRef]
- Li, Y.; Ge, H.; Zhou, H.; Zhou, W.; Zheng, J.; Chen, W.; Cao, X. Impact of environmental cleaning on the colonization and infection rates of multidrug-resistant Acinetobacter baumannii in patients within the intensive care unit in a tertiary hospital. Antimicrob. Resist. Infect. Control 2021, 10, 4. [Google Scholar] [CrossRef]
- de Castro Franco, L.M.; Cota, G.F.; Pinto, T.S.; Ercole, F.F. Preoperative bathing of the surgical site with chlorhexidine for infection prevention: Systematic review with meta-analysis. Am. J. Infect. Control 2017, 45, 343–349. [Google Scholar] [CrossRef]
- Day, S.R.; Smith, D.; Harris, K.; Cox, H.L.; Mathers, A.J. An infectious diseases physician-led antimicrobial stewardship program at a small community hospital associated with improved susceptibility patterns and cost-savings after the first year. Open Forum Infect. Dis. 2015, 2, ofv064. [Google Scholar] [CrossRef]
- Medina-Polo, J.; Gil-Moradillo, J.; González-Díaz, A.; Abad-López, P.; Santos-Pérez de la Blanca, R.; Hernández-Arroyo, M.; Peña-Vallejo, H.; Téigell-Tobar, J.; Calzas-Montalvo, C.; Caro-González, P.; et al. Observational study over 8-year period evaluating microbiological characteristics and risk factor for isolation of multidrug-resistant organisms (MDRO) in patients with healthcare-associated infections (HAIs) hospitalized in a urology ward. GMS Infect. Dis. 2021, 9, Doc04. [Google Scholar] [PubMed]
- Hurtado, D.; Varela, M.; Juarez, A.; Nguyen, Y.-N.; Nhean, S. Impact of Antimicrobial Stewardship Program Intervention Acceptance on Hospital Length of Stay. Hosp. Pharm. 2023, 58, 491–495. [Google Scholar] [CrossRef] [PubMed]
- Suh, Y.; Ah, Y.-M.; Chun, H.-J.; Lee, S.-M.; Kim, H.-s.; Gu, H.-J.; Kim, A.-J.; Chung, J.-E.; Cho, Y.; Lee, Y.-H. Potential impact of the involvement of clinical pharmacists in antimicrobial stewardship programs on the incidence of antimicrobial-related adverse events in hospitalized patients: A multicenter retrospective study. Antibiotics 2021, 10, 853. [Google Scholar] [CrossRef] [PubMed]
- Kaki, R.; Elligsen, M.; Walker, S.; Simor, A.; Palmay, L.; Daneman, N. Impact of antimicrobial stewardship in critical care: A systematic review. J. Antimicrob. Chemother. 2011, 66, 1223–1230. [Google Scholar] [CrossRef] [PubMed]
- Akpan, M.R.; Ahmad, R.; Shebl, N.A.; Ashiru-Oredope, D. A Review of Quality Measures for Assessing the Impact of Antimicrobial Stewardship Programs in Hospitals. Antibiotics 2016, 5, 5. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, S. Integrating DMAIC approach of Lean Six Sigma and theory of constraints toward quality improvement in healthcare. Rev. Environ. Health 2019, 34, 427–434. [Google Scholar] [CrossRef] [PubMed]
- Mettler, C. Developing Gantt Charts. In Engineering Design; Springer: Berlin/Heidelberg, Germany, 2023; pp. 213–231. [Google Scholar] [CrossRef]
- Antony, J.; Palsuk, P.; Gupta, S.; Mishra, D.; Barach, P. Six Sigma in healthcare: A systematic review of the literature. Int. J. Qual. Reliab. Manag. 2018, 35, 1075–1092. [Google Scholar] [CrossRef]
- Almorsy, L.; Khalifa, M. Lean Six Sigma in Health Care: Improving Utilization and Reducing Waste. Stud. Health Technol. Inf. 2016, 226, 194–197. [Google Scholar]
- Amaratunga, T.; Dobranowski, J. Systematic Review of the Application of Lean and Six Sigma Quality Improvement Methodologies in Radiology. J. Am. Coll. Radiol. 2016, 13, 1088–1095.e1087. [Google Scholar] [CrossRef]
- Niemeijer, G.C.; Trip, A.; de Jong, L.J.; Wendt, K.W.; Does, R.J. Impact of 5 years of lean six sigma in a University Medical Center. Qual. Manag. Health Care 2012, 21, 262–268. [Google Scholar] [CrossRef]
- Trzeciak, S.; Mercincavage, M.; Angelini, C.; Cogliano, W.; Damuth, E.; Roberts, B.W.; Zanotti, S.; Mazzarelli, A.J. Lean Six Sigma to Reduce Intensive Care Unit Length of Stay and Costs in Prolonged Mechanical Ventilation. J. Healthc. Qual. JHQ 2018, 40, 36–43. [Google Scholar] [CrossRef] [PubMed]
- Chassin, R. The Six Sigma initiative at Mount Sinai Medical Center. Mt. Sinai J. Med. 2008, 75, 45–52. [Google Scholar] [CrossRef] [PubMed]
- Monmaturapoj, T.; Scott, J.; Smith, P.; Watson, M.C. What influences the implementation and sustainability of antibiotic stewardship programmes in hospitals? A qualitative study of antibiotic pharmacists’ perspectives across South West England. Eur. J. Hosp. Pharm. 2022, 29, e46–e51. [Google Scholar] [CrossRef] [PubMed]
- Mendelson, M.; Morris, A.M.; Thursky, K.; Pulcini, C. How to start an antimicrobial stewardship programme in a hospital. Clin. Microbiol. Infect. 2020, 26, 447–453. [Google Scholar] [CrossRef] [PubMed]
- Satterfield, J.; Miesner, A.R.; Percival, K.M. The role of education in antimicrobial stewardship. J. Hosp. Infect. 2020, 105, 130–141. [Google Scholar] [CrossRef]
- Rout, J.; Essack, S.; Brysiewicz, P. Guideline recommendations for antimicrobial stewardship education for clinical nursing practice in hospitals: A scoping review. S. Afr. J. Crit. Care 2021, 37, 104–114. [Google Scholar] [CrossRef]
- Sangwan, R.; Neels, A.J.; Gwini, S.M.; Saha, S.K.; Athan, E. Is Education Alone Enough to Sustain Improvements of Antimicrobial Stewardship in General Practice in Australia? Results of an Intervention Follow-Up Study. Antibiotics 2023, 12, 594. [Google Scholar] [CrossRef]
- Rehman, S. A parallel and silent emerging pandemic: Antimicrobial resistance (AMR) amid COVID-19 pandemic. J. Infect. Public Health 2023, 16, 611–617. [Google Scholar] [CrossRef]
- Ghosh, S.; Bornman, C.; Zafer, M.M. Antimicrobial Resistance Threats in the emerging COVID-19 pandemic: Where do we stand? J. Infect. Public Health 2021, 14, 555–560. [Google Scholar] [CrossRef]
- Malik, S.S.; Mundra, S. Increasing Consumption of Antibiotics during the COVID-19 Pandemic: Implications for Patient Health and Emerging Anti-Microbial Resistance. Antibiotics 2022, 12, 45. [Google Scholar] [CrossRef]
- Massarine, N.C.M.; de Souza, G.H.A.; Nunes, I.B.; Salomé, T.M.; Barbosa, M.D.S.; Faccin, I.; Rossato, L.; Simionatto, S. How Did COVID-19 Impact the Antimicrobial Consumption and Bacterial Resistance Profiles in Brazil? Antibiotics 2023, 12, 1374. [Google Scholar] [CrossRef] [PubMed]
- Gul, B.; Sana, M.; Saleem, A.; Mustafa, Z.U.; Salman, M.; Khan, Y.H.; Mallhi, T.H.; Sono, T.M.; Meyer, J.C.; Godman, B.B. Antimicrobial Dispensing Practices during COVID-19 and the Implications for Pakistan. Antibiotics 2023, 12, 1018. [Google Scholar] [CrossRef] [PubMed]
- Micheli, G.; Sangiorgi, F.; Catania, F.; Chiuchiarelli, M.; Frondizi, F.; Taddei, E.; Murri, R. The Hidden Cost of COVID-19: Focus on Antimicrobial Resistance in Bloodstream Infections. Microorganisms 2023, 11, 1299. [Google Scholar] [CrossRef] [PubMed]
- Hashad, N.; Stewart, D.; Perumal, D.; Abdulrazzaq, N.; Tonna, A.P. The impact of COVID-19 on antimicrobial stewardship programme implementation in hospitals—An exploration informed by the Consolidated Framework for Implementation Research. J. Hosp. Infect. 2022, 129, 144–152. [Google Scholar] [CrossRef]
- Hashad, N.; Stewart, D.; Perumal, D.; Abdulrazzaq, N.; Tonna, A.P. Antimicrobial stewardship programme implementation in the UAE: Perspectives of key stakeholders using Consolidated Framework for Implementation Research. J. Hosp. Infect. 2023, 137, 69–76. [Google Scholar] [CrossRef]
- Carboneau, C.; Benge, E.; Jaco, M.T.; Robinson, M. A lean Six Sigma team increases hand hygiene compliance and reduces hospital-acquired MRSA infections by 51%. J. Healthc. Qual. 2010, 32, 61–70. [Google Scholar] [CrossRef]
- Berkhout, C.; Berbra, O.; Favre, J.; Collins, C.; Calafiore, M.; Peremans, L.; Van Royen, P. Defining and evaluating the Hawthorne effect in primary care, a systematic review and meta-analysis. Front. Med. 2022, 9, 1033486. [Google Scholar] [CrossRef]
| Study Phase | Duration | Mean Expenditure in AED 1 | Mean Expenditure in Units | Mean DDD 2 per 100 Bed-Days | Mean Admissions |
|---|---|---|---|---|---|
| Baseline | 1 January 2021–31 March 2021 | 661,680 | 5597 | 2.417 | 616 |
| Define | 1 April 2021–31 May 2021 | 417,320.5 | 4298 | 2.155 | 723.5 |
| Measure/Analyze | 1 June 2021–31 March 2022 | 105,240.5 | 2624.2 | 1.704 | 709.9 |
| Improve/Control | 1 April 2022–31 July 2022 | 87,249 | 2092.75 | 1.758 | 791.75 |
| Cause Identified from Ishikawa Diagram | Corresponding Intervention |
|---|---|
| Limited health information technology tools | Utilization of local antibiogram and adherence to culture and susceptibility results; guidelines for antimicrobial use |
| Difficulty in accessing laboratory microbiologic culture results | Utilization of local antibiogram and adherence to culture and susceptibility results |
| Unrestricted access to some antimicrobial agents | Guidelines for antimicrobial use; formulary restriction with prior authorization |
| Complexity in process | Formulary restriction with prior authorization; conversion from IV to PO antimicrobials |
| Variation in process | Utilization audits; assessment of antimicrobial use |
| Adherence gaps in guidelines | Leadership support; feedback/education |
| Clarity on ASP goals | Leadership support; utilization audits |
| Empirical antimicrobial use | Guidelines for antimicrobial use; feedback/education |
| Lack of guidelines in the early COVID-19 phase | Feedback/education |
| Lack of EHR supporting tools | Guidelines for antimicrobial use |
| Weak data collection/monitoring system | Utilization audits |
| Lack of automated order sets | Guidelines for antimicrobial use |
| Doctors’ old practices | Feedback/education |
| Variable competency levels | Utilization audits; feedback/education |
| Physicians’ fears and concerns about legal charges | Leadership support |
| Intervention | Measures Taken |
|---|---|
| Leadership support | The multidisciplinary team for the ASP at MWEL includes senior leaders from the hospital, such as the medical director, pharmacy manager, quality officer, and other key physicians and unit managers. These individuals possess the necessary expertise and skills to address significant shortcomings and effectively train their peers on ASP guidelines, promoting adherence to best practices. Also, MWEL leadership demonstrated a commitment to the requisite human, financial, and information technology resources essential for the success of our ASP initiative. |
| Guidelines for antimicrobial use | Allocated necessary resources, personnel, and budget to support the implementation of ASP strategies. Data comparisons of antimicrobial use before and after the introduction of the guidelines to measure their effectiveness. |
| Formulary restriction with prior authorization | Established clear communication channels for disseminating ASP goals, progress, and achievements |
| Utilization audits | Established a dedicated ASP team comprising interdisciplinary members to oversee program implementation |
| Utilization of local antibiogram and adherence to culture and susceptibility results | Conducted regular meetings to update hospital leadership on ASP progress, challenges, and achievements |
| Conversion from IV to PO antimicrobials | Encouraged hospital executives to actively participate in ASP-related activities and initiatives |
| Assessment of antimicrobial use (selection, dosage, route, and duration) | Developed evidence-based guidelines for appropriate antimicrobial prescribing and usage |
| Feedback/education | Ensured guidelines were regularly updated based on the latest clinical evidence and emerging resistance patterns |
| Proper cleaning and hand hygiene | Created a user-friendly electronic platform (Intranet) for easy access to and dissemination of the antimicrobial guidelines to all clinical staff |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sallam, M.; Snygg, J. Improving Antimicrobial Stewardship Program Using the Lean Six Sigma Methodology: A Descriptive Study from Mediclinic Welcare Hospital in Dubai, the UAE. Healthcare 2023, 11, 3048. https://doi.org/10.3390/healthcare11233048
Sallam M, Snygg J. Improving Antimicrobial Stewardship Program Using the Lean Six Sigma Methodology: A Descriptive Study from Mediclinic Welcare Hospital in Dubai, the UAE. Healthcare. 2023; 11(23):3048. https://doi.org/10.3390/healthcare11233048
Chicago/Turabian StyleSallam, Mohammed, and Johan Snygg. 2023. "Improving Antimicrobial Stewardship Program Using the Lean Six Sigma Methodology: A Descriptive Study from Mediclinic Welcare Hospital in Dubai, the UAE" Healthcare 11, no. 23: 3048. https://doi.org/10.3390/healthcare11233048
APA StyleSallam, M., & Snygg, J. (2023). Improving Antimicrobial Stewardship Program Using the Lean Six Sigma Methodology: A Descriptive Study from Mediclinic Welcare Hospital in Dubai, the UAE. Healthcare, 11(23), 3048. https://doi.org/10.3390/healthcare11233048







