Preliminary Insights into the Diagnostic Accuracy of the Modified Arm Care Screen Test for Overhead Athletes: An On-Field Tool for Injury Prevention
Abstract
:1. Introduction
2. Materials and Methods
2.1. Sample
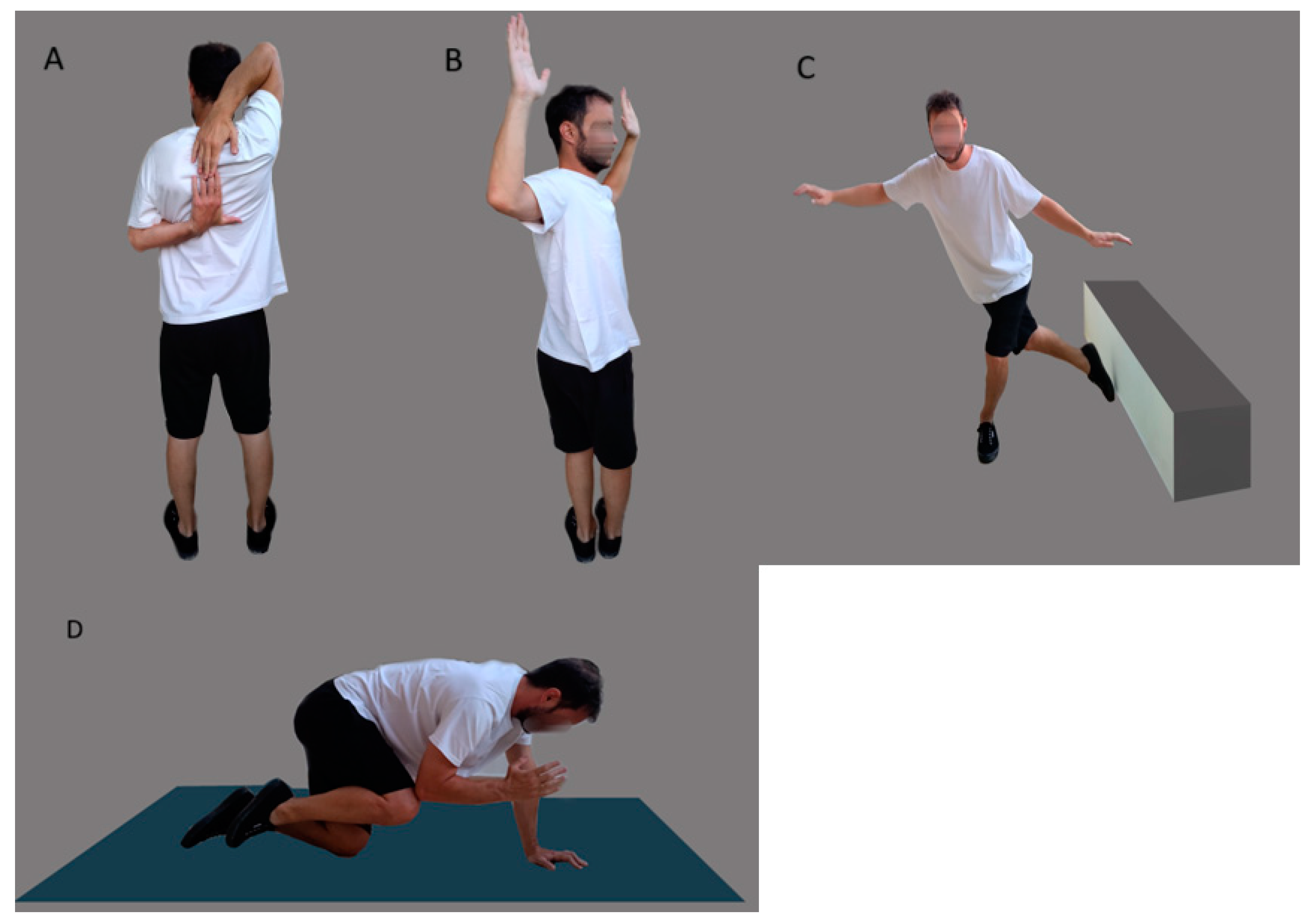
2.2. Modified ACS
2.3. Risk Factors
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lintner, D.; Noonan, T.J.; Kibler, W.B. Injury patterns and biomechanics of the athlete’s shoulder. Clin. Sports Med. 2008, 27, 527–551. [Google Scholar] [CrossRef] [PubMed]
- Frisch, K.E.; Clark, J.; Hanson, C.; Fagerness, C.; Conway, A.; Hoogendoorn, L. High prevalence of nontraumatic shoulder pain in a regional sample of female high school volleyball athletes. Orthop. J. Sports Med. 2017, 5, 2325967117712236. [Google Scholar] [CrossRef] [PubMed]
- Paraskevopoulos, E.; Pamboris, G.M.; Papandreou, M. The Changing Landscape in Upper Limb Sports Rehabilitation and Injury Prevention. Sports 2023, 11, 80. [Google Scholar] [CrossRef]
- McElheny, K.; Sgroi, T.; Carr, J.B., 2nd. Efficacy of Arm Care Programs for Injury Prevention. Curr. Rev. Musculoskelet. Med. 2021, 14, 160–167. [Google Scholar] [CrossRef]
- Matsel, K.A.; Butler, R.J.; Malone, T.R.; Hoch, M.C.; Westgate, P.M.; Uhl, T.L. Current concepts in arm care exercise programs and injury risk reduction in adolescent baseball players: A clinical review. Sports Health 2021, 13, 245–250. [Google Scholar] [CrossRef]
- Mullaney, M.; Nicholas, S.; Tyler, T.; Fukunaga, T.; McHugh, M. Evidence based arm care: The throwers 10 revisited. Int. J. Sports Phys. Ther. 2021, 16, 1379. [Google Scholar] [CrossRef] [PubMed]
- Pamias-Velázquez, K.J.; Figueroa-Negrón, M.M.; Tirado-Crespo, J.; Mulero-Portela, A.L. Compliance with Injury Prevention Measures in Youth Pitchers: Survey of Coaches in Little League of Puerto Rico. Sports Health 2016, 8, 274–277. [Google Scholar] [CrossRef]
- Matsel, K.A.; Hoch, M.C.; Butler, R.J.; Westgate, P.M.; Malone, T.R.; Uhl, T.L. A Field-expedient Arm Care Screening Tool Can Identify Musculoskeletal Risk Factors in Baseball Players. Sports Health 2022, 15, 19417381221125465. [Google Scholar] [CrossRef]
- Yamaura, K.; Mifune, Y.; Inui, A.; Nishimoto, H.; Kurosawa, T.; Mukohara, S.; Yoshikawa, T.; Hoshino, Y.; Niikura, T.; Kokubu, T.; et al. Relationship between glenohumeral internal rotation deficit and shoulder conditions in professional baseball pitchers. J. Shoulder Elb. Surg. 2021, 30, 2073–2081. [Google Scholar] [CrossRef]
- Shitara, H.; Kobayashi, T.; Yamamoto, A.; Shimoyama, D.; Ichinose, T.; Tajika, T.; Osawa, T.; Iizuka, H.; Takagishi, K. Prospective multifactorial analysis of preseason risk factors for shoulder and elbow injuries in high school baseball pitchers. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 3303–3310. [Google Scholar] [CrossRef]
- Sekiguchi, T.; Hagiwara, Y.; Yabe, Y.; Tsuchiya, M.; Itaya, N.; Yoshida, S.; Yano, T.; Sogi, Y.; Suzuki, K.; Itoi, E. Restriction in the hip internal rotation of the stride leg is associated with elbow and shoulder pain in elite young baseball players. J. Shoulder Elb. Surg. 2020, 29, 139–145. [Google Scholar] [CrossRef]
- Hamano, N.; Shitara, H.; Tajika, T.; Ichinose, T.; Sasaki, T.; Kamiyama, M.; Miyamoto, R.; Kuboi, T.; Endo, F.; Yamamoto, A.; et al. Relationship between tightness of the hip joint and shoulder/elbow injury in high school baseball pitchers: A prospective study. Sci. Rep. 2020, 10, 19979. [Google Scholar] [CrossRef] [PubMed]
- Sakata, J.; Nakamura, E.; Suzukawa, M.; Akaike, A.; Shimizu, K. Physical Risk Factors for a Medial Elbow Injury in Junior Baseball Players: A Prospective Cohort Study of 353 Players. Am. J. Sports Med. 2017, 45, 135–143. [Google Scholar] [CrossRef] [PubMed]
- Salamh, P.; Jones, E.; Bashore, M.; Liu, X.; Hegedus, E.J. Injuries and associated risk factors of the shoulder and elbow among adolescent baseball pitchers: A systematic review and meta-analysis. Phys. Ther. Sport 2020, 43, 108–119. [Google Scholar] [CrossRef] [PubMed]
- Matsel, K.; Brown, S.; Hoch, M.; Butler, R.; Westgate, P.; Malone, T.; Uhl, T. The Intra- and Inter-rater Reliability of an Arm Care Screening Tool in High School Baseball Coaches. Int. J. Sports Phys. Ther. 2021, 16, 1532. [Google Scholar] [CrossRef] [PubMed]
- Liaghat, B.; Pedersen, J.R.; Husted, R.S.; Pedersen, L.L.; Thorborg, K.; Juhl, C.B. Diagnosis, prevention and treatment of common shoulder injuries in sport: Grading the evidence-a statement paper commissioned by the Danish Society of Sports Physical Therapy (DSSF). Br. J. Sports Med. 2023, 57, 408–416. [Google Scholar] [CrossRef] [PubMed]
- Barfield, J.W.; Bordelon, N.M.; Wasserberger, K.W.; Oliver, G.D. Preliminary Analysis of Closed Kinetic Chain Upper Extremity Stability Test Differences Between Healthy and Previously Injured/In-Pain Baseball Pitchers. Sports Health 2023, 15, 290–294. [Google Scholar] [CrossRef] [PubMed]
- Richardson, E.; Lewis, J.S.; Gibson, J.; Morgan, C.; Halaki, M.; Ginn, K.; Yeowell, G. Role of the kinetic chain in shoulder rehabilitation: Does incorporating the trunk and lower limb into shoulder exercise regimes influence shoulder muscle recruitment patterns? Systematic review of electromyography studies. BMJ Open Sport Exerc. Med. 2020, 6, e000683. [Google Scholar] [CrossRef]
- Buderer, N.M. Statistical methodology: I. Incorporating the prevalence of disease into the sample size calculation for sensitivity and specificity. Acad. Emerg. Med. 1996, 3, 895–900. [Google Scholar] [CrossRef]
- Paraskevopoulos, E.; Simeonidis, T.; Tsolakis, C.; Koulouvaris, P.; Papandreou, M. Mirror Cross-Exercise on a Kinetic Chain Approach Improves Throwing Performance in Professional Volleyball Athletes with Scapular Dyskinesis. J. Sport Rehabil. 2021, 31, 131–139. [Google Scholar] [CrossRef]
- Paraskevopoulos, E.; Simeonidis, T.; Tsolakis, C.; Koulouvaris, P.; Papandreou, M. The adjunctive benefits of mirror cross education on kinetic chain exercise approach in volleyball athletes with scapular dyskinesis. J. Sports Med. Phys. Fit. 2021, 62, 98–109. [Google Scholar] [CrossRef]
- Plisky, P.J.; Gorman, P.P.; Butler, R.J.; Kiesel, K.B.; Underwood, F.B.; Elkins, B. The reliability of an instrumented device for measuring components of the star excursion balance test. N. Am. J. Sports Phys. Ther. 2009, 4, 92–99. [Google Scholar]
- Teyhen, D.S.; Shaffer, S.W.; Lorenson, C.L.; Halfpap, J.P.; Donofry, D.F.; Walker, M.J.; Dugan, J.L.; Childs, J.D. The functional movement screen: A reliability study. J. Orthop. Sports Phys. Ther. 2012, 42, 530–540. [Google Scholar] [CrossRef] [PubMed]
- Goldbeck, T.G.; Davies, G.J. Test-retest reliability of the closed kinetic chain upper extremity stability test: A clinical field test. J. Sport Rehabil. 2000, 9, 35–45. [Google Scholar] [CrossRef]
- Pontillo, M.; Spinelli, B.A.; Sennett, B.J. Prediction of In-Season Shoulder Injury from Preseason Testing in Division I Collegiate Football Players. Sports Health 2014, 6, 497–503. [Google Scholar] [CrossRef] [PubMed]
- Ellenbecker, T.; Manske, R.; Davies, G. Closed kinetic chain testing techniques of the upper extremities. Orthop. Phys. Ther. Clin. N. Am. 2000, 9, 219–230. [Google Scholar]
- Bullock, G.S.; Faherty, M.S.; Ledbetter, L.; Thigpen, C.A.; Sell, T.C. Shoulder Range of Motion and Baseball Arm Injuries: A Systematic Review and Meta-Analysis. J. Athl. Train. 2018, 53, 1190–1199. [Google Scholar] [CrossRef]
- Shanley, E.; Kissenberth, M.J.; Thigpen, C.A.; Bailey, L.B.; Hawkins, R.J.; Michener, L.A.; Tokish, J.M.; Rauh, M.J. Preseason shoulder range of motion screening as a predictor of injury among youth and adolescent baseball pitchers. J. Shoulder Elb. Surg. 2015, 24, 1005–1013. [Google Scholar] [CrossRef] [PubMed]
- Wilk, K.E.; Macrina, L.C.; Fleisig, G.S.; Porterfield, R.; Simpson, C.D., 2nd; Harker, P.; Paparesta, N.; Andrews, J.R. Correlation of glenohumeral internal rotation deficit and total rotational motion to shoulder injuries in professional baseball pitchers. Am. J. Sports Med. 2011, 39, 329–335. [Google Scholar] [CrossRef]
- Wilk, K.E.; Macrina, L.C.; Fleisig, G.S.; Aune, K.T.; Porterfield, R.A.; Harker, P.; Evans, T.J.; Andrews, J.R. Deficits in glenohumeral passive range of motion increase risk of shoulder injury in professional baseball pitchers: A prospective study. Am. J. Sports Med. 2015, 43, 2379–2385. [Google Scholar] [CrossRef]
- Hiramoto, M.; Morihara, T.; Kida, Y.; Matsui, T.; Azuma, Y.; Seo, K.; Miyazaki, T.; Watanabe, Y.; Kai, Y.; Yamada, Y.; et al. Hip, Trunk, and Shoulder Rotational Range of Motion in Healthy Japanese Youth and High-school Baseball Pitchers. Prog. Rehabil. Med. 2019, 4, 20190009. [Google Scholar] [CrossRef] [PubMed]
- Zhou, X.; Imai, K.; Liu, X.; Chen, Z.; Watanabe, E. Assessing the Association of Shoulder Pain Risk with Physical Fitness in Badminton Players at National Tournament Level. Asian J. Sports Med. 2022, 13, e129916. [Google Scholar] [CrossRef]
- Saito, M.; Kenmoku, T.; Kameyama, K.; Murata, R.; Yusa, T.; Ochiai, N.; Kijima, T.; Takahira, N.; Fukushima, K.; Ishige, N. Relationship between tightness of the hip joint and elbow pain in adolescent baseball players. Orthop. J. Sports Med. 2014, 2, 2325967114532424. [Google Scholar] [CrossRef] [PubMed]
- Ryman Augustsson, S.; Ageberg, E. Weaker lower extremity muscle strength predicts traumatic knee injury in youth female but not male athletes. BMJ Open Sport Exerc. Med. 2017, 3, e000222. [Google Scholar] [CrossRef]
- De Noronha, M.; França, L.C.; Haupenthal, A.; Nunes, G. Intrinsic predictive factors for ankle sprain in active university students: A prospective study. Scand. J. Med. Sci. Sports 2013, 23, 541–547. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.-Y. Statistical notes for clinical researchers: Chi-squared test and Fisher’s exact test. Restor. Dent. Endod. 2017, 42, 152–155. [Google Scholar] [CrossRef]
- Farrington, D.P.; Loeber, R. Relative improvement over chance (RIOC) and phi as measures of predictive efficiency and strength of association in 2 × 2 tables. J. Quant. Criminol. 1989, 5, 201–213. [Google Scholar] [CrossRef]
- Trevethan, R. Sensitivity, specificity, and predictive values: Foundations, pliabilities, and pitfalls in research and practice. Front. Public Health 2017, 5, 307. [Google Scholar] [CrossRef]
- Shreffler, J.; Huecker, M.R. Diagnostic Testing Accuracy: Sensitivity, Specificity, Predictive Values and Likelihood Ratios; StatPearls Publishing: Treasure Island, FL, USA, 2020. [Google Scholar]
- Dhaliwal, G.; Saint, S.; Drazen, J.; Solomon, C. Clinical Problem-Solving. N. Engl. J. Med. 2006, 80, 141. [Google Scholar]
- Mısırlıoğlu, T.; Eren, İ.; Canbulat, N.; Çobanoğlu, E.; Günerbüyük, C.; Demirhan, M. Does a core stabilization exercise program have a role on shoulder rehabilitation? A comparative study in young females. Turk. J. Phys. Med. Rehabil. 2018, 64, 328–336. [Google Scholar] [CrossRef]
- Shanley, E.; Rauh, M.J.; Michener, L.A.; Ellenbecker, T.S.; Garrison, J.C.; Thigpen, C.A. Shoulder range of motion measures as risk factors for shoulder and elbow injuries in high school softball and baseball players. Am. J. Sports Med. 2011, 39, 1997–2006. [Google Scholar] [CrossRef]
- Hams, A.; Evans, K.; Adams, R.; Waddington, G.; Witchalls, J. Reduced shoulder strength and change in range of motion are risk factors for shoulder injury in water polo players. Phys. Ther. Sport 2019, 40, 231–237. [Google Scholar] [CrossRef] [PubMed]
- Johnson, J.E.; Fullmer, J.A.; Nielsen, C.M.; Johnson, J.K.; Moorman, C.T., 3rd. Glenohumeral Internal Rotation Deficit and Injuries: A Systematic Review and Meta-analysis. Orthop. J. Sports Med. 2018, 6, 2325967118773322. [Google Scholar] [CrossRef]
- Schwank, A.; Blazey, P.; Asker, M.; Møller, M.; Hägglund, M.; Gard, S.; Skazalski, C.; Haugsbø, A.S.; Horsley, I.; Whiteley, R.; et al. 2022 Bern Consensus Statement on Shoulder Injury Prevention, Rehabilitation, and Return to Sport for Athletes at All Participation Levels. J. Orthop. Sports Phys. Ther. 2021, 52, 11–28. [Google Scholar] [CrossRef] [PubMed]
- Alqarni, A.M.; Nuhmani, S.; Muaidi, Q.I. Glenohumeral internal rotation deficit in volleyball players with and without a history of shoulder pain. Res. Sports Med. 2022, 1–10. [Google Scholar] [CrossRef]
- Moreno-Pérez, V.; Moreside, J.; Barbado, D.; Vera-Garcia, F.J. Comparison of shoulder rotation range of motion in professional tennis players with and without history of shoulder pain. Man. Ther. 2015, 20, 313–318. [Google Scholar] [CrossRef] [PubMed]
- Myers, J.B.; Laudner, K.G.; Pasquale, M.R.; Bradley, J.P.; Lephart, S.M. Glenohumeral range of motion deficits and posterior shoulder tightness in throwers with pathologic internal impingement. Am. J. Sports Med. 2006, 34, 385–391. [Google Scholar] [CrossRef] [PubMed]
- Zaremski, J.L.; Wasser, J.G.; Vincent, H.K. Mechanisms and Treatments for Shoulder Injuries in Overhead Throwing Athletes. Curr. Sports Med. Rep. 2017, 16, 179–188. [Google Scholar] [CrossRef]
- Sundaram, B.; Bhargava, S.; Karuppannan, S. Glenohumeral rotational range of motion differences between fast bowlers and spin bowlers in elite cricketers. Int. J. Sports Phys. Ther. 2012, 7, 576. [Google Scholar]
- Dutton, M.; Tam, N.; Divekar, N.; Prins, D.; Gray, J. The association between gird and overhead throwing biomechanics in cricket. J. Biomech. 2021, 126, 110658. [Google Scholar] [CrossRef]
- Guermont, H.; Mittelheisser, G.; Reboursière, E.; Gauthier, A.; Drigny, J. Shoulder muscle imbalance as a risk factor for shoulder injury in elite badminton players: A prospective study. Phys. Ther. Sport 2023, 61, 149–155. [Google Scholar] [CrossRef] [PubMed]
- Achenbach, L.; Laver, L.; Walter, S.S.; Zeman, F.; Kuhr, M.; Krutsch, W. Decreased external rotation strength is a risk factor for overuse shoulder injury in youth elite handball athletes. Knee Surg. Sports Traumatol. Arthrosc. 2020, 28, 1202–1211. [Google Scholar] [CrossRef] [PubMed]
- Schmalzl, J.; Walter, H.; Rothfischer, W.; Blaich, S.; Gerhardt, C.; Lehmann, L.-J. GIRD syndrome in male handball and volleyball players: Is the decrease of total range of motion the turning point to pathology? J. Back Musculoskelet. Rehabil. 2022, 35, 755–762. [Google Scholar] [CrossRef] [PubMed]
- Moreno-Pérez, V.; López-Samanes, Á.; Domínguez, R.; Fernández-Elías, V.E.; González-Frutos, P.; Fernández-Ruiz, V.; Pérez-López, A.; Fernández-Fernández, J. Acute effects of a single tennis match on passive shoulder rotation range of motion, isometric strength and serve speed in professional tennis players. PLoS ONE 2019, 14, e0215015. [Google Scholar] [CrossRef] [PubMed]
- Keller, R.A.; De Giacomo, A.F.; Neumann, J.A.; Limpisvasti, O.; Tibone, J.E. Glenohumeral Internal Rotation Deficit and Risk of Upper Extremity Injury in Overhead Athletes: A Meta-Analysis and Systematic Review. Sports Health 2018, 10, 125–132. [Google Scholar] [CrossRef]
- Oliver, G.D.; Downs, J.L.; Barbosa, G.M.; Camargo, P.R. Descriptive profile of shoulder range of motion and strength in youth athletes participating in overhead sports. Int. J. Sports Phys. Ther. 2020, 15, 1090–1098. [Google Scholar] [CrossRef] [PubMed]
- Clarsen, B.; Bahr, R.; Andersson, S.H.; Munk, R.; Myklebust, G. Reduced glenohumeral rotation, external rotation weakness and scapular dyskinesis are risk factors for shoulder injuries among elite male handball players: A prospective cohort study. Br. J. Sports Med. 2014, 48, 1327–1333. [Google Scholar] [CrossRef]
- Camp, C.L.; Zajac, J.M.; Pearson, D.B.; Sinatro, A.M.; Spiker, A.M.; Werner, B.C.; Altchek, D.W.; Coleman, S.H.; Dines, J.S. Decreased Shoulder External Rotation and Flexion Are Greater Predictors of Injury Than Internal Rotation Deficits: Analysis of 132 Pitcher-Seasons in Professional Baseball. Arthrosc. J. Arthrosc. Relat. Surg. 2017, 33, 1629–1636. [Google Scholar] [CrossRef]
- Hickey, D.; Solvig, V.; Cavalheri, V.; Harrold, M.; McKenna, L. Scapular dyskinesis increases the risk of future shoulder pain by 43% in asymptomatic athletes: A systematic review and meta-analysis. Br. J. Sports Med. 2018, 52, 102–110. [Google Scholar] [CrossRef]
- Chorley, J.; Eccles, R.E.; Scurfield, A. Care of Shoulder Pain in the Overhead Athlete. Pediatr. Ann. 2017, 46, e112–e113. [Google Scholar] [CrossRef]
- Van Dillen, L.R.; Bloom, N.J.; Gombatto, S.P.; Susco, T.M. Hip rotation range of motion in people with and without low back pain who participate in rotation-related sports. Phys. Ther. Sport 2008, 9, 72–81. [Google Scholar] [CrossRef]
- Vad, V.; Gebeh, A.; Dines, D.; Altchek, D.; Norris, B. Hip and shoulder internal rotation range of motion deficits in professional tennis players. J. Sci. Med. Sport 2003, 6, 71–75. [Google Scholar] [CrossRef] [PubMed]
- Vad, V.B.; Bhat, A.L.; Basrai, D.; Gebeh, A.; Aspergren, D.D.; Andrews, J.R. Low back pain in professional golfers: The role of associated hip and low back range-of-motion deficits. Am. J. Sports Med. 2004, 32, 494–497. [Google Scholar] [CrossRef] [PubMed]
- Scher, S.; Anderson, K.; Weber, N.; Bajorek, J.; Rand, K.; Bey, M.J. Associations among hip and shoulder range of motion and shoulder injury in professional baseball players. J. Athl. Train. 2010, 45, 191–197. [Google Scholar] [CrossRef] [PubMed]
- Garrison, J.C.; Arnold, A.; Macko, M.J.; Conway, J.E. Baseball players diagnosed with ulnar collateral ligament tears demonstrate decreased balance compared to healthy controls. J. Orthop. Sports Phys. Ther. 2013, 43, 752–758. [Google Scholar] [CrossRef]
- Istvan, B. Sport system building and long-term athlete development in British Columbia. Coach. Rep. 2001, 8, 22–28. [Google Scholar]
- Bahr, R. Why screening tests to predict injury do not work—And probably never will…: A critical review. Br. J. Sports Med. 2016, 50, 776–780. [Google Scholar] [CrossRef]
- Van Dyk, N.; Bahr, R.; Whiteley, R.; Tol, J.L.; Kumar, B.D.; Hamilton, B.; Farooq, A.; Witvrouw, E. Hamstring and quadriceps isokinetic strength deficits are weak risk factors for hamstring strain injuries: A 4-year cohort study. Am. J. Sports Med. 2016, 44, 1789–1795. [Google Scholar] [CrossRef]
- Pareja-Blanco, F.; Rodríguez-Rosell, D.; Sánchez-Medina, L.; Sanchis-Moysi, J.; Dorado, C.; Mora-Custodio, R.; Yáñez-García, J.M.; Morales-Alamo, D.; Pérez-Suárez, I.; Calbet, J.A.L.; et al. Effects of velocity loss during resistance training on athletic performance, strength gains and muscle adaptations. Scand. J. Med. Sci. Sports 2017, 27, 724–735. [Google Scholar] [CrossRef]
| ACS | Risk Factors |
|---|---|
| Reciprocal shoulder mobility |
|
| Total Body Rotation |
|
| Lower Body Diagonal Reach |
|
| Rotary Stability |
| Mean Age | 21.4 |
| Gender (Male–Female) | 26–36 |
| Height (cm) | 177.7 ± 10.8 |
| Weight (kg) | 72.6 ± 13.8 |
| BMI | 23 |
| Limb dominance (L: Left, R: Right) | 4 L–58 R |
| Experience (years) | 7.7 ± 4.6 |
| Sport | |
| Volleyball | 36 |
| Basketball | 19 |
| Tennis | 7 |
| Reciprocal Shoulder Mobility | 90/90 Total Body Rotation | Lower-Body Diagonal Reach | Core Stability | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| ≥1 Risk Factor | ≥1 Risk Factor | ≥1 Risk Factor | ≥1 Risk Factor | ||||||||
| Shoulder mobility | Yes | No | Total Body Rotation | Yes | No | Diagonal Reach | Yes | No | Rotary Stability | Yes | No |
| Fail | 25 | 18 | Fail | 23 | 2 | Fail | 31 | 4 | Fail | 13 | 5 |
| Pass | 5 | 14 | Pass | 3 | 34 | Pass | 4 | 23 | Pass | 3 | 41 |
| Chi-square for association | p = 0.032, phi = 0.273 | p = 0.001, phi = 0.905 | p = 0.001, phi = 0.704 | p = 0.001, phi = 0.678 | |||||||
| ACS Component | Reciprocal Shoulder Mobility | Total Body Rotation | Lower Body Diagonal Reach | Rotary Stability | ||||
|---|---|---|---|---|---|---|---|---|
| Statistic | Value | 95% CI | Value | 95% CI | Value | 95% CI | Value | 95% CI |
| Sensitivity | 83.33% | 65.28% to 94.36% | 88.46% | 69.85% to 97.55% | 88.57% | 73.26% to 96.80% | 81.25% | 54.35% to 95.95% |
| Specificity | 43.75% | 26.36% to 62.34% | 94.44% | 81.34% to 99.32% | 85.19% | 66.27% to 95.81% | 89.13% | 76.43% to 96.38% |
| Positive Likelihood Ratio | 1.48 | 1.05 to 2.09 | 15.92 | 4.11 to 61.67 | 5.98 | 2.40 to 14.89 | 7.47 | 3.16 to 17.67 |
| Negative Likelihood Ratio | 0.38 | 0.16 to 0.93 | 0.12 | 0.04 to 0.36 | 0.13 | 0.05 to 0.34 | 0.21 | 0.08 to 0.59 |
| Disease Prevalence | 48.39% | 35.50% to 61.44% | 41.94% | 29.51% to 55.15% | 56.45% | 43.26% to 69.01% | 25.81% | 15.53% to 38.50% |
| Positive Predictive Value | 58.14% | 49.59% to 66.23% | 92.00% | 74.81% to 97.80% | 88.57% | 75.68% to 95.07% | 72.22% | 52.38% to 86.01% |
| Negative Predictive Value | 73.68% | 53.45% to 87.23% | 91.89% | 79.58% to 97.05% | 85.19% | 69.29% to 93.61% | 93.18% | 83.06% to 97.44% |
| Accuracy | 62.90% | 49.69% to 74.84% | 91.94% | 82.17% to 97.33% | 87.10% | 76.15% to 94.26% | 87.10% | 76.15% to 94.26% |
| Odds Ratio | 3.88 | 1.18 to 12.74 | 130.3 | 20.171 to 842.128 | 48.87 | 11.086 to 215.461 | 35.53 | 7.4562 to 169.338 |
| ACS Component | Reciprocal Shoulder Mobility | Total Body Rotation | Lower Body Diagonal Reach | Rotary Stability | ||||
|---|---|---|---|---|---|---|---|---|
| Value | 95% CI | Value | 95% CI | Value | 95% CI | Value | 95% CI | |
| Inter-rater reliability | 0.85 | 0.71 to 0.98 | 0.86 | 0.74 to 0.97 | 0.90 | 0.80 to 0.99 | 0.88 | 0.76 to 0.99 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Paraskevopoulos, E.; Kottaridis, F.-M.; Moutzouri, M.; Koumantakis, G.A.; Antonakis-Karamintzas, D.; Tsolakis, C.; Koulouvaris, P.; Christakou, A.; Papandreou, M. Preliminary Insights into the Diagnostic Accuracy of the Modified Arm Care Screen Test for Overhead Athletes: An On-Field Tool for Injury Prevention. Healthcare 2023, 11, 3046. https://doi.org/10.3390/healthcare11233046
Paraskevopoulos E, Kottaridis F-M, Moutzouri M, Koumantakis GA, Antonakis-Karamintzas D, Tsolakis C, Koulouvaris P, Christakou A, Papandreou M. Preliminary Insights into the Diagnostic Accuracy of the Modified Arm Care Screen Test for Overhead Athletes: An On-Field Tool for Injury Prevention. Healthcare. 2023; 11(23):3046. https://doi.org/10.3390/healthcare11233046
Chicago/Turabian StyleParaskevopoulos, Eleftherios, Fotis-Marios Kottaridis, Maria Moutzouri, George A. Koumantakis, Dimitrios Antonakis-Karamintzas, Charilaos Tsolakis, Panagiotis Koulouvaris, Anna Christakou, and Maria Papandreou. 2023. "Preliminary Insights into the Diagnostic Accuracy of the Modified Arm Care Screen Test for Overhead Athletes: An On-Field Tool for Injury Prevention" Healthcare 11, no. 23: 3046. https://doi.org/10.3390/healthcare11233046
APA StyleParaskevopoulos, E., Kottaridis, F.-M., Moutzouri, M., Koumantakis, G. A., Antonakis-Karamintzas, D., Tsolakis, C., Koulouvaris, P., Christakou, A., & Papandreou, M. (2023). Preliminary Insights into the Diagnostic Accuracy of the Modified Arm Care Screen Test for Overhead Athletes: An On-Field Tool for Injury Prevention. Healthcare, 11(23), 3046. https://doi.org/10.3390/healthcare11233046









