Acupuncture Therapy for Military Veterans Suffering from Posttraumatic Stress Disorder and Related Symptoms: A Scoping Review of Clinical Studies
Abstract
:1. Introduction
2. Materials and Methods
- What are the characteristics of the studies that have investigated the use of acupuncture for managing PTSD in military veterans, including research design and target population?
- What clinical outcomes have been examined in previous studies on PTSD management in military veterans?
- What is the acupuncture therapy regimen for managing PTSD in military veterans?
- What is the effectiveness and safety of using acupuncture for treating PTSD in military veterans, as reported in previous studies?
3. Results
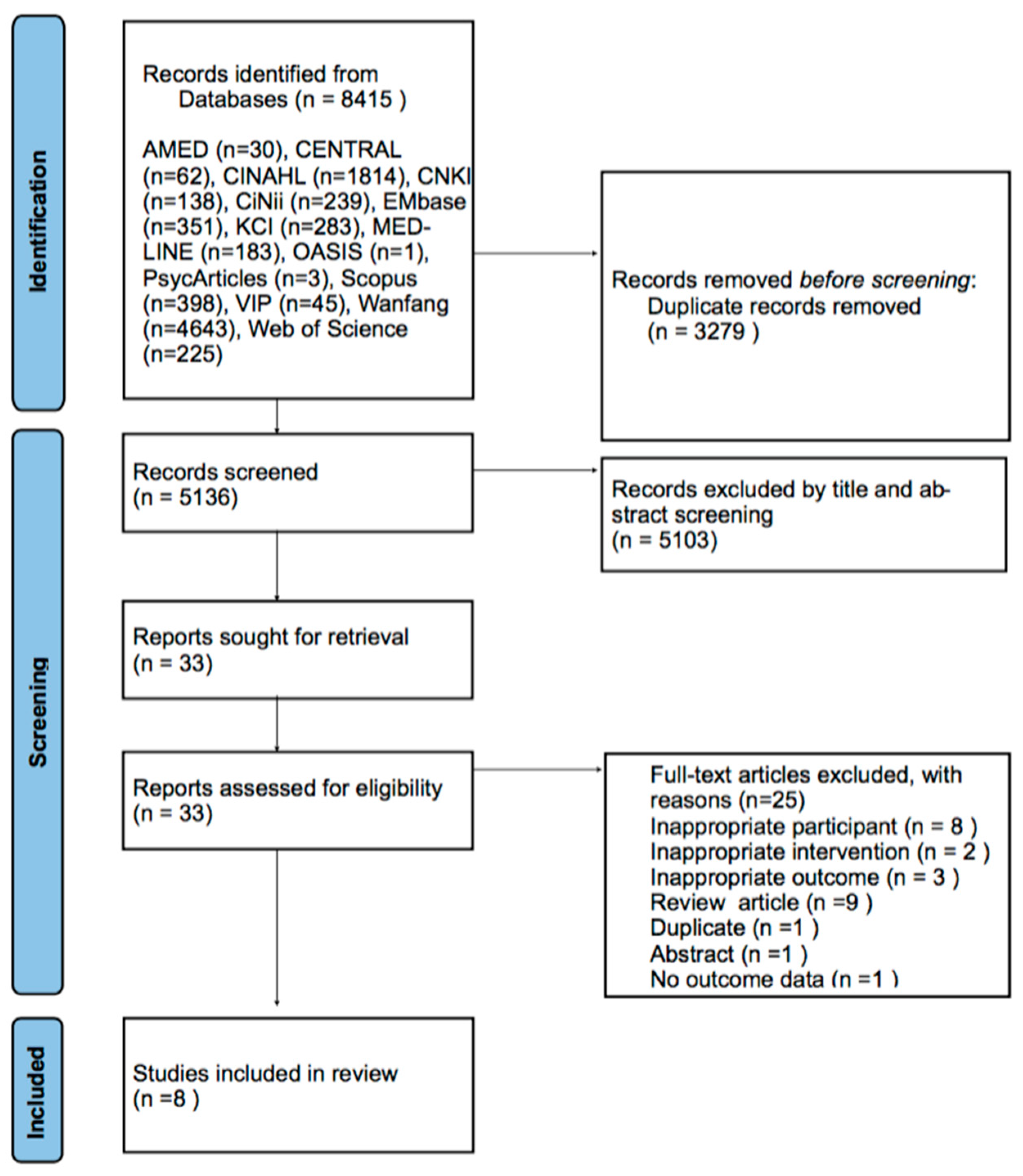
3.1. Study Selection
3.2. General Characteristics of the Included Studies
3.2.1. RCTs
3.2.2. Before-After Studies
3.2.3. Case Series Study
3.2.4. Qualitative Study
3.3. Details of the Acupuncture Methods
3.4. Reported Effectiveness and Safety of Acupuncture for PTSD
3.4.1. Effectiveness in RCTs
3.4.2. Effectiveness in the Before-After Study
3.4.3. Effectiveness in the Case Series
3.4.4. Effectiveness in the Qualitative Study
3.4.5. Safety of Acupuncture
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5; American Psychiatric Association: Washington, DC, USA, 2013; Volume 5. [Google Scholar]
- Lehavot, K.; Katon, J.G.; Chen, J.A.; Fortney, J.C.; Simpson, T.L. Post-traumatic stress disorder by gender and veteran status. Am. J. Prev. Med. 2018, 54, e1–e9. [Google Scholar] [CrossRef] [PubMed]
- Kang, H.K.; Natelson, B.H.; Mahan, C.M.; Lee, K.Y.; Murphy, F.M. Post-traumatic stress disorder and chronic fatigue syndrome-like illness among Gulf War veterans: A population-based survey of 30,000 veterans. Am. J. Epidemiol. 2003, 157, 141–148. [Google Scholar] [CrossRef] [PubMed]
- Dursa, E.K.; Reinhard, M.J.; Barth, S.K.; Schneiderman, A.I. Prevalence of a positive screen for PTSD among OEF/OIF and OEF/OIF-era veterans in a large population-based cohort. J. Trauma. Stress 2014, 27, 542–549. [Google Scholar] [CrossRef] [PubMed]
- Klemanski, D.H.; Mennin, D.S.; Borelli, J.L.; Morrissey, P.M.; Aikins, D.E. Emotion-related regulatory difficulties contribute to negative psychological outcomes in active-duty Iraq War soldiers with and without posttraumatic stress disorder. Depress. Anxiety 2012, 29, 621–628. [Google Scholar] [CrossRef]
- Smith, N.D.L.; Cottler, L.B. The epidemiology of post-traumatic stress disorder and alcohol use disorder. Alcohol Res. 2018, 39, 113–120. [Google Scholar]
- Solomon, Z.; Debby-Aharon, S.; Zerach, G.; Horesh, D. Marital adjustment, parental functioning, and emotional sharing in war veterans. J. Fam. Issues 2011, 32, 127–147. [Google Scholar] [CrossRef]
- Watkins, L.E.; Sprang, K.R.; Rothbaum, B.O. Treating PTSD: A review of evidence-based psychotherapy interventions. Front. Behav. Neurosci. 2018, 12, 258. [Google Scholar] [CrossRef]
- Goode, J.; Swift, J.K. An empirical examination of stigma toward mental health problems and psychotherapy use in veterans and active duty service members. Mil. Psychol. 2019, 31, 335–345. [Google Scholar] [CrossRef]
- Pietrzak, R.H.; Johnson, D.C.; Goldstein, M.B.; Malley, J.C.; Southwick, S.M. Perceived stigma and barriers to mental health care utilization among OEF-OIF veterans. Psychiatr. Serv. 2009, 60, 1118–1122. [Google Scholar] [CrossRef]
- Hoge, C.W.; Grossman, S.H.; Auchterlonie, J.L.; Riviere, L.A.; Milliken, C.S.; Wilk, J.E. PTSD treatment for soldiers after combat deployment: Low utilization of mental health care and reasons for dropout. Psychiatr. Serv. 2014, 65, 997–1004. [Google Scholar] [CrossRef]
- Hamblen, J.L.; Norman, S.B.; Sonis, J.H.; Phelps, A.J.; Bisson, J.I.; Nunes, V.D.; Megnin-Viggars, O.; Forbes, D.; Riggs, D.S.; Schnurr, P.P. A guide to guidelines for the treatment of posttraumatic stress disorder in adults: An update. Psychotherapy 2019, 56, 359–373. [Google Scholar] [CrossRef]
- Sonis, J.; Cook, J.M. Medication versus trauma-focused psychotherapy for adults with posttraumatic stress disorder: A systematic review and meta-analysis. Psychiatry Res. 2019, 282, 112637. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, A.F.; Sharma, M.S.; Brunoni, A.R.; Vieta, E.; Fava, G.A. The safety, tolerability and risks associated with the use of newer generation antidepressant drugs: A critical review of the literature. Psychother. Psychosom. 2016, 85, 270–288. [Google Scholar] [CrossRef] [PubMed]
- Fava, G.A.; Gatti, A.; Belaise, C.; Guidi, J.; Offidani, E. Withdrawal symptoms after selective serotonin reuptake inhibitor discontinuation: A systematic review. Psychother. Psychosom. 2015, 84, 72–81. [Google Scholar] [CrossRef]
- Zhou, W.; Benharash, P. Effects and mechanisms of acupuncture based on the principle of meridians. J. Acupunct. Meridian Stud. 2014, 7, 190–193. [Google Scholar] [CrossRef] [PubMed]
- Hui, K.K.; Liu, J.; Makris, N.; Gollub, R.L.; Chen, A.J.; Moore, C.I.; Kennedy, D.N.; Rosen, B.R.; Kwong, K.K. Acupuncture modulates the limbic system and subcortical gray structures of the human brain: Evidence from fMRI studies in normal subjects. Hum. Brain Mapp. 2000, 9, 13–25. [Google Scholar] [CrossRef]
- Kwon, C.Y.; Lee, B.; Kim, S.H. Efficacy and underlying mechanism of acupuncture in the treatment of posttraumatic stress disorder: A systematic review of animal studies. J. Clin. Med. 2021, 10, 1575. [Google Scholar] [CrossRef] [PubMed]
- Bisson, J.I.; van Gelderen, M.; Roberts, N.P.; Lewis, C. Non-pharmacological and non-psychological approaches to the treatment of PTSD: Results of a systematic review and meta-analyses. Eur. J. Psychotraumatol. 2020, 11, 1795361. [Google Scholar] [CrossRef]
- Grant, S.; Colaiaco, B.; Motala, A.; Shanman, R.; Sorbero, M.; Hempel, S. Acupuncture for the treatment of adults with posttraumatic stress disorder: A systematic review and meta-analysis. J. Trauma Dissociation 2018, 19, 39–58. [Google Scholar] [CrossRef]
- Walker, P.H.; Pock, A.; Ling, C.G.; Kwon, K.N.; Vaughan, M. Battlefield acupuncture: Opening the door for acupuncture in Department of Defense/Veteran’s Administration health care. Nurs. Outlook 2016, 64, 491–498. [Google Scholar] [CrossRef]
- Carter, K.; Olshan-Perlmutter, M. NADA protocol: Integrative acupuncture in addictions. J. Addict. Nurs. 2014, 25, 182–187, quiz 188. [Google Scholar] [CrossRef] [PubMed]
- Federman, D.G.; Radhakrishnan, K.; Gabriel, L.; Poulin, L.M.; Kravetz, J.D. Group battlefield acupuncture in primary care for veterans with pain. South. Med. J. 2018, 111, 619–624. [Google Scholar] [CrossRef] [PubMed]
- Korol, I.; Strakhova, K.; Azevedo, M.; Baumeisterm, R.H. Battlefield acupuncture: Effectiveness for treatment of acute and subacute pain in a military primary care setting. Int. J. Appl. Res. 2021, 7, 100–102. [Google Scholar] [CrossRef]
- Kim, S.H.; Kwon, C.Y.; Kim, S.T.; Han, S.Y. Ear acupuncture for posttraumatic symptoms among long-term evacuees following the 2017 Pohang earthquake: A retrospective case series study. Integr. Med. Res. 2020, 9, 100415. [Google Scholar] [CrossRef]
- Munn, Z.; Peters, M.D.J.; Stern, C.; Tufanaru, C.; McArthur, A.; Aromataris, E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med. Res. Methodol. 2018, 18, 143. [Google Scholar] [CrossRef] [PubMed]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Levac, D.; Colquhoun, H.; O’Brien, K.K. Scoping studies: Advancing the methodology. Implement. Sci. 2010, 5, 69. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Seung, H.B.; Leem, J.T.; Kwak, H.Y.; Kwon, C.Y.; Kim, S.H. Acupuncture for military veterans with posttraumatic stress disorder and related symptoms after combat exposure: Protocol for a scoping review of clinical studies. PLoS ONE 2023, 18, e0273131. [Google Scholar] [CrossRef]
- The Institutional Review Board. Case Reports and Case Series. (IRB) In Boston Medical Center and Boston University Medical Campus. Available online: https://www.bumc.bu.edu/irb/submission-requirements/special-submission-requirements/case-reports-and-case-series/ (accessed on 11 November 2022).
- King, H.C.; Spence, D.L.; Hickey, A.H.; Sargent, P.; Elesh, R.; Connelly, C.D. Auricular acupuncture for sleep disturbance in veterans with post-traumatic stress disorder: A feasibility study. Mil. Med. 2015, 180, 582–590. [Google Scholar] [CrossRef]
- Prisco, M.K.; Jecmen, M.C.; Bloeser, K.J.; McCarron, K.K.; Akhter, J.E.; Duncan, A.D.; Balish, M.S.; Amdur, R.L.; Reinhard, M.J. Group auricular acupuncture for PTSD-related insomnia in veterans: A randomized trial. Med. Acupunct. 2013, 25, 407–422. [Google Scholar] [CrossRef]
- Engel, C.C.; Cordova, E.H.; Benedek, D.M.; Liu, X.; Gore, K.L.; Goertz, C.; Freed, M.C.; Crawford, C.; Jonas, W.B.; Ursano, R.J. Randomized effectiveness trial of a brief course of Acupuncture for posttraumatic stress disorder. Med. Care 2014, 52 (Suppl. 5), S57–S64. [Google Scholar] [CrossRef] [PubMed]
- Huang, W.; Johnson, T.M.; Kutner, N.G.; Halpin, S.N.; Weiss, P.; Griffiths, P.C.; Bliwise, D.L. Acupuncture for treatment of persistent disturbed sleep: A randomized clinical trial in veterans with mild traumatic brain injury and posttraumatic stress disorder. J. Clin. Psychiatry 2018, 80, E1–E8. [Google Scholar] [CrossRef] [PubMed]
- Eisenlohr, V.; Römer, H.-W.; Zimmermann, P. Acupuncture—A new option in the therapy of traumatized German soldiers? Dtsch. Z. Akupunkt. 2010, 53, 29–34. [Google Scholar] [CrossRef]
- Cronin, C.; Conboy, L. Evaluation of the national acupuncture detoxification association protocol to treat combat stress induced insomnia. J. Altern. Complement. Med. 2013, 19, A31. [Google Scholar]
- Arhin, A.O.; Gallop, K.; Mann, J.; Cannon, S.; Tran, K.; Wang, M.C. Acupuncture as a treatment option in treating posttraumatic stress disorder–related tinnitus in war veterans: A case presentation. J. Holist. Nurs. 2016, 34, 56–63. [Google Scholar] [CrossRef]
- King, C.H.; Moore, L.C.; Spence, C.D. Exploring self-reported benefits of auricular acupuncture among veterans with posttraumatic stress disorder. J. Holist. Nurs. 2016, 34, 291–299. [Google Scholar] [CrossRef]
- Cohen, M.M.; Smit, V.; Andrianopoulos, N.; Ben-Meir, M.; Taylor, D.M.; Parker, S.J.; Xue, C.C.; Cameron, P.A. Acupuncture for analgesia in the emergency department: A multicentre, randomised, equivalence and non-inferiority trial. Med. J. Aust. 2017, 206, 494–499. [Google Scholar] [CrossRef]
- Yang, J.; Ganesh, R.; Wu, Q.; Li, L.; Ogletree, S.P.; Del Fabro, A.S.; Wahner-Roedler, D.L.; Xiong, D.; Bauer, B.A.; Chon, T.Y. Battlefield acupuncture for adult pain: A systematic review and meta-analysis of randomized controlled trials. Am. J. Chin. Med. 2021, 49, 25–40. [Google Scholar] [CrossRef]
- Benedict, T.M.; Keenan, P.G.; Nitz, A.J.; Moeller-Bertram, T. Post-traumatic stress disorder symptoms contribute to worse pain and health outcomes in veterans with PTSD compared to those without: A systematic review with meta-analysis. Mil. Med. 2020, 185, e1481–e1491. [Google Scholar] [CrossRef]
- Weathers, F.; Huska, J.; Keane, T. The PTSD Checklist Military Version (PCL-M); National Center for PTSD: Boston, MA, USA, 1991; p. 42. [Google Scholar] [CrossRef]
- Yarberry, M. The Use of the NADA Protocol for PTSD in Kenya. Dtsch. Z. Akupunkt. 2010, 53, 6–11. [Google Scholar] [CrossRef]
- Arai, Y.C.; Sakakima, Y.; Kawanishi, J.; Nishihara, M.; Ito, A.; Tawada, Y.; Maruyama, Y. Auricular acupuncture at the “shenmen” and “point zero” points induced parasympathetic activation. Evid. Based Complement. Altern. Med. 2013, 2013, 945063. [Google Scholar] [CrossRef] [PubMed]
- Xu, S.F.; Wang, L.Z.; Cooper, E.; Zhang, M.; Manheimer, E.; Berman, B.; Shen, X.Y.; Lao, L.X. Adverse events of acupuncture: A systematic review of case reports. Evid. Based Complement. Altern. Med. 2013, 2013, 581203. [Google Scholar] [CrossRef] [PubMed]
- Melchart, D.; Weidenhammer, W.; Streng, A.; Reitmayr, S.; Hoppe, A.; Ernst, E.; Linde, K. Prospective investigation of adverse effects of acupuncture in 97,733 patients. Arch. Intern. Med. 2004, 164, 104–105. [Google Scholar] [CrossRef]
- Tan, J.Y.; Molassiotis, A.; Wang, T.; Suen, L.K. Adverse events of auricular therapy: A systematic review. Evid. Based Complement. Altern. Med. 2014, 2014, 506758. [Google Scholar] [CrossRef]
- Giese, N.; Heirs, M.K. Development of provisional acupuncture guidelines for pelvic pain in endometriosis using an e-Delphi consensus process. J. Integr. Complement. Med. 2023, 29, 169–180. [Google Scholar] [CrossRef]
- Hellhammer, D.H.; Wüst, S.; Kudielka, B.M. Salivary cortisol as a biomarker in stress research. Psychoneuroendocrinology 2009, 34, 163–171. [Google Scholar] [CrossRef]
- Stein, P.K.; Pu, Y. Heart rate variability, sleep and sleep disorders. Sleep Med. Rev. 2012, 16, 47–66. [Google Scholar] [CrossRef]
- Song, C.; Boly, M.; Tagliazucchi, E.; Laufs, H.; Tononi, G. fMRI spectral signatures of sleep. Proc. Natl. Acad. Sci. USA 2022, 119, e2016732119. [Google Scholar] [CrossRef]
- Rundo, J.V.; Downey, R., III. Polysomnography. Handb. Clin. Neurol. 2019, 160, 381–392. [Google Scholar] [CrossRef]
- Russell, L.B.; Gold, M.R.; Siegel, J.E.; Daniels, N.; Weinstein, M.C. The role of cost-effectiveness analysis in health and medicine. Panel on Cost-Effectiveness in Health and Medicine. JAMA 1996, 276, 1172–1177. [Google Scholar] [CrossRef] [PubMed]
| Study (Country) | Design | Sample Size (Included →Analyzed) | Mean Age (Range) (Years) | Sex (Male/Female) | Population (Diagnostic Tool) | Affiliation and Rank |
|---|---|---|---|---|---|---|
| King 2015 (USA) [32] | RCT | 29 (15:14)→20 (12:8) | 33.3 ± 6.1/32.8 ± 9.2 | 29:0 | OEF/OIF veterans with PTSD (DSM-IV) | Active-duty Enlisted 18 Officer 2 |
| Prisco 2013 (USA) [33] | RCT | 35 (12:12:11)→25 (8:8:9) | 37.8 ±11.4/37.9 ± 10.3/37.6 ± 8.0 | 25:10 | OEF/OIF Veterans suffered from PTSD-related insomnia(DSM-IV-TR) | Enlisted 29 Officer 4 Warrant officer 2 |
| Engel 2014 (USA) [34] | RCT | 55 (28:27)→55 (28:27) | 37.2 ± 11.3/32.6 ± 8.3 | 38:17 | PTSD (DSM-IV) | Active duty Enlisted 39 |
| Huang 2019 (USA) [35] | RCT | 60 (30:30)→55 (27:28)→52 (25:27) | 40.7 ± 10.8/40.3 ± 10.1 | 46:14 | mTBI, PTSD (subgroup analysis) | Veterans receiving care from the Atlanta VAMC(Atlanta Veterans Affairs Medical Center) TBI clinic |
| Eisenloh 2010 (Germany) [36] | Before-after study | 27→25 | 32.96 ± 9.66 | 21:6 | History of trauma-related experiences (ICD-10) | Service women and men of the Bundeswehr Non-commissioned officers 15 Officer 6 Enlisted 6 |
| Cronin 2013 (USA) [37] | Before-after study | 5→5 | 29–48 | 3:2 | Participants in the Veterans Sustainable Agriculture Training Program (VSAT). Four had combat experience and one had military sexual assault trauma. PTSD diagnosis was made in 4 people except 1 veteran | Army medic 1 Navy corpsman 1 Did not disclose their former military jobs 2 Who had experienced military sexual trauma 1 |
| Arhin 2016 (USA) [38] | Case series | 3→3 | 41–59 | 3:0 | Patient of PTSD with tinnitus | NR |
| King 2016 (USA) [39] | Qualitative study | 17→17 | 18–49 | 17:0 | PTSD (DSM-IV) | Active-duty military personnel Marine 8 Navy 6 Army 3 |
| Study (Country) | Sample Size (Included →Analyzed) | (A) Treatment Intervention | (B) Control Intervention | Duration of Treatment/Follow Up | Outcome | Results Reported | Adverse Events Reported |
|---|---|---|---|---|---|---|---|
| King, 2015 (USA) [32] | 29 (15:14)→20 (12:8) | Auricular acupuncture | Waiting list control | 3 weeks | (1-1) Actigraphy- SOL (1-2) WASO (1-3) Sleep Efficiency (%) (1-4) NOA (1-5) Total Sleep Time (2-1) Consensus Sleep Diary-SOL (2-2) WASO (2-3) Sleep Efficiency(%) (2-4) NOA (2-5) Total Sleep Time (3) PCL-M (4) PHQ-9 (5-1)PSQI- Sleep quality (5-2) sleep latency (5-3) sleep duration (5-4) sleep efficiency (5-5) sleep disturbance (5-6) sleep medication (5-7) daytime dysfunction | (1-1) N.S (1-2) N.S (1-3) N.S (1-4) N.S (1-5) N.S (2-1) N.S (2-2) N.S (2-3) N.S (2-4) N.S (2-5) N.S (3) N.S (4) N.S (5-1) A) > (B) ++ (5-2) N.S (5-3) N.S (5-4) N.S (5-5) N.S (5-6) N.S (5-7) (A) > (B) ++ | (A): 1 fall down. (B): 2 alcohol-related events, 1 wrist injury, 1 incident of suicidal ideation. |
| Prisco, 2013 (USA) [33] | 35 (12:12:11)→25 (8:8:9) | (a) Auricular acupuncture | (b) Sham auricular acupuncture (c) WTL | 2 months | (1-1) MSD—refreshness rating (1-2) soundness rating (2) ISI -Total Score (3-1) MSD—TST (3-2) SL (3-3) SE (3-4) Naps (4-1) Actigraphy—TST (4-2) SL (4-3) SE (4-4) Naps | (1-1) N.S (1-2) N.S (2) (a) > (b),(c) + after 1 month, N.S after 2 month (3-1) N.S (3-2) N.S (3-3) N.S (3-4) N.S (4-1) N.S (4-2) N.S (4-3) N.S (4-4) N.S | (a): dropped out due to discomfort with acupuncture (b),(c): none |
| Engel, 2014 (USA) [34] | 55 (28:27)→55 (28:27) | Manual acupuncture + Usual PTSD care | Usual PTSD Care | 4 weeks | (1) PCL (2) CAPS (3) NRS (4) BDI (5-1) SF-36 PCS (5-2) MCS | (1) (A) > (B) ++ (2) (A) > (B) + (3) (A) > (B) ++ (4) (A) > (B) ++ (5-1) (A) > (B) ++ (5-2) (A) > (B) ++ | (A), (B): None |
| Huang, 2019 (USA) [35] | 60 (30:30)→55 (27:28)→52 (25:27) | Manual acupuncture | Sham meridian acupuncture | 1 month | (1) PSQI global score (2) Actigraphy sleep efficiency | (1) (A) > (B) ++ (2) (A) > (B) + PTSD status did not interact with this effect. | NR |
| Study (Country) | Sample Size (Included →Analyzed) | Treatment Intervention | Duration of Treatment/Follow Up | Outcome | Results Reported | Adverse Events Reported |
|---|---|---|---|---|---|---|
| Eisenlohr 2010 [36] | 27→25 | Manual acupuncture + Auricular acupuncture | NR | (1) Subjective trauma-related symptoms (1-1) Sleep disorder (1-2) Restlessness (1-3) Agitation (1-4) Frightfulness (1-5) Aggression | (1-1) post treatment: improved * (1-2) post treatment: improved * (1-3) post treatment: improved * (1-4) post treatment: improved * (1-5) post treatment: improved * | Excessive sleep, drunken feeling; All improved after excluding specific acupoint. |
| Cronin 2013 (USA) [37] | 5→5 | Manual acupuncture | 5 days/2 weeks | (1) PSQI (2) PCL-M | (1) post treatment: improved + follow up: improved + (2) post treatment: improved + follow up: improved + | NR |
| Study (Country) | Sample Size (Included →Analyzed) | Treatment Intervention | Duration of Treatment/Follow Up | Outcome | Results Reported |
|---|---|---|---|---|---|
| Arhin 2016 (USA) [38] | 3→3 | Manual acupuncture | Various | Subjective statement of the degree of improvement in tinnitus | In all cases, tinnitus improved after acupuncture, and preference for the treatment procedure had been identified. Associated PTSD symptoms also improved. |
| Study (Country) | Sample Size (Included →Analyzed) | Treatment Intervention | Duration of Treatment/Follow Up | Extracted Key Themes | Major Specific Statements |
|---|---|---|---|---|---|
| King 2016 (USA) [39] | 17→17 | Auricular acupuncture | 3 weeks | (1) improved sleep (2) increased relaxation (3) decreased pain (4) loved/liked the auricular acupuncture treatments | (1) Ability to fall asleep faster, stay asleep longer, fall asleep during auricular acupuncture treatments, and experience fewer nightmares, improvement of daytime functioning (2) Increased relaxation both during and after receiving the auricular acupuncture treatments. (3) Improvements in low back pain, hip pain, neck pain, and headache (4) participant “loved” and “liked” the treatment and no negative written comments were found |
| Study ID | Acupuncture Rationale | Practitioner Background | Details of Needling | Treatment Regimen | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Type of Acupuncture | Number of Needle Insertions Per Participant Per Session | Location Of Points Used | Depth of Insertion | Response Sought | Needle Type | Number of Treatment Sessions | Frequency and Duration of Treatment Sessions | |||
| Diameter, Length, and Manufacturer or Material | ||||||||||
| King, 2015 [32] | Acupoint selection was based on review of previous AA insomnia studies and expert opinion. | Privileged military acupuncture provider, who had 2 years of clinical experience (over 500 treatments). | Auricular Acupuncture | 24 | Shenmen, Zero point, Brain, Thalamus Point, Pineal Gland, Master Cerebral, Insomnia 1, 2; Kidney C, Heart C, Occiput, Forehead. | NR | NR | 0.20 mm diameter, 15 mm in length, D type needles, SEIRIN Corporation, Shizuoka, Japan) | 9 | 30 min 3 times/week |
| Cronin 2013 [37] | NADA protocol | NR | Auricular Acupuncture | 12 | Shenmen, Sympathetic, Kidney, Liver and Lung/Heart | NR | NR | Seirin D-Type needles (40 gauge—red) | 5 | 45 min 1 time/day |
| Prisco 2013 [32,39] | Using a Traditional Chinese Medicine (TCM) map as a guide, Selection of the points was based on acupuncture interventions for insomnia and the study acupuncturist’s experience with OEF/OIF veterans with PTSD-related insomnia. | All acupuncture services were performed in accordance with the established principles and practices of the National Certification Commission for Acupuncture and Oriental Medicine. | Auricular Acupuncture | 10 | Shenmen, Sympathetic, Kidney, Liver, Hippocampus | Needles inserted straight, reached the ear cartilage and to a depth where the needle could stand by itself. No guide tube used. | no needle manipulation. | DBC Brand Spring Handle Needles, size 0.16 × 15 mm | 16 | 2 times/week 2 months |
| King 2016 [38] | Same as King, et al. [27] | Military nurse with supple- mental privileges to perform auricular acupuncture and had 2 years of clinical experience performing auricular acupuncture treatments. | Auricular Acupuncture | 24 | Shenmen, Zero point, Brain, Thalamus Point, Pineal Gland, Master Cerebral, Insomnia 1, 2; Kidney C, Heart C, Occiput, Forehead. | NR | NR | 0.20 mm diameter, 15 mm in length, D type needles, SEIRIN Corporation, Shizuoka, Japan) | 9 | 30 min 3 times/week |
| Eisenlohr 2010 [35] | NR | Trained acupuncturist with B diploma and 10 years of experience | Manual Acupuncture | NR | GV20, HT5, 7; ST23, SP6; LR3, PC6, 7; BL62, Extra point Anmian 1, 2; Extra point KH1; PT1, 2. | NR | NR | Cloud&Dragon 0.30 × 30 mm + 0.20 × 15 mm; Permanent needles Sedatelec ASP steel with stimulation magnet | NR | 35 min 2–3 times/week |
| Arhin 2016 [37] | Korean four-needle technique | NR | Manual Acupuncture | 4 | NR | NR | NR | NR | 4–6 | 1 time/2 weeks |
| Engel 2014 [33] | First 4 sessions were standardized for all participants, and the last 4 sessions allowed acupuncturists flexibility to individualize based on standard diagnostic criteria (pulse, tongue, symptoms, color, odor, etc). | Acupuncturists were licensed, practicing regularly, and recipients of advanced degrees (M.Ac.) from the Tai Sophia Institute for the Healing Arts, a program emphasizing traditional Chinese medicine philosophies and using 5 elements theory as overall guide to treatment. | Manual Acupuncture + Auricular Acupuncture | NR | BL 13, 14, 15, 18, 20, 23; LR 3; LI4; HT5, 7; PC 6; KI3, 9; Ren 4, 15; Du 24; Ear Shenmen; Yintang. (Used at least 1 time) | NR | NR | Seirin brand, J type: 0.14, 0.16, and 0.2 mm and L type: 0.2 mm | 8 | 15–30 min (depending on point prescription) 2 times/week |
| Huang 2019 [34] | Most commonly used acupoints in prior sleep studies for treatments | Board-certified physiatrist with advanced training in acupuncture | Meridian Acupuncture + Auricular Acupuncture | Various | Auricular shenmen, PC-6, SP-6; Other points are selected according to standardized principles according to the symptoms of the therapist. | NR | no needle manipulation. | Sterile, 34-gauge single-use disposable metal real or sham acupuncture needles | 6–10 | 30 min 2 times/week |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kwak, H.-Y.; Leem, J.; Seung, H.-b.; Kwon, C.-Y.; Jeong, H.-S.; Kim, S.-H. Acupuncture Therapy for Military Veterans Suffering from Posttraumatic Stress Disorder and Related Symptoms: A Scoping Review of Clinical Studies. Healthcare 2023, 11, 2957. https://doi.org/10.3390/healthcare11222957
Kwak H-Y, Leem J, Seung H-b, Kwon C-Y, Jeong H-S, Kim S-H. Acupuncture Therapy for Military Veterans Suffering from Posttraumatic Stress Disorder and Related Symptoms: A Scoping Review of Clinical Studies. Healthcare. 2023; 11(22):2957. https://doi.org/10.3390/healthcare11222957
Chicago/Turabian StyleKwak, Hui-Yong, Jungtae Leem, Hye-bin Seung, Chan-Young Kwon, Hye-Seon Jeong, and Sang-Ho Kim. 2023. "Acupuncture Therapy for Military Veterans Suffering from Posttraumatic Stress Disorder and Related Symptoms: A Scoping Review of Clinical Studies" Healthcare 11, no. 22: 2957. https://doi.org/10.3390/healthcare11222957
APA StyleKwak, H.-Y., Leem, J., Seung, H.-b., Kwon, C.-Y., Jeong, H.-S., & Kim, S.-H. (2023). Acupuncture Therapy for Military Veterans Suffering from Posttraumatic Stress Disorder and Related Symptoms: A Scoping Review of Clinical Studies. Healthcare, 11(22), 2957. https://doi.org/10.3390/healthcare11222957







