Effectiveness of Palliative Care before Death in Reducing Emergency Care Utilization for Patients with Terminal Cancer and Trends in the Utilization of Palliative Care from 2005–2018
Abstract
1. Introduction
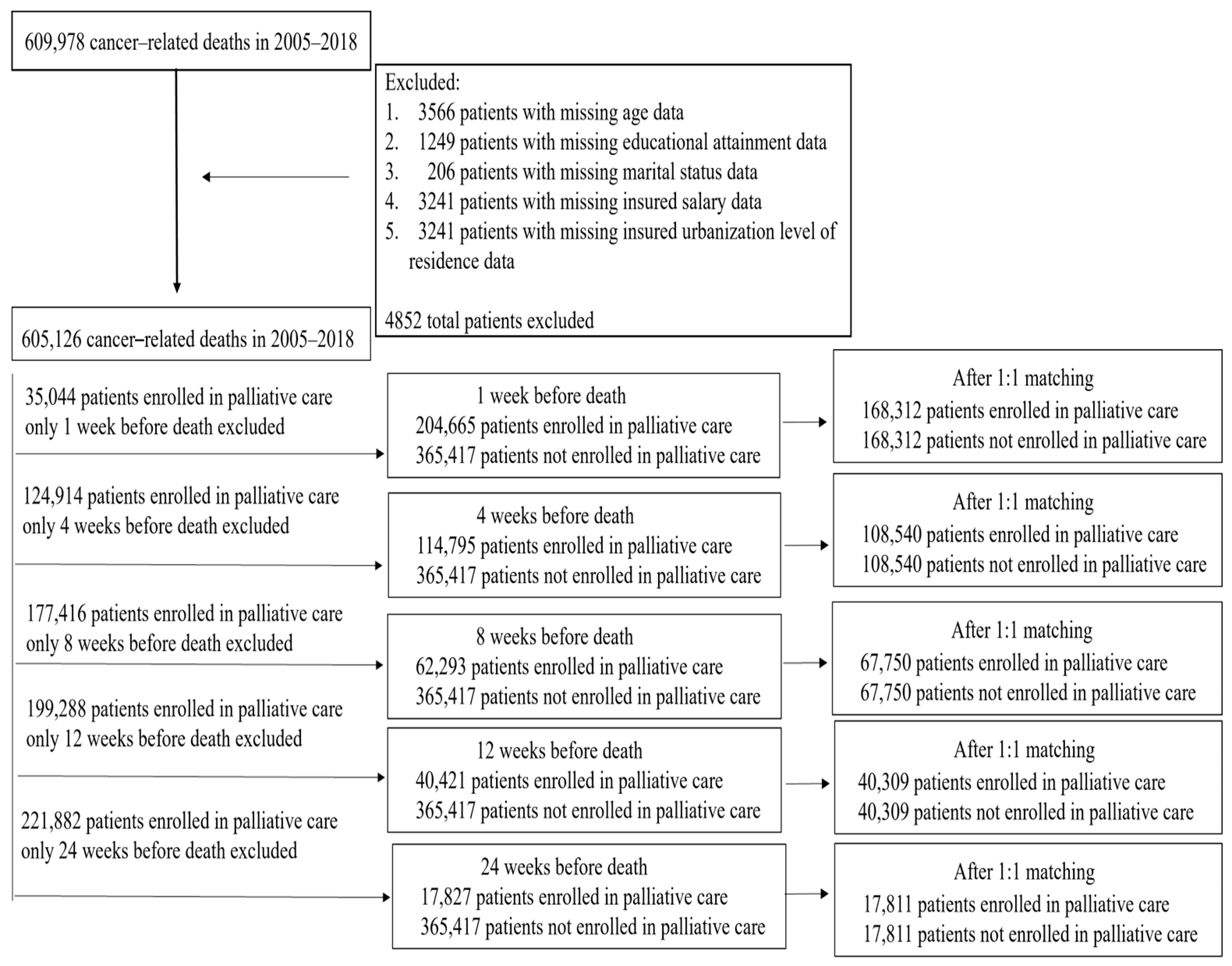
2. Materials and Methods
2.1. Data Sources and Participants
2.2. Variables Description
2.3. Statistical Analysis
3. Results
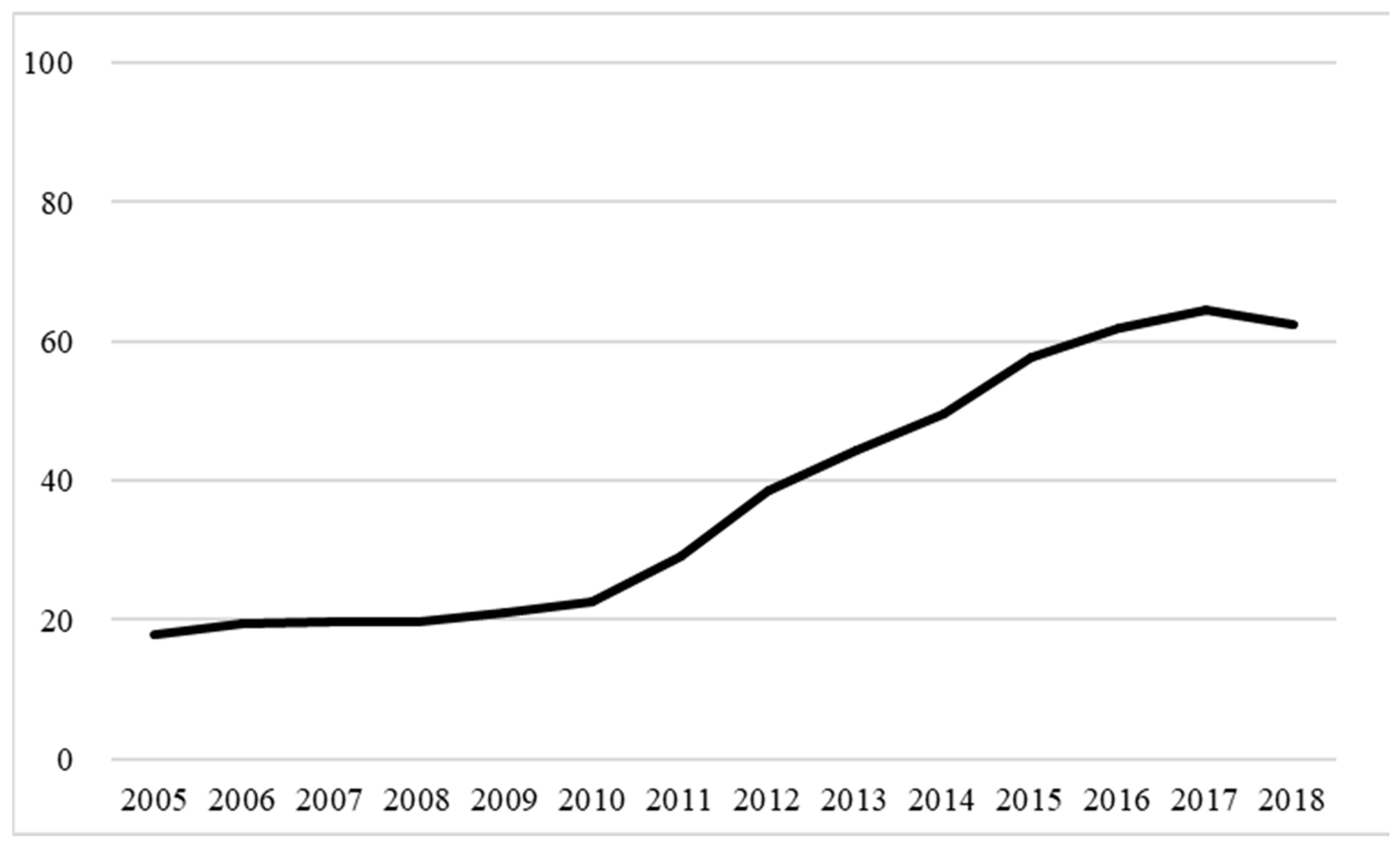
3.1. Utilization and Trends of Palliative Care for Patients with Terminal Cancer before Death
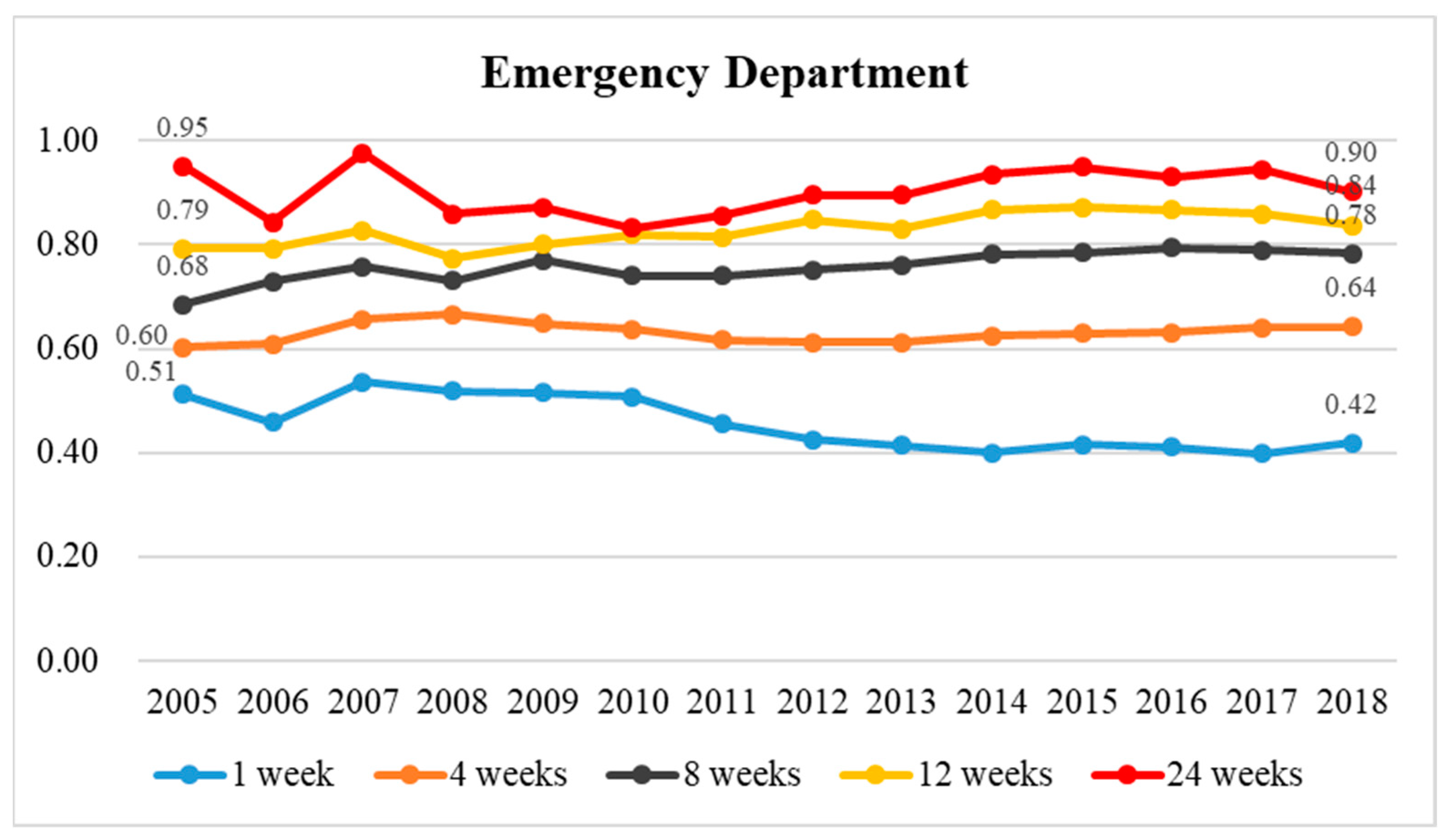
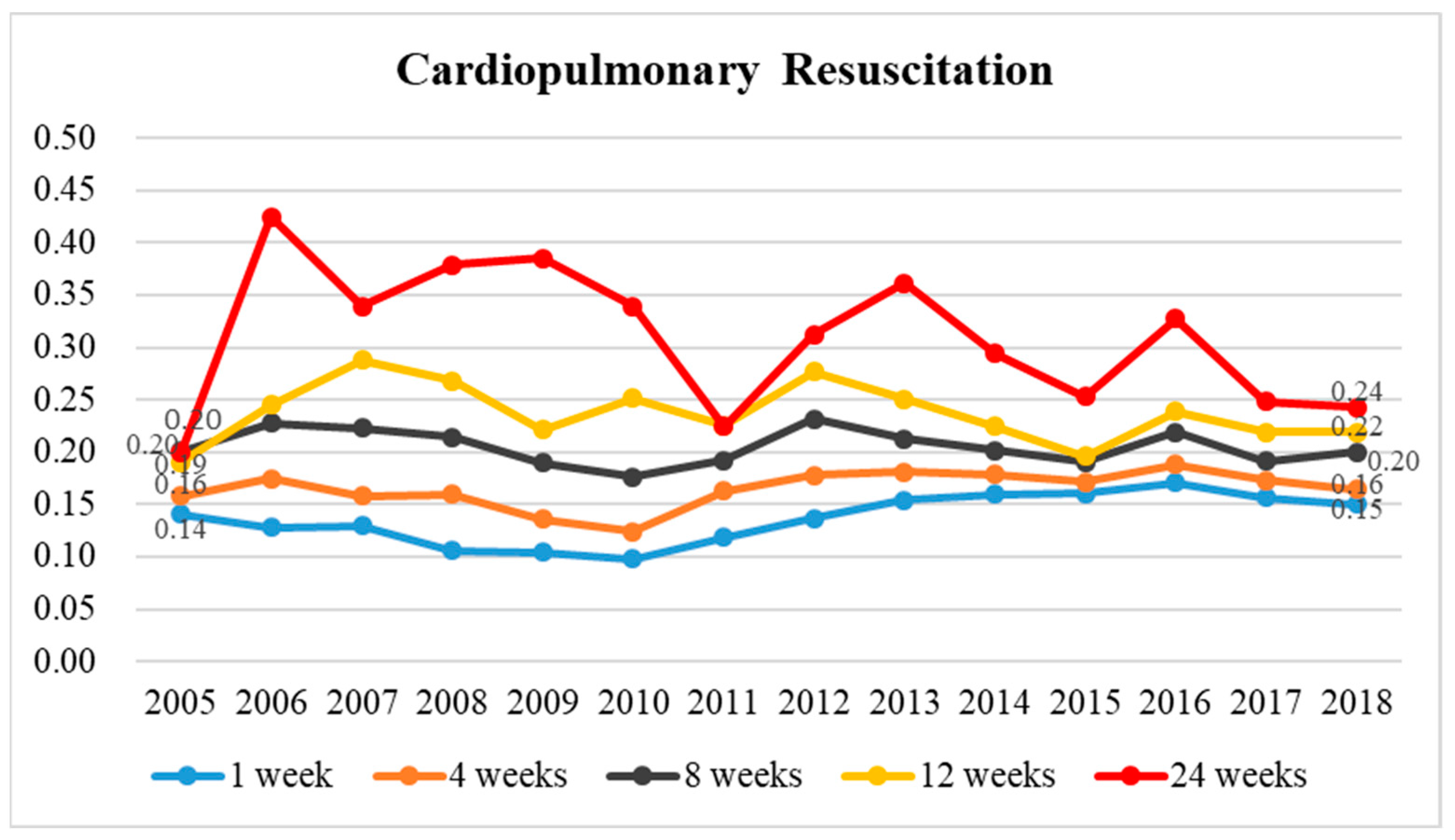
3.2. Comparison of Differences in Emergency Care Utilization, CPR, ICU Admission, and Intubation among the Two Groups
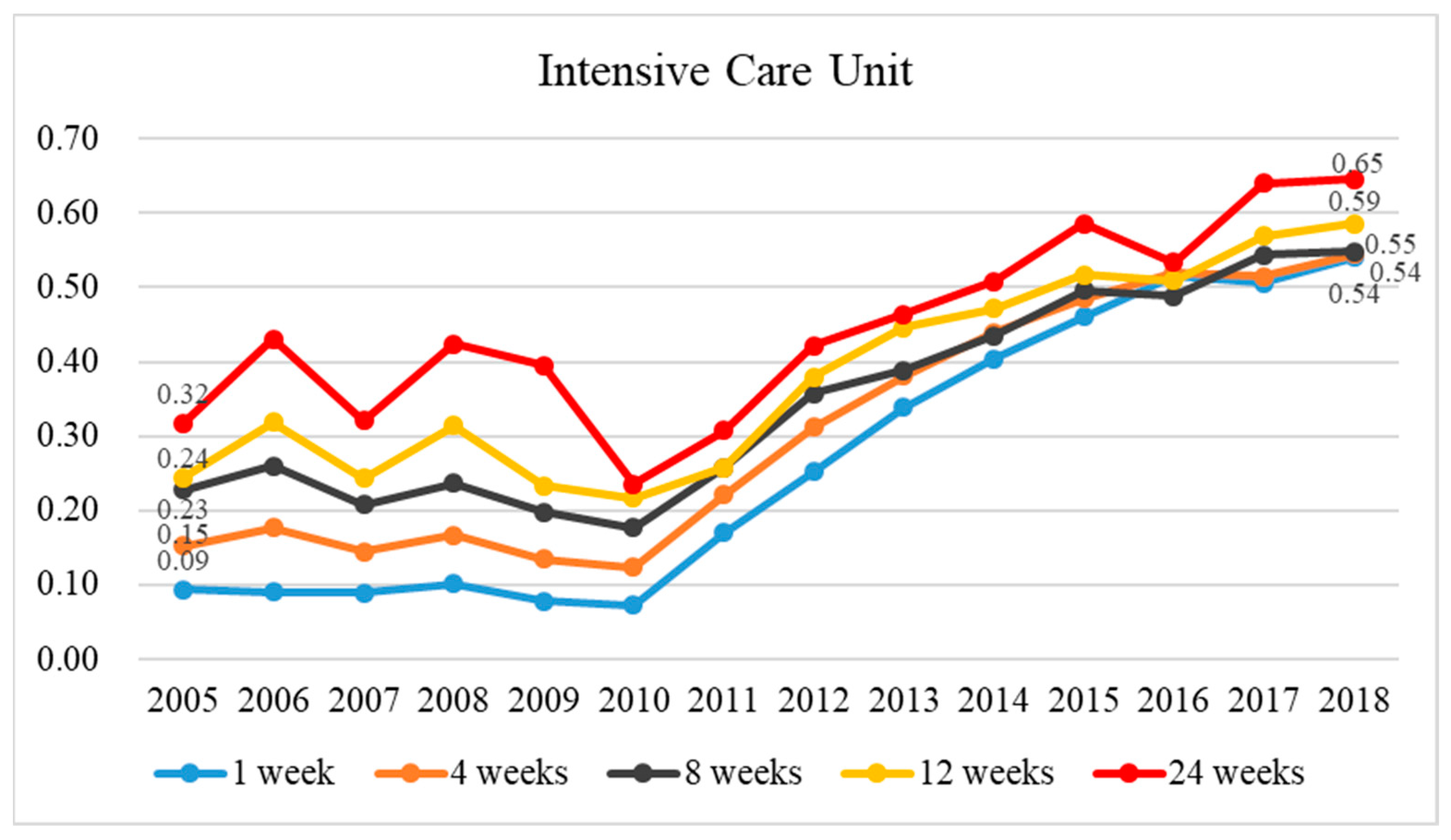
3.3. Yearly Trends in the Differences in Palliative Care with Respect to Emergency Care Utilization, CPR, ICU Admission, and Intubation
4. Discussion
Limitations of the Study
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Cancer. 2022. Available online: https://www.who.int/news-room/fact-sheets/detail/cancer (accessed on 3 February 2022).
- Atun, R.; Cavalli, F. The global fight against cancer: Challenges and opportunities. Lancet 2018, 391, 412–413. [Google Scholar] [CrossRef] [PubMed]
- Claessen, S.J.; Francke, A.L.; Echteld, M.A.; Schweitzer, B.P.; Donker, G.A.; Deliens, L. GPs’ Recognition of Death in the Foreseeable Future and Diagnosis of a Fatal Condition: A National Survey. BMC Fam. Pract. 2013, 14, 104. [Google Scholar] [CrossRef]
- Seow, H.; O’Leary, E.; Perez, R.; Tanuseputro, P. Access to Palliative Care by Disease Trajectory: A Population-Based Cohort of Ontario Decedents. BMJ Open 2018, 8, e021147. [Google Scholar] [CrossRef]
- Teno, J.M.; Gozalo, P.; Trivedi, A.N.; Bunker, J.; Lima, J.; Ogarek, J.; Mor, V. Site of Death, Place of Care, and Health Care Transitions among US Medicare Beneficiaries, 2000–2015. JAMA 2018, 320, 264–271. [Google Scholar] [CrossRef] [PubMed]
- Loke, S.-S.; Rau, K.-M.; Huang, C.-F. Impact of Combined Hospice Care on Terminal Cancer Patients. J. Palliat. Med. 2011, 14, 683–687. [Google Scholar] [CrossRef]
- Alsirafy, S.A.; Raheem, A.A.; Al-Zahrani, A.S.; Mohammed, A.A.; Sherisher, M.A.; El-Kashif, A.T.; Ghanem, H.M. Emergency Department Visits at the End of Life of Patients with Terminal Cancer: Pattern, Causes, and Avoidability. Am. J. Hosp. Palliat. Med. 2015, 33, 658–662. [Google Scholar] [CrossRef]
- Delgado-Guay, M.O.; Rodriguez-Nunez, A.; Shin, S.H.; Chisholm, G.; Williams, J.; Frisbee-Hume, S.; Bruera, E. Characteristics and Outcomes of Patients with Advanced Cancer Evaluated by a Palliative Care Team at an Emergency Center. A retrospective study. Support. Care Cancer 2015, 24, 2287–2295. [Google Scholar] [CrossRef]
- Earle, C.C.; Park, E.R.; Lai, B.; Weeks, J.C.; Ayanian, J.Z.; Block, S. Identifying Potential Indicators of the Quality of End-of-Life Cancer Care from Administrative Data. J. Clin. Oncol. 2003, 21, 1133–1138. [Google Scholar] [CrossRef]
- Grunfeld, E.; Urquhart, R.; Mykhalovskiy, E.; Folkes, A.; Johnston, G.; Burge, F.I.; Earle, C.C.; Dent, S. Toward Population-Based Indicators of Quality End-of-Life Care: Testing Stakeholder Agreement. Cancer 2008, 112, 2301–2308. [Google Scholar] [CrossRef]
- Cardona-Morrell, M.; Kim, J.; Turner, R.; Anstey, M.; Mitchell, I.; Hillman, K. Non-Beneficial Treatments in Hospital at the End of Life: A Systematic Review on Extent of the Problem. Int. J. Qual. Health Care 2016, 28, 456–469. [Google Scholar] [CrossRef] [PubMed]
- Luta, X.; Maessen, M.; Egger, M.; Stuck, A.E.; Goodman, D.; Clough-Gorr, K.M. Measuring Intensity of End of Life Care: A Systematic Review. PLoS ONE 2015, 10, e0123764. [Google Scholar] [CrossRef]
- Tang, S.T.; Wu, S.-C.; Hung, Y.-N.; Huang, E.-W.; Chen, J.-S.; Liu, T.-W. Trends in Quality of End-of-Life Care for Taiwanese Cancer Patients Who Died in 2000–2006. Ann. Oncol. 2009, 20, 343–348. [Google Scholar] [CrossRef] [PubMed]
- Lorenz, K.A.; Lynn, J.; Dy, S.M.; Shugarman, L.R.; Wilkinson, A.; Mularski, R.A.; Morton, S.C.; Hughes, R.G.; Hilton, L.K.; Maglione, M.; et al. Evidence for Improving Palliative Care at the End of Life: A Systematic Review. Ann. Intern. Med. 2008, 148, 147–159. [Google Scholar] [CrossRef] [PubMed]
- Temel, J.S.; Greer, J.A.; Muzikansky, A.; Gallagher, E.R.; Admane, S.; Jackson, V.A.; Dahlin, C.M.; Blinderman, C.D.; Jacobsen, J.; Pirl, W.F.; et al. Early Palliative Care for Patients with Metastatic Non–Small-Cell Lung Cancer. N. Engl. J. Med. 2010, 363, 733–742. [Google Scholar] [CrossRef]
- Billiot, A.A.; Danos, D.M.; Stevens, J.; Vance, K.M.; Raven, M.C.; Lyons, J.M. Palliative Care Reduces Emergency Room Visits and Total Hospital Days among Patients with Metastatic HPB and GI Cancers. Sci. Rep. 2022, 12, 21068. [Google Scholar] [CrossRef] [PubMed]
- Amado-Tineo, J.P.; Oscanoa-Espinoza, T.; Vásquez-Alva, R.; Huari-Pastrana, R.; Delgado-Guay, M.O. Emergency Department Use by Terminally Ill Patients: A Systematic Review. J. Pain Symptom Manag. 2020, 61, 531–543. [Google Scholar] [CrossRef]
- Dunn, E.J.; Markert, R.; Hayes, K.; McCollom, J.; Bains, L.; Kahlon, D.; Kumar, G. The Influence of Palliative Care Consultation on Health-Care Resource Utilization During the Last 2 Months of Life: Report from an Integrated Palliative Care Program and Review of the Literature. Am. J. Hosp. Palliat. Med. 2016, 35, 117–122. [Google Scholar] [CrossRef]
- Kao, C.-Y.; Wang, H.-M.; Tang, S.-C.; Huang, K.-G.; Jaing, T.-H.; Liu, C.-Y.; Liu, K.-H.; Shen, W.-C.; Wu, J.-H.; Hung, Y.-S.; et al. Predictive Factors for Do-Not-Resuscitate Designation among Terminally Ill Cancer Patients Receiving Care from a Palliative Care Consultation Service. J. Pain Symptom Manag. 2014, 47, 271–282. [Google Scholar] [CrossRef]
- Wang, J.P.; Wu, C.-Y.; Hwang, I.-H.; Kao, C.-H.; Hung, Y.-P.; Hwang, S.-J.; Li, C.-P. How Different Is the Care of Terminal Pancreatic Cancer Patients in Inpatient Palliative Care Units and Acute Hospital Wards? A Nationwide Population-Based Study. BMC Palliat. Care 2016, 15, 1. [Google Scholar] [CrossRef]
- Welfare, Ministry of Health and Palliative Care. 2021. Available online: https://www.hpa.gov.tw/Pages/List.aspx?nodeid=210 (accessed on 25 August 2021).
- Wang, H.-M.; Koong, S.L.; Hsiao, S.C.; Chen, J.-S.; Liu, T.-W.; Tang, S.T. Impact of Availability of an Inpatient Hospice Unit on the Parent Hospital’s Quality of Palliative Care for Taiwanese Cancer Decedents, 2001–2006. J. Pain Symptom Manag. 2011, 42, 400–409. [Google Scholar] [CrossRef] [PubMed]
- Kao, Y.-H.; Chiang, J.-K. Effect of Hospice Care on Quality Indicators of End-of-Life Care among Patients with Liver Cancer: A National Longitudinal Population-Based Study in Taiwan 2000-2011. BMC Palliat. Care 2015, 14, 39. [Google Scholar] [CrossRef] [PubMed]
- Hui, D.; Kim, S.H.; Roquemore, J.; Dev, R.; Chisholm, G.; Bruera, E. Impact of Timing and Setting of Palliative Care Referral on Quality of End-of-Life Care in Cancer Patients. Cancer 2014, 120, 1743–1749. [Google Scholar] [CrossRef] [PubMed]
- Scibetta, C.; Kerr, K.; Mcguire, J.; Rabow, M.W. The Costs of Waiting: Implications of the Timing of Palliative Care Consultation among a Cohort of Decedents at a Comprehensive Cancer Center. J. Palliat. Med. 2016, 19, 69–75. [Google Scholar] [CrossRef] [PubMed]
- Ferrell, B.R.; Temel, J.S.; Temin, S.; Alesi, E.R.; Balboni, T.A.; Basch, E.M.; Firn, J.I.; Paice, J.A.; Peppercorn, J.M.; Phillips, T.; et al. Integration of Palliative Care Into Standard Oncology Care: American Society of Clinical Oncology Clinical Practice Guideline Update. J. Clin. Oncol. 2017, 35, 96–112. [Google Scholar] [CrossRef]
- Liu, C.Y.; Hung, Y.T.; Chuang, Y.L.; Chen, Y.J.; Weng, W.S.; Liu, J.S.; Liang, K.Y. Incorporating Development Stratification of Taiwan Townships into Sampling Design of Large Scale Health Interview Survey. J. Health Manag. 2006, 4, 1–22. [Google Scholar] [CrossRef]
- Deyo, R.A.; Cherkin, D.C.; Ciol, M.A. Adapting a Clinical Comorbidity Index for Use with ICD-9-CM Administrative Databases. J. Clin. Epidemiol. 1992, 45, 613–619. [Google Scholar] [CrossRef] [PubMed]
- Hill, A.D.; Stukel, T.A.; Fu, L.; Scales, D.C.; Laupacis, A.; Rubenfeld, G.D.; Wunsch, H.; Downar, J.; Rockwood, K.; Heyland, D.K.; et al. Trends in Site of Death and Health Care Utilization at the End of Life: A Population-Based Cohort Study. CMAJ Open 2019, 7, E306–E315. [Google Scholar] [CrossRef]
- Bhulani, N.; Gupta, A.; Gao, A.; Li, J.; Guenther, C.; Ahn, C.; Paulk, E.; Houck, S.; Beg, M.S. Palliative Care and End-of-Life Health Care Utilization in Elderly Patients with Pancreatic Cancer. J. Gastrointest. Oncol. 2018, 9, 495–502. [Google Scholar] [CrossRef]
- Romano, A.M.; Gade, K.E.; Nielsen, G.; Havard, R.; Harrison, J.H.; Barclay, J.; Stukenborg, G.J.; Read, P.W.; Blackhall, L.J.; Dillon, P.M. Early Palliative Care Reduces End-of-Life Intensive Care Unit (ICU) Use but Not ICU Course in Patients with Advanced Cancer. Oncologist 2017, 22, 318–323. [Google Scholar] [CrossRef]
- Vranas, K.C.; Lapidus, J.A.; Ganzini, L.; Slatore, C.G.; Sullivan, D.R. Association of Palliative Care Use and Setting with Health-care Utilization and Quality of Care at the End of Life among Patients with Advanced Lung Cancer. Chest 2020, 158, 2667–2674. [Google Scholar] [CrossRef] [PubMed]
- Jang, R.W.; Krzyzanowska, M.K.; Zimmermann, C.; Taback, N.; Alibhai, S.M.H. Palliative Care and the Aggressiveness of End-of-Life Care in Patients with Advanced Pancreatic Cancer. JNCI J. Natl. Cancer Inst. 2015, 107, dju424. [Google Scholar] [CrossRef] [PubMed]
- Liu, Q.; Qin, M.; Zhou, J.; Zheng, H.; Liu, W.; Shen, Q. Can Primary Palliative Care Education Change Life-Sustaining Treatment Intensity of Older Adults at the End of Life? A Retrospective Study. BMC Palliat. Care 2021, 20, 84. [Google Scholar] [CrossRef]
- Lu, C.-Y.; Shen, W.-C.; Kao, C.-Y.; Wang, H.-M.; Tang, S.-C.; Chin, T.-L.; Chi, C.-C.; Yang, J.-M.; Chang, C.-W.; Lai, Y.-F.; et al. Impact of Palliative Care Consultation Service on Terminally Ill Cancer Patients: A 9-Year Observational Cohort Study in Taiwan. Medicine 2016, 95, e2981. [Google Scholar] [CrossRef] [PubMed]
- Mayer, D.K.; Travers, D.; Wyss, A.; Leak, A.; Waller, A. Why Do Patients with Cancer Visit Emergency Departments? Results of a 2008 Population Study in North Carolina. J. Clin. Oncol. 2011, 29, 2683–2688. [Google Scholar] [CrossRef]
- Lee, Y.-H.; Chu, D.; Yang, N.-P.; Chan, C.-L.; Cheng, S.-P.; Pai, J.-T.; Chang, N.-T. Emergency Visits among End-of-Life Cancer Patients in Taiwan: A Nationwide Population-Based Study. BMC Palliat. Care 2015, 14, 25. [Google Scholar] [CrossRef]
- Choi, Y.; Keam, B.; Kim, T.M.; Lee, S.-H.; Kim, D.-W.; Heo, D.S. Cancer Treatment near the End-of-Life Becomes More Aggressive: Changes in Trend during 10 Years at a Single Institute. Cancer Res. Treat. 2015, 47, 555–563. [Google Scholar] [CrossRef][Green Version]

| 1 Week before Death | 4 Weeks before Death | 8 Weeks before Death | 12 Weeks before Death | 24 Weeks before Death | |||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Utilization of Healthcare Resources | χ2 | Utilization of Healthcare Resources | χ2 | Utilization of Healthcare Resources | χ2 | Utilization of Healthcare Resources | χ2 | Utilization of Healthcare Resources | χ2 | ||||||||||||||||
| Variable | N | % | n1 | % | p-Value | N | % | n1 | % | p-Value | N | % | n1 | % | p-Value | N | % | n1 | % | p-Value | N | % | n1 | % | p-Value |
| Emergency care total | 336,624 | 100.00 | 73,299 | 21.77 | 217,080 | 100.00 | 98,425 | 45.34 | 123,500 | 100.00 | 73,656 | 59.64 | 80,618 | 100.00 | 53,959 | 66.93 | 35,622 | 100.00 | 27,006 | 75.81 | |||||
| Palliative care | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | ||||||||||||||||||||
| Not enrolled | 168,312 | 50.00 | 51,264 | 30.46 | 108,540 | 50.00 | 60,369 | 55.62 | 61,750 | 50.00 | 41,523 | 67.24 | 40,309 | 50.00 | 29,216 | 72.48 | 17,811 | 50.00 | 14,082 | 79.06 | |||||
| Enrolled | 168,312 | 50.00 | 22,035 | 13.09 | 108,540 | 50.00 | 38,056 | 35.06 | 61,750 | 50.00 | 32,133 | 52.04 | 40,309 | 50.00 | 24,743 | 61.38 | 17,811 | 50.00 | 12,924 | 72.56 | |||||
| CPR total | 336,624 | 100.00 | 23,434 | 6.96 | 217,080 | 100.00 | 16,175 | 7.45 | 123,500 | 100.00 | 9640 | 7.81 | 80,618 | 100.00 | 6446 | 8.00 | 35,622 | 100.00 | 3005 | 8.44 | |||||
| Palliative care | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | ||||||||||||||||||||
| Not enrolled | 168,312 | 50.00 | 20,458 | 12.15 | 108,540 | 50.00 | 13,811 | 12.72 | 61,750 | 50.00 | 8006 | 12.97 | 40,309 | 50.00 | 5244 | 13.01 | 17,811 | 50.00 | 2338 | 13.13 | |||||
| Enrolled | 168,312 | 50.00 | 2976 | 1.77 | 108,540 | 50.00 | 2364 | 2.18 | 61,750 | 50.00 | 1634 | 2.65 | 40,309 | 50.00 | 1202 | 2.98 | 17,811 | 50.00 | 667 | 3.74 | |||||
| ICU total | 336,624 | 100.00 | 61,166 | 18.17 | 217,080 | 100.00 | 44,118 | 20.32 | 123,500 | 100.00 | 27,827 | 22.53 | 80,618 | 100.00 | 19,561 | 24.26 | 35,622 | 100.00 | 9967 | 27.98 | |||||
| Palliative care | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | ||||||||||||||||||||
| Not enrolled | 168,312 | 50.00 | 45,574 | 27.08 | 108,540 | 50.00 | 31,491 | 29.01 | 61,750 | 50.00 | 19,431 | 31.47 | 40,309 | 50.00 | 13,308 | 33.01 | 17,811 | 50.00 | 6482 | 36.39 | |||||
| Enrolled | 168,312 | 50.00 | 15,592 | 9.26 | 108,540 | 50.00 | 12,627 | 11.63 | 61,750 | 50.00 | 8396 | 13.60 | 40,309 | 50.00 | 6253 | 15.51 | 17,811 | 50.00 | 3485 | 19.57 | |||||
| Intubation total | 336,624 | 100.00 | 42,203 | 12.54 | 217,080 | 100.00 | 29,858 | 13.75 | 123,500 | 100.00 | 18,266 | 14.79 | 80,618 | 100.00 | 12,467 | 15.46 | 35,622 | 100.00 | 5958 | 16.73 | |||||
| Palliative care | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | ||||||||||||||||||||
| Not enrolled | 168,312 | 50.00 | 35,380 | 21.02 | 108,540 | 50.00 | 24,530 | 22.60 | 61,750 | 50.00 | 14,821 | 24.00 | 40,309 | 50.00 | 9918 | 24.60 | 17,811 | 50.00 | 4512 | 25.33 | |||||
| Enrolled | 168,312 | 50.00 | 6823 | 4.05 | 108,540 | 50.00 | 5328 | 4.91 | 61,750 | 50.00 | 3445 | 5.58 | 40,309 | 50.00 | 2549 | 6.32 | 17,811 | 50.00 | 1446 | 8.12 | |||||
| 1 Week before Death | 4 Week before Death | 8 Week before Death | 12 Week before Death | 24 Week before Death | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | OR | 95% CI | p-Value | OR | 95% CI | p-Value | OR | 95% CI | p-Value | OR | 95% CI | p-Value | OR | 95% CI | p-Value | |||||
| Emergency | ||||||||||||||||||||
| Palliative care | ||||||||||||||||||||
| Enrolled vs. no (ref) | 0.34 | 0.34–0.35 | <0.001 | 0.41 | 0.41–0.42 | <0.001 | 0.50 | 0.49–0.50 | <0.001 | 0.57 | 0.56–0.59 | <0.001 | 0.68 | 0.65–0.72 | <0.001 | |||||
| CPR | ||||||||||||||||||||
| Palliative care | ||||||||||||||||||||
| Enrolled vs. no (ref) | 0.13 | 0.13–0.14 | <0.001 | 0.15 | 0.15–0.16 | <0.001 | 0.18 | 0.17–0.19 | <0.001 | 0.21 | 0.19–0.22 | <0.001 | 0.26 | 0.24–0.28 | <0.001 | |||||
| ICU | ||||||||||||||||||||
| Palliative care | ||||||||||||||||||||
| Enrolled vs. no (ref) | 0.27 | 0.26–0.27 | <0.001 | 0.31 | 0.31–0.32 | <0.001 | 0.33 | 0.32–0.34 | <0.001 | 0.36 | 0.34–0.37 | <0.001 | 0.40 | 0.39–0.43 | <0.001 | |||||
| Intubation | ||||||||||||||||||||
| Palliative care | ||||||||||||||||||||
| Enrolled vs. no (ref) | 0.15 | 0.15–0.16 | <0.001 | 0.17 | 0.17–0.18 | <0.001 | 0.18 | 0.18–0.19 | <0.001 | 0.20 | 0.20–0.21 | <0.001 | 0.26 | 0.24–0.28 | <0.001 | |||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tsai, Y.-S.; Tsai, W.-C.; Chiu, L.-T.; Kung, P.-T. Effectiveness of Palliative Care before Death in Reducing Emergency Care Utilization for Patients with Terminal Cancer and Trends in the Utilization of Palliative Care from 2005–2018. Healthcare 2023, 11, 2907. https://doi.org/10.3390/healthcare11212907
Tsai Y-S, Tsai W-C, Chiu L-T, Kung P-T. Effectiveness of Palliative Care before Death in Reducing Emergency Care Utilization for Patients with Terminal Cancer and Trends in the Utilization of Palliative Care from 2005–2018. Healthcare. 2023; 11(21):2907. https://doi.org/10.3390/healthcare11212907
Chicago/Turabian StyleTsai, Yi-Shiun, Wen-Chen Tsai, Li-Ting Chiu, and Pei-Tseng Kung. 2023. "Effectiveness of Palliative Care before Death in Reducing Emergency Care Utilization for Patients with Terminal Cancer and Trends in the Utilization of Palliative Care from 2005–2018" Healthcare 11, no. 21: 2907. https://doi.org/10.3390/healthcare11212907
APA StyleTsai, Y.-S., Tsai, W.-C., Chiu, L.-T., & Kung, P.-T. (2023). Effectiveness of Palliative Care before Death in Reducing Emergency Care Utilization for Patients with Terminal Cancer and Trends in the Utilization of Palliative Care from 2005–2018. Healthcare, 11(21), 2907. https://doi.org/10.3390/healthcare11212907





