Light-Weight Wearable Gyroscopic Actuators Can Modulate Balance Performance and Gait Characteristics: A Proof-of-Concept Study
Abstract
:1. Introduction
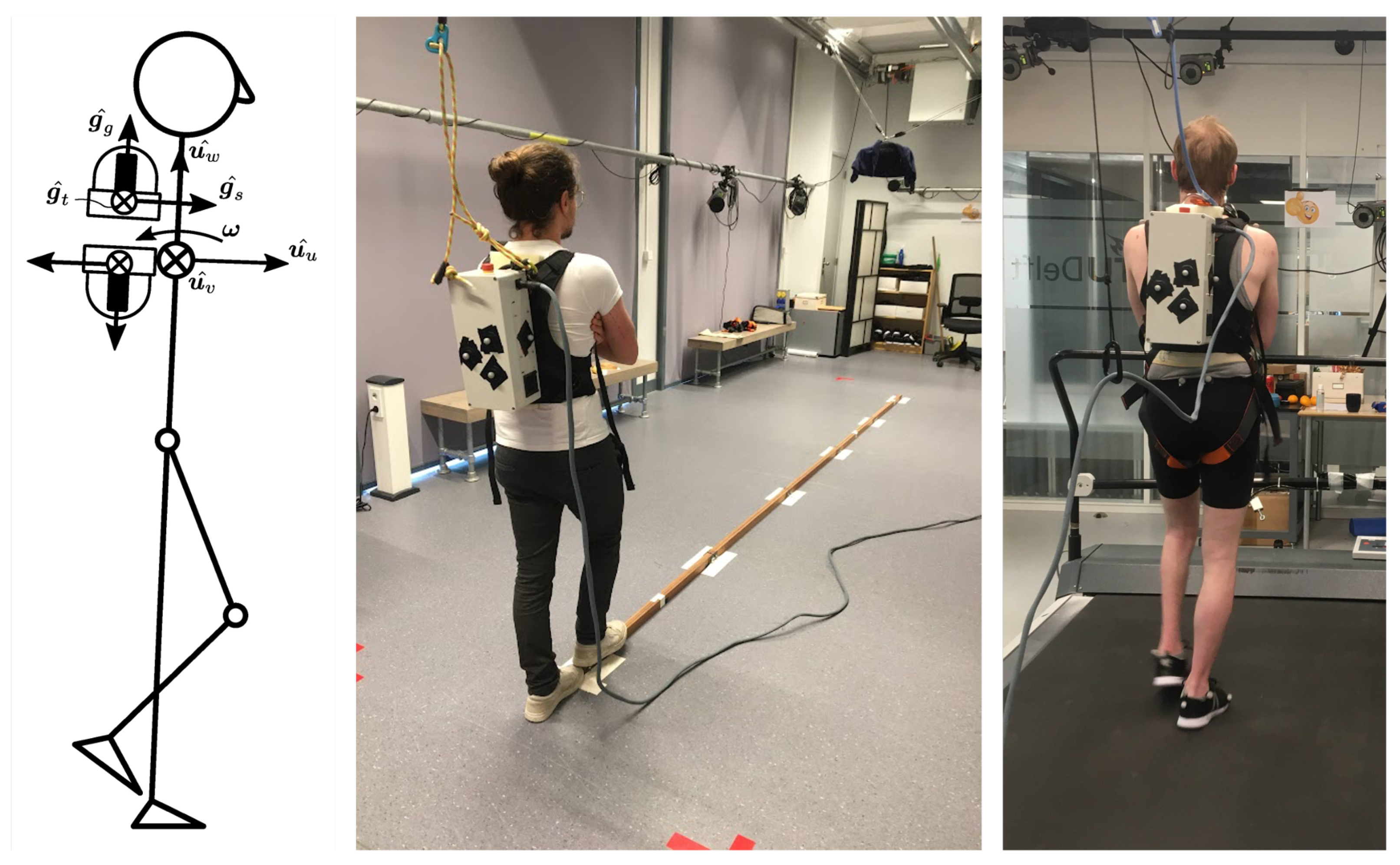
2. Materials and Methods
- Pre-baseline: baseline, no device donned;
- Unpowered: device donned, but turned OFF, i.e., not powered;
- device ON conditions (fully randomised):
- (a)
- Placebo: placebo/sham;
- (b)
- Negative: negative damper;
- (c)
- Low: low-intensity damper;
- (d)
- High: high-intensity damper;
- Unpowered: device donned, but turned OFF, i.e., not powered;
- Post-baseline: baseline, no device donned.

3. Results
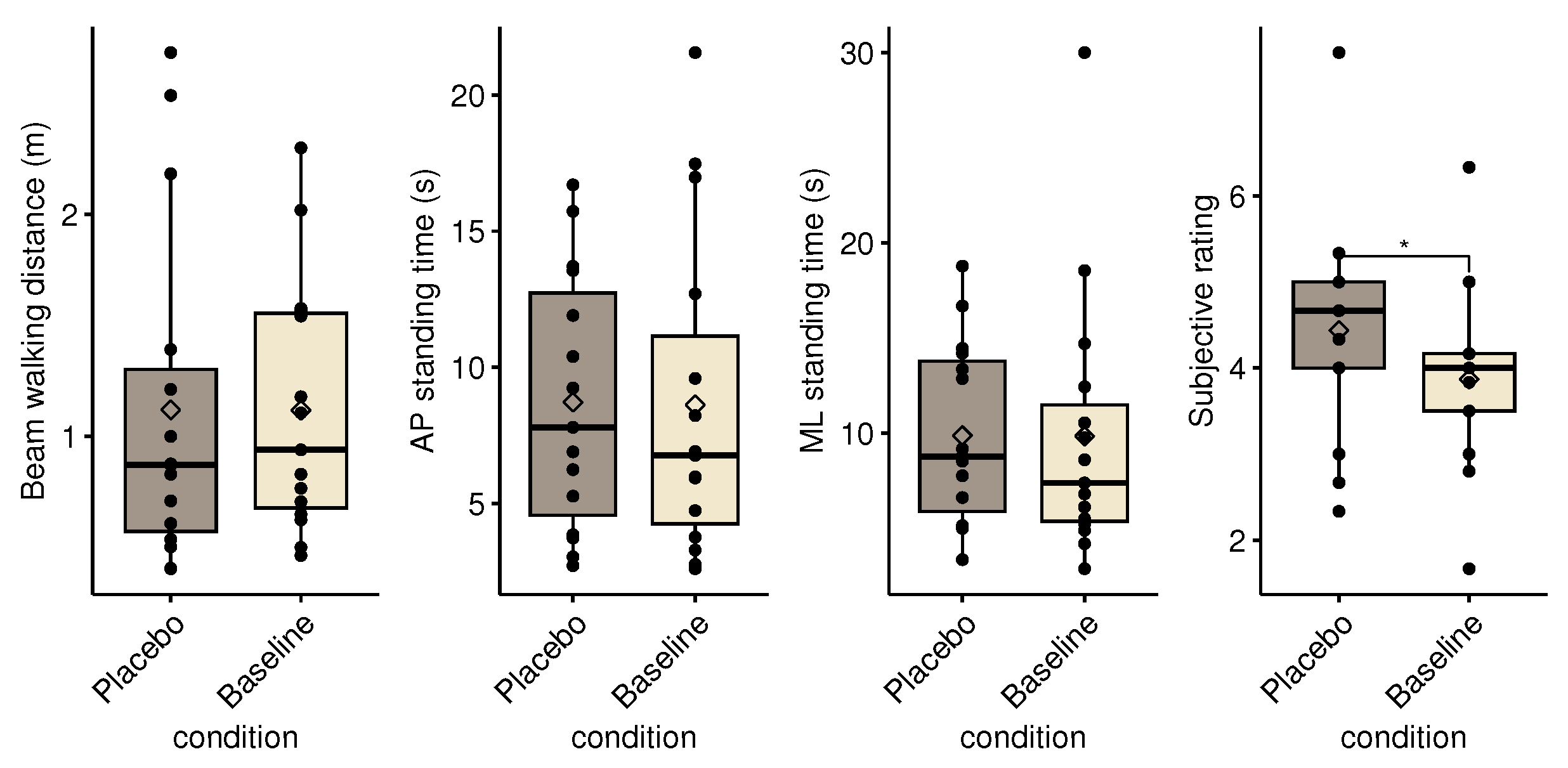
3.1. Placebo Effect
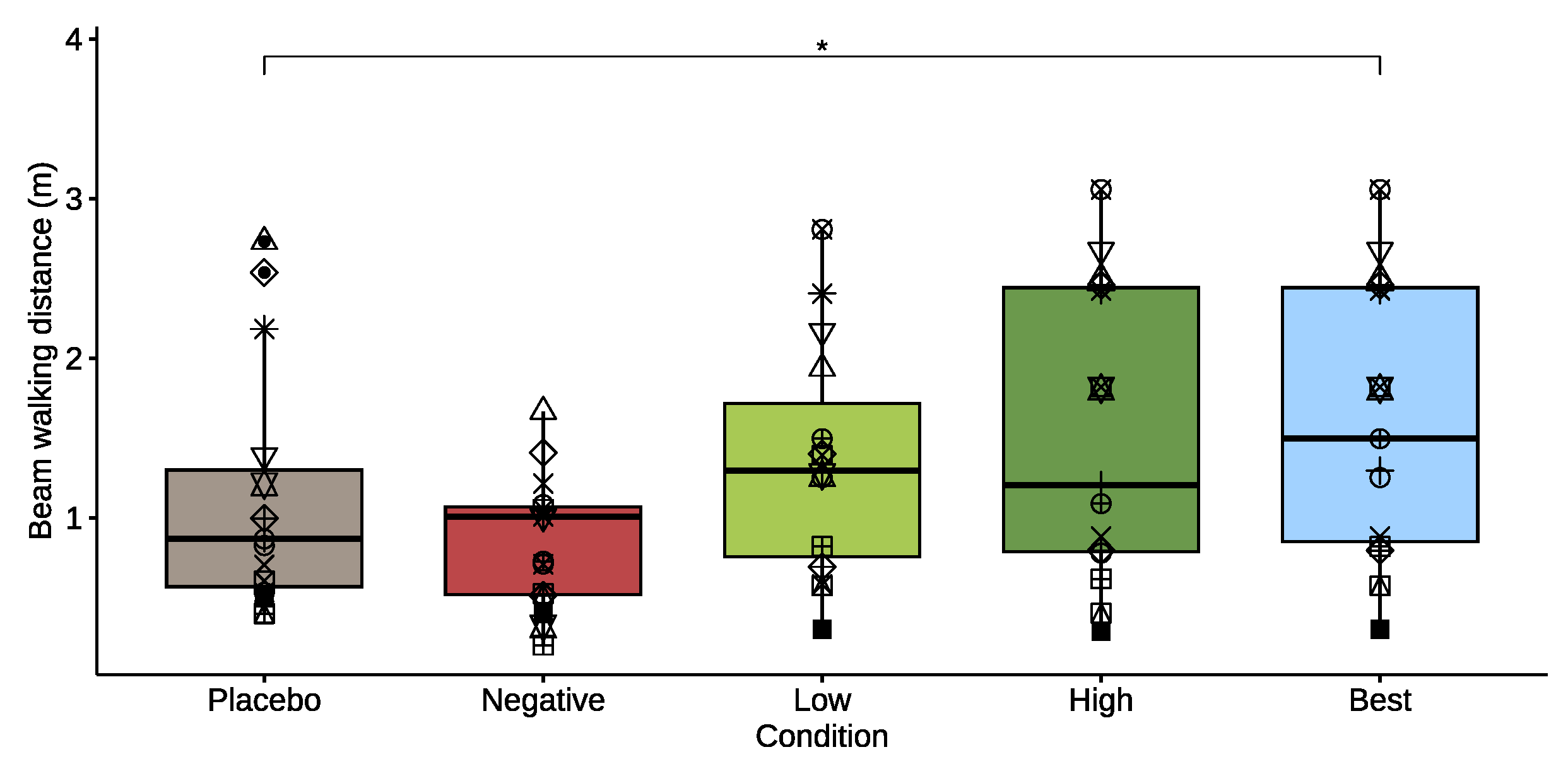
3.2. Balance Beam
3.2.1. Beam Walking
3.2.2. Mediolateral Standing
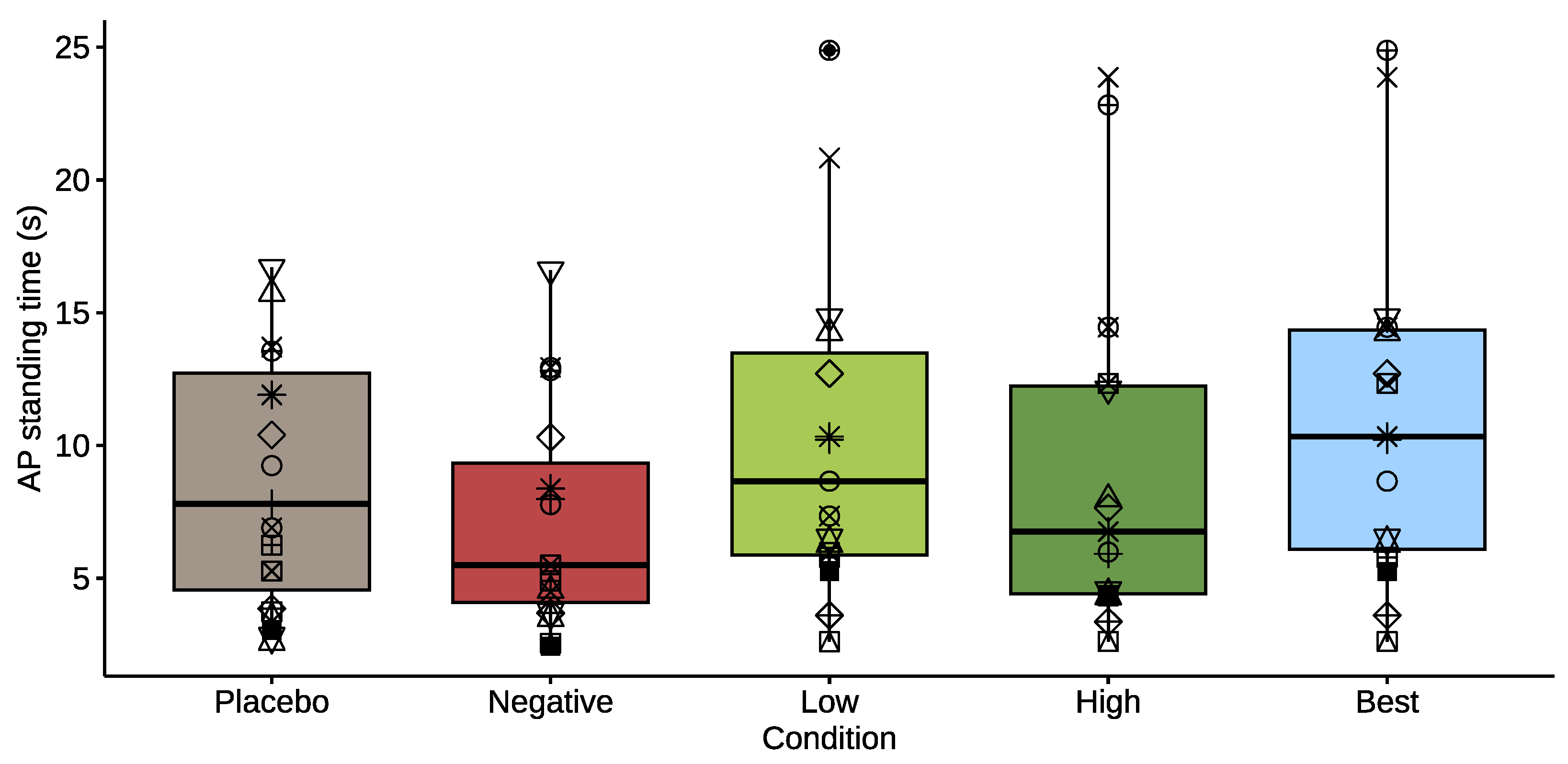
3.2.3. Anteroposterior Standing
3.2.4. Subjective Rating
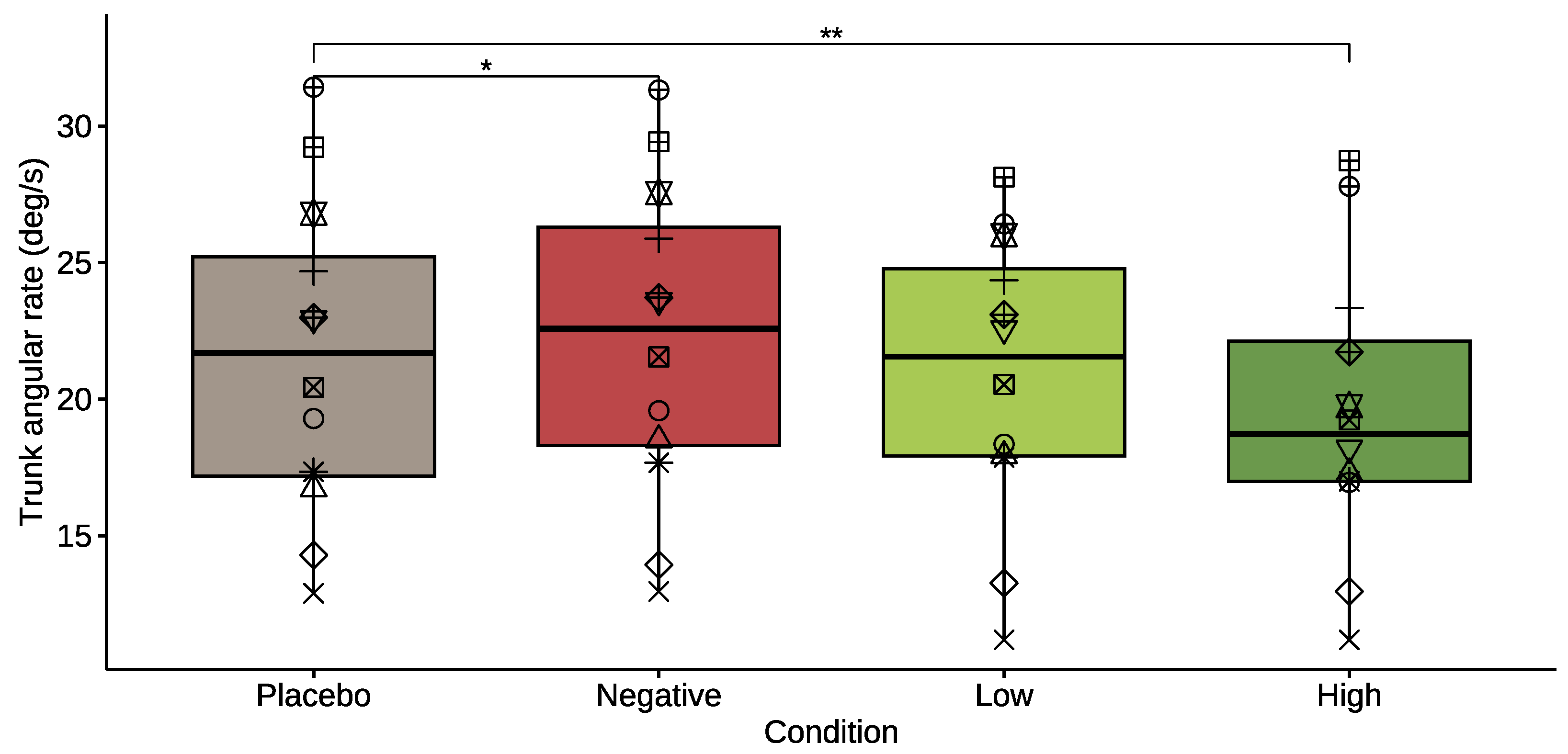
3.3. Treadmill Walking
3.4. Pre- and Post-Baseline
4. Discussion
4.1. Limitations
4.2. Future Work
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ML | Mediolateral |
| AP | Anteroposterior |
| CMG | Control Moment Gyroscope |
| IMU | Inertial Measurement Unit |
| whole-body centroidal angular momentum | |
| Trunk angular velocity vector | |
| Trunk angular rate | |
| Trunk angular velocity variability |
Appendix A
References
- Salari, N.; Darvishi, N.; Ahmadipanah, M.; Shohaimi, S.; Mohammadi, M. Global prevalence of falls in the older adults: A comprehensive systematic review and meta-analysis. J. Orthop. Surg. Res. 2022, 17, 334. [Google Scholar] [CrossRef] [PubMed]
- Tieland, M.; Trouwborst, I.; Clark, B.C. Skeletal muscle performance and ageing: Skeletal muscle performance and ageing. J. Cachexia Sarcopenia Muscle 2018, 9, 3–19. [Google Scholar] [CrossRef] [PubMed]
- Bruijn, S.M.; Meijer, O.G.; Beek, P.J.; van Dieën, J.H. Assessing the stability of human locomotion: A review of current measures. J. R. Soc. Interface 2013, 10, 20120999. [Google Scholar] [CrossRef] [PubMed]
- Jahn, K.; Freiberger, E.; Eskofier, B.M.; Bollheimer, C.; Klucken, J. Balance and mobility in geriatric patients: Assessment and treatment of neurological aspects. Z. Für Gerontol. Und Geriatr. 2019, 52, 316–323. [Google Scholar] [CrossRef] [PubMed]
- Mombaur, K.; Vallery, H.; Hu, Y.; Buchli, J.; Bhounsule, P.; Boaventura, T.; Wensing, P.M.; Revzen, S.; Ames, A.D.; Poulakakis, I.; et al. Chapter 4—Control of Motion and Compliance. In Bioinspired Legged Locomotion; Sharbafi, M.A., Seyfarth, A., Eds.; Butterworth-Heinemann: Oxford, UK, 2017; pp. 135–346. [Google Scholar] [CrossRef]
- Bruijn, S.M.; van Dieën, J.H. Control of human gait stability through foot placement. J. R. Soc. Interface 2018, 15, 20170816. [Google Scholar] [CrossRef] [PubMed]
- Reimann, H.; Fettrow, T.; Jeka, J.J. Strategies for the Control of Balance During Locomotion. Kinesiol. Rev. 2018, 7, 18–25. [Google Scholar] [CrossRef]
- England, S.A.; Granata, K.P. The influence of gait speed on local dynamic stability of walking. Gait Posture 2007, 25, 172–178. [Google Scholar] [CrossRef] [PubMed]
- Kuo, A.D.; Donelan, J.M. Dynamic Principles of Gait and Their Clinical Implications. Phys. Ther. 2010, 90, 157–174. [Google Scholar] [CrossRef]
- Neptune, R.R.; Vistamehr, A. Dynamic Balance During Human Movement: Measurement and Control Mechanisms. J. Biomech. Eng. 2019, 141, 070801. [Google Scholar] [CrossRef]
- Hamacher, D.; Singh, N.; Van Dieën, J.; Heller, M.; Taylor, W. Kinematic measures for assessing gait stability in elderly individuals: A systematic review. J. R. Soc. Interface 2011, 8, 1682–1698. [Google Scholar] [CrossRef]
- Dingwell, J.B.; Cusumano, J.P.; Cavanagh, P.R.; Sternad, D. Local Dynamic Stability Versus Kinematic Variability of Continuous Overground and Treadmill Walking. J. Biomech. Eng. 2006, 123, 27–32. [Google Scholar] [CrossRef] [PubMed]
- Hof, A.; Gazendam, M.; Sinke, W. The condition for dynamic stability. J. Biomech. 2005, 38, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Nott, C.; Neptune, R.; Kautz, S. Relationships between frontal-plane angular momentum and clinical balance measures during post-stroke hemiparetic walking. Gait Posture 2014, 39, 129–134. [Google Scholar] [CrossRef] [PubMed]
- Herr, H.; Popovic, M. Angular momentum in human walking. J. Exp. Biol. 2008, 211, 467–481. [Google Scholar] [CrossRef] [PubMed]
- Matjačić, Z.; Zadravec, M.; Olenšek, A. Feasibility of robot-based perturbed-balance training during treadmill walking in a high-functioning chronic stroke subject: A case-control study. J. Neuroeng. Rehabil. 2018, 15, 32. [Google Scholar] [CrossRef] [PubMed]
- McCrum, C.; Gerards, M.H.G.; Karamanidis, K.; Zijlstra, W.; Meijer, K. A systematic review of gait perturbation paradigms for improving reactive stepping responses and falls risk among healthy older adults. Eur. Rev. Aging Phys. Act. 2017, 14, 3. [Google Scholar] [CrossRef] [PubMed]
- Apte, S.; Plooij, M.; Vallery, H. Influence of body weight unloading on human gait characteristics: A systematic review. J. Neuroeng. Rehabil. 2018, 15, 53. [Google Scholar] [CrossRef] [PubMed]
- Mahaki, M.; IJmker, T.; Houdijk, H.; Bruijn, S.M. How does external lateral stabilization constrain normal gait, apart from improving medio-lateral gait stability? R. Soc. Open Sci. 2021, 8, 202088. [Google Scholar] [CrossRef]
- Jayakaran, P.; DeSouza, L.; Cossar, J.; Gilhooly, K. Influence of a walking aid on temporal and spatial parameters of gait in healthy adults. PM&R 2014, 6, 796–801. [Google Scholar] [CrossRef]
- Dafarra, S.; Bertrand, S.; Griffin, R.J.; Metta, G.; Pucci, D.; Pratt, J. Non-Linear Trajectory Optimization for Large Step-Ups: Application to the Humanoid Robot Atlas. In Proceedings of the 2020 IEEE/RSJ International Conference on Intelligent Robots and Systems (IROS), Las Vegas, NV, USA, 24 October 2020–24 January 2021; pp. 3884–3891. [Google Scholar] [CrossRef]
- Baimyshev, A.; Finn-Henry, M.; Goldfarb, M. Feasibility of a Wearable Cold-Gas Thruster for Fall Prevention. J. Dyn. Syst. Meas. Control 2022, 144, 084501. [Google Scholar] [CrossRef]
- Finn-Henry, M.; Brenes, J.L.; Baimyshev, A.; Goldfarb, M. Preliminary Evaluation of a Wearable Thruster for Arresting Backwards Falls. In Proceedings of the 2023 IEEE International Conference on Robotics and Automation (ICRA), London, UK, 29 May–2 June 2023; pp. 12604–12609. [Google Scholar] [CrossRef]
- Berry, A.; Lemus, D.; Babuška, R.; Vallery, H. Directional Singularity-Robust Torque Control for Gyroscopic Actuators. IEEE/ASME Trans. Mechatron. 2016, 21, 2755–2763. [Google Scholar] [CrossRef]
- Romtrairat, P. A performance study of a wearable balance assistance device consisting of scissored-pair control moment gyroscopes and a two-axis inclination sensor. J. Biomech. 2020, emph109, 109957. [Google Scholar] [CrossRef] [PubMed]
- Romtrairat, P.; Virulsri, C.; Tangpornprasert, P. An application of scissored-pair control moment gyroscopes in a design of wearable balance assistance device for the elderly. J. Biomech. 2019, 87, 183–188. [Google Scholar] [CrossRef] [PubMed]
- Oya, H.; Fujimoto, Y. Preliminary experiments for postural control using wearable-CMG. In Proceedings of the IECON 2017—43rd Annual Conference of the IEEE Industrial Electronics Society, Beijing, China, 29 October–1 November 2017; pp. 7602–7607. [Google Scholar] [CrossRef]
- Lemus, D.; Berry, A.; Jabeen, S.; Jayaraman, C.; Hohl, K.; van der Helm, F.C.T.; Jayaraman, A.; Vallery, H. Controller synthesis and clinical exploration of wearable gyroscopic actuators to support human balance. Sci. Rep. 2020, 10, 10412. [Google Scholar] [CrossRef] [PubMed]
- Chiu, J.; Goswami, A. Design of a Wearable Scissored-Pair Control Moment Gyroscope (SP-CMG) for Human Balance Assist. In Proceedings of the Volume 5A: 38th Mechanisms and Robotics Conference, Buffalo, NY, USA, 17–20 August 2014; p. V05AT08A023. [Google Scholar] [CrossRef]
- Meijneke, C.; Sterke, B.; Hermans, G.; Gregoor, W.; Vallery, H.; Lemus, D. Design and Evaluation of Pint-Sized Gyroscopic Actuators. In Proceedings of the 2021 IEEE/ASME International Conference on Advanced Intelligent Mechatronics (AIM), Delft, The Netherlands, 12–16 July 2021; pp. 454–461. [Google Scholar] [CrossRef]
- Ijmker, T.; Houdijk, H.; Lamoth, C.J.C.; Beek, P.J.; van der Woude, L.H.V. Energy cost of balance control during walking decreases with external stabilizer stiffness independent of walking speed. J. Biomech. 2013, 46, 2109–2114. [Google Scholar] [CrossRef] [PubMed]
- Quinlivan, B.T.; Lee, S.; Malcolm, P.; Rossi, D.M.; Grimmer, M.; Siviy, C.; Karavas, N.; Wagner, D.; Asbeck, A.; Galiana, I.; et al. Assistance magnitude versus metabolic cost reductions for a tethered multiarticular soft exosuit. Sci. Robot. 2017, 2, eaah4416. [Google Scholar] [CrossRef] [PubMed]
- Poggensee, K.L.; Collins, S.H. How adaptation, training, and customization contribute to benefits from exoskeleton assistance. Sci. Robot. 2021, 6, eabf1078. [Google Scholar] [CrossRef] [PubMed]
- Ingraham, K.A.; Remy, C.D.; Rouse, E.J. The role of user preference in the customized control of robotic exoskeletons. Sci. Robot. 2022, 7, eabj3487. [Google Scholar] [CrossRef]
- Elnaggar, R.K.; Alhowimel, A.; Alotaibi, M.; Abdrabo, M.S.; Elfakharany, M.S. Exploring Temporospatial Gait Asymmetry, Dynamic Balance, and Locomotor Capacity After a 12-Week Split-Belt Treadmill Training in Adolescents with Unilateral Cerebral Palsy: A Randomized Clinical Study. Phys. Occup. Ther. Pediatr. 2023, 43, 6. [Google Scholar] [CrossRef]
- Patton, J.L.; Aghamohammadi, N.R.; Bittman, M.F.; Klamroth-Marganska, V.; Riener, R.; Huang, F.C. Error Fields: Robotic training forces that forgive occasional movement mistakes. Res. Sq. 2022; in review. [Google Scholar] [CrossRef]
- Wojtara, T.; Sasaki, M.; Konosu, H.; Yamashita, M.; Shimoda, S.; Alnajjar, F.; Kimura, H. Artificial balancer—Supporting device for postural reflex. Gait Posture 2012, 35, 316–321. [Google Scholar] [CrossRef] [PubMed]
- Mahaki, M.; Bruijn, S.M.; Van Dieën, J.H. The effect of external lateral stabilization on the use of foot placement to control mediolateral stability in walking and running. PeerJ 2019, 2019, e7939. [Google Scholar] [CrossRef] [PubMed]
- Wu, M.; Brown, G.; Gordon, K.E. Control of locomotor stability in stabilizing and destabilizing environments. Gait Posture 2017, 55, 191–198. [Google Scholar] [CrossRef] [PubMed]
- Godi, M.; Franchignoni, F.; Caligari, M.; Giordano, A.; Turcato, A.M.; Nardone, A. Comparison of Reliability, Validity, and Responsiveness of the Mini-BESTest and Berg Balance Scale in Patients With Balance Disorders. Phys. Ther. 2013, 93, 158–167. [Google Scholar] [CrossRef] [PubMed]
- Siragy, T.; Mezher, C.; Hill, A.; Nantel, J. Active arm swing and asymmetric walking leads to increased variability in trunk kinematics in young adults. J. Biomech. 2020, 99, 109529. [Google Scholar] [CrossRef] [PubMed]
- Begue, J.; Peyrot, N.; Lesport, A.; Turpin, N.A.; Watier, B.; Dalleau, G.; Caderby, T. Segmental contribution to whole-body angular momentum during stepping in healthy young and old adults. Sci. Rep. 2021, 11, 19969. [Google Scholar] [CrossRef] [PubMed]
- Russell, K.; Duncan, M.; Price, M.; Mosewich, A.; Ellmers, T.; Hill, M. A comparison of placebo and nocebo effects on objective and subjective postural stability: A double-edged sword? Front. Hum. Neurosci. 2022, 16, 967722. [Google Scholar] [CrossRef] [PubMed]
- Horváth, A.; Szabo, A.; Gál, V.; Suhaj, C.; Aranyosy, B.; Köteles, F. Are there placebo or nocebo effects in balancing performance? Cogn. Res. Princ. Implic. 2023, 8, 25. [Google Scholar] [CrossRef]
- Marchal-Crespo, L.; Tsangaridis, P.; Obwegeser, D.; Maggioni, S.; Riener, R. Haptic Error Modulation Outperforms Visual Error Amplification When Learning a Modified Gait Pattern. Front. Neurosci. 2019, 13, 61. [Google Scholar] [CrossRef]
- Franchignoni, F.; Horak, F.; Godi, M.; Nardone, A.; Giordano, A. Using psychometric techniques to improve the Balance Evaluation Systems Test: The mini-BESTest. J. Rehabil. Med. 2010, 42, 323–331. [Google Scholar] [CrossRef]
- Van Schooten, K.S.; Sloot, L.H.; Bruijn, S.M.; Kingma, H.; Meijer, O.G.; Pijnappels, M.; Van Dieën, J.H. Sensitivity of trunk variability and stability measures to balance impairments induced by galvanic vestibular stimulation during gait. Gait Posture 2011, 33, 656–660. [Google Scholar] [CrossRef]
- Hodrien, A.; Fernando, T. A Review of Post-Study and Post- Task Subjective Questionnaires to Guide Assessment of System Usability. J. Usability Stud. 2021, 16, 203–232. [Google Scholar]
- Hinata, R.; Nenchev, D.N. Balance stabilization with angular momentum damping derived from the reaction null-space. In Proceedings of the 2018 IEEE-RAS 18th International Conference on Humanoid Robots (Humanoids), Beijing, China, 6–9 November 2018; IEEE: New York, NY, USA, 2018; pp. 188–195. [Google Scholar]
- Reinkensmeyer, D.J.; Marchal-Crespo, L.; Dietz, V. (Eds.) Neurorehabilitation Technology; Springer International Publishing: Cham, Switzerland, 2022. [Google Scholar] [CrossRef]
- De Luca, A.; Squeri, V.; Barone, L.M.; Vernetti Mansin, H.; Ricci, S.; Pisu, I.; Cassiano, C.; Capra, C.; Lentino, C.; De Michieli, L.; et al. Dynamic Stability and Trunk Control Improvements Following Robotic Balance and Core Stability Training in Chronic Stroke Survivors: A Pilot Study. Front. Neurol. 2020, 11, 494. [Google Scholar] [CrossRef] [PubMed]
- Ingraham, K.A.; Tucker, M.; Ames, A.D.; Rouse, E.J.; Shepherd, M.K. Leveraging user preference in the design and evaluation of lower-limb exoskeletons and prostheses. Curr. Opin. Biomed. Eng. 2023, 28, 100487. [Google Scholar] [CrossRef]
- Devittori, G.; Ranzani, R.; Dinacci, D.; Romiti, D.; Califfi, A.; Petrillo, C.; Rossi, P.; Gassert, R.; Lambercy, O. Automatic and Personalized Adaptation of Therapy Parameters for Unsupervised Robot-Assisted Rehabilitation: A Pilot Evaluation. In Proceedings of the 2022 International Conference on Rehabilitation Robotics (ICORR), Rotterdam, The Netherlands, 25–29 July 2022; pp. 1–6. [Google Scholar] [CrossRef]
- De Bock, S.; Ghillebert, J.; Govaerts, R.; Tassignon, B.; Rodriguez-Guerrero, C.; Crea, S.; Veneman, J.; Geeroms, J.; Meeusen, R.; De Pauw, K. Benchmarking occupational exoskeletons: An evidence mapping systematic review. Appl. Ergon. 2022, 98, 103582. [Google Scholar] [CrossRef] [PubMed]
- Beedie, C.; Benedettie, F.; Barbiani, D.; Camerone, E.; Lindheimer, J.; Roelands, B. Incorporating methods and findings from neuroscience to better understand placebo and nocebo effects in sport. Eur. J. Sport Sci. 2020, 20, 313–325. [Google Scholar] [CrossRef] [PubMed]
- Domingo, A.; Ferris, D.P. Effects of physical guidance on short-term learning of walking on a narrow beam. Gait Posture 2009, 30, 464–468. [Google Scholar] [CrossRef] [PubMed]
- Desmet, D.M.; Sawers, A.; Grabiner, M.D. Ensuring accurate estimates of step width variability during treadmill walking requires more than 400 consecutive steps. J. Biomech. 2019, 91, 160–163. [Google Scholar] [CrossRef]
- Ginis, P.; Nackaerts, E.; Nieuwboer, A.; Heremans, E. Cueing for people with Parkinson’s disease with freezing of gait: A narrative review of the state-of-the-art and novel perspectives. Ann. Phys. Rehabil. Med. 2018, 61, 407–413. [Google Scholar] [CrossRef]
- Rao, N.; Mehta, N.; Patel, P.; Parikh, P.J. Effects of aging on conditional visuomotor learning for grasping and lifting eccentrically weighted objects. J. Appl. Physiol. 2021, 131, 937–948. [Google Scholar] [CrossRef]
- Chen, S.C.; Lin, C.H.; Su, S.W.; Chang, Y.T.; Lai, C.H. Feasibility and effect of interactive telerehabilitation on balance in individuals with chronic stroke: A pilot study. J. NeuroEng. Rehabil. 2021, 18, 71. [Google Scholar] [CrossRef]
- Jabeen, S.; Baines, P.M.; Harlaar, J.; Vallery, H.; Berry, A. Reaction moments matter when designing lower-extremity robots for tripping recovery. PLoS ONE 2023, 18, e0280158. [Google Scholar] [CrossRef]
- Valk, L.; Berry, A.; Vallery, H. Directional Singularity Escape and Avoidance for Single-Gimbal Control Moment Gyroscopes. J. Guid. Control Dyn. 2018, 41, 1095–1107. [Google Scholar] [CrossRef]




Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sterke, B.T.; Poggensee, K.L.; Ribbers, G.M.; Lemus, D.; Vallery, H. Light-Weight Wearable Gyroscopic Actuators Can Modulate Balance Performance and Gait Characteristics: A Proof-of-Concept Study. Healthcare 2023, 11, 2841. https://doi.org/10.3390/healthcare11212841
Sterke BT, Poggensee KL, Ribbers GM, Lemus D, Vallery H. Light-Weight Wearable Gyroscopic Actuators Can Modulate Balance Performance and Gait Characteristics: A Proof-of-Concept Study. Healthcare. 2023; 11(21):2841. https://doi.org/10.3390/healthcare11212841
Chicago/Turabian StyleSterke, Bram T., Katherine L. Poggensee, Gerard M. Ribbers, Daniel Lemus, and Heike Vallery. 2023. "Light-Weight Wearable Gyroscopic Actuators Can Modulate Balance Performance and Gait Characteristics: A Proof-of-Concept Study" Healthcare 11, no. 21: 2841. https://doi.org/10.3390/healthcare11212841
APA StyleSterke, B. T., Poggensee, K. L., Ribbers, G. M., Lemus, D., & Vallery, H. (2023). Light-Weight Wearable Gyroscopic Actuators Can Modulate Balance Performance and Gait Characteristics: A Proof-of-Concept Study. Healthcare, 11(21), 2841. https://doi.org/10.3390/healthcare11212841




