Effectiveness of Spironolactone in Terms of Galectin-3 Levels in Patients with Heart Failure with a Reduced Ejection Fraction in the Vietnamese Population
Abstract
:1. Introduction
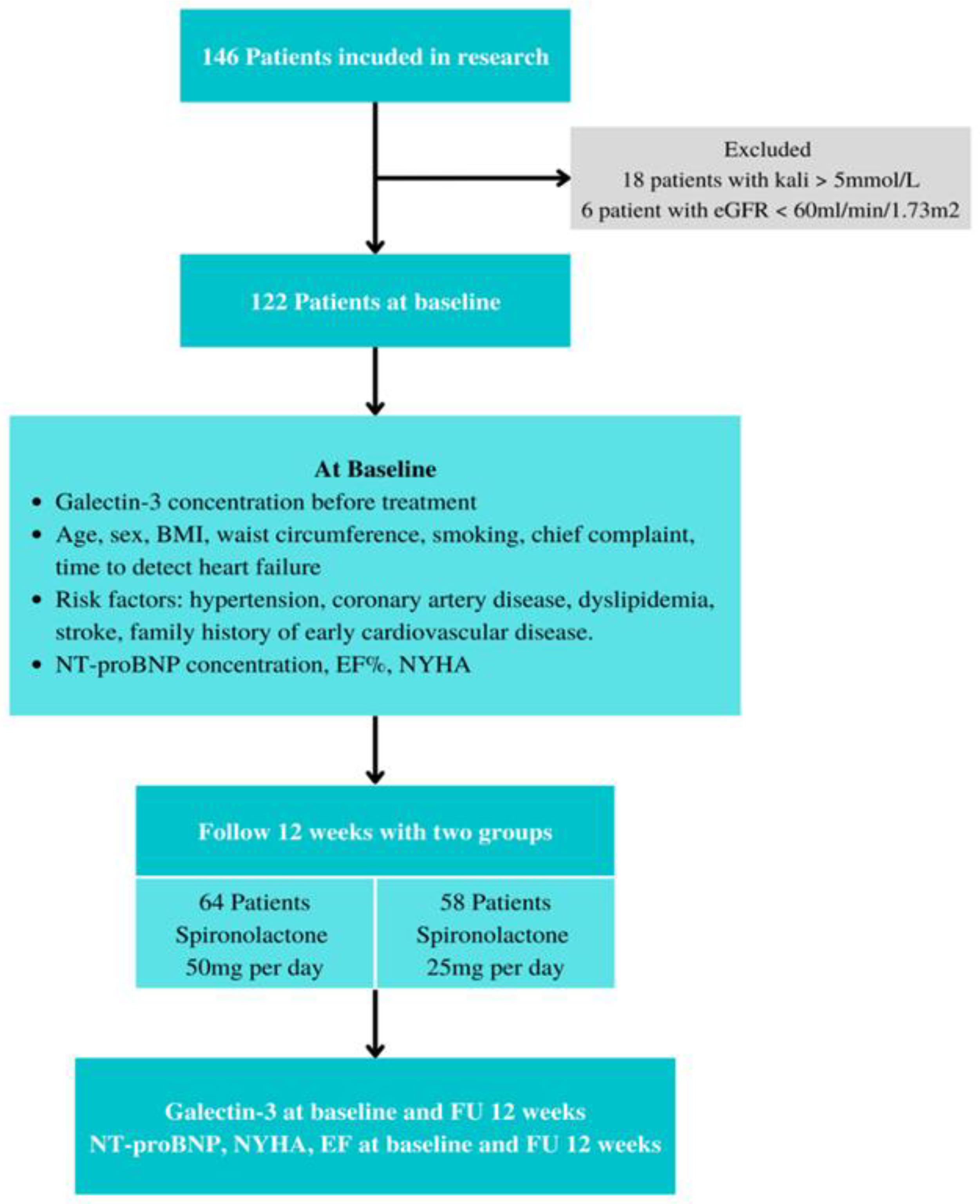
2. Materials and Methods
2.1. Study Population
2.1.1. Materials
2.1.2. Inclusion Criteria
2.1.3. Exclusion Criteria
- -
- Patients currently taking spironolactone prior to participating in this study.
- -
- -
- Patients with a low life expectancy (<1 year).
- -
- Patients with advanced cancer (Figure 1).
2.2. Methods
2.2.1. Study Design
2.2.2. Sample Size
2.3. Data Collection
2.4. Data Analysis
2.5. Measurements
2.6. Statistical Analysis
3. Results
3.1. Baseline Subject Characteristics
3.2. The Proportion of Increased Galectin-3 and the Relationship between Some Cardiovascular Risk Factors and Galectin-3
3.3. The Variation in Galectin-3 after 12 Weeks of Treatment with Spironolactone
4. Discussion
4.1. Some Factors Associated with Elevated Serum Galectin-3 Levels in Patients with Heart Failure with a Reduced Ejection Fraction
4.2. Multivariate Correlation between Galectin-3 and Risk Factors in Patients with Heart Failure
4.3. Results of Controlling Serum Galectin-3 Levels Using Spironolactone in Heart Failure Patients with a Reduced Ejection Fraction
4.4. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
List of Abbreviations
| HFrEF | Heart failure with reduced ejection fraction |
| HFpEF | Heart failure with preserved ejection fraction |
| NT-proBNP | N-terminal pro B-type natriuretic peptide |
| BNP | B-type natriuretic peptide |
| EF | Ejection fraction |
| NYHA | The New York Heart Association |
| BMI | Body mass Index |
| ESC | The European Society of Cardiology |
| AST | Aspartate transaminase |
| ALT | Alanine transaminase |
| SD | Standard deviation |
| eGFR | Estimated glomerular filtration rate |
| CI | Confidence interval |
| CRP | C-reactive protein |
| SGLT2i | Sodium-glucose cotransporter-2 inhibitors |
| ARNI | Angiotensin Receptor-Neprilysin Inhibitor |
| ACEIs/ARBs | Angiotensin-converting-enzyme inhibitors/angiotensin II receptor blockers |
References
- Ambrosy, A.P.; Fonarow, G.C.; Butler, J.; Chioncel, O. The global health and economic burden of hospitalizations for heart failure: Lessons learned from hospitalized heart failure registries. J. Am. Coll. Cardiol. 2014, 63, 1123–1133. [Google Scholar] [CrossRef]
- De Boer, R.; Van Veldhuisen, D.; Gansevoort, R.; Muller Kobold, A. The fibrosis marker galectin-3 and outcome in the general population. J. Intern. Med. 2012, 272, 55–64. [Google Scholar] [CrossRef]
- Lok, D.J.; Van Der Meer, P.; de la Porte, P.W.; Lipsic, E. Prognostic value of galectin-3, a novel marker of fibrosis, in patients with chronic heart failure: Data from the DEAL-HF study. Clin. Res. Cardiol. 2010, 99, 323–328. [Google Scholar] [CrossRef] [Green Version]
- De Boer, R.A.; Lok, D.J.; Jaarsma, T.; van der Meer, P. Predictive value of plasma galectin-3 levels in heart failure with reduced and preserved ejection fraction. Ann. Med. 2011, 43, 60–68. [Google Scholar] [CrossRef]
- Mares, A.; Rodriguez, T.; Deoker, A.; Lehker, A. Effect of Mineralocorticoid Receptor Antagonists in Heart Failure with Preserved Ejection Fraction and with Reduced Ejection Fraction-A Narrative Review. Curr. Vasc. Pharmacol. 2022, 20, 46–51. [Google Scholar] [CrossRef]
- Deveci, O.; Çelik, A.; İkikardeş, M.; Çağlıyan, C. A novel BioTarget in Treatment of Heart Failure: Changes in Serum Galectin-3 Levels after Spironolactone Therapy. J. Hypertens. 2015, 115, S38. [Google Scholar] [CrossRef]
- Gucuk Ipek, E.; Akin Suljevic, S.; Demirel, H.; Karalok, N. Spironolactone Reduces Galectin-3 Levels in Mildly Symptomatic Systolic Heart Failure Patients. Circulation 2013, 128, A9294. [Google Scholar]
- Lax, A.; Sanchez-Mas, J.; Asensio-Lopez, M.C.; Fernandez-Del Palacio, M.J. Mineralocorticoid receptor antagonists modulate galectin-3 and interleukin-33/ST2 signaling in left ventricular systolic dysfunction after acute myocardial infarction. JACC Heart Fail. 2015, 3, 50–58. [Google Scholar] [CrossRef]
- Ponikowski, P.; Voors, A.A.; Anker, S.D.; Bueno, H. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 2016, 37, 2129–2200. [Google Scholar] [CrossRef] [Green Version]
- McDonagh, T.A.; Metra, M.; Adamo, M.; Gardner, R.S. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: Developed by the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur. Heart J. 2021, 42, 3599–3726. [Google Scholar]
- Gustafsson, F.; Steensgaard-Hansen, F.; Badskjær, J.; Poulsen, A.H. Diagnostic and prognostic performance of N-terminal ProBNP in primary care patients with suspected heart failure. J. Card. Fail. 2005, 11, S15–S20. [Google Scholar] [CrossRef]
- Januzzi, J.L.; van Kimmenade, R.; Lainchbury, J.; Bayes-Genis, A. NT-proBNP testing for diagnosis and short-term prognosis in acute destabilized heart failure: An international pooled analysis of 1256 patients: The International Collaborative of NT-proBNP Study. Eur. Heart J. 2006, 27, 330–337. [Google Scholar] [CrossRef] [PubMed]
- Tan, Y.H.; Lim, J.P.; Lim, W.S.; Gao, F. Obesity in Older Adults and Associations with Cardiovascular Structure and Function. Obes. Facts 2022, 15, 336–343. [Google Scholar] [CrossRef]
- Christenson, R.H.; Duh, S.-H.; Wu, A.H.; Smith, A. Multi-center determination of galectin-3 assay performance characteristics: Anatomy of a novel assay for use in heart failure. Clin. Biochem. 2010, 43, 683–690. [Google Scholar] [CrossRef] [PubMed]
- Hrynchyshyn, N.; Jourdain, P.; Desnos, M.; Diebold, B. Galectin-3: A new biomarker for the diagnosis, analysis and prognosis of acute and chronic heart failure. Arch. Cardiovasc. Dis. 2013, 106, 541–546. [Google Scholar] [CrossRef] [Green Version]
- Felker, G.M.; Fiuzat, M.; Shaw, L.K.; Clare, R. Galectin-3 in ambulatory patients with heart failure: Results from the HF-ACTION study. Circ. Heart Fail. 2012, 5, 72–78. [Google Scholar] [CrossRef] [Green Version]
- Blanda, V.; Bracale, U.M.; Di Taranto, M.D.; Fortunato, G. Galectin-3 in cardiovascular diseases. Int. J. Mol. Sci. 2020, 21, 9232. [Google Scholar] [CrossRef] [PubMed]
- Falcone, C.; Lucibello, S.; Mazzucchelli, I.; Bozzini, S. Galectin-3 plasma levels and coronary artery disease: A new possible biomarker of acute coronary syndrome. Int. J. Immunopathol. Pharmacol. 2011, 24, 905–913. [Google Scholar] [CrossRef]
- Oikonomou, E.; Karlis, D.; Tsalamadris, S.; Siasos, G. Galectin-3 and arterial stiffness in patients with heart failure: A pilot study. Curr. Vasc. Pharmacol. 2019, 17, 396–400. [Google Scholar] [CrossRef]
- Tran, S.; Huynh, H.; Ngo Hoang, T.; Nguyen, A.; Vo, C.; Nguyen, T.; Van Huynh, M. Effectiveness of combination of perindopril and indapamide on ambulatory arterial stiffness index in Vietnamese patients with primary hypertension. Pharm. Sci. Asia 2022, 49, 478–485. [Google Scholar] [CrossRef]
- Hall, C. NT-ProBNP: The mechanism behind the marker. J. Card. Fail. 2005, 11, S81–S83. [Google Scholar] [CrossRef]
- Oremus, M.; Don-Wauchope, A.; McKelvie, R.; Santaguida, P.L. BNP and NT-proBNP as prognostic markers in persons with chronic stable heart failure. Heart Fail. Rev. 2014, 19, 471–505. [Google Scholar] [CrossRef] [PubMed]
- Florido, R.; Kwak, L.; Echouffo-Tcheugui, J.B.; Zhang, S.; Michos, E.D.; Nambi, V.; Goldberg, R.B.; Hoogeveen, R.C.; Lazo, M.; Gerstenblith, G.; et al. Obesity, Galectin-3, and Incident Heart Failure: The ARIC Study. J. Am. Heart Assoc. 2022, 11, e023238. [Google Scholar] [CrossRef] [PubMed]
- McGavock, J.; Victor, R.; Unger, R.; Szczepaniak, L. American College of Physicians and the American Physiological Society, Adiposity of the heart, revisited. Ann. Intern. Med. 2006, 144, 517–524. [Google Scholar] [CrossRef]
- Johnson, A.M.; Hou, S.; Li, P. Inflammation and insulin resistance: New targets encourage new thinking: Galectin-3 and LTB4 are pro-inflammatory molecules that can be targeted to restore insulin sensitivity. Bioessays 2017, 39, 2–14. [Google Scholar] [CrossRef]
- Son, T.K.; Toan, N.H.; Thang, N.; Le Trong Tuong, H. Prediabetes and insulin resistance in a population of patients with heart failure and reduced or preserved ejection fraction but without diabetes, overweight or hypertension. Cardiovasc. Diabetol. 2022, 21, 75. [Google Scholar] [CrossRef]
- Ho, J.E.; Liu, C.; Lyass, A.; Courchesne, P. Galectin-3, a marker of cardiac fibrosis, predicts incident heart failure in the community. J. Am. Coll. Cardiol. 2012, 60, 1249–1256. [Google Scholar] [CrossRef] [Green Version]
- Shah, R.V.; Chen-Tournoux, A.A.; Picard, M.H.; van Kimmenade, R.R. Galectin-3, cardiac structure and function, and long-term mortality in patients with acutely decompensated heart failure. Eur. J. Heart Fail. 2010, 12, 826–832. [Google Scholar] [CrossRef]
- Kang, S.-H.; Park, J.J.; Choi, D.-J.; Yoon, C.-H. Prognostic value of NT-proBNP in heart failure with preserved versus reduced EF. Heart 2015, 101, 1881–1888. [Google Scholar] [CrossRef]
- McKie, P.M.; Burnett, J.C. NT-proBNP: The gold standard biomarker in heart failure. J. Am. Coll. Cardiol. 2016, 68, 2437–2439. [Google Scholar] [CrossRef]
- Jensen, J.; Ma, L.-P.; Fu, M.L.; Svaninger, D. Inflammation increases NT-proBNP and the NT-proBNP/BNP ratio. Clin. Res. Cardiol. 2010, 99, 445–452. [Google Scholar] [CrossRef] [PubMed]
- Edelmann, F.; Holzendorf, V.; Wachter, R.; Nolte, K. Galectin-3 in patients with heart failure with preserved ejection fraction: Results from the Aldo-DHF trial. Eur. J. Heart Fail. 2015, 17, 214–223. [Google Scholar] [CrossRef]
- Packer, M.; Butler, J.; Zannad, F.; Filippatos, G. Effect of empagliflozin on worsening heart failure events in patients with heart failure and preserved ejection fraction: EMPEROR-Preserved trial. Circulation 2021, 144, 1284–1294. [Google Scholar] [CrossRef] [PubMed]
- Jariwala, P.; Jadhav, K.; Khetan, S. Safety and effectiveness of angiotensin receptor-neprilysin inhibitors in patients with heart failure with preserved ejection fraction (ARNI-PRESERVED study). Eur. Heart J. Acute Cardiovasc. Care 2022, 11, 1. [Google Scholar] [CrossRef]

| Characteristics | N (%) or Mean ± SD | |
|---|---|---|
| Male | 54 (44.3) | |
| Age | 31–49 | 7 (5.74) |
| 50–69 | 73 (59.83) | |
| ≥ 70 | 42 (34.43) | |
| BMI (kg/m2) | Male | 22.72 ± 3.87 |
| Female | 23.07 ± 3.90 | |
| Waist circumference (cm) | Male | 87.17 ± 8.90 |
| Femal | 85.10 ± 12.45 | |
| Time to detection of heart failure (years) | 5.10 ± 4.05 | |
| Coronary artery disease | 45 (36.9) | |
| Cerebrovascular accident | 17 (13.9) | |
| Dyslipidemia | 107 (87.7) | |
| Smoking | 20 (16.4) | |
| Family history of early cardiovascular disease | 69 (56.6) | |
| Hypertension | 75 (61.5) | |
| NYHA | II | 44 (36.1) |
| III | 74 (60.6) | |
| IV | 4 (3.3) | |
| Hypertension | Normal | 47 (38.5) |
| Grade 1 | 44 (36.1) | |
| Grade 2 | 24 (19.7) | |
| Grade 3 | 7 (5.7) | |
| Systolic blood pressure (mmHg) | Male | 142.96 ± 22.29 |
| Female | 140.29 ± 23.88 | |
| Diastolic blood pressure (mmHg) | Male | 87.78 ± 14.46 |
| Female | 85.53 ± 15.24 | |
| NT-proBNP | Male | 4557.26 ± 2897.29 |
| Female | 4559.18 ± 2466.73 | |
| EF% | Male | 33.17 ± 5.54 |
| Female | 32.81 ± 5.08 | |
| Spironolacton | 25 mg | 58 (47.5) |
| 50 mg | 64 (52.5) | |
| Medications | ACEIs/ARBs | 75 (61.5) |
| Beta-blockers | 56 (45.9) | |
| Diuretics | 28 (22.95) | |
| Digoxin | 15 (12.30) | |
| Antiplatelets | 62 (50.82) | |
| Statin | 114 (93.44) | |
| Nitrate | 8 (6.56) | |
| Galectin-3 (ng/mL) | 54.82 ± 26.06 | |
| Cardiovascular Risk Factors | Galectin-3 | |
|---|---|---|
| r | p | |
| Age | 0.325 | <0.001 |
| Time to detection of heart failure | 0.714 | <0.001 |
| NT-proBNP | 0.744 | <0.001 |
| EF | −0.701 | <0.001 |
| BMI | 0.344 | <0.001 |
| Waist circumference | 0.388 | <0.001 |
| Cardiovascular Risk Factors | β | Std. Error | t | 95% CI β | p |
|---|---|---|---|---|---|
| Age | 0.218 | 0.149 | 1.461 | −0.078–0.514 | 0.147 |
| Time to detection of heart failure | 2.265 | 0.444 | 5.098 | 1.385–3.146 | <0.001 |
| Systolic blood pressure (mmHg) | −0.183 | 0.147 | −1.245 | −0.475–0.108 | 0.216 |
| Diastolic blood pressure (mmHg) | 0.374 | 0.229 | 1.631 | −0.080–0.827 | 0.106 |
| BMI | 0.537 | 0.465 | 1.154 | −0.385–1.459 | 0.251 |
| Waist circumference | −0.064 | 0.166 | −0.385 | −0.393–0.265 | 0.701 |
| NT-proBNP | 0.003 | 0.001 | 3.716 | 0.001–0.005 | <0.001 |
| EF | −0.992 | 0.423 | −2.345 | −1.830–(−0.154) | 0.021 |
| Risk Factors | Galectin-3 | n | ( + SD) | Changing | p (Paired Sample t-test) | |
|---|---|---|---|---|---|---|
| Galectin-3 | Baseline | 122 | 54.82 ± 26.06 | 10.62 ± 17.15 | <0.001 | |
| Follow up | 122 * | 44.20 ± 24.36 | ||||
| Classification of blood pressure | Normal | Baseline | 47 | 46.43 ± 23.96 | 8.34 ± 11.67 | <0.001 |
| Follow up | 47 * | 38.09 ± 21.15 | ||||
| Grade 1 | Baseline | 44 | 58.10 ± 25.58 | 9.29 ± 23.43 | 0.012 | |
| Follow up | 44 * | 48.81 ± 28.30 | ||||
| Grade 2 | Baseline | 24 | 60.34 ± 21.15 | 14.35 ± 10.64 | <0.001 | |
| Follow up | 24 * | 45.99 ± 18.38 | ||||
| Grade 3 | Baseline | 7 | 71.67 ± 42.44 | 21.49 ± 16.53 | 0.014 | |
| Follow up | 7 * | 50.19 ± 31.53 | ||||
| NYHA classification | NYHA II | Baseline | 44 | 36.41 ± 21.52 | 6.85 ± 22.70 | 0.052 |
| Follow up | 44 * | 29.56 ± 24.72 | ||||
| NYHA III | Baseline | 74 | 63.04 ± 20.79 | 12.28 ± 12.60 | <0.001 | |
| Follow up | 74 * | 50.76 ± 18.70 | ||||
| NYHA IV | Baseline | 4 | 105.38 ± 13.52 | 21.48 ± 13.46 | 0.05 | |
| Follow up | 4 * | 83.90 ± 18.91 | ||||
| Spironolacton | 25 mg per day | Baseline | 58 | 50.34 ± 28.33 | 3.46 ± 6.81 | <0.001 |
| Follow up | 58 | 46.87 ± 25.09 | ||||
| 50 mg per day | Baseline | 64 | 58.89 ± 23.29 | 17.11 ± 20.81 | <0.001 | |
| Follow up | 64 | 41.78 ± 23.60 | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tran, S.K.; Ngo, T.H.; Lai, T.T.; Truong, G.K.; Tran, K.D.D.; Vo, P.M.; Nguyen, P.T.; Nguyen, P.H.; Nguyen, T.T.; Nguyen, O.T.K.; et al. Effectiveness of Spironolactone in Terms of Galectin-3 Levels in Patients with Heart Failure with a Reduced Ejection Fraction in the Vietnamese Population. Healthcare 2023, 11, 253. https://doi.org/10.3390/healthcare11020253
Tran SK, Ngo TH, Lai TT, Truong GK, Tran KDD, Vo PM, Nguyen PT, Nguyen PH, Nguyen TT, Nguyen OTK, et al. Effectiveness of Spironolactone in Terms of Galectin-3 Levels in Patients with Heart Failure with a Reduced Ejection Fraction in the Vietnamese Population. Healthcare. 2023; 11(2):253. https://doi.org/10.3390/healthcare11020253
Chicago/Turabian StyleTran, Son Kim, Toan Hoang Ngo, Tin Trung Lai, Giang Khanh Truong, Khoa Dang Dang Tran, Phuong Minh Vo, Phi The Nguyen, Phi Hoang Nguyen, Thuan Tuan Nguyen, Oanh Thi Kim Nguyen, and et al. 2023. "Effectiveness of Spironolactone in Terms of Galectin-3 Levels in Patients with Heart Failure with a Reduced Ejection Fraction in the Vietnamese Population" Healthcare 11, no. 2: 253. https://doi.org/10.3390/healthcare11020253
APA StyleTran, S. K., Ngo, T. H., Lai, T. T., Truong, G. K., Tran, K. D. D., Vo, P. M., Nguyen, P. T., Nguyen, P. H., Nguyen, T. T., Nguyen, O. T. K., Nguyen, T., Nguyen, K. T., & Tran, H. D. (2023). Effectiveness of Spironolactone in Terms of Galectin-3 Levels in Patients with Heart Failure with a Reduced Ejection Fraction in the Vietnamese Population. Healthcare, 11(2), 253. https://doi.org/10.3390/healthcare11020253







