The Association between Non-Alcoholic Fatty Liver Disease and Dynapenia in Men Diagnosed with Type 2 Diabetes Mellitus
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zheng, Y.; Ley, S.H.; Hu, F.B. Global etiology and epidemiology of type 2 diabetes mellitus and its complications. Nat. Rev. Endocrinol. 2018, 14, 88–98. [Google Scholar] [CrossRef] [PubMed]
- Younossi, Z.M.; Stepanova, M.; Afendy, M.; Fang, Y.; Younossi, Y.; Mir, H.; Srishord, M. Changes in the Prevalence of the Most Common Causes of Chronic Liver Diseases in the United States From 1988 to 2008. Clin. Gastroenterol. Hepatol. 2011, 9, 524–530.e1. [Google Scholar] [CrossRef]
- Herath, H.M.M.; Kodikara, I.; Weerarathna, T.P.; Liyanage, G. Prevalence and associations of non-alcoholic fatty liver disease (NAFLD) in Sri Lankan patients with type 2 diabetes: A single center study. Diabetes Metab. Syndr. Clin. Res. Rev. 2018, 13, 246–250. [Google Scholar] [CrossRef]
- Tilg, H.; Moschen, A.R.; Roden, M. NAFLD and diabetes mellitus. Nat. Rev. Gastroenterol. Hepatol. 2017, 14, 32–42. [Google Scholar] [CrossRef] [PubMed]
- Clark, B.C.; Manini, T.M. Sarcopenia =/= dynapenia. J. Gerontol. A Biol. Sci. Med. Sci. 2008, 63, 829–834. [Google Scholar] [CrossRef] [PubMed]
- Manini, T.M.; Clark, B.C. Dynapenia and aging: An update. J. Gerontol. A Biol. Sci. Med. Sci. 2012, 67, 28–40. [Google Scholar] [CrossRef] [PubMed]
- Clark, B.C.; Manini, T.M. What is dynapenia? Nutrition 2012, 28, 495–503. [Google Scholar] [CrossRef]
- Zhang, Y.; Lu, D.; Wang, R.; Fu, W.; Zhang, S. Relationship between Muscle Mass/Strength and Hepatic Fat Content in Post-Menopausal Women. Medicine 2019, 55, 629. [Google Scholar] [CrossRef]
- Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes-2020. Diabetes Care 2020, 43 (Suppl. 1), S14–S31. [CrossRef]
- Rubenstein, L.Z.; Harker, J.O.; Salvà, A.; Guigoz, Y.; Vellas, B. Screening for Undernutrition in Geriatric Practice: Developing the Short-Form Mini-Nutritional Assessment (MNA-SF). J. Gerontol. A Biol. Sci. Med. Sci. 2001, 56, M366–M372. [Google Scholar] [CrossRef]
- Mathias, S.; Nayak, U.S.; Isaacs, B. Balance in elderly patients: The "get-up and go" test. Arch. Phys. Med. Rehabil. 1986, 67, 387–389. [Google Scholar] [PubMed]
- Newman, D.G.; Pearn, J.; Barnes, A.; Young, C.M.; Kehoe, M.; Newman, J. Norms for hand grip strength. Arch. Dis. Child 1984, 59, 453–459. [Google Scholar] [CrossRef] [PubMed]
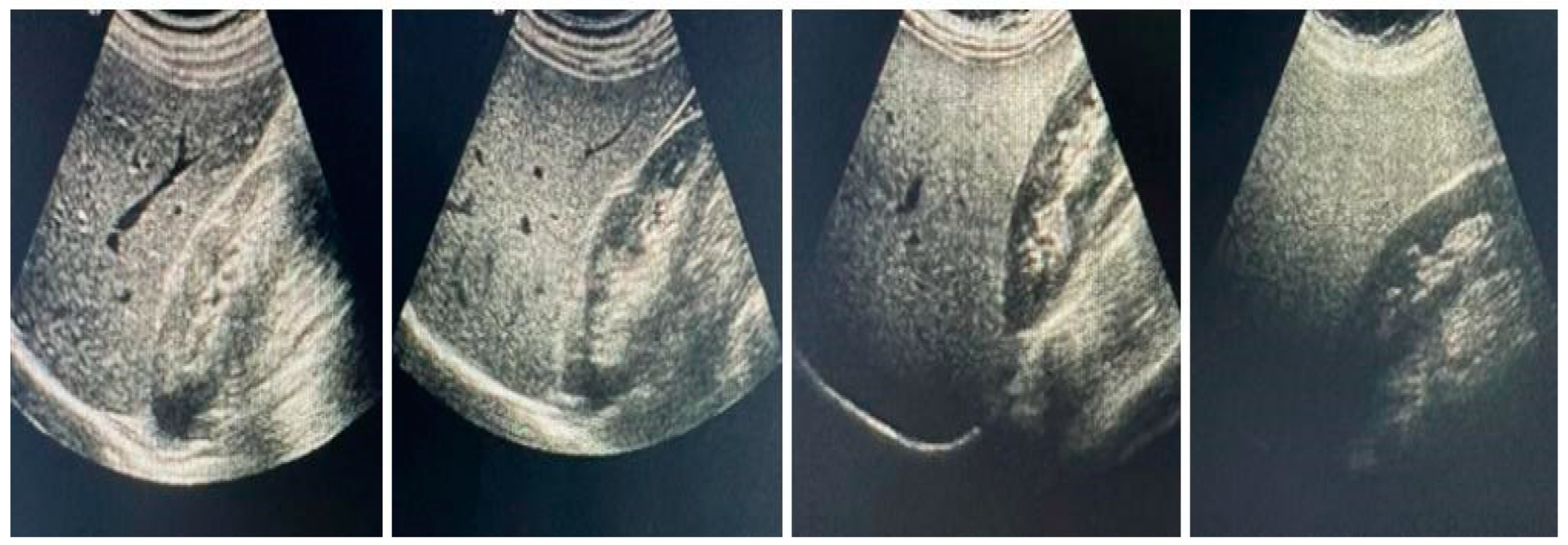
- Piazzolla, V.A.; Mangia, A. Noninvasive Diagnosis of NAFLD and NASH. Cells 2020, 9, 1005. [Google Scholar] [CrossRef] [PubMed]
- Ferraioli, G.; Monteiro, L.B.S. Ultrasound-based techniques for the diagnosis of liver steatosis. World J. Gastroenterol. 2019, 25, 6053–6062. [Google Scholar] [CrossRef]
- Idilman, İ.; Karçaaltıncaba, M. Karaciğer yağlanması tanısında ve yağlanma miktarının belirlenmesinde radyolojik tanı yöntemleri. Güncel Gastroenteloji 2014, 18, 112–118. [Google Scholar]
- Godoy-Matos, A.F.; Silva Júnior, W.S.; Valerio, C.M. NAFLD as a continuum: From obesity to metabolic syndrome and diabetes. Diabetol. Metab. Syndr. 2020, 12, 60. [Google Scholar] [CrossRef]
- Mori, H.; Kuroda, A.; Ishizu, M.; Ohishi, M.; Takashi, Y.; Otsuka, Y.; Taniguchi, S.; Tamaki, M.; Kurahashi, K.; Yoshida, S.; et al. Association of accumulated advanced glycation end-products with a high prevalence of sarcopenia and dynapenia in patients with type 2 diabetes. J. Diabetes Investig. 2019, 10, 1332–1340. [Google Scholar] [CrossRef]
- Palikaras, K.; Mari, M.; Petanidou, B.; Pasparaki, A.; Filippidis, G.; Tavernarakis, N. Ectopic fat deposition contributes to age-associated pathology in Caenorhabditis elegans. J. Lipid Res. 2017, 58, 72–80. [Google Scholar] [CrossRef]
- Sivritepe, R. The Relationship Between Dynapenia and Vitamin D Level in Geriatric Women with Type 2 Diabetes Mellitus. North. Clin. İstanbul 2022, 9, 64–73. [Google Scholar] [CrossRef]
- Hashimoto, Y.; Osaka, T.; Fukuda, T.; Tanaka, M.; Yamazaki, M.; Fukui, M. The relationship between hepatic steatosis and skeletal muscle mass index in men with type 2 diabetes. Endocr. J. 2016, 63, 877–884. [Google Scholar] [CrossRef]
- Nomura, T.; Ikeda, Y.; Nakao, S.; Ito, K.; Ishida, K.; Suehiro, T.; Hashimoto, K. Muscle Strength is a Marker of Insulin Resistance in Patients with Type 2 Diabetes: A Pilot Study. Endocr. J. 2007, 54, 791–796. [Google Scholar] [CrossRef] [PubMed]
- Li, A.A.; Ahmed, A.; Kim, D. Extrahepatic Manifestations of Nonalcoholic Fatty Liver Disease. Gut Liver 2020, 14, 168–178. [Google Scholar] [CrossRef]
- Nishikawa, H.; Yoh, K.; Enomoto, H.; Nishiguchi, S.; Iijima, H. Dynapenia Rather Than Sarcopenia Is Associated with Metabolic Syndrome in Patients with Chronic Liver Diseases. Diagnostics 2021, 11, 1262. [Google Scholar] [CrossRef] [PubMed]
- Nilwik, R.; Snijders, T.; Leenders, M.; Groen, B.B.; van Kranenburg, J.; Verdijk, L.B.; van Loon, L.J. The decline in skeletal muscle mass with aging is mainly attributed to a reduction in type II muscle fiber size. Exp. Gerontol. 2013, 48, 492–498. [Google Scholar] [CrossRef] [PubMed]
- Hamaguchi, M.; Kojima, T.; Takeda, N.; Nakagawa, T.; Taniguchi, H.; Fujii, K.; Omatsu, T.; Nakajima, T.; Sarui, H.; Shimazaki, M.; et al. The metabolic syndrome as a predictor of non-alcoholic fatty liver disease. Ann. Intern. Med. 2005, 143, 722–728. [Google Scholar] [CrossRef] [PubMed]
| Parameter | Median | Minimum | Maximum |
|---|---|---|---|
| Age (years) | 55 | 45 | 65 |
| Height (cm) | 165 | 145 | 189 |
| Weight (kg) | 76 | 44 | 130 |
| BMI (kg/m2) | 28.6 | 17 | 49.3 |
| Muscle Strength (kg) | 36 | 18 | 60 |
| Upper arm circumference (cm) | 24 | 14 | 41 |
| Calf circumference (cm) | 32 | 21 | 39 |
| SMMI index | 39.4 | 26.6 | 61.8 |
| Hba1c (4.7–5.6%) | 9.6 | 6.5 | 15.3 |
| Glucose (70–100 mg/dL) | 188 | 69 | 373 |
| Creatinine (<1 mg/dL) | 0.7 | 0.5 | 1.1 |
| C-reactive protein (<3 mg/L) | 9 | 0.2 | 25 |
| Diabetes Duration (years) | 6.1 | 1 | 23 |
| HDL (40–60 mg/dL) | 33 | 5 | 75 |
| Total Cholesterol (<200 mg/dL) | 245 | 107 | 359 |
| Triglyceride (<150 mg/dL) | 145 | 59 | 321 |
| Leukocyte (4.1–8.9 103/uL) | 9 | 3 | 15.3 |
| Blood Urea Nitrogen (10–20 mg/dL) | 32 | 15 | 57 |
| Hemoglobin (12.4–14.8 g/L) | 14.3 | 10.8 | 17.7 |
| Platelet (150.000–450.000/mm3) | 176 | 100 | 485 |
| Med (Min-Max) | Non-NAFLD | Mild NAFLD | Moderate NAFLD | Severe NAFLD | p Value |
|---|---|---|---|---|---|
| Age (years) | 54.5 (46–65) | 57 (47–65) | 54 (45–65) | 55 (45–65) | 0.626 |
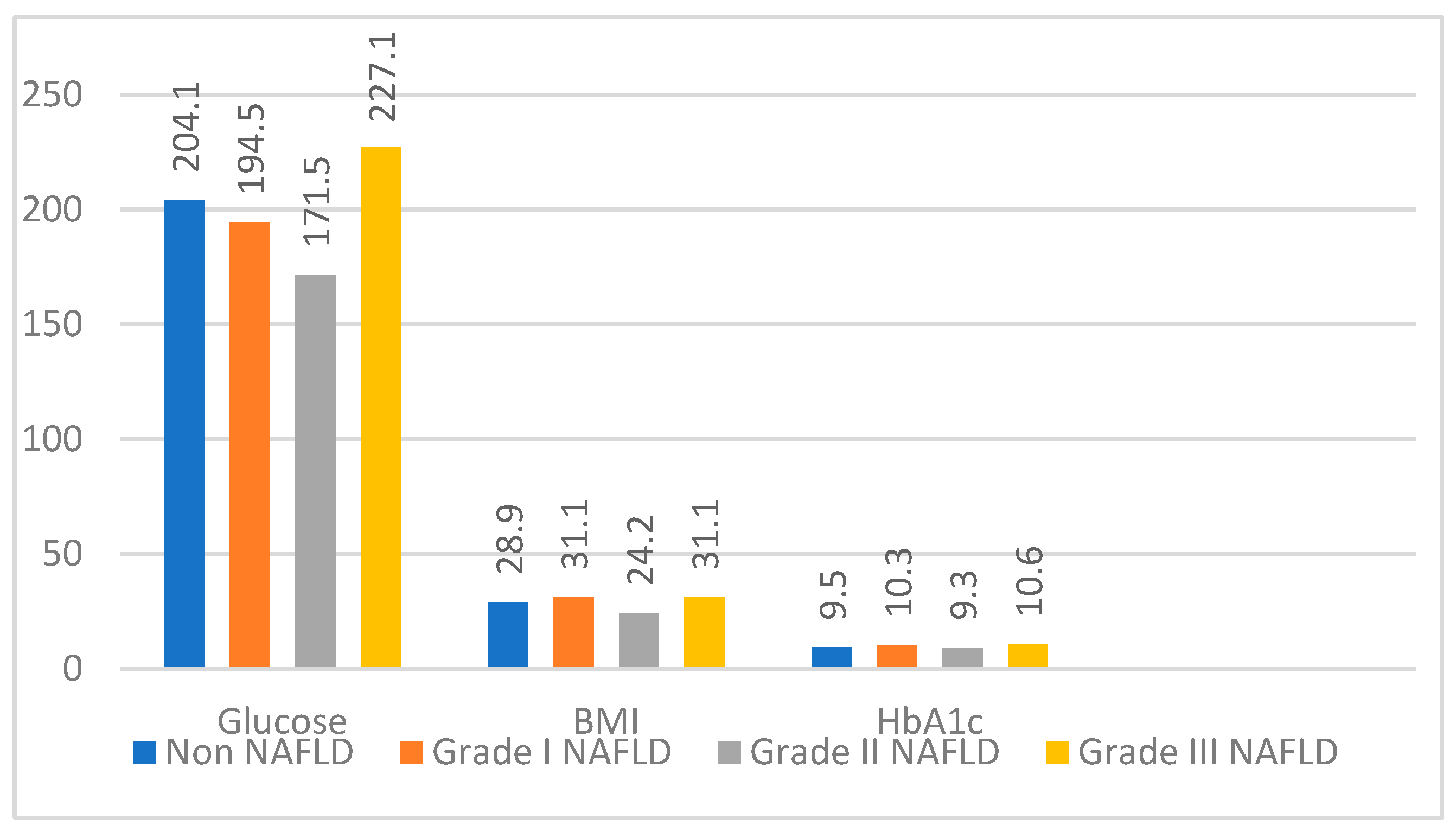
| BMI (kg/m2) | 28.9 (17–49.3) | 31.1 (19.6–41.3) | 24.2 (18,6–43,8) | 31.1 (17.4–42) | 0.362 |
| Muscle Strength (kg) | 44 (24–50) | 38 (28–60) | 30 (18–50) | 24 (18–42) | <0.001 * |
| SMMI % | 39.1 (28.9–48.3) | 39.4 (27.1–47) | 40 (26.6–61.8) | 38.4 (29.2–44) | 0.312 |
| Upper arm circumference (cm) | 28 (15–34) | 26 (24–27) | 21 (17–24) | 18 (14–41) | <0.001 * |
| Calf circumference (cm) | 34 (21–39) | 33.5 (28–39) | 30.5 (26–36) | 29 (21–39) | <0.001 * |
| Hba1c (4.7–5.6%) | 9.5 (6.5–14.2) | 10.3 (6.5–14.5) | 9.3 (6.5–13.6) | 10.6 (6.5–15.3) | 0.126 |
| Glucose (70–100 mg/dL) | 204.1 (110–372) | 194.5 (101–367) | 171.5 (69–365) | 227.1 (92–373) | 0.211 |
| Blood Urea Nitrogen (10–20 mg/dL) | 35 (15–54.9) | 34 (15–57) | 31 (15–51) | 27 (16–46) | 0.031 |
| Creatinine (<1 mg/dL) | 0.7 (0.5–1.1) | 0.7 (0.5–1.1) | 0.7 (0.5–1.1) | 0.7 (0.5–1.1) | 0.448 |
| C-reactive protein (<3 mg/L) | 9.3 (0.2–20) | 6.5 (2–23.4) | 9 (0.7–25) | 13.4 (0.2–24) | 0.137 |
| Total Cholesterol (<200 mg/dL) | 259 (107–359) | 236 (107–302) | 245 (108–356) | 235 (137–359) | 0.124 |
| HDL (40–60 mg/dL) | 30 (5–75) | 33 (5–72) | 33.5 (5–56) | 37 (12–38) | 0.354 |
| Triglyceride (<150 mg/dL) | 122.5 (60–258) | 159.5 (59–298) | 138 (60–321) | 154 (72–299) | 0.058 |
| Leukocyte (4.1–8.9 103/uL) | 8.8 (5.3–15.2) | 9 (4–15.1) | 9 (4–15.2) | 9.6 (3–15.3) | 0.8 |
| Hemoglobin (12.4–14.8 g/l) | 14.2 (11.7–16.7) | 14.5 (11.7–17.3) | 14 (10.8–15.9) | 15 (11.5–17.7) | 0.16 |
| Platelet (15–450.000/mm3) | 168.5 (100–458) | 182 (112–428) | 177 (102–485) | 182 (103–441) | 0.87 |
| Hand Dynamometer | Upper Arm Circumference | Calf Circumference | Get Up and Go Test | |
|---|---|---|---|---|
| Normal-Mild | 1.00 | 0.215 | 1.00 | 1.00 |
| Normal-Moderate | <0.001 | <0.001 | <0.001 | 0.032 |
| Normal-Severe | <0.001 | <0.001 | <0.001 | 0.242 |
| Mild-Moderate | 0.003 | <0.001 | 0.002 | 0.039 |
| Mild-Severe | <0.001 | <0.001 | <0.001 | 0.273 |
| Modarate-Severe | 0.333 | 0,977 | 0.108 | 1.00 |
| Dynapenia Group (n,%) | Nondynapenia Group (n,%) | |
|---|---|---|
| Non-NAFLD | 4 (9.5%) | 30 (32.3%) |
| Mild NAFLD | 2 (4.8%) | 32 (34.4%) |
| Moderate NAFLD | 22 (52.4%) | 26 (28.0%) |
| Severe NAFLD | 14 (33.3%) | 5 (5.4%) |
| Med (Min-Max) | Dynapenia Group N = 42 | Nondynapenia Group N = 93 | p-Value |
|---|---|---|---|
| Age (years) | 55 (45–65) | 55 (45–65) | 0.4771 |
| BMI (kg/m2) | 28.4 (17.4–40.7) | 28.6 (17–49.3) | 0.7472 |
| Muscle Strength (kg) | 24 (18–28) | 40 (30–60) | <0.001 * |
| Muscle Mass (kg) | 52.4 (31.1–61.3) | 51.1 (29.3–70.5) | 0.9642 |
| SMMI % | 40 (26.6–62) | 39 (20.1–48.3) | 0.1782 |
| Upper arm circumference (cm) | 20 (15–41) | 26 (14–34) | <0.001 * |
| Calf circumference (cm) | 30 (21–39) | 32 (21–39) | <0.001 * |
| Up and go test | 1 (1–3) | 1 (1–4) | 0.0442 * |
| Hba1c (4.7–5.6%) | 10.4 (6.5–15.3) | 9.4 (6.5–14.5) | 0.0862 |
| Glucose (70–100 mg/dL) | 183 (70–373) | 190 (69–372) | 0.8552 |
| Blood Urea Nitrogen (10–20 mg/dL) | 31 (15–51) | 34 (15–57) | 0.2722 |
| Creatinine (<1 mg/dL) | 0.7 (0.5–1.1) | 0.7 (0.5–1.1) | 0.6512 |
| C-reactive protein (<3 mg/L) | 9 (0.2–23.4) | 9 (0.2–25) | 0.8972 |
| Total Cholesterol (<200 mg/dL) | 240 (107–356) | 246 (107–359) | 0.7942 |
| HDL (40–60 mg/dL) | 31.5 (5–43) | 33 (5–75) | 0.9202 |
| Triglyceride (<150 mg/dL) | 138 (60–305) | 146 (59–321) | 0.8512 |
| Leukocyte (4.1–8.9 103/uL) | 9.4 (3–15.3) | 9 (4–15.2) | 0.9002 |
| Hemoglobin (12.4–14.8 g/l) | 14.4 (10.58–17.7) | 14.3 (11.5–17.3) | 0.2212 |
| Platelet (15–450.000/mm3) | 183.5 (101–485) | 174 (100–458) | 0.8872 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bulur, A.; Sivritepe, R. The Association between Non-Alcoholic Fatty Liver Disease and Dynapenia in Men Diagnosed with Type 2 Diabetes Mellitus. Healthcare 2023, 11, 243. https://doi.org/10.3390/healthcare11020243
Bulur A, Sivritepe R. The Association between Non-Alcoholic Fatty Liver Disease and Dynapenia in Men Diagnosed with Type 2 Diabetes Mellitus. Healthcare. 2023; 11(2):243. https://doi.org/10.3390/healthcare11020243
Chicago/Turabian StyleBulur, Atilla, and Rıdvan Sivritepe. 2023. "The Association between Non-Alcoholic Fatty Liver Disease and Dynapenia in Men Diagnosed with Type 2 Diabetes Mellitus" Healthcare 11, no. 2: 243. https://doi.org/10.3390/healthcare11020243
APA StyleBulur, A., & Sivritepe, R. (2023). The Association between Non-Alcoholic Fatty Liver Disease and Dynapenia in Men Diagnosed with Type 2 Diabetes Mellitus. Healthcare, 11(2), 243. https://doi.org/10.3390/healthcare11020243





