Improved Trends in the Mortality-to-Incidence Ratios for Liver Cancer in Countries with High Development Index and Health Expenditures
Abstract
1. Introduction
2. Methods
3. Results
3.1. Epidemiology of Liver Cancer by Region
3.2. Epidemiology and Parameters of Development and Health Expenditure with Regard to Liver Cancer in the Selected Countries
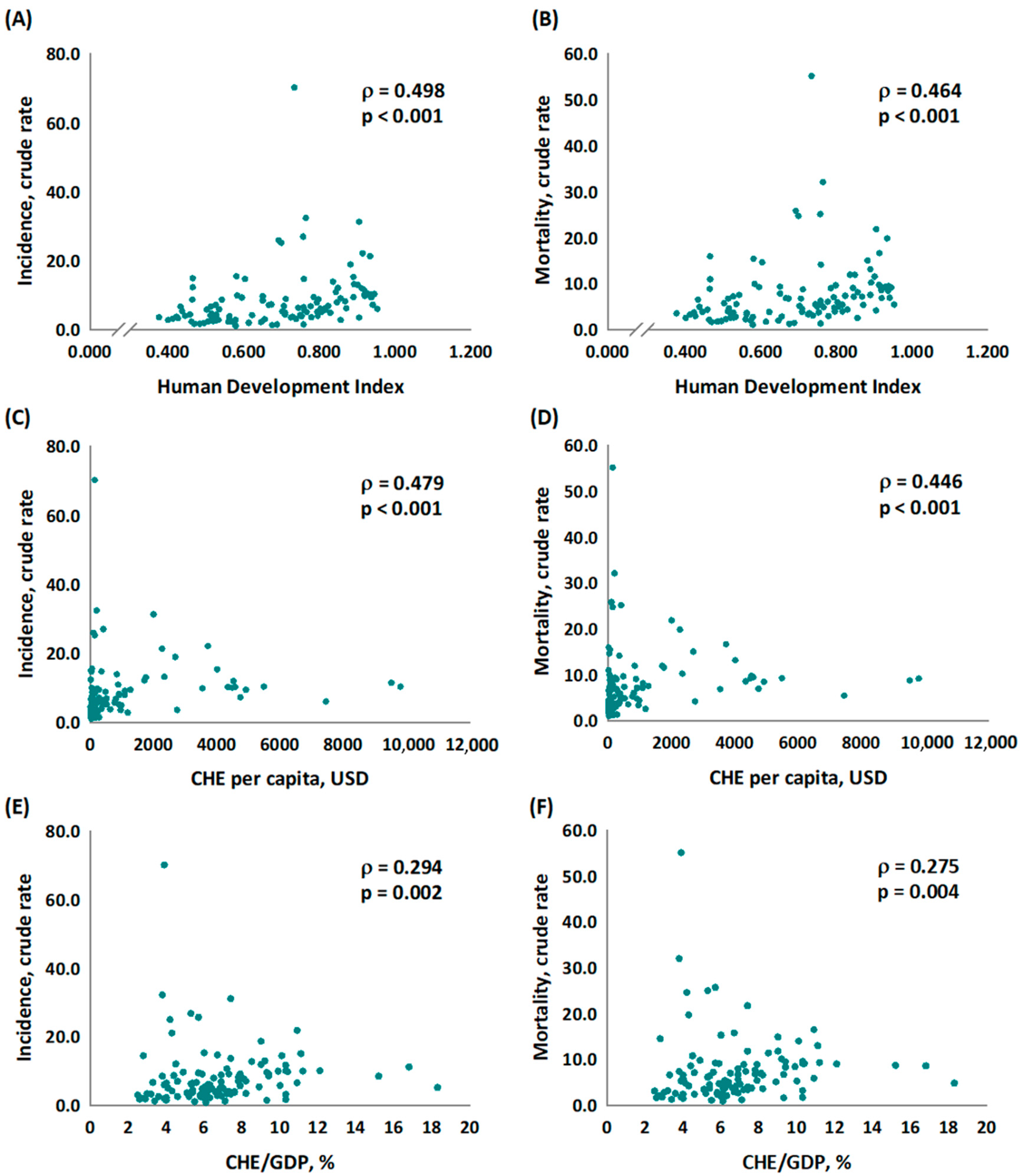
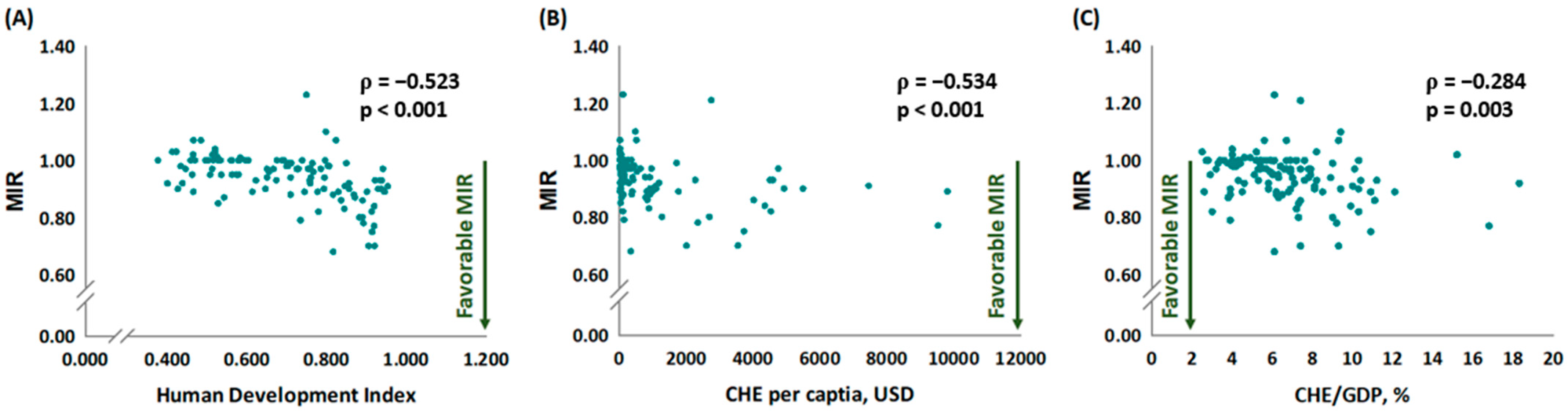
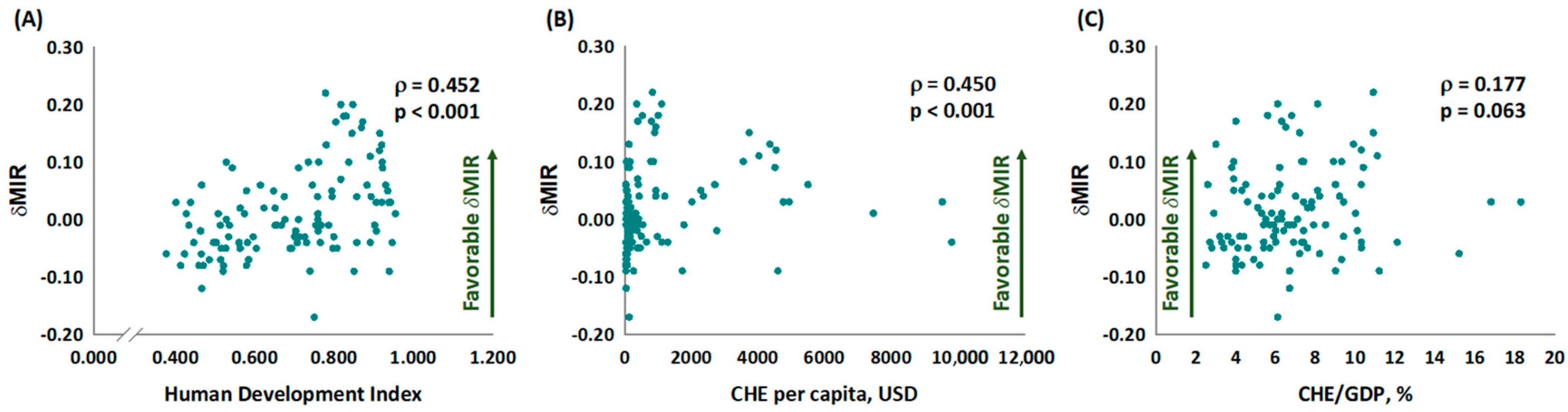
3.3. The Association between MIR and δMIR and Parameters of Development and Health Expenditure of the Selected Countries
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef] [PubMed]
- Nagtegaal, I.D.; Odze, R.D.; Klimstra, D.; Paradis, V.; Rugge, M.; Schirmacher, P.; Washington, K.M.; Carneiro, F.; Cree, I.A.; The WHO Classification of Tumours Editorial Board. The 2019 WHO classification of tumours of the digestive system. Histopathology 2020, 76, 182–188. [Google Scholar] [CrossRef] [PubMed]
- Marrero, J.A.; Kulik, L.M.; Sirlin, C.B.; Zhu, A.X.; Finn, R.S.; Abecassis, M.M.; Roberts, L.R.; Heimbach, J.K. Diagnosis, staging, and management of hepatocellular carcinoma: 2018 practice guidance by the American Association for the Study of Liver Diseases. Hepatology 2018, 68, 723–750. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, K.; Graham, S.M.; Arora, N.; Shuhart, M.C.; Kim, H.N. Hepatocellular carcinoma among US and non-US-born patients with chronic hepatitis B: Risk factors and age at diagnosis. PLoS ONE 2018, 13, e0204031. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.D.; Altekruse, S.F.; Nguyen, M.H.; Gores, G.J.; Roberts, L.R. Impact of country of birth on age at the time of diagnosis of hepatocellular carcinoma in the United States. Cancer 2017, 123, 81–89. [Google Scholar] [CrossRef]
- Tyson, G.L.; El-Serag, H.B. Risk factors for cholangiocarcinoma. Hepatology 2011, 54, 173–184. [Google Scholar] [CrossRef]
- Bertuccio, P.; Bosetti, C.; Levi, F.; Decarli, A.; Negri, E.; La Vecchia, C. A comparison of trends in mortality from primary liver cancer and intrahepatic cholangiocarcinoma in Europe. Ann. Oncol. 2013, 24, 1667–1674. [Google Scholar] [CrossRef]
- Baecker, A.; Liu, X.; La Vecchia, C.; Zhang, Z.F. Worldwide incidence of hepatocellular carcinoma cases attributable to major risk factors. Eur. J. Cancer Prev. 2018, 27, 205–212. [Google Scholar] [CrossRef]
- Plummer, M.; de Martel, C.; Vignat, J.; Ferlay, J.; Bray, F.; Franceschi, S. Global burden of cancers attributable to infections in 2012: A synthetic analysis. Lancet Glob. Health 2016, 4, e609–e616. [Google Scholar] [CrossRef]
- Yang, J.D.; Hainaut, P.; Gores, G.J.; Amadou, A.; Plymoth, A.; Roberts, L.R. A global view of hepatocellular carcinoma: Trends, risk, prevention and management. Nat. Rev. Gastroenterol. Hepatol. 2019, 16, 589–604. [Google Scholar] [CrossRef]
- Lee, Y.C.; Cohet, C.; Yang, Y.C.; Stayner, L.; Hashibe, M.; Straif, K. Meta-analysis of epidemiologic studies on cigarette smoking and liver cancer. Int. J. Epidemiol. 2009, 38, 1497–1511. [Google Scholar] [CrossRef]
- Zhang, H.; Yang, T.; Wu, M.; Shen, F. Intrahepatic cholangiocarcinoma: Epidemiology, risk factors, diagnosis and surgical management. Cancer Lett. 2016, 379, 198–205. [Google Scholar] [CrossRef]
- Clements, O.; Eliahoo, J.; Kim, J.U.; Taylor-Robinson, S.D.; Khan, S.A. Risk factors for intrahepatic and extrahepatic cholangiocarcinoma: A systematic review and meta-analysis. J. Hepatol. 2020, 72, 95–103. [Google Scholar] [CrossRef]
- Watanapa, P.; Watanapa, W.B. Liver fluke-associated cholangiocarcinoma. Br. J. Surg. 2002, 89, 962–970. [Google Scholar] [CrossRef]
- Larroca, S.G.-T.; Arevalo-Serrano, J.; Vila, A.D.; Recarte, M.P.; Hernandez, I.C.; Pierna, A.S.; Bonelli, S.L.; De Leon-Luis, J. Human Development Index (HDI) of the maternal country of origin as a predictor of perinatal outcomes-a longitudinal study conducted in Spain. BMC Pregnancy Childbirth 2017, 17, 314. [Google Scholar]
- World Health Organization. Current Health Expenditure (CHE) per Capita in US$. Available online: https://www.who.int/data/gho/indicator-metadata-registry/imr-details/4951 (accessed on 20 October 2022).
- Fuchs, V.R. The gross domestic product and health care spending. N. Engl. J. Med. 2013, 369, 107–109. [Google Scholar] [CrossRef]
- World Health Organization. Current Health Expenditure (CHE) as Percentage of Gross Domestic Product (GDP) (%). Available online: https://www.who.int/data/gho/indicator-metadata-registry/imr-details/4950 (accessed on 20 October 2022).
- Sunkara, V.; Hébert, J.R. The application of the mortality--to--incidence ratio for the evaluation of cancer care disparities globally. Cancer 2016, 122, 487–488. [Google Scholar] [CrossRef]
- Choi, E.; Lee, S.; Nhung, B.C.; Suh, M.; Park, B.; Jun, J.K.; Choi, K.S. Cancer mortality-to-incidence ratio as an indicator of cancer management outcomes in Organization for Economic Cooperation and Development countries. Epidemiol. Health 2017, 39, e2017006. [Google Scholar] [CrossRef]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef]
- Ghislandi, S.; Sanderson, W.C.; Scherbov, S. A Simple Measure of Human Development: The Human Life Indicator. Popul. Dev. Rev. 2019, 45, 219–233. [Google Scholar] [CrossRef]
- United Nations Development Programme. Human Development Index (HDI). Available online: https://hdr.undp.org/en/content/human-development-index-hdi (accessed on 20 October 2022).
- Ferlay, J.; Ervik, M.; Lam, F.; Colombet, M.; Mery, L.; Piñeros, M. Global Cancer Observatory: Cancer Today. Available online: https://gco.iarc.fr/today (accessed on 12 February 2022).
- Sunkara, V.; Hebert, J.R. The colorectal cancer mortality-to-incidence ratio as an indicator of global cancer screening and care. Cancer 2015, 121, 1563–1569. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.L.; Wang, S.C.; Ho, C.J.; Kao, Y.L.; Hsieh, T.Y.; Chen, W.J.; Chen, C.J.; Wu, P.R.; Ko, J.L.; Lee, H.; et al. Prostate Cancer Mortality-To-Incidence Ratios Are Associated with Cancer Care Disparities in 35 Countries. Sci. Rep. 2017, 7, 40003. [Google Scholar] [CrossRef] [PubMed]
- Sung, W.W.; Wang, S.C.; Hsieh, T.Y.; Ho, C.J.; Huang, C.Y.; Kao, Y.L.; Chen, W.J.; Chen, S.L. Favorable mortality-to-incidence ratios of kidney Cancer are associated with advanced health care systems. BMC Cancer 2018, 18, 792. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.C.; Sung, W.W.; Kao, Y.L.; Hsieh, T.Y.; Chen, W.J.; Chen, S.L.; Chang, H.R. The gender difference and mortality-to-incidence ratio relate to health care disparities in bladder cancer: National estimates from 33 countries. Sci. Rep. 2017, 7, 4360. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.C.; Chan, L.; Hsieh, T.Y.; Wang, C.H.; Chen, S.L.; Sung, W.W. Limited improvement in prostate cancer mortality-to-incidence ratios in countries with high health care expenditures. Aging (Albany NY) 2020, 12, 21308–21315. [Google Scholar] [CrossRef]
- Akinyemiju, T.; Abera, S.; Ahmed, M.; Alam, N.; Alemayohu, M.A.; Allen, C.; Al-Raddadi, R.; Alvis-Guzman, N.; Amoako, Y.; Artaman, A. The burden of primary liver cancer and underlying etiologies from 1990 to 2015 at the global, regional, and national level: Results from the global burden of disease study 2015. JAMA Oncol. 2017, 3, 1683–1691. [Google Scholar]
- Petrick, J.L.; Florio, A.A.; Znaor, A.; Ruggieri, D.; Laversanne, M.; Alvarez, C.S.; Ferlay, J.; Valery, P.C.; Bray, F.; McGlynn, K.A. International trends in hepatocellular carcinoma incidence, 1978–2012. Int. J. Cancer 2020, 147, 317–330. [Google Scholar] [CrossRef]
- World Health Organization. Immunization Coverage. Available online: https://www.who.int/news-room/fact-sheets/detail/immunization-coverage (accessed on 20 October 2022).
- Klushkina, V.V.; Kyuregyan, K.K.; Kozhanova, T.V.; Popova, O.E.; Dubrovina, P.G.; Isaeva, O.V.; Gordeychuk, I.V.; Mikhailov, M.I. Impact of Universal Hepatitis B Vaccination on Prevalence, Infection-Associated Morbidity and Mortality, and Circulation of Immune Escape Variants in Russia. PLoS ONE 2016, 11, e0157161. [Google Scholar] [CrossRef]
- Khetsuriani, N.; Zaika, O.; Chitadze, N.; Slobodianyk, L.; Allahverdiyeva, V.; O’Connor, P.; Huseynov, S. Seroprevalence of hepatitis B virus infection markers among children in Ukraine, 2017. Vaccine 2021, 39, 1485–1492. [Google Scholar] [CrossRef]
- Prueksapanich, P.; Piyachaturawat, P.; Aumpansub, P.; Ridtitid, W.; Chaiteerakij, R.; Rerknimitr, R. Liver Fluke-Associated Biliary Tract Cancer. Gut. Liver 2018, 12, 236–245. [Google Scholar] [CrossRef]
- Kim, E.; Viatour, P. Hepatocellular carcinoma: Old friends and new tricks. Exp. Mol. Med. 2020, 52, 1898–1907. [Google Scholar] [CrossRef]
- de Villa, V.; Lo, C.M. Liver transplantation for hepatocellular carcinoma in Asia. Oncologist 2007, 12, 1321–1331. [Google Scholar] [CrossRef]
- Shao, S.Y.; Hu, Q.D.; Wang, M.; Zhao, X.Y.; Wu, W.T.; Huang, J.M.; Liang, T.B. Impact of national Human Development Index on liver cancer outcomes: Transition from 2008 to 2018. World J. Gastroenterol. 2019, 25, 4749–4763. [Google Scholar] [CrossRef]
- Tu, H.A.T.; de Vries, R.; Woerdenbag, H.J.; Li, S.C.; Le, H.H.; van Hulst, M.; Postma, M.J. Cost-Effectiveness Analysis of Hepatitis B Immunization in Vietnam: Application of Cost-Effectiveness Affordability Curves in Health Care Decision Making. Value Health Reg. Issues 2012, 1, 7–14. [Google Scholar] [CrossRef]
- Cho, E.J.; Kim, S.E.; Suk, K.T.; An, J.; Jeong, S.W.; Chung, W.J.; Kim, Y.J. Current status and strategies for hepatitis B control in Korea. Clin. Mol. Hepatol. 2017, 23, 205–211. [Google Scholar] [CrossRef]
- Papanicolas, I.; Woskie, L.R.; Jha, A.K. Health Care Spending in the United States and Other High-Income Countries. JAMA 2018, 319, 1024–1039. [Google Scholar] [CrossRef]
- Ghamari, S.H.; Yoosefi, M.; Abbasi-Kangevari, M.; Malekpour, M.R.; Saeedi Moghaddam, S.; Shahin, S.; Esfahani, Z.; Koolaji, S.; Shobeiri, P.; Ghaffari, A.; et al. Trends in Global, Regional, and National Burden and Quality of Care Index for Liver Cancer by Cause from Global Burden of Disease 1990–2019. Hepatol. Commun. 2022, 6, 1764–1775. [Google Scholar] [CrossRef]
| New Cases | Deaths | MIR | |||||
|---|---|---|---|---|---|---|---|
| Region | Number | CR | ASR | Number | CR | ASR | |
| Africa | 63.186 | 4.9 | 8.1 | 61.962 | 4.8 | 8.0 | 0.98 |
| Asia | 578.027 | 12.8 | 10.9 | 533.364 | 11.8 | 10.0 | 0.92 |
| Europe | 73.469 | 10.1 | 4.9 | 65.993 | 9.1 | 4.1 | 0.90 |
| Latin America and the Caribbean | 34.209 | 5.3 | 4.6 | 32.376 | 5.0 | 4.4 | 0.94 |
| North America | 39.416 | 11.1 | 6.5 | 30.714 | 8.6 | 4.6 | 0.77 |
| Oceania | 3724 | 9.2 | 6.7 | 3252 | 8.0 | 5.5 | 0.87 |
| HDI | Current Health Expenditure | Incidence | Mortality | Mortality-to-Incidence Ratio | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Country | Per Capita | % of GDP | Number | CR | ASR | Number | CR | ASR | MIR, 2012 | MIR, 2018 | dMIR | |
| Argentina | 0.830 | 998 | 6.8 | 2074 | 4.7 | 3.4 | 1850 | 4.2 | 3.0 | 1.07 | 0.89 | 0.18 |
| Australia | 0.938 | 4934 | 9.4 | 2231 | 9.2 | 5.5 | 2020 | 8.3 | 4.5 | 0.93 | 0.90 | 0.03 |
| Austria | 0.914 | 4536 | 10.3 | 994 | 11.7 | 5.2 | 821 | 9.6 | 4.1 | 0.94 | 0.82 | 0.12 |
| Bangladesh | 0.614 | 32 | 2.6 | 2940 | 1.8 | 2.1 | 2730 | 1.6 | 2.0 | 0.95 | 0.89 | 0.06 |
| Brazil | 0.761 | 780 | 8.9 | 11,256 | 5.4 | 4.4 | 10,673 | 5.1 | 4.1 | 1.04 | 0.94 | 0.10 |
| Burkina Faso | 0.434 | 33 | 5.4 | 1289 | 6.5 | 13.6 | 1262 | 6.4 | 13.3 | 0.97 | 0.98 | −0.01 |
| Côte d’Ivoire | 0.516 | 75 | 5.4 | 1110 | 4.5 | 8.1 | 1119 | 4.5 | 8.2 | 0.95 | 1.00 | −0.05 |
| Cambodia | 0.581 | 70 | 6.0 | 2474 | 15.3 | 20.8 | 2473 | 15.3 | 20.8 | 0.96 | 1.00 | −0.04 |
| Canada | 0.922 | 4508 | 10.4 | 3534 | 9.8 | 5.1 | 3275 | 9.1 | 4.2 | 1.02 | 0.93 | 0.09 |
| Chile | 0.847 | 1102 | 8.1 | 1387 | 7.7 | 5.0 | 1261 | 7.0 | 4.5 | 1.11 | 0.91 | 0.20 |
| China | 0.758 | 426 | 5.3 | 378,016 | 26.8 | 17.7 | 352,962 | 25.0 | 16.4 | 0.97 | 0.93 | 0.04 |
| Congo | 0.459 | 20 | 4.3 | 3519 | 4.2 | 7.5 | 3530 | 4.2 | 7.7 | 0.92 | 1.00 | −0.08 |
| Czechia | 0.891 | 1284 | 7.3 | 959 | 9.2 | 3.9 | 772 | 7.4 | 3.0 | 0.76 | 0.80 | −0.04 |
| Egypt | 0.700 | 157 | 4.2 | 24,724 | 25.0 | 31.2 | 24,420 | 24.6 | 30.8 | 0.95 | 0.98 | −0.03 |
| Ethiopia | 0.470 | 24 | 4.0 | 1574 | 1.5 | 2.6 | 1622 | 1.5 | 2.7 | 0.92 | 1.00 | −0.08 |
| France | 0.891 | 4026 | 11.1 | 9525 | 15.1 | 7.6 | 8223 | 13.0 | 5.9 | 0.97 | 0.86 | 0.11 |
| Germany | 0.939 | 4592 | 11.2 | 7974 | 10.0 | 4.1 | 7467 | 9.3 | 3.5 | 0.84 | 0.93 | −0.09 |
| Ghana | 0.596 | 80 | 5.9 | 2681 | 9.1 | 14.6 | 2665 | 9.1 | 14.6 | 0.97 | 1.00 | −0.03 |
| Guatemala | 0.651 | 224 | 5.7 | 1627 | 9.5 | 13.9 | 1585 | 9.2 | 13.6 | 0.96 | 0.97 | −0.01 |
| Guinea | 0.466 | 25 | 4.5 | 1573 | 12.1 | 21.5 | 1404 | 10.8 | 19.2 | 0.95 | 0.89 | 0.06 |
| Hungary | 0.845 | 894 | 7.2 | 1012 | 10.7 | 5.2 | 847 | 8.9 | 4.2 | 0.98 | 0.83 | 0.15 |
| India | 0.647 | 63 | 3.9 | 26,651 | 2.0 | 2.1 | 24,749 | 1.8 | 2.0 | 0.95 | 0.90 | 0.05 |
| Indonesia | 0.707 | 112 | 3.3 | 17,890 | 6.7 | 7.2 | 17,572 | 6.6 | 7.1 | 0.95 | 0.99 | −0.04 |
| Iran | 0.797 | 366 | 7.6 | 3138 | 3.8 | 4.2 | 3085 | 3.8 | 4.1 | 0.95 | 1.00 | −0.05 |
| Italy | 0.883 | 2700 | 9.0 | 10,661 | 18.7 | 7.6 | 8490 | 14.9 | 5.3 | 0.86 | 0.80 | 0.06 |
| Japan | 0.915 | 3733 | 10.9 | 26,641 | 21.9 | 6.9 | 20,048 | 16.5 | 4.6 | 0.90 | 0.75 | 0.15 |
| Kazakhstan | 0.817 | 379 | 3.9 | 1091 | 6.0 | 5.5 | 974 | 5.3 | 4.9 | 0.95 | 0.88 | 0.07 |
| Kenya | 0.579 | 70 | 5.2 | 1325 | 2.6 | 5.2 | 1310 | 2.6 | 5.2 | 0.92 | 1.00 | −0.08 |
| Lao | 0.604 | 53 | 2.8 | 1008 | 14.5 | 21.5 | 1005 | 14.5 | 21.5 | 0.95 | 1.00 | −0.05 |
| Malaysia | 0.804 | 386 | 4.0 | 1869 | 5.9 | 6.0 | 1851 | 5.8 | 5.9 | 1.15 | 0.98 | 0.17 |
| Mexico | 0.767 | 535 | 5.9 | 6412 | 4.9 | 5.0 | 6044 | 4.7 | 4.7 | 0.95 | 0.96 | −0.01 |
| Mongolia | 0.735 | 152 | 3.9 | 2182 | 70.1 | 90.0 | 1716 | 55.1 | 71.8 | 0.89 | 0.79 | 0.10 |
| Mozambique | 0.446 | 28 | 5.4 | 1165 | 3.8 | 6.3 | 1138 | 3.7 | 6.4 | 0.93 | 0.97 | −0.04 |
| Myanmar | 0.584 | 59 | 4.9 | 5214 | 9.7 | 9.8 | 5270 | 9.8 | 9.9 | 0.94 | 1.01 | −0.07 |
| Nigeria | 0.534 | 97 | 3.6 | 5053 | 2.6 | 4.7 | 5078 | 2.6 | 4.8 | 0.97 | 1.00 | −0.03 |
| Pakistan | 0.560 | 38 | 2.7 | 4280 | 2.1 | 3.0 | 4159 | 2.1 | 2.9 | 0.96 | 1.00 | −0.04 |
| Peru | 0.759 | 323 | 5.3 | 2032 | 6.3 | 6.0 | 1967 | 6.1 | 5.8 | 0.98 | 0.97 | 0.01 |
| Philippines | 0.712 | 127 | 4.4 | 9234 | 8.7 | 10.8 | 9096 | 8.6 | 10.6 | 0.96 | 0.99 | −0.03 |
| Poland | 0.872 | 797 | 6.3 | 2252 | 6.0 | 3.1 | 1935 | 5.2 | 2.5 | 1.04 | 0.87 | 0.17 |
| Portugal | 0.850 | 1722 | 9.0 | 1191 | 11.9 | 5.1 | 1178 | 11.8 | 4.9 | 0.90 | 0.99 | −0.09 |
| Russian Federation | 0.824 | 524 | 5.6 | 9513 | 6.7 | 3.7 | 10,282 | 7.2 | 3.9 | 1.25 | 1.07 | 0.18 |
| Senegal | 0.514 | 36 | 4.0 | 1060 | 6.5 | 12.2 | 1068 | 6.6 | 12.3 | 0.95 | 1.02 | −0.07 |
| Singapore | 0.935 | 2280 | 4.3 | 1206 | 21.1 | 11.1 | 1128 | 19.7 | 10.2 | 0.98 | 0.93 | 0.05 |
| South Korea | 0.906 | 2013 | 7.4 | 15,687 | 31.1 | 16.8 | 10,978 | 21.7 | 11.0 | 0.73 | 0.70 | 0.03 |
| Spain | 0.893 | 2354 | 9.2 | 5822 | 13.0 | 6.2 | 4518 | 10.1 | 4.4 | 0.82 | 0.78 | 0.04 |
| Tanzania | 0.528 | 32 | 6.1 | 1483 | 2.5 | 4.7 | 1462 | 2.5 | 4.7 | 1.00 | 1.00 | 0.00 |
| Thailand | 0.765 | 217 | 3.8 | 22,051 | 32.2 | 20.3 | 21,900 | 32.0 | 20.2 | 0.95 | 0.99 | −0.04 |
| Turkey | 0.807 | 455 | 4.1 | 4044 | 5.0 | 4.2 | 3989 | 4.9 | 4.1 | 0.93 | 0.98 | −0.05 |
| Uganda | 0.528 | 46 | 7.3 | 1793 | 4.1 | 7.4 | 1534 | 3.5 | 6.6 | 0.95 | 0.85 | 0.10 |
| Ukraine | 0.750 | 125 | 6.1 | 1714 | 4.0 | 2.2 | 2106 | 4.9 | 2.6 | 1.06 | 1.23 | −0.17 |
| United Kingdom | 0.920 | 4356 | 9.9 | 6458 | 10.0 | 4.7 | 5415 | 8.4 | 3.6 | 0.97 | 0.84 | 0.13 |
| United States of America | 0.920 | 9536 | 16.8 | 35,868 | 11.2 | 6.7 | 27430 | 8.6 | 4.7 | 0.80 | 0.77 | 0.03 |
| Uzbekistan | 0.710 | 134 | 6.2 | 1352 | 4.2 | 5.2 | 1195 | 3.7 | 4.6 | 0.97 | 0.88 | 0.09 |
| Venezuela | 0.726 | 973 | 3.2 | 1077 | 3.3 | 3.3 | 1039 | 3.2 | 3.2 | 0.94 | 0.97 | −0.03 |
| Viet Nam | 0.693 | 117 | 5.7 | 24,493 | 25.7 | 22.9 | 24,571 | 25.7 | 22.9 | 0.95 | 1.00 | −0.05 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Su, C.-C.; Chen, B.-S.; Chen, H.-H.; Sung, W.-W.; Wang, C.-C.; Tsai, M.-C. Improved Trends in the Mortality-to-Incidence Ratios for Liver Cancer in Countries with High Development Index and Health Expenditures. Healthcare 2023, 11, 159. https://doi.org/10.3390/healthcare11020159
Su C-C, Chen B-S, Chen H-H, Sung W-W, Wang C-C, Tsai M-C. Improved Trends in the Mortality-to-Incidence Ratios for Liver Cancer in Countries with High Development Index and Health Expenditures. Healthcare. 2023; 11(2):159. https://doi.org/10.3390/healthcare11020159
Chicago/Turabian StyleSu, Chang-Cheng, Brian-Shiian Chen, Hsin-Hung Chen, Wen-Wei Sung, Chi-Chih Wang, and Ming-Chang Tsai. 2023. "Improved Trends in the Mortality-to-Incidence Ratios for Liver Cancer in Countries with High Development Index and Health Expenditures" Healthcare 11, no. 2: 159. https://doi.org/10.3390/healthcare11020159
APA StyleSu, C.-C., Chen, B.-S., Chen, H.-H., Sung, W.-W., Wang, C.-C., & Tsai, M.-C. (2023). Improved Trends in the Mortality-to-Incidence Ratios for Liver Cancer in Countries with High Development Index and Health Expenditures. Healthcare, 11(2), 159. https://doi.org/10.3390/healthcare11020159







