Stress, Burnout, and General Mental Health among Healthcare Workers in Poland during the Long-Lasting COVID-19 Pandemic
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Data Collection (Procedure, Instruments)
2.3. Ethics
2.4. Statistical Analysis
3. Results
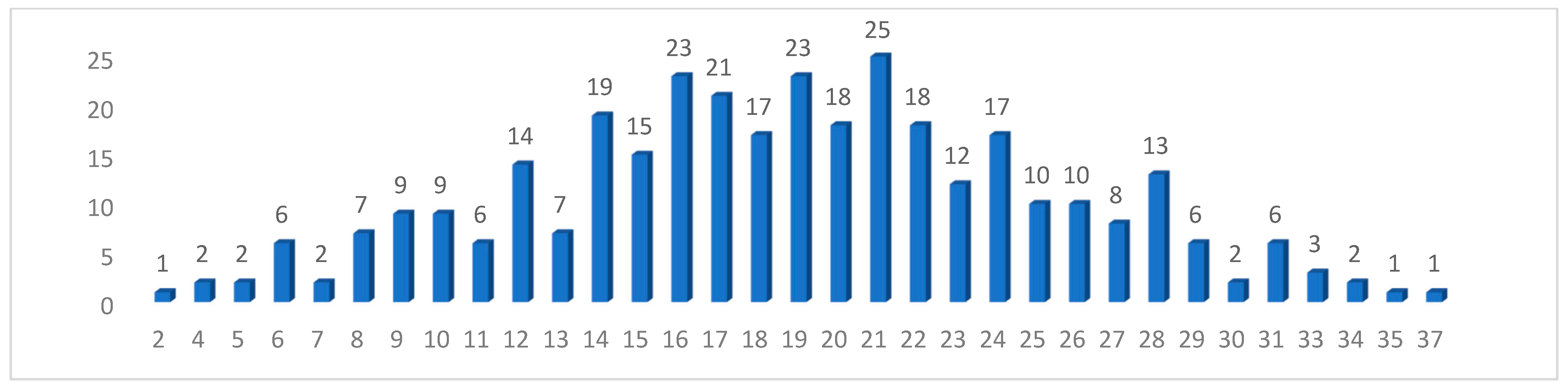
3.1. Description of the Group of Respondents
3.2. Level of Perceived Stress (PSS-10 Results)
3.3. Burnout Level (LBQ Scores)
3.4. Health Assessment (GHQ-28)
3.5. Correlations between the Level of Perceived Stress, the Assessment of Mental Health and Burnout, and the Variables Studied
3.6. Differences between Occupational Groups
3.7. The Importance of Working in a COVID Ward for the PSS-10, LBQ, and GHQ-28 Test Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Søvold, L.E.; Naslund, J.A.; Kousoulis, A.A.; Saxena, S.; Qoronfleh, M.W.; Grobler, C.; Münter, L. Prioritizing the Mental Health and Well-Being of Healthcare Workers: An Urgent Global Public Health Priority. Front. Public Health 2021, 9, 679397. [Google Scholar] [CrossRef]
- Zisook, S.; Doran, N.; Mortali, M.; Hoffman, L.; Downs, N.; Davidson, J.; Fergerson, B.; Rubanovich, C.K.; Shapiro, D.; Tai-Seale, M.; et al. Relationship between burnout and Major Depressive Disorder in health professionals: A HEAR report. J. Affect. Disord. 2022, 312, 259–267. [Google Scholar] [CrossRef]
- Liang, Y.; Wu, K.; Zhou, Y.; Huang, X.; Zhou, Y.; Zhang, X.Y. Mental health in frontline medical workers during the 2019 novel coronavirus disease epidemic in china: A comparison with the general population. Int. J. Environ. Res. Public Health 2020, 17, 6550. [Google Scholar] [CrossRef]
- Zhang, X.; Zhao, K.; Zhang, G.; Feng, R.; Chen, J.; Xu, D.; Liu, X.; Ngoubene-Atioky, A.J.; Huang, H.; Liu, Y.; et al. Occupational stress and mental health: A comparison between frontline medical staff and non-frontline medical staff during the 2019 novel coronavirus disease outbreak. Front. Psychiatry 2020, 11, 555703. [Google Scholar] [CrossRef]
- Han, S.; Choi, S.; Cho, S.; Lee, J.; Yun, J. Associations between the working experiences at frontline of covid-19 pandemic and mental health of korean public health doctors. BMC Psychiatry 2021, 21, 298. [Google Scholar] [CrossRef]
- Cocchiara, R.A.; Peruzzo, M.; Mannocci, A.; Ottolenghi, L.; Villari, P.; Polimeni, A.; Guerra, F.; La Torre, G. The Use of Yoga to Manage Stress and Burnout in Healthcare Workers: A Systematic Review. J. Clin. Med. 2019, 8, 284. [Google Scholar] [CrossRef]
- Khammissa, R.A.; Nemutandani, S.; Shangase, S.L.; Feller, G.; Lemmer, J.; Feller, L. The burnout construct with reference to healthcare providers: A narrative review. SAGE Open Med. 2022, 10, 20503121221083080. [Google Scholar] [CrossRef]
- Białek, K.; Sadowski, M. Level of stress and strategies used to cope with stress by physicians working in intensive care units. Anaesthesiol. Intensive Ther. 2019, 51, 361–369. [Google Scholar] [CrossRef]
- Santinello, M. LBQ Kwestionariusz Wypalenia Zawodowego Link. Podręcznik; Pracownia Testów Psychologicznych Polskiego Towarzystwa Psychologicznego: Warszawa, Poland, 2014. [Google Scholar]
- Peterson, U.; Demerouti, E.; Bergström, G.; Samuelsson, M.; Asberg, M.; Nygren, A. Burnout and physical and mental health among Swedish healthcare workers. J. Adv. Nurs. 2008, 62, 84–95. [Google Scholar] [CrossRef]
- Jaracz, M.; Rosiak, I.; Bertrand-Bucińska, A.; Jaskulski, M.; Nieżurawska, J.; Borkowska, A. Affective temperament, job stress and professional burnout in nurses and civil servants. PLoS ONE 2017, 12, e0176698. [Google Scholar] [CrossRef]
- Owoc, J.; Mańczak, M.; Tombarkiewicz, M.; Olszewski, R. Burnout, well-being, and self-reported medical errors among physicians. Pol. Arch. Intern. Med. 2021, 131, 626–632. [Google Scholar] [CrossRef] [PubMed]
- Nowakowska, I.; Rasińska, R.; Głowacka, M.D. The influence of factors of work environment and burnout syndrome on self-efficacy of medical staff. Ann. Agric. Environ. Med. AAEM 2016, 23, 304–309. [Google Scholar] [CrossRef] [PubMed]
- Kwiatkowska-Ciotucha, D.; Załuska, U.; Kozyra, C. The Perception of Occupation by Hospital Nurses in Poland and Germany in Terms of the Risk of Excessive Stress and Burnout as Well as Possible Coping and Preventive Solutions. Int. J. Environ. Res. Public Health 2021, 18, 1797. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation. Available online: https://covid19.who.int/ (accessed on 18 July 2023).
- The Official Website of the Government of Poland. Available online: www.gov.pl (accessed on 18 July 2023).
- Wojczyk, M.; Niewiadomska, E.; Kowalska, M. The Incidence Proportion of SARS-CoV-2 Infections and the Percentage of Deaths among Infected Healthcare Workers in Poland. J. Clin. Med. 2023, 12, 3714. [Google Scholar] [CrossRef]
- Park, S.Y.; Cheong, H.S.; Kwon, K.T.; Sohn, K.M.; Heo, S.T.; Lee, S.; Chung, U.S.; Lee, S.H. Guidelines for Infection Control and Burnout Prevention in Healthcare Workers Responding to COVID-19. Infect. Chemother. 2023, 55, 150–165. [Google Scholar] [CrossRef] [PubMed]
- Szwamel, K.; Kaczorowska, A.; Lepsy, E.; Mroczek, A.; Golachowska, M.; Mazur, E.; Panczyk, M. Predictors of the Occupational Burnout of Healthcare Workers in Poland during the COVID-19 Pandemic: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2022, 19, 3634. [Google Scholar] [CrossRef]
- Ulfa, M.; Azuma, M.; Steiner, A. Burnout status of healthcare workers in the world during the peak period of the COVID-19 pandemic. Front. Psychol. 2022, 13, 952783. [Google Scholar] [CrossRef]
- Hajebi, A.; Abbasinejad, M.; Zafar, M.; Hajebi, A.; Taremian, F. Mental Health, Burnout, and Job Stressors Among Healthcare Workers During the COVID-19 Pandemic in Iran: A Cross-Sectional Survey. Front. Psychiatry 2022, 13, 891430. [Google Scholar] [CrossRef]
- Ochronne śluzy z PWr w szpitalach w Legnicy i Wrocławiu. Available online: https://pwr.edu.pl/uczelnia/aktualnosci/ochronne-sluzy-z-pwr-w-szpitalach-w-legnicy-i-wroclawiu-11975.html (accessed on 18 July 2023).
- “Brawa Dla Was”. Podziękowania i Oklaski dla Walczących z Pandemią w Polskich Miastach. Available online: https://tvn24.pl/polska/koronawirus-w-polsce-brawa-dla-was-oklaski-dla-lekarzy-i-sluzb-medycznych-4546955 (accessed on 18 July 2023).
- Rośnie Hejt Wobec Medyków w Czasie Koronawirusa. Teraz to “Łajza, co Zarazę Przenosi”. Available online: https://lodz.wyborcza.pl/lodz/7,35136,25880123,klaskalismy-dla-medyka-bo-walczy-z-koronawiursem-teraz-to.html (accessed on 18 July 2023).
- Zatrzymaj Hejt. Available online: https://nszzp.pl/aktualnosci/zatrzymaj-hejt-czyli-wspierajmedyka/ (accessed on 18 July 2023).
- Apuke, O.D.; Omar, B. Modelling the antecedent factors that affect online fake news sharing on COVID-19: The moderating role of fake news knowledge. Health Educ. Res. 2020, 35, 490–503. [Google Scholar] [CrossRef]
- OECD. Health at a Glance 2019: OECD Indicators; OECD Publishing: Paris, France, 2019. [Google Scholar] [CrossRef]
- OECD. Health at a Glance 2021: OECD Indicators; OECD Publishing: Paris, France, 2021. [Google Scholar] [CrossRef]
- Juczyński, Z.; Ogińska-Bulik, N. Narzędzia Pomiaru Stresu i Radzenia Sobie ze Stresem; Pracownia Testów Psychologicznych Polskiego Towarzystwa Psychologicznego: Warszawa, Poland, 2012. [Google Scholar]
- Makowska, Z.; Merecz, D. Ocena Zdrowia Psychicznego na Podstawie Badań Kwestionariuszami Davida Goldberga Polska Adaptacja Kwestionariuszy Ogólnego Stanu Zdrowia Davida Goldberga: GHQ-12 i GHQ-28; Instytut Medycyny Pracy im Prof, J. Nofera: Łódź, Poland, 2001. [Google Scholar]
- Goldberg, D.; Williams, P. Podręcznik dla Użytkowników Kwestionariusza Ogólnego Stanu Zdrowia; Instytut Medycyny Pracy im Prof, J. Nofera: Łódź, Poland, 2001. [Google Scholar]
- Ciułkowicz, M.; Maciaszek, J.; Misiak, B.; Pałȩga, A.; Rymaszewska, J.; Szcześniak, D.M. Coping Strategies and Psychopathological Responses Among Medical and Non-medical Professionals—A Cross-Sectional Online Survey. Front. Psychiatry 2021, 12, 663224. [Google Scholar] [CrossRef]
- Akerstrom, M.; Sengpiel, V.; Hadžibajramović, E.; Carlsson, Y.; Graner, S.; Andersson, O.; Jonsson, M.; Naurin, E.; Veje, M.; Wessberg, A.; et al. The COPE Staff study: Study description and initial report regarding job satisfaction, work-life conflicts, stress, and burnout among Swedish maternal and neonatal healthcare workers during the COVID-19 pandemic. Int. J. Gynaecol. Obstet. 2023, 162, 989–997. [Google Scholar] [CrossRef]
- Lee, B.E.C.; Ling, M.; Boyd, L.; Olsson, C.; Sheen, J. The prevalence of probable mental health disorders among hospital healthcare workers during COVID-19: A systematic review and meta-analysis. J. Affect. Disord. 2023, 330, 329–345. [Google Scholar] [CrossRef]
- Babicki, M.; Szewczykowska, I.; Mastalerz-Migas, A. Mental Health in the Era of the Second Wave of SARS-CoV-2: A Cross-Sectional Study Based on an Online Survey among Online Respondents in Poland. Int. J. Environ. Res. Public Health 2021, 18, 2522. [Google Scholar] [CrossRef]
- Nadeem, M.U.; Kulich, S.J.; Bokhari, I.H. The assessment and validation of the depression, anxiety, and stress scale (DASS-21) among frontline doctors in Pakistan during fifth wave of COVID-19. Front. Public Health 2023, 11, 1192733. [Google Scholar] [CrossRef]
- Tabano, S.; Tassi, L.; Cannone, M.G.; Brescia, G.; Gaudioso, G.; Ferrara, M.; Colapietro, P.; Fontana, L.; Miozzo, M.R.; Croci, G.A.; et al. Mental health and the effects on methylation of stress-related genes in front-line versus other health care professionals during the second wave of COVID-19 pandemic: An Italian pilot study. Eur. Arch. Psychiatry Clin. Neurosci. 2023, 273, 347–356. [Google Scholar] [CrossRef]
- Alshekaili, M.; Hassan, W.; Al Said, N.; Al Sulaimani, F.; Jayapal, S.K.; Al-Mawali, A.; Chan, M.F.; Mahadevan, S.; Al-Adawi, S. Factors associated with mental health outcomes across healthcare settings in Oman during COVID-19: Frontline versus non-frontline healthcare workers. BMJ Open 2020, 10, e042030. [Google Scholar] [CrossRef]
- Yan, X.G.; Sun, H.Y.; Yoo, B.W. A Cross-Sectional Study on the Psychological Changes of Medical Personnel in Hospitals Who Experienced Special COVID-19 Situations. Inq. A J. Med. Care Organ. Provis. Financ. 2023, 60, 469580231161435. [Google Scholar] [CrossRef]
- Chhablani, N.; Choudhari, S.G. Behind the Frontline: A Review on the Impact of COVID-19 Pandemic on Healthcare Workers. Cureus 2022, 14, e29349. [Google Scholar] [CrossRef]
- Czepiel, D.; Hoek, H.W.; van der Markt, A.; Rutten, B.P.F.; Veling, W.; Schirmbeck, F.; Mascayano, F.; Susser, E.S.; van der Ven, E. The Association Between Exposure to COVID-19 and Mental Health Outcomes Among Healthcare Workers. Front. Public Health 2022, 10, 896843. [Google Scholar] [CrossRef]
- Zhao, Y.J.; Xing, X.; Tian, T.; Wang, Q.; Liang, S.; Wang, Z.; Cheung, T.; Su, Z.; Tang, Y.L.; Ng, C.H.; et al. Post COVID-19 mental health symptoms and quality of life among COVID-19 frontline clinicians: A comparative study using propensity score matching approach. Transl. Psychiatry 2022, 12, 376. [Google Scholar] [CrossRef]
- Abid, A.; Shahzad, H.; Khan, H.A.; Piryani, S.; Khan, A.R.; Rabbani, F. Perceived risk and distress related to COVID-19 in healthcare versus non-healthcare workers of Pakistan: A cross-sectional study. Hum. Resour. Health 2022, 20, 11. [Google Scholar] [CrossRef]
- Rosenström, T.; Tuisku, K.; Suvisaari, J.; Pukkala, E.; Junttila, K.; Haravuori, H.; Elovainio, M.; Haapa, T.; Jylhä, P.; Laukkala, T. Healthcare workers’ heterogeneous mental-health responses to prolonging COVID-19 pandemic: A full year of monthly follow up in Finland. BMC Psychiatry 2022, 22, 724. [Google Scholar] [CrossRef] [PubMed]
- Brooks, S.K.; Dunn, R.; Amlôt, R.; Rubin, G.J.; Greenberg, N. A Systematic, Thematic Review of Social and Occupational Factors Associated with Psychological Outcomes in Healthcare Employees During an Infectious Disease Outbreak. J. Occup. Environ. Med. 2018, 60, 248–257. [Google Scholar] [CrossRef]
- Rosales Vaca, K.M.; Cruz Barrientos, O.I.; Girón López, S.; Noriega, S.; More Árias, A.; Guariente, S.M.M.; Zazula, R. Mental health of healthcare workers of Latin American countries: A review of studies published during the first year of COVID-19 pandemic. Psychiatry Res. 2022, 311, 114501. [Google Scholar] [CrossRef] [PubMed]
- De Kock, J.H.; Latham, H.A.; Leslie, S.J.; Grindle, M.; Munoz, S.A.; Ellis, L.; Polson, R.; O’Malley, C.M. A rapid review of the impact of COVID-19 on the mental health of healthcare workers: Implications for supporting psychological well-being. BMC Public Health 2021, 21, 104. [Google Scholar] [CrossRef] [PubMed]
- Pappa, S.; Chen, J.; Barnett, J.; Chang, A.; Dong, R.K.; Xu, W.; Yin, A.; Chen, B.Z.; Delios, A.Y.; Chen, R.Z.; et al. A systematic review and meta-analysis of the mental health symptoms during the COVID-19 pandemic in Southeast Asia. Psychiatry Clin. Neurosci. 2022, 76, 41–50. [Google Scholar] [CrossRef]
- Rathod, S.; Pallikadavath, S.; Young, A.H.; Graves, L.; Rahman, M.M.; Brooks, A.; Soomro, M.; Rathod, P.; Phiri, P. Psychological impact of COVID-19 pandemic: Protocol and results of first three weeks from an international cross-section survey—Focus on health professionals. J. Affect. Disord. Rep. 2020, 1, 100005. [Google Scholar] [CrossRef] [PubMed]
- Xiong, N.N.; Fan, T.T.; Leonhart, R.; Fritzsche, K.; Liu, Q.; Luo, L.; Stein, B.; Waller, C.; Huang, M.; Müller, M.M.; et al. Workplace factors can predict the stress levels of healthcare workers during the COVID-19 pandemic: First interim results of a multicenter follow-up study. Front. Public Health 2022, 10, 1002927. [Google Scholar] [CrossRef] [PubMed]
- Ibar, C.; Fortuna, F.; Gonzalez, D.; Jamardo, J.; Jacobsen, D.; Pugliese, L.; Giraudo, L.; Ceres, V.; Mendoza, C.; Repetto, E.M.; et al. Evaluation of stress, burnout and hair cortisol levels in health workers at a University Hospital during COVID-19 pandemic. Psychoneuroendocrinology 2021, 128, 105213. [Google Scholar] [CrossRef]
- Briciu, V.; Leucuta, D.C.; Tőkés, G.E.; Colcear, D. Burnout, Depression, and Job Stress Factors in Healthcare Workers of a Romanian COVID-19 Dedicated Hospital, after Two Pandemic Years. Int. J. Environ. Res. Public Health 2023, 20, 4118. [Google Scholar] [CrossRef]
- Pan, S.J.; Qian, W.Y.; Yang, Y.P.; Zhang, M.X.; Hu, X.M.; Chen, H.X.; Tung, T.H. Evaluation of burnout among stay-behind healthcare workers during the current Omicron wave of COVID-19 in Taizhou, China. Front. Psychiatry 2022, 13, 1022881. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.; Wang, X.; Zhang, X.; Liu, W.; Wang, C. Burnout and associative emotional status and coping style of healthcare workers in COVID-19 epidemic control: A cross-sectional study. Front. Public Health 2023, 11, 1079383. [Google Scholar] [CrossRef] [PubMed]
- Choi, Y.E.; Lee, S.H.; Kim, Y.J.; Lee, J.G.; Yi, Y.H.; Tak, Y.J.; Kim, G.L.; Ra, Y.J.; Lee, S.Y.; Cho, Y.H.; et al. Burnout in healthcare workers in COVID-19-dedicated hospitals. J. Public Health 2023, 45, fdad038. [Google Scholar] [CrossRef]
- Burrowes, S.A.B.; Casey, S.M.; Pierre-Joseph, N.; Talbot, S.G.; Hall, T.; Christian-Brathwaite, N.; Del-Carmen, M.; Garofalo, C.; Lundberg, B.; Mehta, P.K.; et al. COVID-19 pandemic impacts on mental health, burnout, and longevity in the workplace among healthcare workers: A mixed methods study. J. Interprofessional Educ. Pract. 2023, 32, 100661. [Google Scholar] [CrossRef]
- Epifanio, M.S.; La Grutta, S.; Piombo, M.A.; Riolo, M.; Spicuzza, V.; Franco, M.; Mancini, G.; De Pascalis, L.; Trombini, E.; Andrei, F. Hopelessness and burnout in Italian healthcare workers during COVID-19 pandemic: The mediating role of trait emotional intelligence. Front. Psychol. 2023, 14, 1146408. [Google Scholar] [CrossRef]
- Załuski, M.; Makara-Studzińska, M. Wzajemne relacje między wypaleniem zawodowym, pracą emocjonalną i zaangażowaniem w pracę u pracowników ochrony zdrowia [The reciprocal relationship between occupational burnout, emotional labor and work engagement in healthcare specialists]. Med. Pr. 2019, 70, 711–722. [Google Scholar] [CrossRef]
- Maciaszek, J.; Ciulkowicz, M.; Misiak, B.; Szczesniak, D.; Luc, D.; Wieczorek, T.; Fila-Witecka, K.; Gawlowski, P.; Rymaszewska, J. Mental Health of Medical and Non-Medical Professionals during the Peak of the COVID-19 Pandemic: A Cross-Sectional Nationwide Study. J. Clin. Med. 2020, 9, 2527. [Google Scholar] [CrossRef]
- Kolivand, P.; Hosseindoost, S.; Kolivand, Z.; Gharaylou, Z. Psychosocial impact of COVID-19 2 years after outbreak on mental health of medical workers in Iran. Middle East Curr. Psychiatry Ain Shams Univ. 2023, 30, 4. [Google Scholar] [CrossRef]
- Babamiri, M.; Bashirian, S.; Khazaei, S.; Sohrabi, M.S.; Heidarimoghadam, R.; Mortezapoor, A.; Zareian, S. Burnout and Mental Health of COVID-19 Frontline Healthcare Workers: Results from an Online Survey. Iran. J. Psychiatry 2022, 17, 136–143. [Google Scholar] [CrossRef]
- Jiang, C.; Jiang, W.; Yue, Y.; Li, L.; Sun, T.; Chen, G.; Xu, W.; Shah, S.M.; Liu, X.; Chen, S.; et al. The trends of psychosomatic symptoms and perceived stress among healthcare workers during the COVID-19 pandemic in China: Four cross-sectional nationwide surveys, 2020-2023. Psychiatry Res. 2023, 326, 115301. [Google Scholar] [CrossRef]
- González Baltazara, R.; Hidalgo Santacruza, G.; León Cortésa, S. Quality of work life and mental health in primary care physicians. Procedia Manuf. 2015, 3, 4935–4940. [Google Scholar] [CrossRef][Green Version]
- Witczak-Błoszyk, K.; Krysińska, K.; Andriessen, K.; Stańdo, J.; Czabański, A. Work-Related Suicide Exposure, Occupational Burnout, and Coping in Emergency Medical Services Personnel in Poland. Int. J. Environ. Res. Public Health 2022, 19, 1156. [Google Scholar] [CrossRef] [PubMed]
- Shoji, K.; Lesnierowska, M.; Smoktunowicz, E.; Bock, J.; Luszczynska, A.; Benight, C.C.; Cieslak, R. What Comes First, Job Burnout or Secondary Traumatic Stress? Findings from Two Longitudinal Studies from the U.S. and Poland. PLoS ONE 2015, 10, e0136730. [Google Scholar] [CrossRef]
- Giusti, E.M.; Veronesi, G.; Callegari, C.; Borchini, R.; Castelnuovo, G.; Gianfagna, F.; Iacoviello, L.; Ferrario, M.M. Pre-pandemic burnout and its changes during the COVID-19 outbreak as predictors of mental health of healthcare workers: A lesson to be learned. Psychiatry Res. 2023, 326, 115305. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Arriaga, R.J.; Dominguez-Rodriguez, A.; Herdoiza-Arroyo, P.E.; Robles-Garcia, R.; de la Rosa-Gómez, A.; Figueroa González, J.A.; Muñoz Anacona, Y.A. Suicide risk and associated factors in healthcare workers seeking psychological support during COVID-19: A cross-sectional study. Psychol. Health Med. 2023, 1–15, advance online publication. [Google Scholar] [CrossRef]
| Characteristic | N | % |
|---|---|---|
| Total | 335 | |
| Gender | ||
| Female | 289 | 86.3% |
| Male | 46 | 13.7% |
| Education | ||
| higher education | 235 | 70.2% |
| bachelor’s, engineer | 50 | 14.9% |
| secondary education | 50 | 14.9% |
| Occupational group | ||
| medical | 195 | 58.2% |
| nurse | 109 | 32.5% |
| physician | 46 | 13.7% |
| other medical workers | 40 | 11.9% |
| other specialists | 36 | 10.9% |
| administration | 140 | 41.8% |
| Health status | ||
| chronic diseases | 97 | 29% |
| depression | 43 | 12.8% |
| anxiety | 28 | 8.4% |
| COVID-19 infection | 126 | 37.6% |
| COVID-19 ward | 92 | 27.5% |
| M | SD | D | Min | Max | |
|---|---|---|---|---|---|
| Psychophysical exhaustion | 19.55 | 6.753 | 13 | 6 | 35 |
| Lack of engagement with customers | 17.71 | 5.889 | 12 | 7 | 36 |
| Feeling of professional ineffectiveness | 13.86 | 5.058 | 9 | 6 | 33 |
| Disappointment | 17.07 | 7.292 | 11 | 6 | 35 |
| Total | 68.19 | 20.357 | 70 | 30 | 134 |
| M | SD | D | Min | Max | |
|---|---|---|---|---|---|
| A: somatic symptoms | 9.23 | 4.626 | 8 | 0 | 21 |
| B: anxiety, insomnia | 9.13 | 5.066 | 7 | 0 | 21 |
| C: functional disorders | 8.81 | 3.284 | 7 | 3 | 21 |
| D: symptoms of depression | 3.31 | 4.489 | 0 | 0 | 21 |
| Total | 30.47 | 14.905 | 17 | 5 | 84 |
| A Somatic Symptoms | B Anxiety, Insomnia | C Functional Disorders | D Symptoms of Depression | Stress | |
|---|---|---|---|---|---|
| Psychophysical exhaustion | 0.517 *** | 0.560 *** | 0.548 *** | 0.474 *** | 0.612 *** |
| Lack of engagement with customers | 0.308 *** | 0.256 *** | 0.294 *** | 0.206 *** | 0.308 *** |
| Feeling of professional ineffectiveness | 0.393 *** | 0.466 *** | 0.566 *** | 0.488 *** | 0.579 *** |
| Disappointment | 0.425 *** | 0.470 *** | 0.485 *** | 0.419 *** | 0.510 *** |
| Stress | 0.632 *** | 0.766 *** | 0.650 ** | 0.627 *** | - |
| PSS-10 | GHQ-28 | ||||
|---|---|---|---|---|---|
| Health Problems | Stress | Somatic Symptoms | Anxiety, Insomnia | Functional Disorders | Symptoms of Depression |
| Chronic illness | 0.033 | 0.073 | 0.085 | 0.093 | 0.119 ** |
| Depression | 0.128 ** | 0.122 ** | 0.119 ** | 0.139 ** | 0.189 *** |
| Anxiety disorders | 0.177 *** | 0.188 *** | 0.184 ** | 0.165 ** | 0.143 ** |
| Other mental illnesses | 0.070 | 0.061 | 0.062 | 0.015 | 0.027 |
| Chronic Illness | Lack | ||||||
|---|---|---|---|---|---|---|---|
| M | SD | M | SD | t | Df | d | |
| Symptoms of depression | 4.14 | 5.264 | 2.97 | 4.097 | 1.974 ** | 145 | 0.271 |
| Depression/Mood disorders | Lack | ||||||
| M | SD | M | SD | t | Df | d | |
| Somatic symptoms | 10.70 | 4.950 | 9.01 | 4.546 | 2.246 ** | 333 | 0.371 |
| Anxiety, insomnia | 10.70 | 5.092 | 8.90 | 5.029 | 2.188 ** | 333 | 0.358 |
| Functional disorders | 10.00 | 3.703 | 8.64 | 3.188 | 2.292 ** | 333 | 0.427 |
| Symptoms of depression | 5.51 | 6.181 | 2.98 | 4.099 | 2.600 ** | 333 | 0.578 |
| Anxiety disorders | Lack | ||||||
| M | SD | M | SD | t | Df | d | |
| Somatic symptoms | 12.11 | 5.202 | 8.96 | 4.488 | 3.499 *** | 333 | 0.677 |
| Anxiety, insomnia | 12.21 | 4.740 | 8.85 | 5.008 | 3.421 *** | 333 | 0.661 |
| Functional disorders | 10.61 | 4.289 | 8.65 | 3.135 | 2.360 ** | 333 | 0.588 |
| Symptoms of depression | 5.43 | 6.735 | 3.11 | 4.190 | 2.634 *** | 333 | 0.513 |
| Definitely Not | Rather Not | It is Hard to Say | Probably Yes | Definitely Yes | |
|---|---|---|---|---|---|
| Do you have access to consultation with a psychologist in the workplace? | 79 | 80 | 61 | 70 | 45 |
| In connection with your work, do you feel the need to consult a psychologist? | 76 | 125 | 62 | 52 | 20 |
| GHQ-28 | A Somatic Symptoms | B Anxiety, Insomnia | C Functional Disorders | D Symptoms of Depression | PSS-10 Stress |
|---|---|---|---|---|---|
| In connection with your work, do you feel the need to consult a psychologist? | 0.147 *** | 0.174 *** | 0.151 *** | 0.180 *** | 0.182 *** |
| LBQ | Psychophysical exhaustion | Lack of engagement with customers | Feeling of professional ineffectiveness | Disappointment | |
| In connection with your work, do you feel the need to consult a psychologist? | 0.262 *** | 0.193 *** | 0.141 *** | 0.166 *** |
| Group A | Group B | Group C | Group D | Group E | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | M | SD | M | SD | F | |
| PSS-10 | 18.74 | 6.76 | 18.37 | 7.23 | 19.48 | 5.87 | 17 | 5.73 | 19.38 | 6.17 | 1.08 |
| LBQ PE | 18.83 | 6.33 | 21.65 | 7.2 | 20.08 | 6.81 | 18.61 | 6.63 | 19.51 | 6.92 | 1.67 |
| LICR | 17.14 | 5.81 | 17.8 | 5.55 | 18.6 | 5.73 | 17.28 | 6.23 | 18.09 | 6.09 | 0.64 |
| PI | 13.77 | 4.82 | 14.93 | 5.56 | 13.95 | 4.53 | 12.39 | 3.88 | 13.96 | 5.56 | 1.31 |
| DIS | 15.1 | 6.43 | 15.63 | 7.32 | 18.63 | 6.64 | 17 | 7.3 | 19.2 | 7.76 | 5.38 *** |
| GHQ-28 A | 9.64 | 5.06 | 8.02 | 4.1 | 8.95 | 4.1 | 8.28 | 4.07 | 9.76 | 4.67 | 1.78 |
| B | 8.98 | 5.26 | 8.74 | 5.02 | 9.68 | 5.04 | 8.06 | 4.39 | 9.62 | 5.12 | 0.85 |
| C | 8.75 | 3.12 | 8.7 | 3.61 | 8.63 | 2.63 | 8.28 | 3.12 | 9.18 | 3.59 | 0.62 |
| D | 2.95 | 4.03 | 3.2 | 5.05 | 3.38 | 3.83 | 3 | 4.39 | 3.81 | 4.96 | 0.54 |
| Yes, I Work | Worked | I Did Not Work | Does Not Apply to Me | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Scale | M | SD | M | SD | M | SD | M | SD | F | ||
| Group A | PSS-10 | 17.77 | 7.37 | 17.57 | 6.88 | 19.72 | 6.46 | 14.33 | 2.52 | 1.21 | |
| Group B | PSS-10 | 19.64 | 6.31 | 15.75 | 5.75 | 18.65 | 8.11 | 18.00 | 0.00 | 0.71 | |
| Group A | LBQ | PE | 17.61 | 6.64 | 18.50 | 6.62 | 19.82 | 6.04 | 12.67 | 3.51 | 1.89 |
| LICR | 16.61 | 5.01 | 18.71 | 6.90 | 17.25 | 5.99 | 13.00 | 4.00 | 0.94 | ||
| PI | 13.58 | 5.76 | 12.29 | 2.56 | 14.34 | 4.68 | 11.00 | 4.58 | 1.08 | ||
| DIS | 13.35 | 6.30 | 15.93 | 6.62 | 16.13 | 6.30 | 8.33 | 3.22 | 2.57 | ||
| Group B | LBQ | PE | 22.64 | 6.95 | 22.38 | 6.28 | 21.23 | 7.80 | 16.00 | 0.00 | 0.32 |
| LICR | 20.36 | 5.84 | 17.88 | 5.33 | 16.69 | 5.45 | 18.00 | 0.00 | 1.14 | ||
| PI | 15.64 | 5.03 | 12.25 | 4.98 | 15.50 | 5.98 | 14.00 | 0.00 | 0.77 | ||
| DIS | 17.27 | 6.92 | 13.88 | 6.66 | 15.58 | 7.90 | 13.00 | 0.00 | 0.36 | ||
| Group A | GHQ-28 | A | 9.90 | 5.74 | 11.21 | 6.52 | 9.28 | 4.34 | 7.00 | 3.61 | 0.85 |
| B | 9.03 | 5.75 | 9.86 | 5.48 | 8.92 | 5.07 | 5.67 | 2.89 | 0.52 | ||
| C | 8.42 | 3.52 | 8.71 | 3.36 | 9.02 | 2.94 | 7.00 | 0.00 | 0.57 | ||
| D | 2.81 | 4.44 | 2.79 | 4.37 | 3.16 | 3.87 | 1.00 | 1.73 | 0.31 | ||
| Group B | GHQ-28 | A | 7.36 | 3.85 | 7.25 | 3.66 | 8.54 | 4.46 | 8.00 | 0.00 | 0.31 |
| B | 8.45 | 4.44 | 8.25 | 4.89 | 9.00 | 5.53 | 9.00 | 0.00 | 0.06 | ||
| C | 8.91 | 2.55 | 8.50 | 3.38 | 8.62 | 4.20 | 10.00 | 0.00 | 0.06 | ||
| D | 3.18 | 2.79 | 1.38 | 3.11 | 3.85 | 6.20 | 1.00 | 0.00 | 0.54 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Budzyńska, N.; Moryś, J. Stress, Burnout, and General Mental Health among Healthcare Workers in Poland during the Long-Lasting COVID-19 Pandemic. Healthcare 2023, 11, 2617. https://doi.org/10.3390/healthcare11192617
Budzyńska N, Moryś J. Stress, Burnout, and General Mental Health among Healthcare Workers in Poland during the Long-Lasting COVID-19 Pandemic. Healthcare. 2023; 11(19):2617. https://doi.org/10.3390/healthcare11192617
Chicago/Turabian StyleBudzyńska, Natalia, and Joanna Moryś. 2023. "Stress, Burnout, and General Mental Health among Healthcare Workers in Poland during the Long-Lasting COVID-19 Pandemic" Healthcare 11, no. 19: 2617. https://doi.org/10.3390/healthcare11192617
APA StyleBudzyńska, N., & Moryś, J. (2023). Stress, Burnout, and General Mental Health among Healthcare Workers in Poland during the Long-Lasting COVID-19 Pandemic. Healthcare, 11(19), 2617. https://doi.org/10.3390/healthcare11192617






