1. Introduction
Elbow pain (EP) is a common sports injury in various overhead sports [
1]. As it is considered an overhead sport, scholars have always been interested in swimming [
2]. However, EP in swimming has been neglected due to the influence of people’s general cognition of sports injuries caused by swimming, with most believing that swimming injuries are concentrated in the shoulder, lower back, and knee and ankle joints [
3]. Meanwhile, due to the influence of different continents and regions, attention to swimming events, EP in swimming has received a low level of attention for a long time. However, the United States, a sports powerhouse, has initiated relevant researches on EP in swimming in the last 10 years [
4].
In China, research on and exploration of EP in swimming are in their initial stages [
5]. As a popular sport, swimming attracts ordinary young people to become elite athletes [
6]. In recent years, the total number of registered elite swimmers on the Chinese mainland has increased steadily, most recently totaling 87,886, but the number of athletes who have been forced to quit because of various overuse injuries has increased yearly [
7]. Although shoulder injuries have the highest incidence rate, lower back pain and injuries of joints such as the knees, ankles, and elbows have been on the rise in recent years [
5,
8,
9]. However, there is a serious lack research evidence on the issue of EP in elite freestyle swimmers. Therefore, assessing EP in this population is a necessary measure to reduce the risk of early retirement from sporting careers.
There are a few Chinese researchers who have initiated investigations into the condition of EP in swimming. Such studies are valuable for assessing the health status of elite swimmers’ upper limbs, highlighting specific risks that require attention, and providing information for targeted interventions aimed at preventing EP [
1,
5,
10,
11]. However, the majority of studies in the existing literature have primarily focused on exploring the relationship between the anthropometric variables of EP athletes (such as height, weight, gender, and forearm length) and their sports performance, as well as the relevance of these factors in participant selection [
12,
13,
14,
15,
16]. The emphasis has been on investigating the impact of these variables and their connections with performance rather than delving into whether these factors directly contribute to the onset of EP [
17,
18]. This lack of investigation has hindered athletes and coaches from making informed decisions to facilitate the return of EP patients to the sport accordingly. A previous study investigated sports injuries in 194 elite swimmers in the city of Shanghai and the province of Zhejiang; its results showed that the incidence of EP was as high as 21% with an upward trend, ranking fourth among swimmers with a high incidence of sports overuse injuries [
11]. This incidence of EP problems among freestyle swimmers is 7–13% higher than in the other three swimming-style athletes [
11,
19]. However, Tianjin, as one of the main training bases for elite swimmers in China, has been registering over 1000 swimming athletes annually since 2017 [
20]. Unlike Shanghai and Zhejiang province, Tianjin has paid little attention to the impact of EP among this population [
10,
21]. Currently, China has not established an Injury Surveillance System (ISS) similar to the National Collegiate Athletic Association (NCAA) in the United States to monitor real-time data on various sports injuries [
3]. This has resulted in a lack of coverage of elite swimming athletes throughout China in EP-related research, which must rely on regional sampling methods for investigation. In addition, the anthropometric characteristics of EP elite swimmers are essential data support for establishing a sports injury detection system in China. In summary, investigating EP problems among elite freestyle swimmers in Tianjin will fill the gap in the study of EP in swimming.
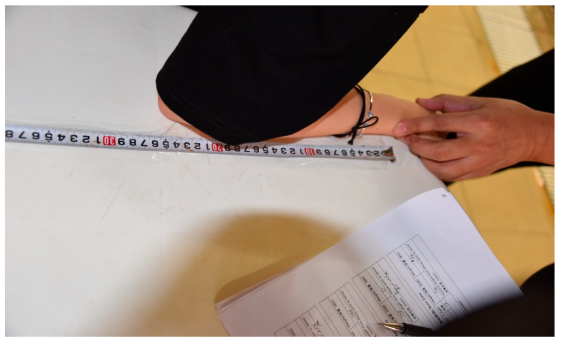
In summary, regional sampling evaluation is one of the primary methods for studying EP in swimming athletes, given the state of development of sports science in China. Regular assessment of athletes’ physiological parameters over time is a necessary injury prevention strategy to safeguard their health and professional safety [
22,
23]. Evaluating the anthropometric characteristics of EP elite swimmers will help establish a similar ISS system that can offer real-time monitoring of various sports injuries and provide data support in the near future. Thus, to the best of our knowledge, this is the first study to evaluate the distribution and prevalence of elbow pain (EP) among elite freestyle swimmers in Tianjin, China. The purpose of this study was to assess the number of swimmers with EP and their anthropometric characteristics in Tianjin, China, as well as the correlation between the anthropometric characteristics of EP swimmers and the assessment results, which will identify factors associated with EP.
3. Results
3.1. Descriptive Statistical Analysis Results of the 311 Subjects
All 311 eligible subjects completed all measurements. The demographic findings in
Table 1 report that the number of EP patients exceeded half of the total number of participants (183 EP patients, accounting for 58.8%). The demographic results by gender indicate that the females were approximately one year younger than the males. Among all EP patients, the number of males was approximately three times that of females. According to gender and pain classification, the number of males with slight pain EP was approximately 3.5 times that of females. In the critical pain category, the proportion of males was approximately 1% higher than females. A total of three participants provided medical diagnosis certificates, which confirmed that they were suffering symptoms of “golfer’s elbow” (
n = 1) and “tennis elbow” (
n = 2), respectively.
Table 2 reports that the majority of the EP patients were from a professional swimming team (PST), accounting for 86.9%. Among them, the number of male EP patients was highest, which was approximately 2.5 times that of females. The average weekly training hours for females was approximately twice that of males. The duration of EP history was similar for both male and female EP patients, which exceeded two weeks. The difference in the 50 m freestyle swimming personal best (PB) time between male and female EP patients was approximately within 0.1 s.
3.2. Pain Category and the Anthropometric Characteristics of 183 EP Subjects
Based on the scoring categories of the UFLE and BPDE, the specific pain categories were determined for all 183 EP patients.
Table 3 presents detailed information regarding these findings. The main results indicate that 147 EP patients were classified into the slight pain category and 36 EP patients into the critical pain category. No EP patients were categorized as having moderate pain.
Among the two pain categories and the EP patients’ anthropometric characteristics, it was found that female EP patients with critical pain had higher values than EP patients with slight pain in terms of age, height, and weight by approximately 0.5 years, 1 cm, and 0.5 kg, respectively. Male EP patients with critical pain had higher values than EP patients with slight pain in terms of age and height, but lower values in terms of weight, with the difference accounting for approximately 1 year, 0.5 cm, and 1 kg, respectively.
Both male and female EP patients with critical pain had longer left forearm lengths compared to those with slight pain, by approximately 2 and 8 mm, respectively. However, when comparing the right forearm length, female EP patients with critical pain had longer lengths than those with slight pain, by approximately 6 mm, while male EP patients with critical pain had shorter lengths than those with slight pain, by approximately 1 mm. All EP patients with critical pain were right-handed (accounting for 100%), while only four in five of EP patients with slight pain were right-handed.
3.3. Correlation between the UFLE and BPDE Scores and All Variables in 183 EP Subjects
The results of the Pearson correlation analysis (
Table 4) indicate that among all variables, gender, weight, organization, and left and right forearm lengths had statistical significance, with
p-values of less than 0.05. The correlation between gender and UFLE and BPDE scores yielded
r-values of −0.299 and −0.152, indicating negative correlations. The correlation between weight and BPDE scores was positive, with an
r-value of 0.146. Organization and left and right forearm lengths demonstrated positive correlations with the ULFE and BPDE scores, with
r-values of 0.648/0.725, 0.409/0.515, and 0.399/0.514, respectively.
Effect and Predictors of the Anthropometric and Demographic Variables on the UFLE and BPDE Scores
The results of the multiple regression analysis (
Table 5) indicate that, among all anthropometric and demographic variables, gender, age, right forearm length, average weekly training hours, and organization had statistical significance, with
p-values of less than 0.05. Gender exhibited a negative correlation with the ULFE and BPDE scores, with β-values of −21.649 and −13.823, respectively. The effects of age, average weekly training hours, organization, and right forearm length showed positive correlations with the ULFE and BPDE scores, with β-values of 0.731/0.484, 0.607/0.572, 9.605/11.431, and 0.518/0.521, respectively.
The elbow pain predictor results of the binary logistic regression (
Table 6) indicate that among all variables, gender and left/right forearm length had statistical significance, with
p-values of less than 0.05. The odds ratio (OR) for the gender factor in ULFE scores ≥ 35 (critical pain category) and BPDE scores ≥ 30 (critical pain category) as the cut-off threshold was calculated to be less than 1 (OR = 0.376), which indicates a protective factor. This suggests that male swimmers tend to have lower assessment scores and lean toward the “slight pain” category. For the left/right forearm length factor, calculated in ULFE scores ≥ 35 (critical pain category) and BPDE scores ≥ 30 (critical pain category) as the cut-off threshold, the ORs were both greater than 1 the (OR = 1.168/1.177), indicating a risk factor. This implies that the longer the forearm length of EP swimmers, the more severe the intensity of their pain sensations.
4. Discussion
In this study, we obtained precise results regarding the number of EP patients, pain categorization, anthropometric characteristics, and distribution among elite freestyle swimmers in Tianjin, China. We also examined the contributing factors to EP. The observed high prevalence rate of EP (accounting for 58.8% of the total subjects) raises concerns about the occupational health development of elite swimmers in China.
The significant majority of male compared to female EP patients among the total number of 183 EP patients indicates that a significant number of male elite swimmers in China may be struggling with EP without finding appropriate solutions. This phenomenon also highlights the current state of occupational health development among Chinese swimmers, which exhibits a gender disparity with better occupational health levels observed among female athletes [
37]. Therefore, our recommendation is that coaches need to pay attention to the occupational health development of male swimmers. Providing more opportunities for communication during daily training would allow these individuals to express their requirements and concerns more effectively [
38]. This means that once an athlete experiences any discomfort, the coach can address it promptly and make a correct decision to prevent their EP from worsening.
This study’s evidence of a correlation between age, height, weight, right forearm length, and organization with the scores of the two EP assessments (UFLE and BPDE) indicates that the root cause of EP problems may lie within these factors. Regarding age, healthy athletes tend to be younger than EP patients. This suggests that the occupational health level of athletes declines with increasing age [
39]. Therefore, we recommend that coaches should provide more sports protection measures and rest time for older athletes. Compared to healthy athletes, EP patients exhibit the anthropometric characteristics of shorter height, lighter weight, and shorter right forearm length. This indicates that athletes who possess these three features are more likely to experience EP problems than others. Therefore, during the athlete selection phase, such as teenagers between the ages of 15 and 18, relevant professionals should exclude individuals with these three anthropometric features or advise them not to participate in competitive swimming training to reduce the risk of EP [
40]. In terms of organizations, although a certain number of EP patients come from university teams (UTs), professional swimming teams (PSTs) remain the primary hotbed for the greatest number of EP patients. Their training management strategies may have deficiencies, leading to a lack of timely and effective protection and intervention measures for EP swimmers to return to the sport promptly. Therefore, we suggest that swimming teams and clubs at all levels should consider implementing “periodization theory” as the training management principle to address deficiencies, which can provide athletes with maximum rest during busy training schedules [
41]. Finally, ligament and tendon injuries could also be among the causes of EP [
42,
43,
44,
45]. In some clinical medical studies and anatomical literature, baseball players with elbow injures typically require surgical rehabilitation [
44,
46]. Therefore, for EP swimmers identified as experiencing critical pain in this study, we recommend further medical examinations to mitigate the risk of ligament and tendon injuries exacerbating their EP condition.
The results of pain categorization in EP patients show that the number of subjects with slight pain was approximately four times that of those with critical pain. This suggests that these subjects did not promptly report their EP and did not receive effective intervention measures to alleviate their EP discomforts. Therefore, we recommend that coaches and relevant professionals conduct frequent assessments of the occupational health of swimming athletes, aiming to detect and treat EP issues at an early stage to prevent the risk of deterioration [
47]. Furthermore, with regards to the anthropometric characteristics of EP patients in relation to pain categorization, it was observed that the right forearm length of EP patients with slight pain was shorter than that of those with critical pain. This suggests that forearm length may impact the pain classification of EP patients, with a shorter forearm length being associated with lower levels of EP pain [
48,
49]. Therefore, based on the EP assessment scoring criteria, we recommend that EP patients with slight pain should undergo unloaded or lightly loaded upper limb strength training, such as isometric training, to improve arm muscle strength and endurance around the elbow joint, as an intervention method rather than relying solely on medication [
50,
51,
52]. For EP patients with critical pain, they should exercise caution when selecting potential intervention methods. Upper limb strength training remains essential, but if the patient experiences any discomfort during the process, it should be immediately discontinued, and EP assessment or medical examination, such as magnetic resonance imaging (MRI), should be performed to avoid the risk of further injury [
53].
In summary, despite the prevalence of EP issues among elite freestyle swimmers in Tianjin, China, potential solutions to reduce the number and risk of EP cases include improving training management strategies, optimizing athlete selection criteria, increasing the frequency of athlete occupational health assessments, and providing timely rest and intervention measures. Additionally, the anthropometric data of EP patients can support the establishment of a sports injury detection system in Chinese swimming teams in the near future.
5. Limitations
The sample inclusion and exclusion criteria may have overlooked some subjects who also suffer from EP, such as butterfly, backstroke, breaststroke, and synchronized swimmers. Additionally, young athletes under the age of 18 and disabled athletes were not included in the evaluation scope. Consequently, results based on such inclusion and exclusion criteria are preferred. Furthermore, factors such as ligament and tendon injuries, as well as shoulder strength, may contribute to EP among swimmers. These aspects were not investigated in the current study, potentially accounting for variations in the results. Therefore, it is advisable for future research to consider the correlation between these factors and elbow pain.
6. Conclusions
The high prevalence of EP issues among elite freestyle swimmers in Tianjin, China, necessitates increased attention from professionals. Special focus should be directed toward young male athletes within the EP swimmer cohort. Regular proactive assessments would benefit these swimmers. Organizational level and training duration emerged as pivotal factors impacting the elbow joint health of swimmers. Athletes of older age, longer forearm length, higher body weight, and taller stature should be prioritized for observation and assessment, and these traits characterize the EP swimmer profile. Finally, it is important to acknowledge the limitations of this study, including the limited sample range and the technical diversity of swimming. We acknowledge that the current inclusion criteria excluded young athletes (under 18 years old) and disabled athletes, and it is unknown whether EP exists in swimmers primarily practicing backstroke, breaststroke, and butterfly. Therefore, we plan to address these topics in future research.