Observational Prospective Study to Determine the Efficacy of ‘Non-Slip Socks’ vs. ‘Adequate Footwear’ Regarding the Number of Falls Observed among Admitted Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Evaluation of Patients
2.3. Statistical Analysis
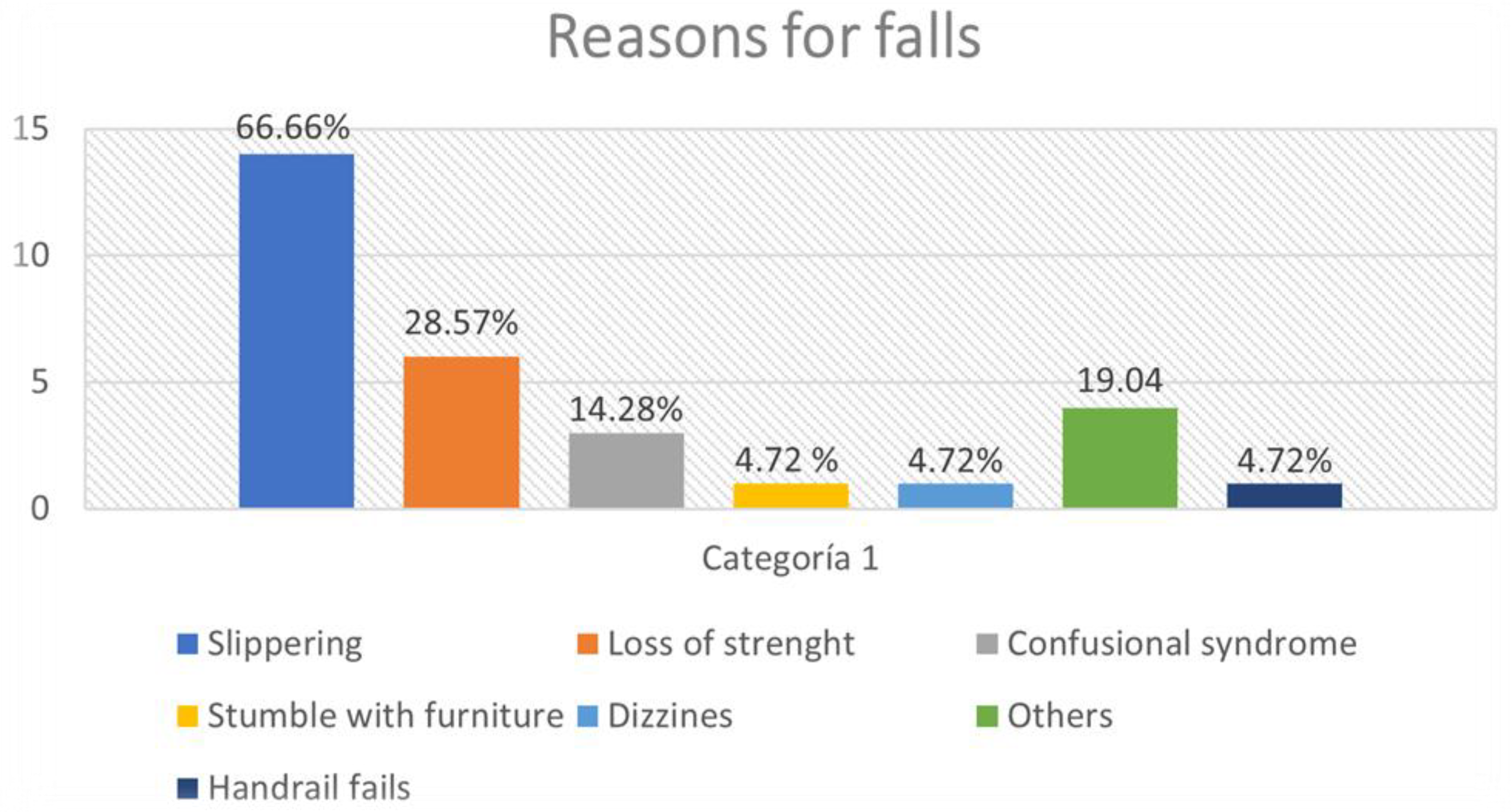
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Caídas. Available online: https://www.who.int/es/news-room/fact-sheets/detail/falls (accessed on 19 February 2023).
- Avanecean, D.; Calliste, D.; Contreras, T.; Lim, Y.; Fitzpatrick, A. Effectiveness of patient-centered interventions on falls in the acute care setting compared to usual care: A systematic review. JBI Database Syst. Rev. Implement. Rep. 2017, 15, 3006–3048. [Google Scholar] [CrossRef] [PubMed]
- Cameron, I.D.; Dyer, S.M.; Panagoda, C.E.; Murray, G.R.; Hill, K.D.; Cumming, R.G.; Kerse, N. Interventions for preventing falls in older people in care facilities and hospitals. Cochrane Database Syst. Rev. 2018, 9, CD005465. [Google Scholar] [CrossRef]
- Sato, N.; Hase, N.; Osaka, A.; Sairyo, K.; Katoh, S. Falls among Hospitalized Patients in an Acute Care Hospital: Analyses of Incident Reports. J. Med. Investig. 2018, 65, 81–84. [Google Scholar] [CrossRef]
- Bouldin, E.L.D.; Andresen, E.M.; Dunton, N.E.; Simon, M.; Waters, T.M.; Liu, M.; Daniels, M.J.; Mion, L.C.; Shorr, R.I. Falls Among Adult Patients Hospitalized in the United States: Prevalence and Trends. J. Patient Saf. 2013, 9, 13–17. [Google Scholar] [CrossRef]
- Falls. 2018. Available online: https://www.nhs.uk/conditions/falls/ (accessed on 19 February 2023).
- Urruela Oliván, M.; Gómez Ahedo, E.; Iglesias Astorga, C.; Valtierra Aragón, M.T.; González Molina, Y.; Escobar Martínez, A.; Latorre, M. Caídas en un hospital de agudos: Características del paciente. Rev. Multidiscip. Gerontol. 2002, 12, 14–18. [Google Scholar]
- Calvo Mesa, M.; Riu Camps, M.; Villares García, M.J. In-hospital accidental falls: A reality. Rev. Enferm. Barc. Spain 2001, 24, 25–30. [Google Scholar]
- Aranda-Gallardo, M.; Morales-Asencio, J.M.; Canca-Sanchez, J.C.; Toribio-Montero, J.C. Circumstances and causes of falls by patients at a Spanish acute care hospital. J. Eval. Clin. Pract. 2014, 20, 631–637. [Google Scholar] [CrossRef]
- Lobo-Rodríguez, C.; García-Pozo, A.M.; Gadea-Cedenilla, C.; Moro-Tejedor, M.N.; Pedraz Marcos, A.; Tejedor-Jorge, A.; Grupo Corporativo PRECAHI. Prevalencia de hiponatremia en pacientes mayores de 65 años que sufren una caída intrahospitalaria. Nefrol. Madr. 2016, 36, 292–298. [Google Scholar] [CrossRef][Green Version]
- Durán, E.R.; Camarero, G.F.R.; Martínez-Esparza, E.H. Incidence and characteristics falls in a hospital intermediate care of Barcelona. Gerokomos 2017, 28, 78–82. [Google Scholar]
- Laguna-Parras, J.M.; Arrabal-Orpez Ma, J.; Zafra-López, F.; García-Fernández, F.P.; Carrascosa-Corral, R.R.; Carrascosa-García Ma, I.; Luque-Martínez, F.M.; Alejo-Esteban, J.A. Incidencia de caídas en un hospital de nivel 1: Factores relacionados. Gerokomos 2011, 22, 167–173. [Google Scholar] [CrossRef]
- García-Hedrera, F.J.; Noguera-Quijada, C.; Sanz-Márquez, S.; Pérez-Fernández, E.; Acevedo-García, M.; Domínguez-Rincón, R.; Martínez-Simón, J.J.; González-Piñero, B.; Carmona-Monge, F.J.; Camacho-Pastor, J.L. Incidence and characteristics of falls in hospitalized patients: A cohort study. Enfermeria Clin. Engl. Ed. 2021, 31, 381–389. [Google Scholar] [CrossRef]
- Sebastián Viana, T.; García Martín, M.R.; Núñez Crespo, F.J.; Velayos Rodríguez, E.M.; Martín Merino, G.; González Ruiz, J.M.; Lema Lorenzo, I.; Nogueira Quintas, C.G. ¿Cuál es la incidencia de caídas real en un hospital? Enferm. Clínica. 2011, 21, 271–274. [Google Scholar] [CrossRef]
- Aldonza-Torres, M.; Ros Añon, M.; Torres Erice, O.; Correas Marín, M.; González Senosiain, I.; Albero Garrido, V. Incidencia de Caídas en Hospitales en España Y Estimación del Coste Sanitario. Ocronos. Vol. V. Nº 6–Junio 2022. Pág. Inicial: Vol. V; nº6: 110 Editorial Científico-Técnica. 2022. Available online: https://revistamedica.com/incidencia-caidas-coste-sanitario/ (accessed on 19 February 2023).
- Duran, E.R.; Rodriguez Camarero, G.F.; Hernandez Martinez-Esparza, E. Incidencia y características de las caídas en un hospital de cuidados intermedios de Barcelona. Gerokomos 2017, 28, 78–82. [Google Scholar]
- Observatorio de Resultados—Portal de Salud de la Comunidad de Madrid. Available online: http://observatorioresultados.sanidadmadrid.org/HospitalesFicha.aspx?ID=201 (accessed on 19 February 2023).
- Instituto Nacional de Estadística. Altas hospitalarias. Available online: https://www.ine.es/ss/Satellite?L=es_ES&c=INESeccion_C&cid=1259926692529&p=%2F&pagename=ProductosYServicios%2FPYSLayout¶m1=PYSDetalle¶m3=1259924822888 (accessed on 29 August 2023).
- Hitcho, E.B.; Krauss, M.J.; Birge, S.; Claiborne Dunagan, W.; Fischer, I.; Johnson, S.; Nast, P.A.; Costantinou, E.; Fraser, V.J. Characteristics and circumstances of falls in a hospital setting: A prospective analysis. J. Gen. Intern. Med. 2004, 19, 732–739. [Google Scholar] [CrossRef] [PubMed]
- Shaw, L.; Kiegaldie, D.; Morris, M.E. Educating health professionals to optimise falls screening in hospitals: Protocol for a mixed methods study. BMC Health Serv. Res. 2020, 20, 54. [Google Scholar] [CrossRef] [PubMed]
- Heng, H.; Jazayeri, D.; Shaw, L.; Kiegaldie, D.; Hill, A.M.; Morris, M.E. Educating hospital patients to prevent falls: Protocol for a scoping review. BMJ Open 2019, 9, e030952. [Google Scholar] [CrossRef] [PubMed]
- Heng, H.; Jazayeri, D.; Shaw, L.; Kiegaldie, D.; Hill, A.M.; Morris, M.E. Hospital falls prevention with patient education: A scoping review. BMC Geriatr. 2020, 20, 140. [Google Scholar] [CrossRef]
- Shaw, L.; Kiegaldie, D.; Farlie, M.K. Education interventions for health professionals on falls prevention in health care settings: A 10-year scoping review. BMC Geriatr. 2020, 20, 460. [Google Scholar] [CrossRef]
- Shorr, R.I.; Mion, L.C.; Chandler, A.M.; Rosenblatt, L.C.; Lynch, D.; Kessler, L.A. Improving the capture of fall events in hospitals: Combining a service for evaluating inpatient falls with an incident report system. J. Am. Geriatr. Soc. 2008, 56, 701–704. [Google Scholar] [CrossRef]
- Morris, M.E.; Iansek, R.; Kirkwood, B. A randomized controlled trial of movement strategies compared with exercise for people with Parkinson’s disease. Mov. Disord. Off. J. Mov. Disord. Soc. 2009, 24, 64–71. [Google Scholar] [CrossRef]
- Morris, M.E.; Ellis, T.D.; Jazayeri, D.; Heng, H.; Thomson, A.; Balasundaram, A.P.; Slade, S.C. Boxing for Parkinson’s Disease: Has Implementation Accelerated Beyond Current Evidence? Front. Neurol. 2019, 10, 1222. [Google Scholar] [CrossRef] [PubMed]
- Vass, C.; Edwards, C.; Smith, A.; Sahota, O.; Drummond, A. What do patients wear on their feet? A service evaluation of footwear in elderly patients. Int. J. Ther. Rehabil. 2015, 22, 225–232. [Google Scholar] [CrossRef]
- Sherrington, C.; Menz, H.B. An evaluation of footwear worn at the time of fall-related hip fracture. Age Ageing 2003, 32, 310–314. [Google Scholar] [CrossRef]
- Stoeckle, A.; Iseler, J.I.; Havey, R.; Aebersold, C. Catching Quality Before It Falls: Preventing Falls and Injuries in the Adult Emergency Department. J. Emerg. Nurs. 2019, 45, 257–264. [Google Scholar] [CrossRef] [PubMed]
- McCarty, C.A.; Harry, M.L.; Woehrle, T.A.; Kitch, L.A. Screening and falls in community hospital emergency rooms in the 12 months following implementation of MEDFRAT. Am. J. Emerg. Med. 2020, 38, 1686–1687. [Google Scholar] [CrossRef]
- Hartung, B.; Lalonde, M. The use of non-slip socks to prevent falls among hospitalized older adults: A literature review. Geriatr. Nurs. 2017, 38, 412–416. [Google Scholar] [CrossRef]
- Chari, S.; Haines, T.; Varghese, P.; Economidis, A. Are non-slip socks really «non-slip»? An analysis of slip resistance. BMC Geriatr. 2009, 9, 39. [Google Scholar] [CrossRef][Green Version]
- Tzeng, H.M.; Yin, C.Y. Frequently observed risk factors for fall-related injuries and effective preventive interventions: A multihospital survey of nurses’ perceptions. J. Nurs. Care Qual. 2013, 28, 130–138. [Google Scholar] [CrossRef]
- Kelsey, J.L.; Procter-Gray, E.; Nguyen, U.S.D.T.; Li, W.; Kiel, D.P.; Hannan, M.T. Footwear and Falls in the Home Among Older Individuals in the MOBILIZE Boston Study. Footwear Sci. 2010, 2, 123–129. [Google Scholar] [CrossRef]
- Hatton, A.L.; Sturnieks, D.L.; Lord, S.R.; Lo, J.C.M.; Menz, H.B.; Menant, J.C. Effects of nonslip socks on the gait patterns of older people when walking on a slippery surface. J. Am. Podiatr. Med. Assoc. 2013, 103, 471–479. [Google Scholar] [CrossRef]
- Hübscher, M.; Thiel, C.; Schmidt, J.; Bach, M.; Banzer, W.; Vogt, L. Slip resistance of non-slip socks—An accelerometer-based approach. Gait Posture 2011, 33, 740–742. [Google Scholar] [CrossRef] [PubMed]
- Pelliard, T.; Brika, M.; Rulleau, T. Prévention des chutes chez les personnes âgées fragiles hospitalisées en court séjour: Utilisation des chaussettes antidérapantes. Une Rev. Systématique Littérature Rech Soins Infirm. 2021, 146, 60–73. [Google Scholar]
- Jazayeri, D.; Heng, H.; Slade, S.C.; Seymour, B.; Lui, R.; Volpe, D.; Jones, C.; Morris, M.E. Benefits and risks of non-slip socks in hospitals: A rapid review. Int. J. Qual. Health Care 2021, 33, mzab057. [Google Scholar] [CrossRef] [PubMed]
- Meddaugh, D.I.; Friedenberg, D.L.; Knisley, R. Special socks for special people: Falls in special care units. Geriatr. Nur. 1996, 17, 24–26. [Google Scholar] [CrossRef] [PubMed]
- Song, Q.; Zhang, X.; Mao, M.; Sun, W.; Zhang, C.; Chen, Y.; Li, L. Relationship of proprioception, cutaneous sensitivity, and muscle strength with the balance control among older adults. J. Sport. Health Sci. 2021, 10, 585–593. [Google Scholar] [CrossRef] [PubMed]
- Pasquetti, P.; Apicella, L.; Mangone, G. Pathogenesis, and treatment of falls in elderly. Clin. Cases Miner. Bone Metab. 2014, 11, 222–225. [Google Scholar] [CrossRef]
- Rubenstein, L.Z. Falls in older people: Epidemiology, risk factors and strategies for prevention. Age Ageing 2006, 35, 37–41. [Google Scholar] [CrossRef]
- Richardson, J.A.; Goldsmith, C.H.; Clase, C.M. Muscle weakness and falls in older adults: A systematic review and meta-analysis. J. Am. Geriatr. Soc. 2004, 52, 1121–1129. [Google Scholar]
- Stalenhoef, P.A.; Diederiks, J.P.; Knottnerus, J.A.; de Witte, L.P.; Crebolder, H.F. The construction of a patient record-based risk model for recurrent falls among elderly people living in the community. Fam. Pract. 2000, 17, 490–496. [Google Scholar] [CrossRef]
- Myers, A.H.; Baker, S.P.; Van Natta, M.L.; Abbey, H.; Robinson, E.G. Risk factors associated with falls and injuries among elderly institutionalized persons. Am. J. Epidemiol. 1991, 133, 1179–1190. [Google Scholar] [CrossRef]
- Kiely, D.K.; Kiel, D.P.; Burrows, A.B.; Lipsitz, L.A. Identifying nursing home residents at risk for falling. J. Am. Geriatr. Soc. 1998, 46, 551–555. [Google Scholar] [CrossRef] [PubMed]
- Landi, F.; Onder, G.; Cesari, M.; Barillaro, C.; Russo, A.; Bernabei, R. Psychotropic medications, and risk for falls among community-dwelling frail older people: An observational study. J. Gerontol. 2005, 60, 622–626. [Google Scholar] [CrossRef] [PubMed]


| Non-Slip Socks | Adequate Footwear | p | |
|---|---|---|---|
| Gender (N) | |||
| Women | 32 | 42 | p < 0.109 |
| Men | 45 | 37 | |
| Age (Mean ± STD) | 76.39 ± 17.55 | 84.45 ± 10.75 | p < 0.001 |
| Treatments (N) | |||
| Psychotropic drugs | |||
| NO | 33 | 24 | p < 0.736 |
| YES | 49 | 36 | |
| Antihypertensives | |||
| NO | 28 | 27 | p < 0.689 |
| YES | 49 | 54 | |
| Anticoagulants | |||
| NO | 74 | 3 | p < 0.341 |
| YES | 3 | 6 | |
| >5 drugs | |||
| NO | 50 | 47 | p < 0.373 |
| YES | 27 | 34 | |
| Visual impairment (N) | |||
| NO | 57 | 55 | p < 0.475 |
| YES | 20 | 25 | |
| Hearing disturbances (N) | |||
| NO | 60 | 17 | p < 0.327 |
| YES | 56 | 24 | |
| Low extremities disabilities (N) | |||
| NO | 61 | 62 | p < 0.502 |
| Paralysis | 15 | 19 | |
| Paresthesia | 1 | 0 | |
| Mental status (N) | |||
| Confusion | 12 | 4 | p < 0.027 |
| Conscious and oriented | 65 | 77 | |
| Risk of falls (N) | |||
| High | 62 | 66 | p < 0.876 |
| Mild/Moderate | 12 | 13 | |
| No risk | 3 | 2 |
| N | Category | Frequency (N) | Frequency (%) | |
|---|---|---|---|---|
| Psychotropic drugs | 21 | NO | 14 | 66.67 |
| YES | 7 | 33.33 | ||
| Antihypertensives | 21 | NO | 15 | 71.43 |
| YES | 6 | 28.57 | ||
| Anticoagulants | 21 | NO | 16 | 76.19 |
| YES | 5 | 23.81 | ||
| >5 drugs | 21 | NO | 8 | 38.01 |
| YES | 13 | 61.90 | ||
| Other drugs | 21 | NO | 17 | 80.95 |
| YES | 4 | 19.05 | ||
| Visual impairment | 21 | NO | 12 | 57.14 |
| YES | 8 | 38.10 | ||
| UNKNOWN | 1 | 4.76 | ||
| Hearing disturbances | 21 | UNKNOWN | 1 | 4.76 |
| NO | 10 | 47.62 | ||
| YES | 10 | 47.62 | ||
| Lower-extremities disabilities | 21 | NO | 10 | 47.62 |
| YES | 11 | 52.38 | ||
| Mental status | 21 | Confusion | ||
| Conscious and oriented | 21 | 100.00 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moreno Rodríguez, R.M.; Solas Gómez, B.; Gallego Marcuello, L.; Diaz Martinez, M.d.C.; Fernández del Palacio, E.; Santiago-Sáez, A. Observational Prospective Study to Determine the Efficacy of ‘Non-Slip Socks’ vs. ‘Adequate Footwear’ Regarding the Number of Falls Observed among Admitted Patients. Healthcare 2023, 11, 2605. https://doi.org/10.3390/healthcare11192605
Moreno Rodríguez RM, Solas Gómez B, Gallego Marcuello L, Diaz Martinez MdC, Fernández del Palacio E, Santiago-Sáez A. Observational Prospective Study to Determine the Efficacy of ‘Non-Slip Socks’ vs. ‘Adequate Footwear’ Regarding the Number of Falls Observed among Admitted Patients. Healthcare. 2023; 11(19):2605. https://doi.org/10.3390/healthcare11192605
Chicago/Turabian StyleMoreno Rodríguez, Rosa M., Beatriz Solas Gómez, Laura Gallego Marcuello, Maria del Carmen Diaz Martinez, Encarnacion Fernández del Palacio, and Andrés Santiago-Sáez. 2023. "Observational Prospective Study to Determine the Efficacy of ‘Non-Slip Socks’ vs. ‘Adequate Footwear’ Regarding the Number of Falls Observed among Admitted Patients" Healthcare 11, no. 19: 2605. https://doi.org/10.3390/healthcare11192605
APA StyleMoreno Rodríguez, R. M., Solas Gómez, B., Gallego Marcuello, L., Diaz Martinez, M. d. C., Fernández del Palacio, E., & Santiago-Sáez, A. (2023). Observational Prospective Study to Determine the Efficacy of ‘Non-Slip Socks’ vs. ‘Adequate Footwear’ Regarding the Number of Falls Observed among Admitted Patients. Healthcare, 11(19), 2605. https://doi.org/10.3390/healthcare11192605





