Acupotomy in Korean Medicine Doctors: A Preliminary Survey on Experiences, Perceptions, and Clinical Usage Status
Abstract
1. Introduction
2. Methodology
2.1. Institutional Review Board Approval and Participant Consent
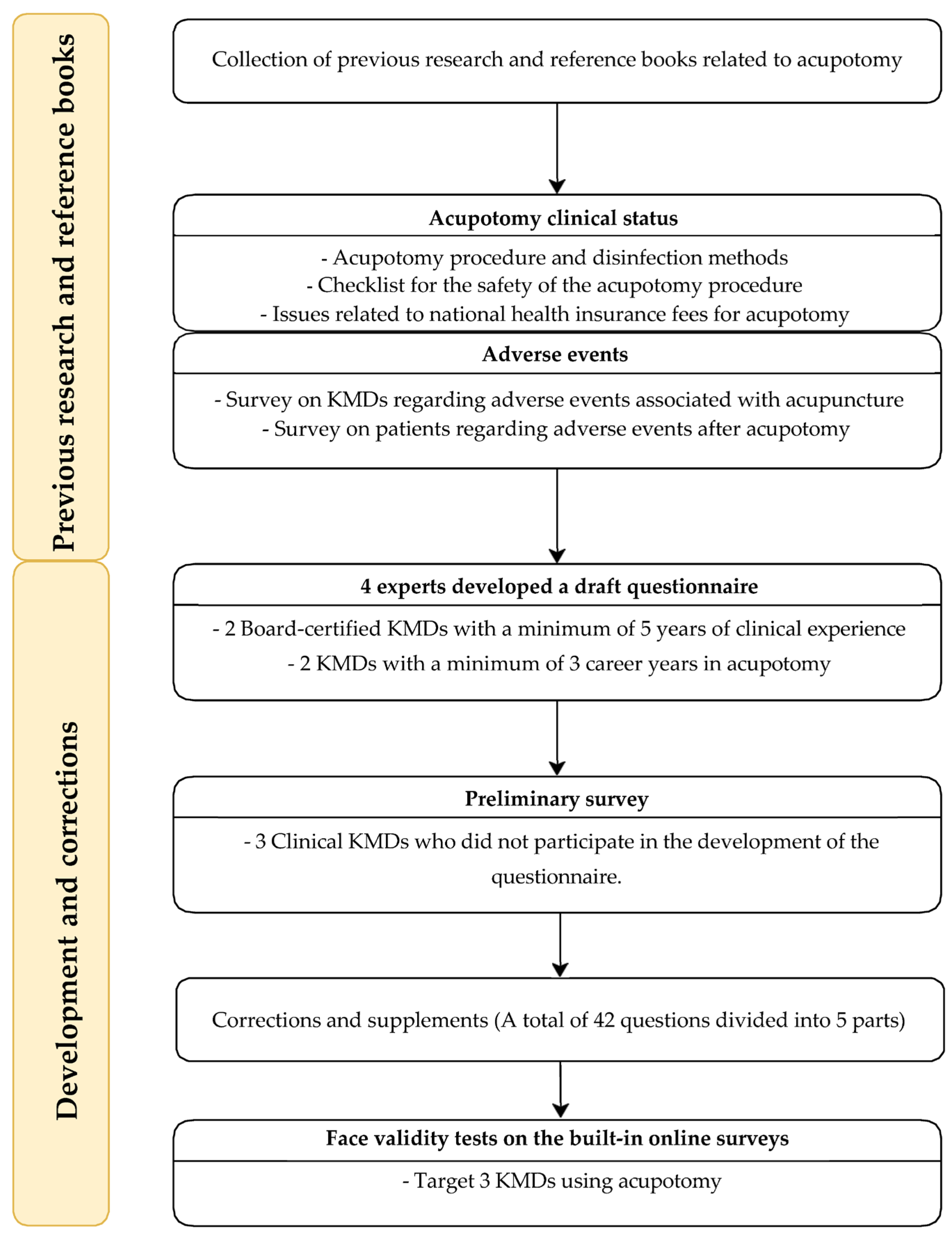
2.2. Development of the Questionnaire
2.3. Items of the Online Survey
- (1)
- Clinical usage status of acupotomy treatment (Q1–15);
- (2)
- Perception of the clinical applicability of the “pre- and post-acupotomy procedure safety checklist” guidelines (Q16–20);
- (3)
- Perceptions about the workload and appropriate price for the acupotomy (Q21–25);
- (4)
- Observed acupotomy-related adverse events and serious adverse events (Q26–33);
- (5)
- Demographic information and other collected data (Q34–42);
2.4. Participants and Survey Administration
2.5. Statistical Analysis Methods
3. Results
3.1. Demographic Analysis
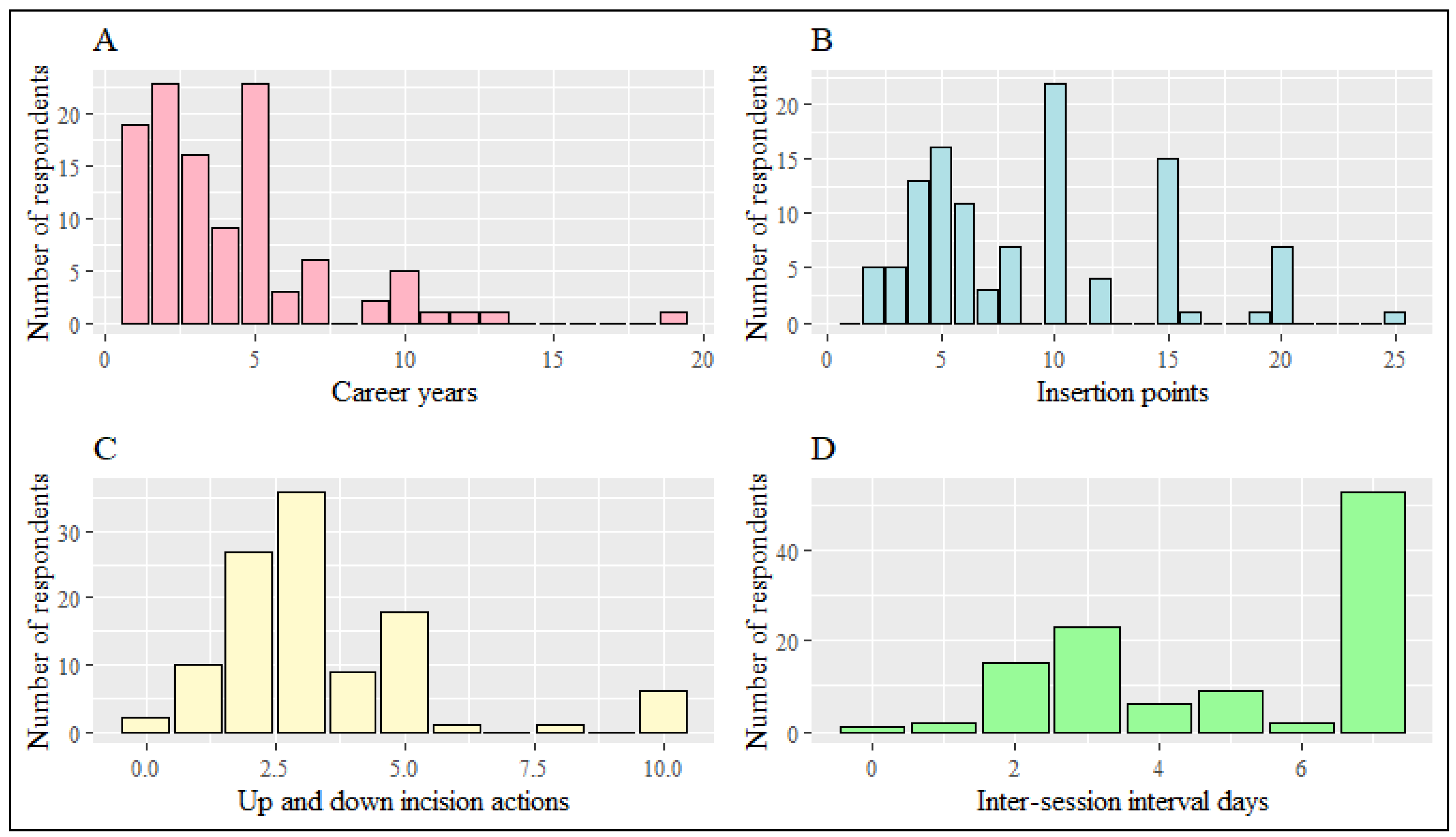
3.2. Clinical Usage Status of Acupotomy
3.3. Differences in Acupotomy Practice between Beginners and Experienced Practitioners
3.4. Perceptions of the Safety Checklists and Health Insurance Coverage of Acupotomy
3.5. Adverse Events and Serious Adverse Events
3.6. Requirements of Clinicians for Safe Procedures
4. Discussion
4.1. Summary of Findings
4.2. Debate
4.3. Demands and Contributions for Developing Procedural Guidelines and Appropriate Insurance Coverage
4.4. Strengths, Limitations, and Considerations for Further Study
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sohn, I.-C.; Kwon, O.-S.; Kim, Y.-L.; Ahn, S.-H.; Kim, J.-H. Literature Study on the Conformation and Application of Nine Classical Needles. Korean J. Acupunct. 2011, 28, 157–169. [Google Scholar]
- Yoon, S.; Kwon, C.; Leem, J. Adverse Events of Miniscalpel-Needle Treatment in Korea: A Systematic Review. Eur. J. Integr. Med. 2019, 27, 7–17. [Google Scholar] [CrossRef]
- Guo, C.; Liu, N.; Li, X.; Sun, H.; Hu, B.; Lu, J.; Gao, Y.; Liang, C.; Xu, H.; Wu, H. Effect of Acupotomy on Nitric Oxide Synthase and Beta-Endorphin in Third Lumbar Vertebrae Transverse Process Syndrome Model Rats. J. Tradit. Chin. Med. 2014, 34, 194–198. [Google Scholar] [CrossRef] [PubMed]
- Yuk, D.I.; Kim, K.M.; Jeon, J.H.; Kim, Y.I.; Kim, J.H. A Review of Trends for Acupotomy. J. Acupunct. Res. 2014, 31, 35–43. [Google Scholar] [CrossRef]
- Qu, B.; Wu, X.; Liu, H.; Cai, W.; Wang, G.; Song, H.; Wang, F. Meta-Analysis and Systematic Review of Acupotomy Combined with Puncture and Moxibustion in the Treatment of Knee Osteoarthritis. Ann. Palliat. Med. 2021, 10, 6637–6649. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.; Kim, S.Y.; Kim, H.S.; Jeong, J.K.; Jung, S.Y.; Han, C.H.; Kim, Y.I. Effectiveness and Safety of Acupotomy for Lumbar Disc Herniation: A Study Protocol for a Randomized, Assessor-Blinded, Controlled Pilot Trial. Integr. Med. Res. 2017, 6, 310–316. [Google Scholar] [CrossRef] [PubMed]
- Hong, H.-W.; Jeong, M.-I.; Jo, H.-I.; Lee, S.-H.; Kim, K.-H.; Choi, S.-W.; Park, J.-W.; Ha, J.-S. Effectiveness of Acupuncture and Acupotomy for Trigger Finger: A Systematic Review and Meta-Analysis. J. Acupunct. Res. 2023, 40, 111–128. [Google Scholar] [CrossRef]
- Jung, H.S.; Jeong, T.S.; Kim, S.C.; Jeong, Y.J.; Kim, S.H.; Lim, J. Effects of Ultrasound-Guided Acupotomy Therapy on a Trigger Finger: A Case Report. J. Acupunct. Res. 2023, 40, 162–166. [Google Scholar] [CrossRef]
- Min, B.K.; Jin, J.S.; Lee, D.E.; Shin, W.B.; Shin, J.H.; Youn, I.A. The Effect of Complex Korean Medical Treatment with Acupotomy on Irritable Bowel Syndrome: A Case Report. J. Acupunct. Res. 2020, 37, 59–63. [Google Scholar] [CrossRef]
- Min, D.L.; Lee, Y.H.; Go, N.G. A Clinical Report on Facial Atrophic Scars Treatment with Acupotomy. J. Korean Med. 2015, 36, 144–153. [Google Scholar] [CrossRef][Green Version]
- Oh, S.J.; Park, M.S.; Lee, J.H.; Jun, S.A.; Gong, H.M.; Choi, S.H.; Hwangbo, M.; Lee, H.J.; Kim, J.S. Problems and Potential Improvements of National Health Insurance Fees Associated with Miniscalpel Acupuncture. J. Acupunct. Res. 2016, 33, 67–73. [Google Scholar] [CrossRef]
- Jo, H.-G.; Song, M.-Y.; Yoon, S.-H.; Jeong, S.-Y.; Kim, J.-H.; Baek, E.-H.; Leem, J. Proposal of Checklists for Patient Safety in Miniscalpel Acupuncture Treatment of Cervical and Lumbar Spine: Pilot Trial. J. Korean Med. Rehabil. 2018, 28, 61–72. [Google Scholar] [CrossRef][Green Version]
- Cho, K.H.; Ki, W.; Yuk, D.I.; Sung, I.S.; Kim, M.J.; Hong, K.E. Literature Study on the Infection Control of Dochim. J. Korean Acupunct. Moxibustion Soc. 2013, 30, 181–187. [Google Scholar] [CrossRef]
- Hou, H.-K.; Liu, C.-Z.; Lin, L.-L. Magnetic Resonance Imaging Study of Safe Needling Depth and Angulation for Acupuncture at BL40. Acupunct. Med. 2021, 39, 343–350. [Google Scholar] [CrossRef] [PubMed]
- Pu, J.; Cao, W.; Chen, Y.; Fan, Y.; Cao, Y. Ultrasound-Guided Injection Acupotomy as a Minimally Invasive Intervention Therapy for Cervical Spondylotic Radiculopathy: A Randomized Control Trial. Ann. Med. 2023, 55, 2233556. [Google Scholar] [CrossRef] [PubMed]
- Yoon, S.-H.; Lee, H.; Kwon, C.-Y.; Jeon, D.; Kim, H.; Jo, H.-G.; Shin, A.; Yun, Y.; Sul, J.-U.; Lee, G.-M.; et al. Development of a Survey Form through Delphi Study about Adverse Events Associated with the Miniscalpel Needle, for Application in Prospective Observational Studies Regarding Safety of Miniscalpel Needles: Study Protocol. Medicine 2018, 97, e12736. [Google Scholar] [CrossRef] [PubMed]
- Yoon, S.-H.; Kwon, C.-Y.; Jo, H.-G.; Sul, J.-U.; Lee, H.; Won, J.; Jeong, S.J.; Lee, J.-H.; Leem, J. Safety of Acupotomy in a Real-World Setting: A Prospective Pilot and Feasibility Study. J. Integr. Med. 2022, 20, 514–523. [Google Scholar] [CrossRef]
- Kim, Y.-H.; Lee, W.-H.; Chang, H.-J.; Lim, S. A Study on the Problem about Oriental Treatment Fee Based on Valuation of Resources. J. Korean Orient. Med. 2008, 29, 15–24. [Google Scholar]
- Balayla, J.; Tulandi, T. Survey Research. J. Obs. Gynaecol. Can. 2019, 41, 901–902. [Google Scholar] [CrossRef] [PubMed]
- Gordon, J.S.; McNew, R. Developing the Online Survey. Nurs. Clin. N. Am. 2008, 43, 605–619. [Google Scholar] [CrossRef] [PubMed]
- Jung, S.; Woo, J.; Chae, H.; Oh, K.; Choi, S.; Lee, J.; Kang, K.; Chu, H.; Ryu, M. A Survey on the Complications Associated with Acupotomy in a Single Korean Medicine Clinic. Korean J. Acupunct. 2020, 37, 253–261. [Google Scholar] [CrossRef]
- Korean Acupuncture & Moxibustion Society Textbook Compilation Committee. The Acupuncture & Moxibustion Medicine; Jipmoondang: Seoul, Republic of Korea, 2014. [Google Scholar]
- Suh, C.Y.; Lee, Y.J.; Kim, M.; Bae, Y.H.; Kim, H.S.; Kim, N.H.; Yang, K.J.; Lee, G.B.; Ha, I.H. A Web-Based Survey for Assessment of Korean Medical Treatment Clinical Practice Patterns for Neck Pain and Cervical Intervertebral Disc Displacement. J. Acupunct. Res. 2016, 33, 65–72. [Google Scholar] [CrossRef]
- Bae, K.H.; Lee, Y.; Park, K.H.; Yoon, Y.; Mun, S.; Lee, S. Perception of Cold and Heat Pattern Identification in Diseases: A Survey of Korean Medicine Doctors. Integr. Med. Res. 2017, 6, 26–32. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.-E.; Do, H.-J.; Song, H.-S.; Shin, J.-K.; Lee, W.-J.; Kim, J.-H.; Lee, K.-J.; Yoon, Y.-S.; Kim, N.-H.; Suh, C.-Y.; et al. A Web-Based Survey for Assessment of Korean Medical Treatment Clinical Practice Patterns for Temporomandibular Disorders. J. Korean Med. Rehabil. 2018, 28, 73–84. [Google Scholar] [CrossRef]
- Lee, J.-E.; Choi, J.-B.; Kim, D.-H.; Jeong, H.-J.; Kim, J.-H. A Web-Based Survey Research on Improving and Utilizing Korean Medicine Clinical Practice Guideline for Ankle Sprain. J. Korean Med. 2019, 40, 1–16. [Google Scholar] [CrossRef]
- Wang, Y.-H.; Zhou, Y.; Xie, Y.-Z.; Fan, X.-H.; Liang, W.-Q.; Wei, X.; Zhao, M.-D.; Huo, Y.-X.; Zhang, T.; Yin, Y. The Effect of Ultrasound-Guided Acupotomy and Juanbi Decoction on Lumbar Disc Herniation: A Randomized Controlled Trial. Medicine 2023, 102, e32622. [Google Scholar] [CrossRef]
- Lee, C.-J.; Luo, W.-T.; Tam, K.-W.; Huang, T.-W. Comparison of the Effects of Acupotomy and Acupuncture on Knee Osteoarthritis: A Systematic Review and Meta-Analysis. Complement. Ther. Clin. Pract. 2023, 50, 101712. [Google Scholar] [CrossRef] [PubMed]
- Li, D.; Wang, X.; Fang, T.; Chen, Y.; Xiang, S.; Qi, J.; Liang, C.; Ren, C.; Zhao, X.; Qiu, Z.; et al. Acupotomy in the Treatment of Tenosynovitis of Hand Flexor Tendons: A Systematic Review and Meta-Analysis. Medicine 2022, 101, e31504. [Google Scholar] [CrossRef]
- Lin, S.; Lai, C.; Wang, J.; Lin, Y.; Tu, Y.; Yang, Y.; Zhang, R. Efficacy of Ultrasound-Guided Acupotomy for Knee Osteoarthritis: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Medicine 2023, 102, e32663. [Google Scholar] [CrossRef]
- Baumler, P.; Zhang, W.; Stubinger, T.; Irnich, D. Acupuncture-Related Adverse Events: Systematic Review and Meta-Analyses of Prospective Clinical Studies. BMJ Open 2021, 11, e045961. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.C. Clinical Characteristics of Poor Responders to Acupotomy and Safety Pretreatment Management. J. Acupunct. Res. 2008, 25, 117–125. [Google Scholar]
- Endres, H.G.; Molsberger, A.; Lungenhausen, M.; Trampisch, H.J. An Internal Standard for Verifying the Accuracy of Serious Adverse Event Reporting: The Example of an Acupuncture Study of 190,924 Patients. Eur. J. Med. Res. 2004, 9, 545–551. [Google Scholar] [PubMed]
- White, A.; Hayhoe, S.; Hart, A.; Ernst, E.; BMAS; AACP. Survey of Adverse Events Following Acupuncture (SAFA): A Prospective Study of 32,000 Consultations. Acupunct. Med. 2001, 19, 84–92. [Google Scholar] [CrossRef] [PubMed]
- Jiang, L.; Zhang, B.; Yu, H. Analysis on adverse event in acupotomy therapy based on literature research. Zhongguo Zhen Jiu 2018, 38, 1007–1012. [Google Scholar] [CrossRef] [PubMed]
- Park, S.-U.; Ko, C.-N.; Bae, H.-S.; Jung, W.-S.; Moon, S.-K.; Cho, K.-H.; Kim, Y.-S.; Park, J.-M. Short-Term Reactions to Acupuncture Treatment and Adverse Events Following Acupuncture: A Cross-Sectional Survey of Patient Reports in Korea. J. Altern. Complement. Med. 2009, 15, 1275–1283. [Google Scholar] [CrossRef] [PubMed]
- Zhou, J.; Zhao, F.-Y.; Li, W.-H.; Yi, P.; Yang, F.; Tang, X.-S.; Li, H.; Tan, M.-S. Safety depth of acupuncture at Yamen (GV 15) in patients with atlantoaxial dislocation. Zhongguo Zhen Jiu 2019, 39, 619–622. [Google Scholar] [CrossRef] [PubMed]
| Characteristics (Answered = 109) | n (%) | |
|---|---|---|
| Gender | Men | 82 (75.2) |
| Women | 27 (24.8) | |
| Age (years) | 20–29 s | 22 (20.2) |
| 30–39 s | 47 (43.1) | |
| 40–49 s | 21 (19.3) | |
| 50–59 s | 16 (14.7) | |
| 60–69 s | 3 (2.7) | |
| Clinical experience (years) | ≤5 | 46 (42.2) |
| 6–10 | 22 (20.2) | |
| 11–20 | 25 (22.9) | |
| 21–30 | 8 (7.3) | |
| 31≤ | 8 (7.3) | |
| Healthcare facility level | General clinic or KM clinic | 80 (73.4) |
| General or KM hospital | 19 (17.4) | |
| Public health center | 10 (9.2) | |
| Board-certified KM doctors | General practitioner | 90 (82.6) |
| Current training (internship or residency) | 8 (7.3) | |
| Specialist for acupuncture and moxibustion medicine | 4 (3.7) | |
| Specialist for rehabilitation medicine of KM | 4 (3.7) | |
| Specialist for internal medicine of KM | 2 (1.8) | |
| Specialist for ophthalmology, otorhinolaryngology, and dermatology of KM | 1 (0.9) | |
| Healthcare facility place * | Urban | 97 (89) |
| Rural | 12 (11) |
| Question Number | Treatment Sites | n (%) | |
|---|---|---|---|
| Q3 | Treatment sites * | 109 (100) | |
| Lumbar and pelvis | 107 (98.2) | ||
| Head and neck | 98 (89.9) | ||
| Upper extremities | 58 (53.2) | ||
| Lower extremities | 45 (41.3) | ||
| Back | 27 (24.8) | ||
| Abdomen | 12 (11) | ||
| Face | 10 (9.2) | ||
| Chest | 10 (9.2) | ||
| Q4 | Indications for acupotomy (KCD code) * | 107 (100) † | |
| Head and neck | Headache R51 | 31 (29) | |
| Cervicalgia, cervical region M5422 | 30 (28) | ||
| Cervical disc disorders with cervicalgia M50 | 29 (27.1) | ||
| Spinal stenosis, cervical region M4802 | 3 (2.8) | ||
| Face | Bell’s palsy G510 | 1 (0.9) | |
| Back | Pain in thoracic spine M546 | 5 (4.7) | |
| Lumbar and pelvis | Low back pain, lumbosacral region M5457 | 37 (34.6) | |
| Thoracic, thoracolumbar, and lumbosacral disc disorders M51 | 35 (32.7) | ||
| Spinal stenosis, lumbosacral region M4807 | 23 (21.5) | ||
| Lumbago with sciatica, lumbosacral region M5447 | 11 (10.3) | ||
| Degeneration of facet joints M47 | 9 (8.4) | ||
| Other myalgia, sacroiliac joint M79158 | 3 (2.8) | ||
| Chest | Thoracic outlet syndrome G540 | 2 (1.9) | |
| Abdomen | Indigestion K30 | 2 (1.9) | |
| Upper extremities | Other myalgia, shoulder region M79118 | 19 (17.8) | |
| Adhesive capsulitis of shoulder M750 | 9 (8.4) | ||
| Tennis elbow M771 | 8 (7.5) | ||
| Neuralgia and neuritis, unspecified, forearm M7923 | 7 (6.5) | ||
| Rotator cuff syndrome M751 | 5 (4.7) | ||
| Trigger finger M653 | 4 (3.7) | ||
| Lower extremities | Neuralgia and neuritis, unspecified, lower leg M7926 | 10 (9.3) | |
| Other myalgia, lower leg M79168 | 6 (5.6) | ||
| Gonarthrosis [arthrosis of knee] M17 | 5 (4.7) | ||
| Other internal derangements of knee M238 | 2 (1.9) | ||
| Plantar fasciitis M722 | 2 (1.9) | ||
| Morton’s metatarsalgia G576 | 1 (0.9) | ||
| Question Number | Features | n (%) | Mean ± SD | |
|---|---|---|---|---|
| Q1 | Career of acupotomy practice (years) | 4.06 ± 3.05 | ||
| Q2 | Blade width (diameter, mm) * | 110 (100) | ||
| 0.35 | 11 (10) | |||
| 0.4 | 97 (88.2) | |||
| 0.5 | 95 (86.3) | |||
| 0.6 | 50 (45.5) | |||
| 0.75 | 12 (10.9) | |||
| 0.8 | 8 (7.3) | |||
| 1 | 8 (7.3) | |||
| 1.2 | 8 (7.3) | |||
| Q5 | Depth of insertion | 110 (100) | ||
| Muscle | 60 (54.5) | |||
| Periosteum | 43 (30.1) | |||
| Dermis | 7 (6.4) | |||
| Q6 | Number of insertion points per session | 8.95 ± 5.08 | ||
| Q7 | Number of up and down incision actions per point | 3.38 ± 2.11 | ||
| Q8 | Recommended inter-session interval for patients (days) | 4.98 ± 2.14 | ||
| Q9 | The average number of acupotomy sessions in one week | 110 (100) | ||
| 1–5 | 32 (28.8) | |||
| 6–10 | 18 (16.2) | |||
| 11–20 | 21 (18.9) | |||
| 21–30 | 16 (14.4) | |||
| 31–40 | 6 (5.4) | |||
| 41–50 | 9 (8.1) | |||
| 60 | 3 (2.7) | |||
| 80 | 2 (1.8) | |||
| 120 | 1 (0.9) | |||
| 150 | 1 (0.9) | |||
| 350 | 1 (0.9) | |||
| 500 | 1 (0.9) | |||
| Question Number | AEs and SAEs | n (%) | |
|---|---|---|---|
| Q26 | Local AEs * | 110 (100) | |
| Bruise | 85 (77.3) | ||
| Pain | 57 (51.8) | ||
| Hematoma | 57 (51.8) | ||
| Bleeding | 44 (40) | ||
| Neurological symptoms | 17 (15.5) | ||
| Local infections | 4 (3.6) | ||
| None | 2 (1.8) | ||
| Cerebrospinal fluid leakage | 1 (0.9) | ||
| Blister | 0 (0) | ||
| Organ damage | 0 (0) | ||
| Pneumothorax | 0 (0) | ||
| Q27 | Systemic AEs * | 111 (100) | |
| Fatigue | 65 (57.7) | ||
| Autonomic nervous system dysfunctions (headache, nausea, dizziness, needle sickness, etc.) | 34 (30.6) | ||
| None | 34 (30.6) | ||
| Psychiatric disorder (anxiety, impatient, etc.) | 0 (0) | ||
| Systemic infection | 0 (0) | ||
| Q28 | Main factors for the occurrence of AEs * | 111 (100) | |
| Insufficient identification of anatomically safe procedure zones | 26 (23.4) | ||
| Incorrect needling depth | 19 (17.1) | ||
| Improper insertion point selection | 15 (13.5) | ||
| Excessive number of up and down incision actions | 14 (12.6) | ||
| Misconduct in the selection of blade width | 14 (12.6) | ||
| Wrong blade direction | 11 (9.9) | ||
| Misconduct of needling speed | 9 (8.1) | ||
| Negligence in the contraindication for acupotomy | 8 (7.2) | ||
| Negligence in the disinfection and patient education (preventing infection, pain control) after acupotomy | 6 (5.4) | ||
| Q29 | Experience of SAEs | 110 (100) | |
| No | 108 (98.2) | ||
| Yes | 2 (1.8) | ||
| Q30 | SAEs * | 2 (100) | |
| Central, peripheral nervous system damage | 1 (50) | ||
| Local infections | 1 (50) | ||
| Q31 | Main factors for the occurrence of SAEs * | 2 (100) | |
| Insufficient identification of anatomically safe procedure zones | 1 (50) | ||
| Improper insertion point selection | 1 (50) | ||
| Negligence in the disinfection and patient education (preventing infection, pain control) after acupotomy | 1 (50) | ||
| Q32 | Consequences of SAEs * | 2 (100) | |
| Complete recovery | 1 (50) | ||
| Recovering | 1 (50) | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jun, H.; Yoon, S.-H.; Ryu, M.; Chae, H.; Chu, H.; Leem, J.; Kim, T.-H. Acupotomy in Korean Medicine Doctors: A Preliminary Survey on Experiences, Perceptions, and Clinical Usage Status. Healthcare 2023, 11, 2577. https://doi.org/10.3390/healthcare11182577
Jun H, Yoon S-H, Ryu M, Chae H, Chu H, Leem J, Kim T-H. Acupotomy in Korean Medicine Doctors: A Preliminary Survey on Experiences, Perceptions, and Clinical Usage Status. Healthcare. 2023; 11(18):2577. https://doi.org/10.3390/healthcare11182577
Chicago/Turabian StyleJun, Hyungsun, Sang-Hoon Yoon, Myungseok Ryu, Hyocheong Chae, Hongmin Chu, Jungtae Leem, and Tae-Hun Kim. 2023. "Acupotomy in Korean Medicine Doctors: A Preliminary Survey on Experiences, Perceptions, and Clinical Usage Status" Healthcare 11, no. 18: 2577. https://doi.org/10.3390/healthcare11182577
APA StyleJun, H., Yoon, S.-H., Ryu, M., Chae, H., Chu, H., Leem, J., & Kim, T.-H. (2023). Acupotomy in Korean Medicine Doctors: A Preliminary Survey on Experiences, Perceptions, and Clinical Usage Status. Healthcare, 11(18), 2577. https://doi.org/10.3390/healthcare11182577





