Sleep Quality and Its Affecting Factors among Hemodialysis Patients: A Multicenter Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Research Design
2.2. Setting
2.3. Sample
2.4. Data Collection Tools
2.5. Ethical Considerations
2.6. Data Analysis
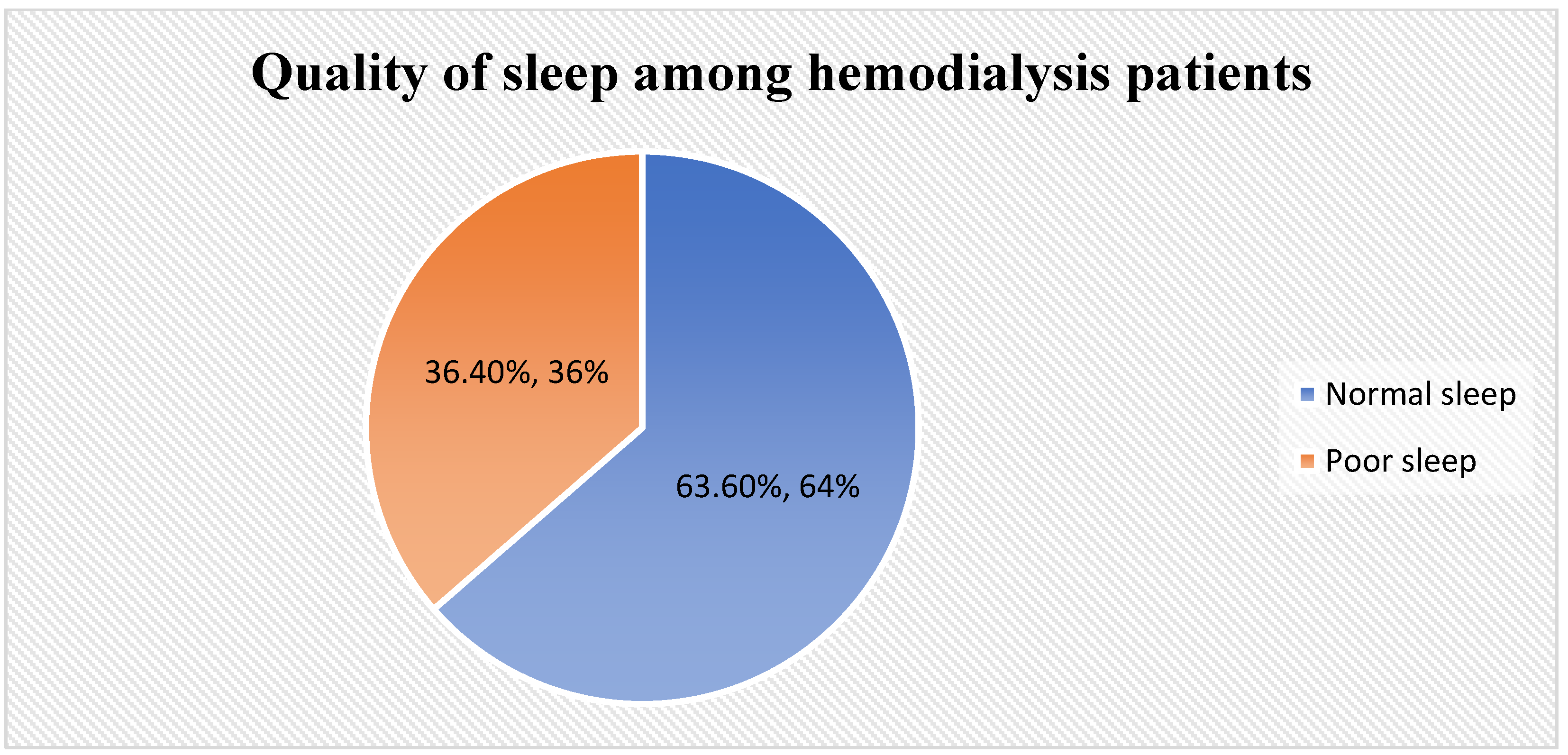
3. Results
4. Discussion
5. Implication to Nursing Practice
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ansari, M.; Al-Adeem, M.; Alshakka, M. Comorbidity among Patients with Kidney Diseases in Hail Region, Saudi Arabia. Int. J. Diabetes Clin. Res. 2019, 6, 104. [Google Scholar] [CrossRef]
- Kovesdy, C.P. Epidemiology of chronic kidney disease: An update 2022. Kidney Int. Suppl. 2022, 12, 7–11. [Google Scholar] [CrossRef]
- Chen, T.K.; Knicely, D.H.; Grams, M.E. Chronic Kidney Disease Diagnosis and Management: A Review. JAMA 2019, 322, 1294–1304. [Google Scholar] [CrossRef]
- Alshammari, B.; Noble, H.; McAneney, H.; O’Halloran, P. An exploration of symptom burden and its management, in Saudi Arabian patients receiving haemodialysis, and their caregivers: A mixed methods study protocol. BMC Nephrol. 2019, 20, 250. [Google Scholar] [CrossRef]
- Abecassis, M.; Bartlett, S.T.; Collins, A.J.; Davis, C.L.; Delmonico, F.L.; Friedewald, J.J.; Hays, R.; Howard, A.; Jones, E.; Leichtman, A.B.; et al. Kidney transplantation as primary therapy for end-stage renal disease: A National Kidney Foundation/Kidney Disease Outcomes Quality Initiative (NKF/KDOQITM) conference. Clin. J. Am. Soc. Nephrol. 2008, 3, 471–480. [Google Scholar] [CrossRef]
- Mousa, D.; Alharbi, A.; Helal, I.; Al-Homrany, M.; Alhujaili, F.; Alhweish, A.; Marie, M.A.; Al Sayyari, A. Prevalence and Associated Factors of Chronic Kidney Disease among Relatives of Hemodialysis Patients in Saudi Arabia. Kidney Int. Rep. 2021, 6, 817–820. [Google Scholar] [CrossRef]
- Cox, K.J.; Parshall, M.B.; Hernandez, S.H.A.; Parvez, S.Z.; Unruh, M.L. Symptoms among patients receiving in-center hemodialysis: A qualitative study. Hemodial. Int. 2017, 21, 524–533. [Google Scholar] [CrossRef]
- Almutary, H.; Bonner, A.; Douglas, C. Which Patients with Chronic Kidney Disease Have the Greatest Symptom Burden? A Comparative Study of Advanced Ckd Stage and Dialysis Modality. J. Ren. Care 2016, 42, 73–82. [Google Scholar] [CrossRef]
- Benetou, S.; Alikari, V.; Vasilopoulos, G.; Polikandrioti, M.; Kalogianni, A.; Panoutsopoulos, G.I.; Toulia, G.; Leftheriotis, D.; Gerogianni, G. Factors Associated with Insomnia in Patients Undergoing Hemodialysis. Cureus 2022, 14, e22197. [Google Scholar] [CrossRef]
- Bollu, P.C.; Kaur, H. Sleep Medicine: Insomnia and Sleep. Mo. Med. 2019, 116, 68–75. [Google Scholar]
- Medic, G.; Wille, M.; Hemels, M.E. Short- and long-term health consequences of sleep disruption. Nat. Sci. Sleep 2017, 9, 151–161. [Google Scholar] [CrossRef]
- Mixson, A.; Waller, J.L.; Bollag, W.B.; Taskar, V.; Baer, S.L.; Padala, S.; Healy, W.J. The Effect of Sleep Disorder Diagnosis on Mortality in End-Stage Renal Disease Patients. Appl. Sci. 2023, 13, 5354. [Google Scholar] [CrossRef]
- Lin, A.; Zhang, F.; Zhang, H. The Relationship between Sleep Quality and Hemodialysis and Nursing Intervention in Uremia Patients Based on Intelligent Data. BioMed Res. Int. 2022, 2022, 3211144. [Google Scholar] [CrossRef]
- Scott, A.J.; Webb, T.L.; Martyn-St James, M.; Rowse, G.; Weich, S. Improving sleep quality leads to better mental health: A meta-analysis of randomised controlled trials. Sleep Med. Rev. 2021, 60, 101556. [Google Scholar] [CrossRef]
- Nagasaka, T.; Washida, N.; Uchiyama, K.; Hama, E.Y.; Kusahana, E.; Nakayama, T.; Yasuda, I.; Morimoto, K.; Itoh, H. Health-Related Quality of Life Sleep Score Predicts Transfer to Hemodialysis among Patients on Peritoneal Dialysis. Healthcare 2022, 10, 1030. [Google Scholar] [CrossRef]
- Chu, G.; Szymanski, K.; Tomlins, M.; Yates, N.; McDonald, V.M. Nursing care considerations for dialysis patients with a sleep disorder. Ren. Soc. Australas. J. 2018, 14, 52–58. [Google Scholar]
- Cukor, D.; Unruh, M.; McCurry, S.M.; Mehrotra, R. The challenge of insomnia for patients on haemodialysis. Nat. Rev. Nephrol. 2021, 17, 147–148. [Google Scholar] [CrossRef]
- Lufiyani, I.; Zahra, A.N.; Yona, S. Factors related to insomnia among end-stage renal disease patients on hemodialysis in Jakarta, Indonesia. Enfermería Clínica 2019, 29, 331–335. [Google Scholar] [CrossRef]
- Anand, S.; Johansen, K.L.; Grimes, B.; Kaysen, G.A.; Dalrymple, L.S.; Kutner, N.G.; Chertow, G.M. Physical activity and self-reported symptoms of insomnia, restless legs syndrome, and depression: The comprehensive dialysis study. Hemodial. Int. 2013, 17, 50–58. [Google Scholar] [CrossRef]
- Al-Jahdali, H.H.; Khogeer, H.A.; Al-Qadhi, W.A.; Baharoon, S.; Tamim, H.; Al-Hejaili, F.F.; Al-Ghamdi, S.M.; Al-Sayyari, A.A. Insomnia in chronic renal patients on dialysis in Saudi Arabia. J. Circadian Rhythm. 2010, 8, 7. [Google Scholar] [CrossRef]
- Huang, C.H.; Cheng, C.S.; Yen, M. Factors associated with poor sleep quality in patients with pre-dialysis chronic kidney disease: A systematic review. J. Adv. Nurs. 2023, 79, 2043–2057. [Google Scholar] [CrossRef] [PubMed]
- Guney, I.; Atalay, H.; Solak, Y.; Altintepe, L.; Toy, H.; Tonbul, H.Z.; Turk, S. Predictors of sleep quality in hemodialysis patients. Int. J.Artif. Organs. 2010, 33, 154–160. [Google Scholar] [CrossRef]
- Samara, A.M.; Sweileh, M.W.; Omari, A.M.; Omari, L.S.; Dagash, H.H.; Sweileh, W.M.; Natour, N.; Zyoud, S. An assessment of sleep quality and daytime sleepiness in hemodialysis patients: A cross-sectional study from Palestine. Sleep Sci. Pract. 2019, 3, 4. [Google Scholar] [CrossRef]
- Wali, S.O.; Alkhouli, A.; Howladar, M.; Ahmad, I.; Alshohaib, S.; Al-Ghamdi, S.; Krayem, A. Risk of obstructive sleep apnea among Saudis with chronic renal failure on hemodialysis. Ann. Thorac. Med. 2015, 10, 263–268. [Google Scholar] [CrossRef] [PubMed]
- Triguero, L.L.; Guillem, A.; Del Castillo, A.; Valdés, I.; Del Rio, R.; Peraita-Adrados, R. Prospective study of iron metabolism and RLS in blood donors. Sleep Med. 2015, 16, S71–S72. [Google Scholar] [CrossRef]
- Albatineh, A.N.; Al-Taiar, A.; Al-Sabah, R.; Zogheib, B. Psychometric Properties of the Arabic Version of the Pittsburgh Sleep Quality Index in Hemodialysis Patients. Sleep Vigil. 2022, 6, 323–333. [Google Scholar] [CrossRef]
- Al Maqbali, M.; Hughes, C.M.; Gracey, J.H.; Rankin, J.; Dunwoody, L.; Hacker, E.D. Validation of the Pittsburgh Sleep Quality Index (PSQI) with Arabic cancer patients. Sleep Biol. Rhythm. 2020, 18, 217–223. [Google Scholar] [CrossRef]
- Kaneez, M.; Zaidi, S.M.J.; Zubair, A.B.; Rehan, M.; Hassan, A.; Sarwar, Z.; Bibi, A.; Azhar, M.; Kinza, K.; Sabir, M. Sleep Quality and Compliance to Medical Therapy Among Hemodialysis Patients with Moderate-to-Severe Depression: A Cross-Sectional Study. Cureus 2021, 13, e13477. [Google Scholar] [CrossRef]
- Ho, L.L.; Chan, Y.M.; Daud, Z.M. Dietary Factors and Sleep Quality Among Hemodialysis Patients in Malaysia. J. Ren. Nutr. 2022, 32, 251–260. [Google Scholar] [CrossRef]
- Mirghaed, M.T.; Sepehrian, R.; Rakhshan, A.; Gorji, H. Sleep Quality in Iranian Hemodialysis Patients: A Systematic Review and Meta-analysis. Iran J. Nurs. Midwifery Res. 2019, 24, 403–409. [Google Scholar]
- Norozi Firoz, M.; Shafipour, V.; Jafari, H.; Hosseini, S.H.; Yazdani-Charati, J. Relationship of Hemodialysis Shift with Sleep Quality and Depression in Hemodialysis Patients. Clin. Nurs. Res. 2019, 28, 356–373. [Google Scholar] [CrossRef] [PubMed]
- Firoz, M.N.; Shafipour, V.; Jafari, H.; Hosseini, S.H.; Charati, J.Y. Sleep Quality and Depression and Their Association with Other Factors in Hemodialysis Patients. Glob. J. Health Sci. 2016, 8, 53485. [Google Scholar] [CrossRef] [PubMed]
- Fonseca, N.T.; Urbano, J.J.; Nacif, S.R.; Silva, A.S.; Peixoto, R.A.; Urbano, G.J.; Oliveira, E.F.; Santos, I.R.; Oliveira, C.S.; Insalaco, G.; et al. A systematic review of sleep disorders in patients with chronic kidney disease undergoing hemodialysis. J. Phys. Ther. Sci. 2016, 28, 2164–2170. [Google Scholar] [CrossRef] [PubMed]
- Elias, R.M.; Chan, C.T.; Paul, N.; Motwani, S.S.; Kasai, T.; Gabriel, J.M.; Spiller, N.; Bradley, T.D. Relationship of pharyngeal water content and jugular volume with severity of obstructive sleep apnea in renal failure. Nephrol. Dial. Transplant. 2013, 28, 937–944. [Google Scholar] [CrossRef]
- Li, H.; Zuo, L.; Long, S.; Li, B. Effects of nonpharmacological intervention on sleep quality in hemodialysis patients: A protocol for systematic review and meta-analysis. Medicine 2021, 100, e26401. [Google Scholar] [CrossRef]
- Otaghi, M.; Bastami, M.; Borji, M.; Tayebi, A.; Azami, M. The Effect of Continuous Care Model on the Sleep Quality of Hemodialysis Patients. Nephrourol. Mon. 2016, 8, e35467. [Google Scholar] [CrossRef]
- Yang, B.; Xu, J.; Xue, Q.; Wei, T.; Xu, J.; Ye, C.; Mei, C.; Mao, Z. Non-pharmacological interventions for improving sleep quality in patients on dialysis: Systematic review and meta-analysis. Sleep Med. Rev. 2015, 23, 68–82. [Google Scholar] [CrossRef]
- Aini, N.N.; Maliya, A. Management of Insomnia in Hemodialysis Patients: A Literature Review. J. Ber. Ilmu Keperawatan 2020, 13, 93–99. [Google Scholar] [CrossRef]
- Crowley, K. Sleep and sleep disorders in older adults. Neuropsychol. Rev. 2011, 21, 41–53. [Google Scholar] [CrossRef]
- Wang, R.; Tang, C.; Chen, X.; Zhu, C.; Feng, W.; Li, P.; Lu, C. Poor sleep and reduced quality of life were associated with symptom distress in patients receiving maintenance hemodialysis. Health Qual. Life Outcomes 2016, 14, 125. [Google Scholar] [CrossRef]
- Miner, B.; Kryger, M.H. Sleep in the Aging Population. Sleep Med. Clin. 2020, 15, 311–318. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Vitiello, M.V.; Gooneratne, N.S. Sleep in Normal Aging. Sleep Med. Clin. 2018, 13, 1–11. [Google Scholar] [CrossRef]
- Eldridge-Smith, E.D.; Holm, K.; Edinger, J.; Depew, A. 0741 Gender Differences in the Association of Household Burden with Sleep Disturbance. Sleep 2023, 46 (Suppl. S1), A326. [Google Scholar] [CrossRef]
- Guo, X.; Meng, Y.; Lian, H.; Li, Y.; Xu, Y.; Zhang, R.; Xu, J.; Wang, H.; Xu, S.; Cai, W.; et al. Marital status and living apart affect sleep quality in male military personnel: A study of the China’s Navy during COVID-19. Front Psychiatry 2023, 14, 1178235. [Google Scholar] [CrossRef] [PubMed]
- Brown, B.J.; Robinson, D.; Jensen, J.F.; Seedall, R.B.; Hodgson, J.; Norton, M.C. Will Improving My Marriage Improve My Sleep? J. Couple Relatsh. Ther. 2019, 18, 85–103. [Google Scholar] [CrossRef]
- Snyder, B.; Cunningham, R.L. Sex differences in sleep apnea and comorbid neurodegenerative diseases. Steroids 2018, 133, 28–33. [Google Scholar] [CrossRef]
- Ruge, M.; Skaaby, T.; Andersson, A.M.; Linneberg, A. Cross-sectional analysis of sleep hours and quality with sex hormones in men. Endocr. Connect. 2019, 8, 141–149. [Google Scholar] [CrossRef]
- Dorsey, A.; de Lecea, L.; Jennings, K.J. Neurobiological and Hormonal Mechanisms Regulating Women’s Sleep. Front Neurosci. 2020, 14, 625397. [Google Scholar] [CrossRef]
- Bai, Y.L.; Lai, L.Y.; Lee, B.O.; Chang, Y.Y.; Chiou, C.P. The impact of depression on fatigue in patients with haemodialysis: A correlational study. J. Clin. Nurs. 2015, 24, 2014–2022. [Google Scholar] [CrossRef]
- Salehi, F.; Dehghan, M.; Mangolian Shahrbabaki, P.; Ebadzadeh, M.R. Effectiveness of exercise on fatigue in hemodialysis patients: A randomized controlled trial. BMC Sports Sci. Med. Rehabil. 2020, 12, 19. [Google Scholar] [CrossRef]
- Wilund, K.R.; Viana, J.L.; Perez, L.M. A Critical Review of Exercise Training in Hemodialysis Patients: Personalized Activity Prescriptions Are Needed. Exerc. Sport Sci. Rev. 2020, 48, 28–39. [Google Scholar] [CrossRef] [PubMed]
- Song, Y.Y.; Hu, R.J.; Diao, Y.S.; Chen, L.; Jiang, X.L. Effects of Exercise Training on Restless Legs Syndrome, Depression, Sleep Quality, and Fatigue Among Hemodialysis Patients: A Systematic Review and Meta-analysis. J. Pain Symptom. Manag. 2018, 55, 1184–1195. [Google Scholar] [CrossRef] [PubMed]
- Hornik, B.; Dulawa, J. Frailty, Quality of Life, Anxiety, and Other Factors Affecting Adherence to Physical Activity Recommendations by Hemodialysis Patients. Int. J. Environ. Res. Public Health 2019, 16, 1827. [Google Scholar] [CrossRef] [PubMed]
- Chilcot, J.; Moss-Morris, R.; Artom, M.; Harden, L.; Picariello, F.; Hughes, H.; Bates, S.; Macdougall, I.C. Psychosocial and Clinical Correlates of Fatigue in Haemodialysis Patients: The Importance of Patients’ Illness Cognitions and Behaviours. Int. J. Behav. Med. 2016, 23, 271–281. [Google Scholar] [CrossRef] [PubMed]
- Goyal, E.; Chaudhury, S.; Saldanha, D. Psychiatric comorbidity in patients undergoing hemodialysis. Ind. Psychiatry J. 2018, 27, 206–212. [Google Scholar] [PubMed]
- Shaheen, F.A.; Al Wakeel, J.; Al-Ghamdi, S.M.; Alhelal, B.; AlGhareeb, S.; Al Obaidli, A.A.; AlSalmi, I.; Abdulaziz, H.E.; Bieber, B.A.; Pisoni, R.L.; et al. Cardiovascular and cerebrovascular comorbidities in hemodialysis patients from the Gulf Cooperation Council countries enrolled in the dialysis outcome and practice pattern study phase 5 (2012–2015). Saudi J. Kidney Dis. Transpl. 2016, 27 (Suppl. S1), S24–S30. [Google Scholar] [CrossRef]
- Jacobson, J.; Ju, A.; Baumgart, A.; Unruh, M.; O’Donoghue, D.; Obrador, G.; Craig, J.C.; Dapueto, J.M.; Dew, M.A.; Germain, M.; et al. Patient Perspectives on the Meaning and Impact of Fatigue in Hemodialysis: A Systematic Review and Thematic Analysis of Qualitative Studies. Am. J. Kidney Dis. 2019, 74, 179–192. [Google Scholar] [CrossRef]
- Mujahid, M.; Nasir, K.; Qureshi, R.; Dhrolia, M.; Ahmad, A. Comparison of the Quality of Sleep in Patients with Chronic Kidney Disease and End-Stage Renal Disease. Cureus 2022, 14, e23862. [Google Scholar] [CrossRef]
- Eslami, A.A.; Rabiei, L.; Khayri, F.; Rashidi Nooshabadi, M.R.; Masoudi, R. Sleep quality and spiritual well-being in hemodialysis patients. Iran Red. Crescent Med. J. 2014, 16, e17155. [Google Scholar] [CrossRef]
- Sevinc, M.; Hasbal, N.B.; Yilmaz, V.; Basturk, T.; Ahbap, E.; Sakaci, T.; Ozcafer, P.N.; Unsal, A. Comparison of Circulating Levels of Uremic Toxins in Hemodialysis Patients Treated with Medium Cut-Off Membranes and High-Flux Membranes: Theranova in Sisli Hamidiye Etfal (THE SHE) Randomized Control Study. Blood Purif. 2020, 49, 733–742. [Google Scholar] [CrossRef]
- Nguyen, Q.L.; Merville, P.; Couzi, L. Impact of the individualized risks of end-stage renal disease on living kidney donor selection. Nephrol. Dial. Transplant. 2018, 33, 2245–2252. [Google Scholar] [CrossRef] [PubMed]
- Daraghmeh, M.; Badran, M.; Janajreh, A.; Hassan, M.; Taha, A.A.; Koni, A.A.; Zyoud, S. Prevalence of pruritus associated with hemodialysis and its association with sleep quality among hemodialysis patients: A multicenter study. BMC Nephrol. 2022, 23, 213. [Google Scholar] [CrossRef] [PubMed]
- Eloot, S.; Holvoet, E.; Dequidt, C.; Maertens, S.J.; Vanommeslaeghe, F.; Van Biesen, W. The complexity of sleep disorders in dialysis patients. Clin. Kidney J. 2021, 14, 2029–2036. [Google Scholar] [CrossRef] [PubMed]
- Masoumi, M.; Naini, A.E.; Aghaghazvini, R.; Amra, B.; Gholamrezaei, A. Sleep quality in patients on maintenance hemodialysis and peritoneal dialysis. Int. J. Prev. Med. 2013, 4, 165–172. [Google Scholar] [CrossRef][Green Version]
- Yu, J.Y.; Kim, J.S.; Hong, C.M.; Lee, K.Y.; Cho, N.J.; Park, S.; Gil, H.W.; Lee, E.Y. Psychological distress of patients with end-stage kidney disease undergoing dialysis during the 2019 coronavirus disease pandemic: A cross-sectional study in a University Hospital. PLoS ONE 2021, 16, e0260929. [Google Scholar] [CrossRef]
- Unruh, M.; Cukor, D.; Rue, T.; Abad, K.; Roumelioti, M.E.; McCurry, S.M.; Heagerty, P.; Mehrotra, R. Sleep-HD trial: Short and long-term effectiveness of existing insomnia therapies for patients undergoing hemodialysis. BMC Nephrol. 2020, 21, 443. [Google Scholar] [CrossRef]
| Variable | N (%) | Normal Sleep | Poor Sleep | p-Value | |
|---|---|---|---|---|---|
| Age | Less than 35 | 53 (21.2) | 39 (24.5%) | 14 (15.4%) | <0.001 |
| 35–50 | 88 (35.2) | 68 (42.8%) | 19 (22.0%) | ||
| More than 50 | 109 (43.6) | 52 (32.7%) | 55 (62.6%) | ||
| Sex | Male | 144 (57.6) | 82 (51.6%) | 62 (68.1%) | 0.011 |
| Female | 106 (42.4) | 77 (48.4%) | 29 (31.9%) | ||
| Marital status | Married | 206 (82.4) | 124 (78.0%) | 82 (90.1%) | 0.015 |
| Single | 44 (17.6) | 35 (22.0%) | 9 (9.9%) | ||
| Occupational status | Employed | 73 (29.2) | 46 (28.9%) | 27 (29.7%) | 0.002 |
| Unemployed | 97 (38.8) | 70 (44.0%) | 27 (29.7%) | ||
| Student | 15 (6.0) | 13 (8.2%) | 2 (2.2%) | ||
| Retired | 65 (26.0) | 30 (18.9%) | 35 (38.5%) | ||
| Level of education | Illiterate | 60 (24.0) | 36 (22.6%) | 24 (26.4%) | |
| Primary | 30 (12.0) | 18 (11.3%) | 12 (13.2%) | 0.811 | |
| Secondary | 113 (45.2) | 73 (45.9%) | 40 (44.0%) | ||
| Higher education | 47 (18.8) | 32 (20.1%) | 15 (16.5%) | ||
| Number of dependent | No dependent | 32 (12.8) | 28 (17.6%) | 4 (4.4%) | 0.016 |
| 1–3 | 77 (30.8) | 49 (30.8%) | 28 (30.8%) | ||
| 4–6 | 82 (32.8) | 50 (31.4%) | 32 (35.2%) | ||
| ≥7 | 59 (23.6) | 32 (20.1%) | 27 (29.7%) | ||
| Financial status | Excellent | 48 (19.2) | 26 (16.4%) | 22 (24.2%) | 0.214 |
| Acceptable | 182 (72.8) | 118 (74.2%) | 64 (70.3%) | ||
| Bad | 20 (8.0) | 15 (9.4%) | 5 (5.5%) | ||
| Exercise | Yes | 29 (11.6) | 24 (15.1%) | 5 (5.5%) | 0.023 |
| No | 221 (88.4) | 135 (84.9%) | 86 (94.5%) | ||
| Number of Comorbidities | No comorbidity | 66 (26.4) | 56 (35.2%) | 10 (11.0%) | <0.001 |
| 1 | 29 (11.6) | 14 (8.8%) | 15 (16.5%) | ||
| 2 | 72 (28.8) | 46 (28.9%) | 26 (28.6%) | ||
| ≥3 | 83 (33.2) | 43 (27.0%) | 40 (44.0%) | ||
| Distance | Less than 10 | 51 (20.4) | 33 (20.8%) | 18 (19.8%) | 0.149 |
| 10–15 | 110 (44.0) | 77 (48.4%) | 33 (36.3%) | ||
| 16–20 | 57 (22.8) | 33 (20.8%) | 24 (26.4%) | ||
| More than 20 | 32 (12.8) | 16 (10.1%) | 16 (17.6%) | ||
| Dialysis duration | One or less | 60 (24.0) | 41 (25.8%) | 19 (20.9%) | 0.014 |
| 2–3 | 74 (29.6) | 55 (34.6%) | 19 (20.9%) | ||
| 4 or more | 116 (46.4) | 63 (39.6%) | 53 (58.2%) | ||
| Satisfaction | Satisfied | 240 (96.0) | 155 (97.5%) | 85 (93.4%) | 0.113 |
| Not satisfied | 10 (4.0) | 4 (2.5%) | 6 (6.6%) | ||
| Preference to change time | Yes | 16 (6.4) | 12 (7.5%) | 4 (4.4%) | 0.030 |
| No | 215 (86.0) | 140 (88.1%) | 75 (82.4%) | ||
| Sometimes | 19 (7.6) | 7 (4.4%) | 12 (13.2%) | ||
| Who select time | Patient | 120 (48.0) | 81 (50.9%) | 39 (42.9%) | 0.218 |
| Not the patient | 130 (52.0) | 78 (49.1%) | 52 (57.1%) | ||
| Factor | B | S.E. | Wald | Sig. | Odds Ratio (95% C.I.) | |
|---|---|---|---|---|---|---|
| Age | 0.010 | 0.016 | 0.411 | 0.522 | 1.010 (0.980–1.041) | |
| Sex | Male | Ref | ||||
| Female | 0.003 | 0.451 | 0.000 | 0.994 | 1.003 (0.415–2.427) | |
| Marital status | Married | Ref | ||||
| Single | −0.608 | 0.518 | 1.380 | 0.240 | 0.544 (0.197–1.501) | |
| Occupational status | Employed | Ref | ||||
| Student | −0.145 | 1.032 | 0.020 | 0.889 | 0.865 (0.114–6.541) | |
| Retired | 0.143 | 0.456 | 0.098 | 0.754 | 1.154 (0.472–2.818) | |
| Unemployed | −0.486 | 0.482 | 1.017 | 0.313 | 0.615 (0.239–1.582) | |
| Number of dependents | 0.024 | 0.066 | 0.136 | 0.713 | 1.025 (0.900–1.167) | |
| Exercise | Yes | Ref | ||||
| No | 1.506 | 0.631 | 5.696 | 0.017 | 4.509 (1.309–15.535) | |
| Number of comorbidities | No | Ref | ||||
| 1 | 1.151 | 0.482 | 5.693 | 0.020 | 3.161 (1.228–8.136) | |
| 2 | 0.383 | 0.400 | 0.919 | 0.338 | 1.467 (0.670–3.212) | |
| Duration of dialysis months | 0.000 | 0.003 | 0.002 | 0.968 | 1.000 (0.995–1.005) | |
| Preference to change time | Yes | Ref | ||||
| No | 0.236 | 0.665 | 0.126 | 0.723 | 1.266 (0.344–4.665) | |
| Sometimes | 1.391 | 0.804 | 2.996 | 0.083 | 4.018 (0.832–19.407) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alshammari, B.; Alkubati, S.A.; Pasay-an, E.; Alrasheeday, A.; Alshammari, H.B.; Asiri, S.M.; Alshammari, S.B.; Sayed, F.; Madkhali, N.; Laput, V.; et al. Sleep Quality and Its Affecting Factors among Hemodialysis Patients: A Multicenter Cross-Sectional Study. Healthcare 2023, 11, 2536. https://doi.org/10.3390/healthcare11182536
Alshammari B, Alkubati SA, Pasay-an E, Alrasheeday A, Alshammari HB, Asiri SM, Alshammari SB, Sayed F, Madkhali N, Laput V, et al. Sleep Quality and Its Affecting Factors among Hemodialysis Patients: A Multicenter Cross-Sectional Study. Healthcare. 2023; 11(18):2536. https://doi.org/10.3390/healthcare11182536
Chicago/Turabian StyleAlshammari, Bushra, Sameer A. Alkubati, Eddieson Pasay-an, Awatif Alrasheeday, Hasna B. Alshammari, Sabah M. Asiri, Sadaa B. Alshammari, Fatimah Sayed, Norah Madkhali, Vivian Laput, and et al. 2023. "Sleep Quality and Its Affecting Factors among Hemodialysis Patients: A Multicenter Cross-Sectional Study" Healthcare 11, no. 18: 2536. https://doi.org/10.3390/healthcare11182536
APA StyleAlshammari, B., Alkubati, S. A., Pasay-an, E., Alrasheeday, A., Alshammari, H. B., Asiri, S. M., Alshammari, S. B., Sayed, F., Madkhali, N., Laput, V., & Alshammari, F. (2023). Sleep Quality and Its Affecting Factors among Hemodialysis Patients: A Multicenter Cross-Sectional Study. Healthcare, 11(18), 2536. https://doi.org/10.3390/healthcare11182536







