The Use of Alternative Rooms in Forensic and Regular Psychiatric Units: A Scoping Review
Abstract
1. Introduction
1.1. Challenges on Psychiatric Wards
1.2. Risk Management and Approaches
1.3. Sensory, Multisensory and Alternative Rooms
1.4. Research Question, Objectives and Hypothesis
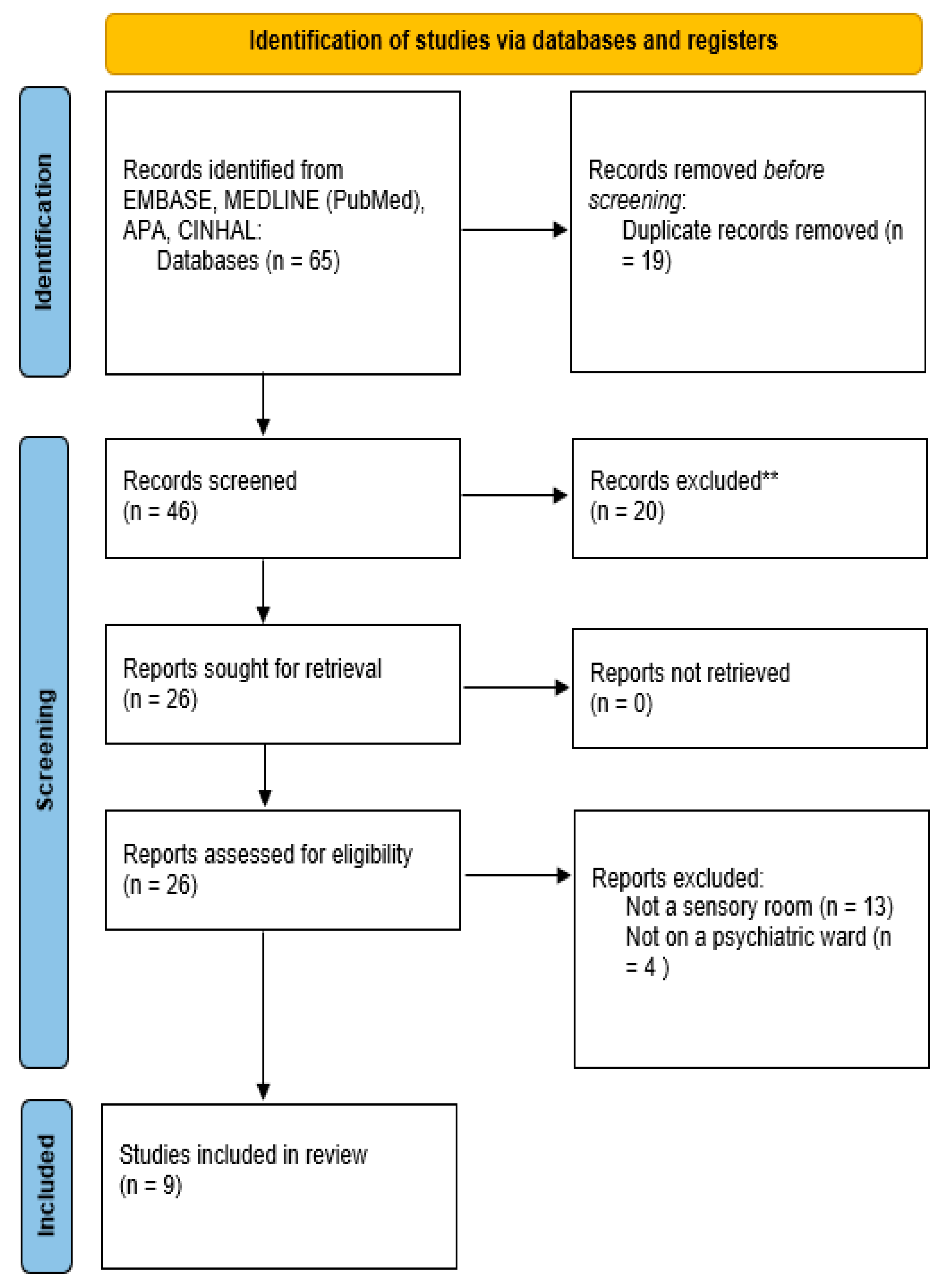
2. Materials and Methods
2.1. Search Strategies
2.2. Study Eligibility
2.3. Data Extraction
2.4. Data Management and Analysis
3. Results
3.1. Description of Studies
3.2. Alternative Rooms
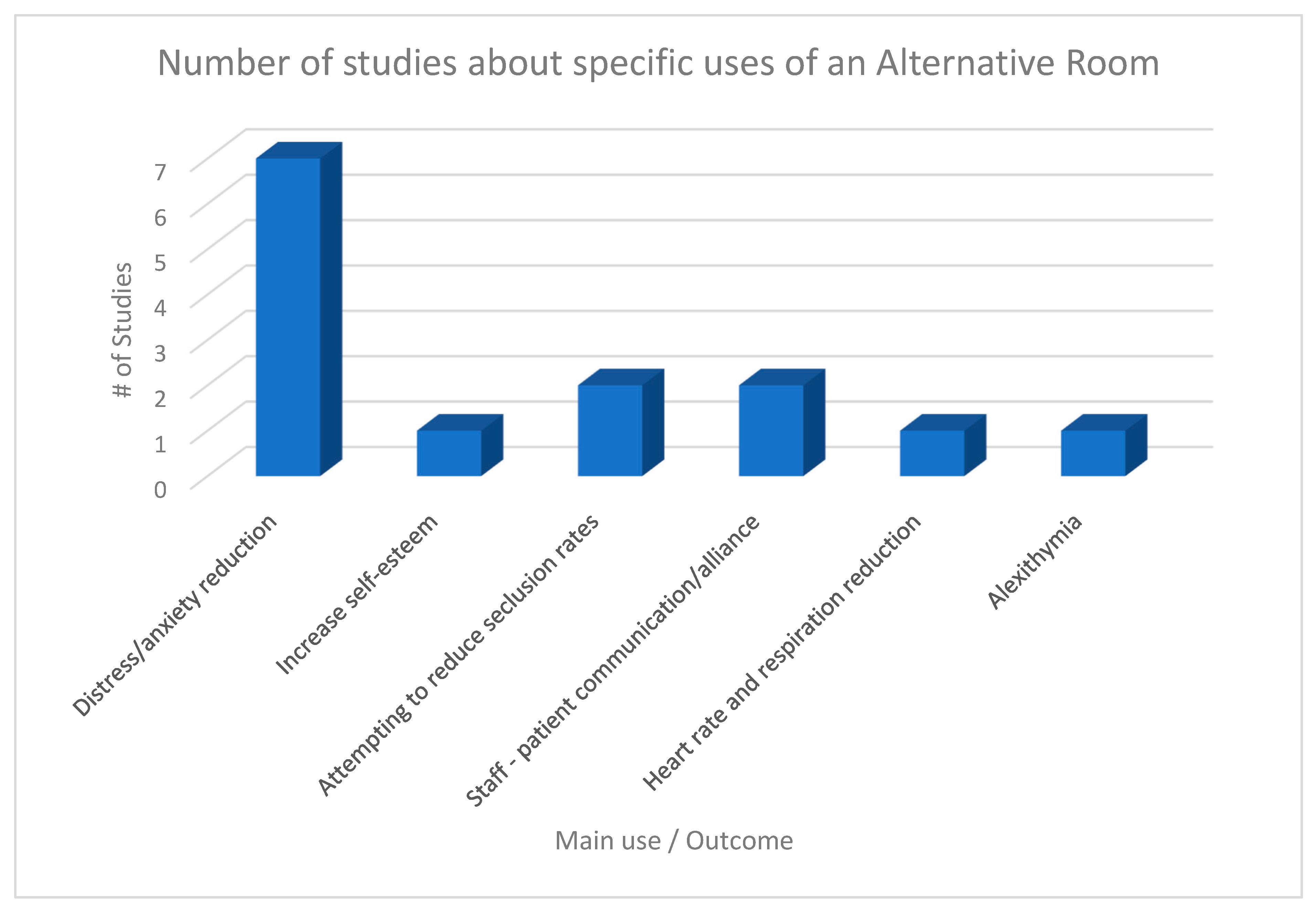
3.3. The Main Uses of Alternative Rooms and Outcomes
3.3.1. Distress and Anxiety Reduction
3.3.2. Increase of Self-Esteem
3.3.3. Impact on Seclusion Rates
3.3.4. Staff and Patients’ Communication and Alliance
3.3.5. Biometrics: Heart Rate and Respiration Rate Reduction
3.3.6. Alexithymia
4. Discussion
4.1. Review of Findings
4.2. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Alternative Rooms | Psychiatric Unit | |
|---|---|---|
| EMBASE | X | psychiatric department/OR mental hospital/ |
| MEDLINE | X | Emergency Services, Psychiatric/or Hospitals, Psychiatric/or Psychiatric Department, Hospital/ |
| APA | sensory room/comfort room | psychiatric hospitals/or psychiatric units/or mental health clinics/ |
| CINHAL | X | |
| Open vocabulary | (((Room OR space OR centre OR studio) N3 (Sport OR sports OR fitness OR relaxation OR meditation OR game OR games OR gaming OR boardgame OR boardgames OR play OR yoga OR alternative OR creative OR art OR arts OR ludic OR multisensory OR sensory OR dining OR quiet or well-being OR well-being OR leisure OR recreation OR recreational OR recreative OR music OR alternative)) OR (Gym OR theater OR swimming pool OR garden OR library)) | (psychiatric OR mental) N2 (department* OR Unit * OR ward * OR hospital * OR clinic * OR centre*) |
References
- Fowler, J.C.; Allen, J.G.; Hart, J.M.; Szlykh, H.; Ellis, T.E.; Frueh, B.C.; Oldham, J.M. Intensive inpatient treatment improves emotion-regulation capacities among adults with severe mental illness. Borderline Personal. Disord. Emot. Dysregul. 2014, 1, 19. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Rufino, K.A.; Ward-Ciesielski, E.F.; Webb, C.A.; Nadorff, M.R. Emotion regulation difficulties are associated with nightmares and suicide attempts in an adult psychiatric inpatient sample. Psychiatry Res. 2020, 293, 113437. [Google Scholar] [CrossRef]
- Alzahrani, N. The effect of hospitalization on patients’ emotional and psychological well-being among adult patients: An integrative review. Appl. Nurs. Res. 2021, 61, 151488. [Google Scholar] [CrossRef]
- Camus, D.; Dan Glauser, E.S.; Gholamrezaee, M.; Gasser, J.; Moulin, V. Factors associated with repetitive violent behaviour of psychiatric inpatients. Psychiatry Res. 2021, 296, 113643. [Google Scholar] [CrossRef] [PubMed]
- Kelly, E.L.; Fenwick, K.; Brekke, J.S.; Novaco, R.W. Well-Being and Safety Among Inpatient Psychiatric Staff: The Impact of Conflict, Assault, and Stress Reactivity. Adm. Policy Ment. Health 2016, 43, 703–716. [Google Scholar] [CrossRef]
- Ulrich, R.S.; Bogren, L.; Gardiner, S.K.; Lundin, S. Psychiatric ward design can reduce aggressive behaviour. J. Environ. Psychol. 2018, 57, 53–66. [Google Scholar] [CrossRef]
- Papoulias, C.; Csipke, E.; Rose, D.; McKellar, S.; Wykes, T. The psychiatric ward as a therapeutic space: Systematic review. Br. J. Psychiatry 2014, 205, 171–176. [Google Scholar] [CrossRef]
- Seppanen, A.; Tormanen, I.; Shaw, C.; Kennedy, H. Modern forensic psychiatric hospital design: Clinical, legal and structural aspects. Int. J. Ment. Health Syst. 2018, 12, 58. [Google Scholar] [CrossRef] [PubMed]
- Robins, L.M.; Lee, D.A.; Bell, J.S.; Srikanth, V.; Mohler, R.; Hill, K.D.; Haines, T.P. Definition and Measurement of Physical and Chemical Restraint in Long-Term Care: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 3639. [Google Scholar] [CrossRef]
- Muir-Cochrane, E.; Oster, C.; Gerace, A.; Dawson, S.; Damarell, R.; Grimmer, K. The effectiveness of chemical restraint in managing acute agitation and aggression: A systematic review of randomized controlled trials. Int. J. Ment. Health Nurs. 2020, 29, 110–126. [Google Scholar] [CrossRef]
- Philip, N.S.; Mello, K.; Carpenter, L.L.; Tyrka, A.R.; Price, L.H. Patterns of quetiapine use in psychiatric inpatients: An examination of off-label use. Ann. Clin. Psychiatry 2008, 20, 15–20. [Google Scholar] [CrossRef]
- Srivastava, A. Limited evidence for the effectiveness of p.r.n. Medications among psychiatric inpatients. J. Psychiatr. Pract. 2009, 15, 193–201. [Google Scholar] [CrossRef] [PubMed]
- Lantta, T.; Varpula, J.; Cheung, T.; Wong, W.K.; Cheng, P.Y.I.; Ng, T.; Ng, C.F.; Yam, C.P.; Ip, G.; Bressington, D.; et al. Prevention and management of aggressive behaviour in patients at psychiatric hospitals: A document analysis of clinical practice guidelines in Hong Kong. Int. J. Ment. Health Nurs. 2020, 29, 1079–1091. [Google Scholar] [CrossRef] [PubMed]
- Haugom, W.; Ruud, T.; Hynnekleiv, T. Ethical challenges of seclusion in psychiatric inpatient wards: A qualitative study of the experiences of Norwegian mental health professionals. BMC Health Serv. Res. 2019, 19, 879. [Google Scholar] [CrossRef] [PubMed]
- Zheng, C.; Li, S.; Chen, Y.; Ye, J.; Xiao, A.; Xia, Z.; Liao, Y.; Xu, Y.; Zhang, Y.; Yu, L.; et al. Ethical consideration on use of seclusion in mental health services. Int. J. Nurs. Sci. 2019, 7, 116–120. [Google Scholar] [CrossRef]
- Cummings, K.S.; Grandfield, S.A.; Coldwell, C.M. Caring with comfort rooms. Reducing seclusion and restraint use in psychiatric facilities. J. Psychosoc. Nurs. Ment. Health Serv. 2010, 48, 26–30. [Google Scholar] [CrossRef]
- Hedlund Lindberg, M.; Samuelsson, M.; Perseius, K.I.; Bjorkdahl, A. The experiences of patients in using sensory rooms in psychiatric inpatient care. Int. J. Ment. Health Nurs. 2019, 28, 930–939. [Google Scholar] [CrossRef]
- Askew, L.; Fisher, P.; Beazley, P. Being in a Seclusion Room: The Forensic Psychiatric Inpatients’ Perspective. J. Psychiatr. Ment. Health Nurs. 2020, 27, 272–280. [Google Scholar] [CrossRef]
- Larue, C.; Dumais, A.; Boyer, R.; Goulet, M.H.; Bonin, J.P.; Baba, N. The experience of seclusion and restraint in psychiatric settings: Perspectives of patients. Issues Ment. Health Nurs. 2013, 34, 317–324. [Google Scholar] [CrossRef]
- Unwin, K.L.; Powell, G.; Jones, C.R. The use of Multisensory Environments with autistic children: Exploring the effect of having control of sensory changes. Autism 2022, 26, 1379–1394. [Google Scholar] [CrossRef]
- Bobier, C.; Boon, T.; Downward, M.; Loomes, B.; Mountford, H.; Swadi, H. Pilot Investigation of the Use and Usefulness of a Sensory Modulation Room in a Child and Adolescent Psychiatric Inpatient Unit. Occup. Ther. Ment. Health 2015, 31, 385–401. [Google Scholar] [CrossRef]
- Backman, C.; Demery-Varin, M.; Cho-Young, D.; Crick, M.; Squires, J. Impact of sensory interventions on the quality of life of long-term care residents: A scoping review. BMJ Open. 2021, 11, e042466. [Google Scholar] [CrossRef]
- Chalmers, A.; Harrison, S.; Mollison, K.; Molloy, N.; Gray, K. Establishing sensory-based approaches in mental health inpatient care: A multidisciplinary approach. Australas. Psychiatry 2012, 20, 35–39. [Google Scholar] [CrossRef]
- Cheng, S.C.; Hsu, W.S.; Shen, S.H.; Hsu, M.C.; Lin, M.F. Dose-Response Relationships of Multisensory Intervention on Hospitalized Patients with Chronic Schizophrenia. J. Nurs. Res. 2017, 25, 13–20. [Google Scholar] [CrossRef] [PubMed]
- Di Taranto, C.; Procenesi, L.; Paterniti, A.M.; Loppi, E.; Speranza, A.R.; Siracusano, A.; Niolu, C. Outcome of the use of the Snoezelen Multisensory Room in an alexithymic patient: A case report. Riv. Psichiatr. 2022, 57, 134–140. [Google Scholar] [PubMed]
- Dorn, E.; Hitch, D.; Stevenson, C. An Evaluation of a Sensory Room within an Adult Mental Health Rehabilitation Unit. Occup. Ther. Ment. Health 2019, 36, 105–118. [Google Scholar] [CrossRef]
- Forsyth, A.S.; Trevarrow, R. Sensory strategies in adult mental health: A qualitative exploration of staff perspectives following the introduction of a sensory room on a male adult acute ward. Int. J. Ment. Health Nurs. 2018, 27, 1689–1697. [Google Scholar] [CrossRef]
- Novak, T.; Scanlan, J.; McCaul, D.; MacDonald, N.; Clarke, T. Pilot study of a sensory room in an acute inpatient psychiatric unit. Australas. Psychiatry 2012, 20, 401–406. [Google Scholar] [CrossRef]
- Smith, S.; Jones, J. Use of a sensory room on an intensive care unit. J. Psychosoc. Nurs. Ment. Health Serv. 2014, 52, 22–30. [Google Scholar] [CrossRef]
- Wiglesworth, S.; Farnworth, L. An Exploration of the Use of a Sensory Room in a Forensic Mental Health Setting: Staff and Patient Perspectives. Occup. Ther. Int. 2016, 23, 255–264. [Google Scholar] [CrossRef]
- Champagne, T.; Stromberg, N. Sensory approaches in inpatient psychiatric settings: Innovative alternatives to seclusion et restraint. J. Psychosoc. Nurs. Ment. Health Serv. 2004, 42, 34–44. [Google Scholar] [CrossRef] [PubMed]
- Adams-Leask, K.; Varona, L.; Dua, C.; Baldock, M.; Gerace, A.; Muir-Cochrane, E. The benefits of sensory modulation on levels of distress for consumers in a mental health emergency setting. Australas. Psychiatry 2018, 26, 514–519. [Google Scholar] [CrossRef] [PubMed]
- Feinstein, J.S.; Khalsa, S.S.; Yeh, H.; Al Zoubi, O.; Arevian, A.C.; Wohlrab, C.; Pantino, M.K.; Cartmell, L.J.; Simmons, W.K.; Stein, M.B.; et al. The Elicitation of Relaxation and Interoceptive Awareness Using Floatation Therapy in Individuals with High Anxiety Sensitivity. Biol. Psychiatry Cogn. Neurosci. Neuroimaging 2018, 3, 555–562. [Google Scholar] [CrossRef] [PubMed]
- Jerath, R.; Crawford, M.W.; Barnes, V.A.; Harden, K. Self-regulation of breathing as a primary treatment for anxiety. Appl. Psychophysiol. Biofeedback 2015, 40, 107–115. [Google Scholar] [CrossRef]
- Souza, E.V., Jr.; Cruz, D.P.; Siqueira, L.R.; Rosa, R.S.; Silva, C.D.S.; Biondo, C.S.; Sawada, N.O. Is self-esteem associated with the elderly person’s quality of life? Rev. Bras. Enferm. 2022, 75 (Suppl. S4), e20210388. [Google Scholar] [CrossRef]
- Fernandes, B.; Newton, J.; Essau, C.A. The mediating effects of self-esteem on anxiety and emotion regulation. Psychol. Rep. 2021, 125, 787–803. [Google Scholar] [CrossRef]
- Li, C.; Fu, P.; Wang, M.; Xia, Y.; Hu, C.; Liu, M.; Zhang, H.; Sheng, X.; Yang, Y. The role of self-esteem and emotion regulation in the associations between childhood trauma and mental health in adulthood: A moderated mediation model. BMC Psychiatry 2023, 23, 241. [Google Scholar] [CrossRef]
- Álvarez, M.-J.; Roura, P.; Osés, A.; Foguet, Q.; Solà, J.; Arrufat, F.-X. Prevalence and clinical impact of childhood trauma in patients with severe mental disorders. J. Nerv. Ment. Dis. 2011, 199, 156–161. [Google Scholar] [CrossRef]
- Andersen, C.; Kolmos, A.; Andersen, K.; Sippel, V.; Stenager, E. Applying sensory modulation to mental health inpatient care to reduce seclusion and restraint: A case control study. Nord. J. Psychiatry 2017, 71, 525–528. [Google Scholar] [CrossRef]
- Bayramzadeh, S.; Ahmadpour, S.; Aghaei, P. The relationship between sensory stimuli and the physical environment in complex healthcare settings: A systematic literature review. Intensive Crit. Care Nurs. 2021, 67, 103111. [Google Scholar] [CrossRef]
- Tölli, S.; Kontio, R.; Partanen, P.; Terkamo-Moisio, A.; Häggman-Laitila, A. Humane and comprehensive management of challenging behaviour in health and Social Care: Cross-sectional study testing newly developed instrument. Healthcare 2023, 11, 753. [Google Scholar] [CrossRef] [PubMed]
- Van den Boogert, F.; Klein, K.; Spaan, P.; Sizoo, B.; Bouman, Y.H.A.; Hoogendijk, W.J.G.; Roza, S.J. Sensory processing difficulties in psychiatric disorders: A meta-analysis. J. Psychiatr. Res. 2022, 151, 173–180. [Google Scholar] [CrossRef] [PubMed]
- Jakobson, L.S.; Rigby, S.N. Alexithymia and Sensory Processing Sensitivity: Areas of Overlap and Links to Sensory Processing Styles. Front. Psychol. 2021, 12, 583786. [Google Scholar] [CrossRef] [PubMed]
| Studies | Type of Room | Population (n) | Clinical Setting | Main Use and Outcomes | Type of Items | Architectural Characteristics |
|---|---|---|---|---|---|---|
| (Chalmers et al., 2012) [23] | Sensory room | Staff and Patients (n: N/A; N/A) | Regular psychiatric unit | Significative decrease in distress Psychometric instruments used: -Fremantle Acute Arousal Scale | Weighted items, Visual items, Olfactive items, Tactile items, Gustatory items, Auditory props | N/A |
| (Cheng et al., 2017) [24] | Multisensory intervention space | Patients with chronic schizophrenia (n = 60) | Regular psychiatric unit | Reduction of anxiety and stabilization of respiration and heart rates. Psychometric instruments used: - Hospital Anxiety and Depression Scale -Schizophrenia Patients’ Subjective Well-being | Weighted items, Visual items, Olfactive items, Tactile items, Gustatory items, Auditory props, Proprioceptive props | N/A |
| (Di Tarantino et al., 2022) [25] | Snoezelen multisensory room | The sister of a patient (n = 1) | Regular psychiatric unit | Alexithymia: Improved ability of narration of her own life and emotions Psychometric instruments used: -Minnesota Multiphasic Personality Inventory-2 -Brief Psychiatric Rating Scale -Hamilton Anxiety Scale Hamilton Rating Scale for Depression -Toronto Alexythimia Scale -Toronto Structured Interview for Alexithymia | Weighted items, Visual items, Olfactive items, Tactile items, Auditory props | N/A |
| (Dorn et al., 2020) [26] | Sensory room | Patients (n = 24) | Rehabilitation unit (locked) | Significantly and consistently decreased consumers’ arousal Psychometric instruments used: - Sensory Modulation Consumer Self Rating Tool | Weighted items, Visual items, Olfactive items, Tactile items, Gustatory items, Auditory props | Locked space |
| (Forsyth et Trevarrow, 2018) [27] | Sensory room: Chillout room | Staff (n = 6) | Acute psychiatric ward | Reducing distress. Enhancing de-escalation interventions, sensory interventions, and positive impact on staff. | Weighted items, Visual items, Tactile items, Auditory props | N/A |
| (Hedlund Lindberg et al., 2019) [17] | Sensory room | Patients (n = 28) | Ten regular psychiatric wards | Enhanced well-being, reduced anxiety, increased self-management and enhanced self-esteem | Weighted items, Visual items, Olfactive items, Tactile items, Gustatory items, Auditory props | N/A |
| (Novak et al., 2012) [28] | Comfort room | Patients (n = 75) | Acute psychiatric ward | Reduction in distress, improvements in a range of disturbed behaviors. Weighted blanket: significantly greater reduction in distress and clinician-rated anxiety. No reduction in seclusion rates. Psychometric instruments used: - Sensory room assessment form (locally developed) | Weighted items, Visual items, Olfactive items, Tactile items, Auditory props | N/A |
| (Smith et al., 2014) [29] | Sensory room | Staff and patients (n = 10; 7) | Intensive psychiatric care unit | Improvement in staff-patient communication. Perception of less seclusion rate by the staff but no actual reduction in seclusion rates. | Visual items, Olfactive items, Tactile items, Gustatory items, Auditory props | 5 m per 2.5 m, blue painted walls, laminate flooring and one window. |
| (Wiglesworth et Farnworth, 2016) [30] | Sensory room | Staff and patients (n = N/A; 5) | Forensic psychiatric unit | Mean decrease in distress. Psychometric instruments used: - Adult/Adolescent Sensory Profile | Weighted items, Visual items, Olfactive items, Tactile items, Gustatory items, Auditory props | N/A |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hudon, A.; Rosca, M.A.; La Charité-Harbec, O.; Allard, J.-M.; Borduas Pagé, S. The Use of Alternative Rooms in Forensic and Regular Psychiatric Units: A Scoping Review. Healthcare 2023, 11, 2432. https://doi.org/10.3390/healthcare11172432
Hudon A, Rosca MA, La Charité-Harbec O, Allard J-M, Borduas Pagé S. The Use of Alternative Rooms in Forensic and Regular Psychiatric Units: A Scoping Review. Healthcare. 2023; 11(17):2432. https://doi.org/10.3390/healthcare11172432
Chicago/Turabian StyleHudon, Alexandre, Maria Alexandra Rosca, Olivier La Charité-Harbec, Jeanne-Marie Allard, and Stéphanie Borduas Pagé. 2023. "The Use of Alternative Rooms in Forensic and Regular Psychiatric Units: A Scoping Review" Healthcare 11, no. 17: 2432. https://doi.org/10.3390/healthcare11172432
APA StyleHudon, A., Rosca, M. A., La Charité-Harbec, O., Allard, J.-M., & Borduas Pagé, S. (2023). The Use of Alternative Rooms in Forensic and Regular Psychiatric Units: A Scoping Review. Healthcare, 11(17), 2432. https://doi.org/10.3390/healthcare11172432








