Sarcopenia and Anemia in Elderly Koreans: A Nationwide Population-Based Study
Abstract
1. Introduction
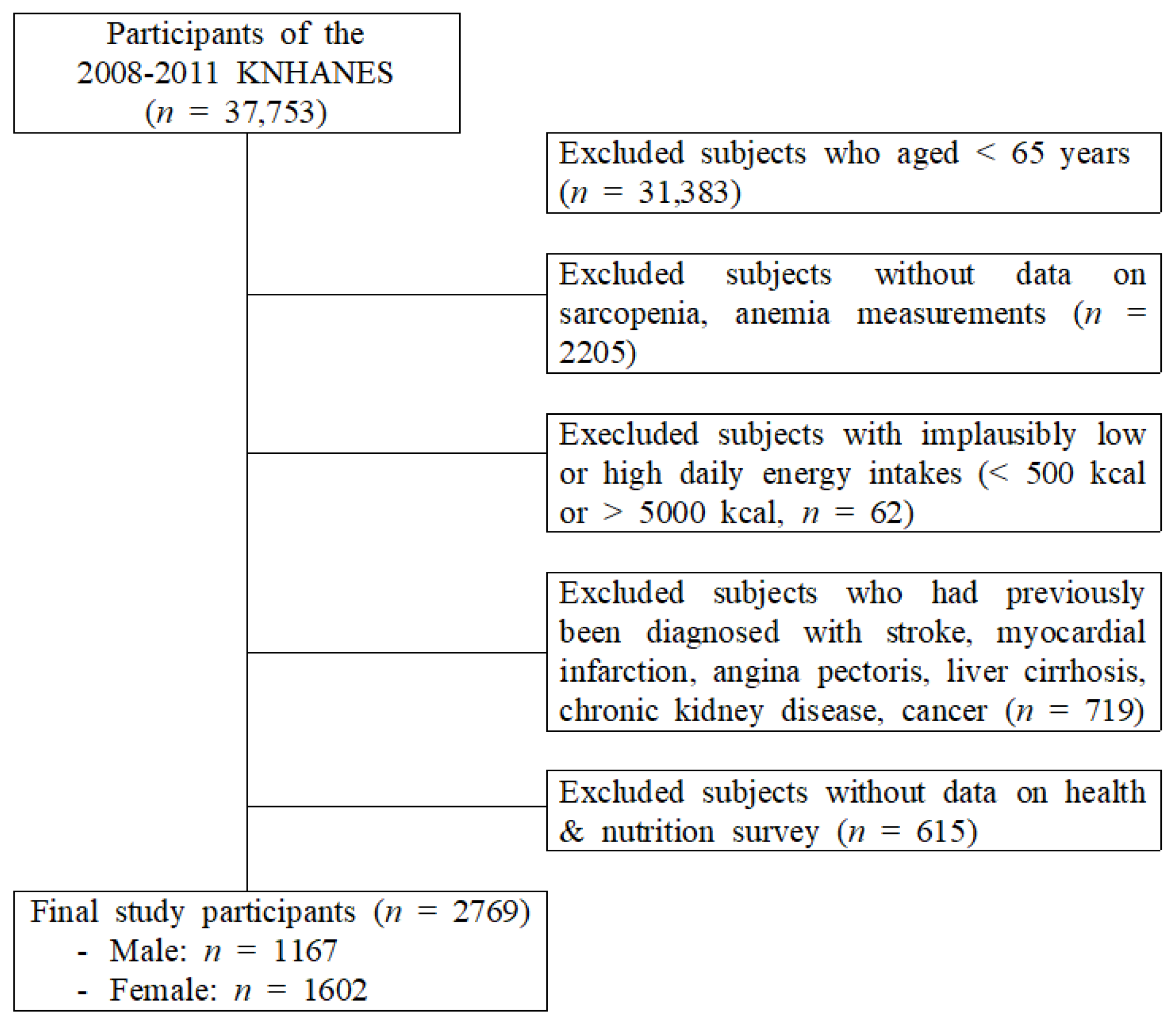
2. Materials and Methods
2.1. Data Source and Sampling
2.2. Measurements of Variables
2.2.1. Covariates
2.2.2. Measurements of Sarcopenia
2.2.3. Measurements of Anemia
2.3. Data Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bao, W.; Sun, Y.; Zhang, T.; Zou, L.; Wu, X.; Wang, D.; Chen, Z. Exercise Programs for Muscle Mass, Muscle Strength and Physical Performance in Older Adults with Sarcopenia: A Systematic Review and Meta-Analysis. Aging Dis. 2020, 11, 863–873. [Google Scholar] [CrossRef] [PubMed]
- Ferrucci, L.; Guralnik, J.M.; Buchner, D.; Kasper, J.; Lamb, S.E.; Simonsick, E.M.; Corti, M.C.; Bandeen-Roche, K.; Fried, L.P. Departures from linearity in the relationship between measures of muscular strength and physical performance of the lower extremities: The Women’s Health and Aging Study. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 1997, 52, M275–M285. [Google Scholar] [CrossRef]
- Lauretani, F.; Russo, C.R.; Bandinelli, S.; Bartali, B.; Cavazzini, C.; Di Iorio, A.; Corsi, A.M.; Rantanen, T.; Guralnik, J.M.; Ferrucci, L. Age-associated changes in skeletal muscles and their effect on mobility: An operational diagnosis of sarcopenia. J. Appl. Physiol. 2003, 95, 1851–1860. [Google Scholar] [CrossRef] [PubMed]
- Janssen, I. Influence of sarcopenia on the development of physical disability: The Cardiovascular Health Study. J. Am. Geriatr. Soc. 2006, 54, 56–62. [Google Scholar] [CrossRef]
- Lee, D.-Y. The Association between Sarcopenia and Pulmonary Function in Koreans: A Cross-Sectional Study. Int. J. Gerontol. 2021, 15, 319–323. [Google Scholar]
- Lee, D.Y.; Shin, S. Association of Sarcopenia with Osteopenia and Osteoporosis in Community-Dwelling Older Korean Adults: A Cross-Sectional Study. J. Clin. Med. 2021, 11, 129. [Google Scholar] [CrossRef]
- Lee, D.Y.; Shin, S. Sarcopenia Is Associated with Metabolic Syndrome in Korean Adults Aged over 50 Years: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2022, 19, 1330. [Google Scholar] [CrossRef] [PubMed]
- Cruz-Jentoft, A.J.; Sayer, A.A. Sarcopenia. Lancet 2019, 393, 2636–2646. [Google Scholar] [CrossRef] [PubMed]
- Curcio, F.; Ferro, G.; Basile, C.; Liguori, I.; Parrella, P.; Pirozzi, F.; Della-Morte, D.; Gargiulo, G.; Testa, G.; Tocchetti, C.G.; et al. Biomarkers in sarcopenia: A multifactorial approach. Exp. Gerontol. 2016, 85, 1–8. [Google Scholar] [CrossRef]
- Cappellini, M.D.; Motta, I. Anemia in Clinical Practice-Definition and Classification: Does Hemoglobin Change with Aging? Semin. Hematol. 2015, 52, 261–269. [Google Scholar] [CrossRef]
- Steensma, D.P.; Tefferi, A. Anemia in the elderly: How should we define it, when does it matter, and what can be done? Mayo Clin. Proc. 2007, 82, 958–966. [Google Scholar] [CrossRef]
- Penninx, B.W.; Guralnik, J.M.; Onder, G.; Ferrucci, L.; Wallace, R.B.; Pahor, M. Anemia and decline in physical performance among older persons. Am. J. Med. 2003, 115, 104–110. [Google Scholar] [CrossRef] [PubMed]
- Penninx, B.W.; Pahor, M.; Cesari, M.; Corsi, A.M.; Woodman, R.C.; Bandinelli, S.; Guralnik, J.M.; Ferrucci, L. Anemia is associated with disability and decreased physical performance and muscle strength in the elderly. J. Am. Geriatr. Soc. 2004, 52, 719–724. [Google Scholar] [CrossRef]
- Ganz, T. Anemia of Inflammation. N. Engl. J. Med. 2019, 381, 1148–1157. [Google Scholar] [CrossRef] [PubMed]
- Johnson-Wimbley, T.D.; Graham, D.Y. Diagnosis and management of iron deficiency anemia in the 21st century. Ther. Adv. Gastroenterol. 2011, 4, 177–184. [Google Scholar] [CrossRef]
- Atkinson, M.A.; Warady, B.A. Anemia in chronic kidney disease. Pediatr. Nephrol. 2018, 33, 227–238. [Google Scholar] [CrossRef] [PubMed]
- Denny, S.D.; Kuchibhatla, M.N.; Cohen, H.J. Impact of anemia on mortality, cognition, and function in community-dwelling elderly. Am. J. Med. 2006, 119, 327–334. [Google Scholar] [CrossRef]
- Madu, A.J.; Ughasoro, M.D. Anaemia of Chronic Disease: An In-Depth Review. Med. Princ. Pract. 2017, 26, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Wiciński, M.; Liczner, G.; Cadelski, K.; Kołnierzak, T.; Nowaczewska, M.; Malinowski, B. Anemia of Chronic Diseases: Wider Diagnostics-Better Treatment? Nutrients 2020, 12, 1784. [Google Scholar] [CrossRef]
- Gomes, M.J.; Martinez, P.F.; Pagan, L.U.; Damatto, R.L.; Cezar, M.D.M.; Lima, A.R.R.; Okoshi, K.; Okoshi, M.P. Skeletal muscle aging: Influence of oxidative stress and physical exercise. Oncotarget 2017, 8, 20428–20440. [Google Scholar] [CrossRef]
- Powers, S.K.; Kavazis, A.N.; McClung, J.M. Oxidative stress and disuse muscle atrophy. J. Appl. Physiol. 2007, 102, 2389–2397. [Google Scholar] [CrossRef]
- Cesari, M.; Penninx, B.W.; Lauretani, F.; Russo, C.R.; Carter, C.; Bandinelli, S.; Atkinson, H.; Onder, G.; Pahor, M.; Ferrucci, L. Hemoglobin levels and skeletal muscle: Results from the InCHIANTI study. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2004, 59, 249–254. [Google Scholar] [CrossRef] [PubMed]
- Frisoli, A., Jr.; Chaves, P.H.; Pinheiro, M.M.; Szejnfeld, V.L. The effect of nandrolone decanoate on bone mineral density, muscle mass, and hemoglobin levels in elderly women with osteoporosis: A double-blind, randomized, placebo-controlled clinical trial. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2005, 60, 648–653. [Google Scholar] [CrossRef] [PubMed]
- Hirani, V.; Naganathan, V.; Blyth, F.; Le Couteur, D.G.; Seibel, M.J.; Waite, L.M.; Handelsman, D.J.; Hsu, B.; Cumming, R.G. Low Hemoglobin Concentrations Are Associated with Sarcopenia, Physical Performance, and Disability in Older Australian Men in Cross-sectional and Longitudinal Analysis: The Concord Health and Ageing in Men Project. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2016, 71, 1667–1675. [Google Scholar] [CrossRef]
- Moon, J.-H.; Kong, M.-H.; Kim, H.-J. Relationship between low muscle mass and anemia in Korean elderly men: Using the Korea National Health and Nutrition Examination Survey (KNHANES IV–V). J. Clin. Gerontol. Geriatr. 2015, 6, 115–119. [Google Scholar] [CrossRef]
- Vinke, J.S.J.; Wouters, H.; Stam, S.P.; Douwes, R.M.; Post, A.; Gomes-Neto, A.W.; van der Klauw, M.M.; Berger, S.P.; Bakker, S.J.L.; De Borst, M.H.; et al. Decreased haemoglobin levels are associated with lower muscle mass and strength in kidney transplant recipients. J. Cachexia Sarcopenia Muscle 2022, 13, 2044–2053. [Google Scholar] [CrossRef]
- Payne, C.F.; Davies, J.I.; Gomez-Olive, F.X.; Hands, K.J.; Kahn, K.; Kobayashi, L.C.; Tipping, B.; Tollman, S.M.; Wade, A.; Witham, M.D. Cross-sectional relationship between haemoglobin concentration and measures of physical and cognitive function in an older rural South African population. J. Epidemiol. Community Health 2018, 72, 796–802. [Google Scholar] [CrossRef]
- Zeng, F.; Huang, L.; Zhang, Y.; Hong, X.; Weng, S.; Shen, X.; Zhao, F.; Yan, S. Additive Effect of Sarcopenia and Anemia on the 10-Year Risk of Cardiovascular Disease in Patients with Type 2 Diabetes. J. Diabetes Res. 2022, 2022, 2202511. [Google Scholar] [CrossRef]
- Oh, J.Y.; Yang, Y.J.; Kim, B.S.; Kang, J.H. Validity and reliability of Korean version of International Physical Activity Questionnaire (IPAQ) short form. J. Korean Acad. Fam. Med. 2007, 28, 532–541. [Google Scholar]
- Chen, L.K.; Woo, J.; Assantachai, P.; Auyeung, T.W.; Chou, M.Y.; Iijima, K.; Jang, H.C.; Kang, L.; Kim, M.; Kim, S.; et al. Asian Working Group for Sarcopenia: 2019 Consensus Update on Sarcopenia Diagnosis and Treatment. J. Am. Med. Dir. Assoc. 2020, 21, 300–307.e302. [Google Scholar] [CrossRef]
- World Health Organization. Nutritional Anaemias: Report of a WHO Scientific Group [Meeting Held in Geneva from 13 to 17 March 1967]; World Health Organization: Geneva, Switzerland, 1968. [Google Scholar]
- Tseng, S.H.; Lee, W.J.; Peng, L.N.; Lin, M.H.; Chen, L.K. Associations between hemoglobin levels and sarcopenia and its components: Results from the I-Lan longitudinal study. Exp. Gerontol. 2021, 150, 111379. [Google Scholar] [CrossRef]
- Mairbäurl, H.; Weber, R.E. Oxygen transport by hemoglobin. Compr. Physiol. 2012, 2, 1463–1489. [Google Scholar] [CrossRef] [PubMed]
- Reeder, B.J.; Wilson, M.T. Hemoglobin and myoglobin associated oxidative stress: From molecular mechanisms to disease States. Curr. Med. Chem. 2005, 12, 2741–2751. [Google Scholar] [CrossRef] [PubMed]
- Moylan, J.S.; Reid, M.B. Oxidative stress, chronic disease, and muscle wasting. Muscle Nerve 2007, 35, 411–429. [Google Scholar] [CrossRef]
- Bianchi, V.E. Anemia in the elderly population. J. Hematol. 2015, 3, 95–106. [Google Scholar] [CrossRef][Green Version]
- Sieber, C.C. Malnutrition and sarcopenia. Aging Clin. Exp. Res. 2019, 31, 793–798. [Google Scholar] [CrossRef] [PubMed]
- Thakur, N.; Chandra, J.; Pemde, H.; Singh, V. Anemia in severe acute malnutrition. Nutrition 2014, 30, 440–442. [Google Scholar] [CrossRef]
- Mitrache, C.; Passweg, J.R.; Libura, J.; Petrikkos, L.; Seiler, W.O.; Gratwohl, A.; Stähelin, H.B.; Tichelli, A. Anemia: An indicator for malnutrition in the elderly. Ann. Hematol. 2001, 80, 295–298. [Google Scholar] [CrossRef]
- Rossman, M.J.; Venturelli, M.; McDaniel, J.; Amann, M.; Richardson, R.S. Muscle mass and peripheral fatigue: A potential role for afferent feedback? Acta Physiol. 2012, 206, 242–250. [Google Scholar] [CrossRef]
- Zwart, A.T.; van der Hoorn, A.; van Ooijen, P.M.A.; Steenbakkers, R.; de Bock, G.H.; Halmos, G.B. CT-measured skeletal muscle mass used to assess frailty in patients with head and neck cancer. J. Cachexia Sarcopenia Muscle 2019, 10, 1060–1069. [Google Scholar] [CrossRef]
- Cruz-Jentoft, A.J.; Kiesswetter, E.; Drey, M.; Sieber, C.C. Nutrition, frailty, and sarcopenia. Aging Clin. Exp. Res. 2017, 29, 43–48. [Google Scholar] [CrossRef]
- Goisser, S.; Guyonnet, S.; Volkert, D. The Role of Nutrition in Frailty: An Overview. J. Frailty Aging 2016, 5, 74–77. [Google Scholar] [CrossRef]
- Bano, G.; Trevisan, C.; Carraro, S.; Solmi, M.; Luchini, C.; Stubbs, B.; Manzato, E.; Sergi, G.; Veronese, N. Inflammation and sarcopenia: A systematic review and meta-analysis. Maturitas 2017, 96, 10–15. [Google Scholar] [CrossRef] [PubMed]
- Iqbal, T.; Stein, J.; Sharma, N.; Kulnigg-Dabsch, S.; Vel, S.; Gasche, C. Clinical significance of C-reactive protein levels in predicting responsiveness to iron therapy in patients with inflammatory bowel disease and iron deficiency anemia. Dig. Dis. Sci. 2015, 60, 1375–1381. [Google Scholar] [CrossRef] [PubMed]
- Kooistra, M.P.; Niemantsverdriet, E.C.; van Es, A.; Mol-Beermann, N.M.; Struyvenberg, A.; Marx, J.J. Iron absorption in erythropoietin-treated haemodialysis patients: Effects of iron availability, inflammation and aluminium. Nephrol. Dial. Transplant. 1998, 13, 82–88. [Google Scholar] [CrossRef]
- Argilés, J.M.; Busquets, S.; Felipe, A.; López-Soriano, F.J. Molecular mechanisms involved in muscle wasting in cancer and ageing: Cachexia versus sarcopenia. Int. J. Biochem. Cell Biol. 2005, 37, 1084–1104. [Google Scholar] [CrossRef]
- Morley, J.E.; Thomas, D.R.; Wilson, M.M. Cachexia: Pathophysiology and clinical relevance. Am. J. Clin. Nutr. 2006, 83, 735–743. [Google Scholar] [CrossRef]
- Ali, S.; Garcia, J.M. Sarcopenia, cachexia and aging: Diagnosis, mechanisms and therapeutic options—A mini-review. Gerontology 2014, 60, 294–305. [Google Scholar] [CrossRef]
- Bowen, T.S.; Schuler, G.; Adams, V. Skeletal muscle wasting in cachexia and sarcopenia: Molecular pathophysiology and impact of exercise training. J. Cachexia Sarcopenia Muscle 2015, 6, 197–207. [Google Scholar] [CrossRef] [PubMed]
- Evans, W.J. Skeletal muscle loss: Cachexia, sarcopenia, and inactivity. Am. J. Clin. Nutr. 2010, 91, 1123s–1127s. [Google Scholar] [CrossRef]
- Beaudart, C.; Dawson, A.; Shaw, S.C.; Harvey, N.C.; Kanis, J.A.; Binkley, N.; Reginster, J.Y.; Chapurlat, R.; Chan, D.C.; Bruyère, O.; et al. Nutrition and physical activity in the prevention and treatment of sarcopenia: Systematic review. Osteoporos. Int. 2017, 28, 1817–1833. [Google Scholar] [CrossRef] [PubMed]
- Bianchi, V.E. Role of nutrition on anemia in elderly. Clin. Nutr. ESPEN 2016, 11, e1–e11. [Google Scholar] [CrossRef] [PubMed]
- Kalra, P.R.; Bolger, A.P.; Francis, D.P.; Genth-Zotz, S.; Sharma, R.; Ponikowski, P.P.; Poole-Wilson, P.A.; Coats, A.J.; Anker, S.D. Effect of anemia on exercise tolerance in chronic heart failure in men. Am. J. Cardiol. 2003, 91, 888–891. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.J.; Latham, N.K. Progressive resistance strength training for improving physical function in older adults. Cochrane Database Syst. Rev. 2009, 2009, CD002759. [Google Scholar] [CrossRef]
- Denison, H.J.; Cooper, C.; Sayer, A.A.; Robinson, S.M. Prevention and optimal management of sarcopenia: A review of combined exercise and nutrition interventions to improve muscle outcomes in older people. Clin. Interv. Aging 2015, 10, 859–869. [Google Scholar] [CrossRef] [PubMed]
- Robinson, S.; Cooper, C.; Aihie Sayer, A. Nutrition and sarcopenia: A review of the evidence and implications for preventive strategies. J. Aging Res. 2012, 2012, 510801. [Google Scholar] [CrossRef]
| Variables | Men | Women | ||||
|---|---|---|---|---|---|---|
| Anemia (n = 104) | Normal (n = 1079) | p | Anemia (n = 244) | Normal (n = 1396) | p | |
| Age (y) | 73.13 ± 0.54 | 71.31 ± 0.16 | 0.001 | 74.45 ± 0.34 | 71.94 ± 0.16 | <0.0001 |
| Sarcopenia, % (n) | 62.4 (67) | 37.7 (408) | <0.0001 | 46.9 (107) | 37.2 (511) | 0.030 |
| Weight (kg) | 58.07 ± 1.11 | 63.44 ± 0.34 | <0.0001 | 52.26 ± 0.74 | 55.26 ± 0.31 | <0.0001 |
| Height (cm) | 163.49 ± 0.75 | 165.02 ± 0.20 | 0.049 | 149.94 ± 0.49 | 150.86 ± 0.19 | 0.077 |
| BMI (kg/m2) | 21.65 ± 0.33 | 23.25 ± 0.11 | <0.0001 | 23.19 ± 0.27 | 24.24 ± 0.12 | <0.0001 |
| Education level, (%) (low/high) | 81.1/18.9 | 75.3/24.7 | 0.049 | 20.7/79.3 | 18.3/81.7 | 0.031 |
| Smoking status, (%) (current-/ex-/nonsmoker) | 50.7/30.6/18.7 | 57.6/27.8/14.5 | 0.375 | 10.2/0.4/89.4 | 9.9/2.3/87.9 | 0.290 |
| Drinking status (%) (current-/nondrinking) | 65.7/34.3 | 72.0/28.0 | 0.215 | 25.1/74.9 | 38.4/61.6 | <0.0001 |
| Marital status, (%) (living with spouse) | 91.4 | 91.4 | 0.989 | 62.0 | 53.2 | 0.030 |
| Income (individual) | 0.025 | 0.623 | ||||
| Q1 (lowest) | 21.0 | 25.0 | 20.8 | 25.1 | ||
| Q2 | 18.2 | 25.9 | 27.7 | 24.7 | ||
| Q3 | 37.5 | 23.5 | 26.1 | 25.0 | ||
| Q4 (highest) | 23.3 | 25.7 | 25.5 | 25.2 | ||
| Resistance exercise | 0.525 | 0.549 | ||||
| Never | 79.3 | 73.8 | 93.9 | 93.2 | ||
| 1–3 days/wk. | 10.0 | 11.9 | 2.5 | 3.8 | ||
| ≥4 days/wk. | 10.6 | 14.2 | 3.6 | 2.9 | ||
| Aerobic exercise (TWT) | 69.59 ± 9.23 | 64.79 ± 3.10 | 0.632 | 68.98 ± 6.74 | 65.40 ± 3.01 | 0.614 |
| Fasting glucose (mg/dL) | 104.34 ± 2.73 | 103.67 ± 0.83 | 0.891 | 101.98 ± 1.75 | 104.45 ± 0.85 | 0.194 |
| Total cholesterol | 164.57 ± 3.25 | 184.52 ± 1.18 | <0.0001 | 191.41 ± 2.24 | 203.98 ± 1.21 | <0.0001 |
| HDL-C | 43.73 ± 1.25 | 45.38 ± 0.45 | 0.213 | 44.05 ± 0.74 | 46.79 ± 0.37 | <0.0001 |
| Triglyceride | 106.08 ± 7.13 | 145.08 ± 3.37 | <0.0001 | 131.34 ± 5.63 | 152.33 ± 3.29 | 0.002 |
| Systolic BP (mmHg) | 127.76 ± 1.78 | 130.68 ± 0.73 | 0.130 | 133.41 ± 1.51 | 132.80 ± 0.62 | 0.701 |
| Diastolic BP (mmHg) | 72.79 ± 1.06 | 77.73 ± 0.38 | <0.0001 | 73.40 ± 0.74 | 77.16 ± 0.35 | <0.0001 |
| Waist circumference (cm) | 80.09 ± 1.17 | 85.04 ± 0.32 | <0.0001 | 80.61 ± 0.79 | 83.75 ± 0.34 | <0.0001 |
| High fasting glucose a | 48.4 | 43,8 | 0.419 | 51.6 | 56.2 | 0.577 |
| Abdominal obesity b | 19.2 | 29.8 | 0.039 | 33.3 | 44.8 | 0.008 |
| High triglyceride c | 16.0 | 34.9 | 0.001 | 29.3 | 39.6 | 0.009 |
| High blood pressure d | 48.1 | 53.4 | 0.347 | 56.1 | 59.7 | 0.394 |
| Low HDL-C e | 48.0 | 37.0 | 0.037 | 72.3 | 66.6 | 0.121 |
| 25(OH)D (ng/mL) | 21.65 ± 1.04 | 21.84 ± 0.35 | 0.852 | 18.67 ± 0.57 | 18.62 ± 0.30 | 0.963 |
| Energy intake (kcal) | 1797.47 ± 65.17 | 1930.00 ± 28.30 | 0.053 | 1372.82 ± 39.60 | 1436.40 ± 16.77 | 0.143 |
| Carbohydrate intake (g) | 326.14 ± 11.43 | 334.51 ± 5.16 | 0.486 | 266.75 ± 7.91 | 276.54 ± 3.36 | 0.264 |
| Protein intake (g) | 58.94 ± 2.95 | 64.53 ± 1.27 | 0.790 | 42.51 ± 1.49 | 44.90 ± 0.72 | 0.145 |
| Fat intake (g) | 23.07 ± 1.47 | 27.79 ± 0.77 | 0.004 | 15.44 ± 0.80 | 17.47 ± 0.43 | 0.024 |
| Iron intake (mg) | 14.52 ± 1.29 | 15.77 ± 0.62 | 0.376 | 11.74 ± 1.10 | 12.056 ± 0.53 | 0.798 |
| ASM (kg) | 18.809 ± 0.29 | 19.75 ± 0.11 | <0.0001 | 13.16 ± 0.16 | 13.51 ± 0.07 | 0.030 |
| SMI (kg/m2) | 6.75 ± 0.08 | 7.23 ± 0.03 | <0.0001 | 5.84 ± 0.06 | 5.92 ± 0.02 | 0.166 |
| Variables | Men | Women | ||||
|---|---|---|---|---|---|---|
| Sarcopenia (n = 475) | Normal (n = 708) | p | Sarcopenia (n = 618) | Normal (n = 1022) | p | |
| Age (y) | 72.85 ± 0.25 | 70.71 ± 0.20 | <0.0001 | 73.18 ± 0.25 | 71.79 ± 0.18 | <0.0001 |
| Sarcopenia, % (n) | 12.8 (67) | 5.1 (37) | <0.0001 | 18.8 (107) | 13.4 (137) | 0.030 |
| Weight (kg) | 56.89 ± 0.41 | 67.03 ± 0.36 | <0.0001 | 50.08 ± 0.36 | 57.78 ± 0.33 | <0.0001 |
| Height (cm) | 164.16 ± 0.30 | 165.39 ± 0.25 | 0.002 | 150.32 ± 0.31 | 150.96 ± 0.21 | 0.079 |
| BMI (kg/m2) | 21.08 ± 0.13 | 24.47 ± 0.11 | <0.0001 | 22.13 ± 0.13 | 25.30 ± 0.12 | <0.0001 |
| Education level, (%) (low/high) | 77.1/22.9 | 75.4/24.6 | 0.402 | 22.7/77.3 | 18.7/81.3 | <0.0001 |
| Smoking status, (%) (current-/ex-/nonsmoker) | 59.3/26.8/13.9 | 55.6/28.9/15.5 | 0.542 | 13.0/1.4/85.7 | 8.0/2.4/89.7 | 0.012 |
| Drinking status (%) (current-/nondrinking) | 67.6/32.4 | 74.0/26.0 | 0.033 | 35.2/64.8 | 37.1/62.9 | 0.546 |
| Marital status, (%) (living with spouse) | 89.6 | 92.7 | 0.119 | 41.5 | 47.9 | 0.032 |
| Income (individual) | 0.020 | 0.731 | ||||
| Q1 (lowest) | 23.5 | 25.4 | 23.0 | 25.4 | ||
| Q2 | 30.9 | 21.5 | 25.7 | 24.9 | ||
| Q3 | 22.4 | 26.1 | 24.7 | 25.4 | ||
| Q4 (highest) | 23.1 | 27.0 | 26.6 | 24.4 | ||
| Resistance exercise | 0.028 | 0.526 | ||||
| Never | 79.3 | 71.0 | 94.1 | 92.9 | ||
| 1–3 days/wk. | 9.1 | 13.6 | 3.5 | 3.7 | ||
| ≥4 days/wk. | 11.7 | 14.5 | 2.4 | 3.4 | ||
| Aerobic exercise (TWT) | 74.30 ± 4.81 | 59.16 ± 3.65 | 0.014 | 70.89 ± 4.36 | 62.83 ± 3.71 | 0.157 |
| Fasting glucose (mg/dL) | 103.45 ± 1.22 | 103.91 ± 1.02 | 0.769 | 102.40 ± 1.28 | 105.12 ± 0.94 | 0.078 |
| Total cholesterol | 180.53 ± 1.90 | 184.45 ± 1.46 | 0.102 | 204.21 ± 1.80 | 200.67 ± 1.33 | 0.110 |
| HDL-C | 46.91 ± 0.63 | 44.16 ± 0.50 | <0.0001 | 47.18 ± 0.56 | 45.85 ± 0.42 | 0.053 |
| Triglyceride | 139.29 ± 4.91 | 143.62 ± 3.91 | 0.466 | 147.29 ± 3.90 | 150.21 ± 3.71 | 0.561 |
| Systolic BP (mmHg) | 130.01 ± 1.13 | 130.78 ± 0.80 | 0.586 | 132.34 ± 0.93 | 133.24 ± 0.72 | 0.421 |
| Diastolic BP (mmHg) | 76.64 ± 0.60 | 77.79 ± 0.44 | 0.109 | 75.38 ± 0.49 | 77.33 ± 0.44 | 0.002 |
| Waist circumference (cm) | 79.78 ± 0.49 | 87.84 ± 0.33 | <0.0001 | 79.03 ± 0.42 | 85.93 ± 0.36 | <0.0001 |
| High fasting glucose a | 41.7 | 45.8 | 0.216 | 41.5 | 45.3 | 0.223 |
| Abdominal obesity b | 12.6 | 39.8 | <0.0001 | 23.3 | 54.4 | <0.0001 |
| High triglyceride c | 23.4 | 34.0 | 0.646 | 37.6 | 38.3 | 0.819 |
| High blood pressure d | 51.7 | 53.8 | 0.583 | 57.3 | 60.3 | 0.331 |
| Low HDL-C e | 32.4 | 41.6 | 0.007 | 67.6 | 58.3 | 0.063 |
| 25(OH)D (ng/mL) | 21.27 ± 0.45 | 22.19 ± 0.45 | 0.098 | 18.15 ± 0.40 | 18.93 ± 0.35 | 0.103 |
| Energy intake (kcal) | 1778.95 ± 37.35 | 2011.69 ± 31.45 | <0.0001 | 1345.73 ± 23.82 | 1477.60 ± 19.29 | <0.0001 |
| Carbohydrate intake (g) | 314.47 ± 6.35 | 346.58 ± 5.89 | <0.0001 | 259.04 ± 4.69 | 285.12 ± 3.90 | 0.001 |
| Protein intake (g) | 58.72 ± 1.76 | 67.60 ± 1.41 | <0.0001 | 41.79 ± 1.00 | 46.25 ± 0.84 | 0.001 |
| Fat intake (g) | 23.76 ± 1.00 | 29.81 ± 0.96 | <0.0001 | 16.38 ± 0.60 | 17.64 ± 0.50 | 0.102 |
| Iron intake (mg) | 14.87 ± 0.63 | 16.19 ± 0.61 | 0.241 | 10.08 ± 0.37 | 13.22 ± 0.73 | <0.0001 |
| ASM (kg) | 17.34 ± 0.10 | 11.94 ± 0.07 | <0.0001 | 11.94 ± 0.07 | 14.41 ± 0.06 | <0.0001 |
| SMI (kg/m2) | 6.42 ± 0.03 | 7.70 ± 0.02 | <0.0001 | 5.28 ± 0.02 | 6.31 ± 0.02 | <0.0001 |
| Model | Sarcopenia | OR (95% CI) | p |
|---|---|---|---|
| Model 1 | Total | 1.805 (1.364–2.388) | <0.0001 |
| Men | 2.746 (1.740–4.334) | <0.0001 | |
| Women | 1.494 (1.045–2.138) | 0.028 | |
| Model 2 | Total | 1.631 (1.228–2.166) | 0.001 |
| Men | 2.514 (1.585–3.988) | <0.0001 | |
| Women | 1.376 (0.950–1.992) | 0.091 | |
| Model 3 | Total | 1.503 (1.098–2.058) | 0.011 |
| Men | 2.777 (1.545–4.991) | 0.001 | |
| Women | 1.221 (0.833–1.788) | 0.305 | |
| Model 4 | Total | 1.455 (1.064–1.989) | 0.019 |
| Men | 2.649 (1.475–4.755) | 0.001 | |
| Women | 1.216 (0.827–1.788) | 0.320 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, D.-Y.; Shin, S. Sarcopenia and Anemia in Elderly Koreans: A Nationwide Population-Based Study. Healthcare 2023, 11, 2428. https://doi.org/10.3390/healthcare11172428
Lee D-Y, Shin S. Sarcopenia and Anemia in Elderly Koreans: A Nationwide Population-Based Study. Healthcare. 2023; 11(17):2428. https://doi.org/10.3390/healthcare11172428
Chicago/Turabian StyleLee, Do-Youn, and Sunghoon Shin. 2023. "Sarcopenia and Anemia in Elderly Koreans: A Nationwide Population-Based Study" Healthcare 11, no. 17: 2428. https://doi.org/10.3390/healthcare11172428
APA StyleLee, D.-Y., & Shin, S. (2023). Sarcopenia and Anemia in Elderly Koreans: A Nationwide Population-Based Study. Healthcare, 11(17), 2428. https://doi.org/10.3390/healthcare11172428







