The Risk Factors of Chronic Pain in Victims of Violence: A Scoping Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Criteria for Selection of Studies
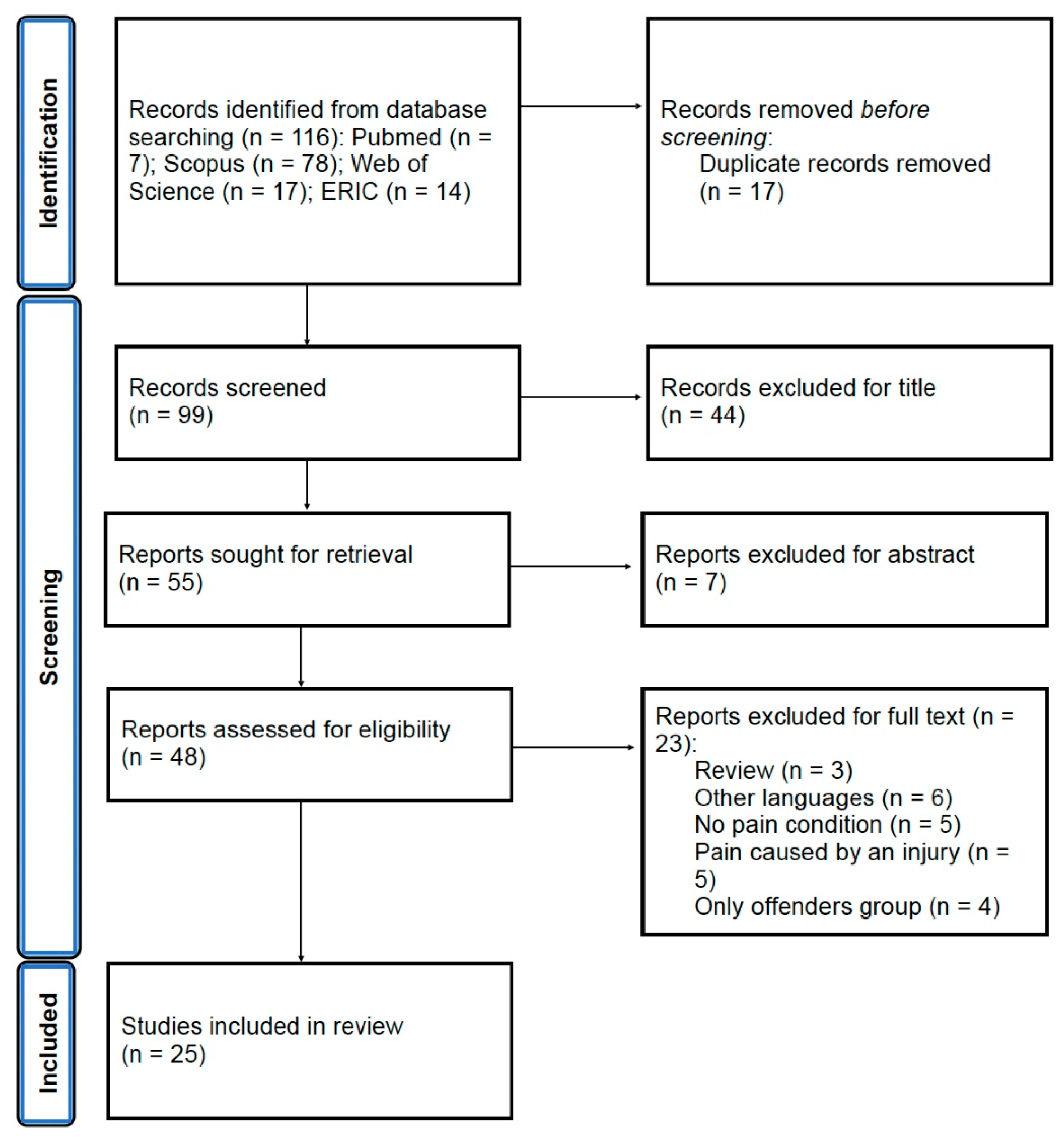
2.3. Study Selection and Data Extraction
2.4. Assessment of Study Quality
3. Results
3.1. Literature Identification, Study Characteristics, and Quality
3.2. Risk Factors
3.3. The Impact of Risk Factors in the Studies
3.3.1. Biological Risk Factors
3.3.2. Psycho-Social Risk Factors
4. Discussion
4.1. The Most Common Conditions
4.2. Other Conditions
4.3. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sachs-Ericsson, N.; Blazer, D.; Plant, E.A.; Arnow, B. Childhood sexual and physical abuse and the 1-year prevalence of medical problems in the National Comorbidity Survey. Health Psychol. 2005, 24, 32–40. [Google Scholar] [CrossRef] [PubMed]
- Danese, A.; Moffitt, T.E.; Harrington, H.; Milne, B.J.; Polanczyk, G.; Pariante, C.M.; Poulton, R.; Caspi, A. Adverse childhood experiences and adult risk factors for age-related disease: Depression, inflammation, and clustering of metabolic risk markers. Arch. Pediatr. Adolesc. 2009, 163, 1135–1143. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Moreno, C.; Heise, L.; Jansen, H.A.; Ellsberg, M.; Watts, C. Public health. Violence against women. Science 2005, 310, 1282–1283. [Google Scholar] [CrossRef] [PubMed]
- Gilbert, R.; Spatz Widom, C.; Browne, K.; Fergusson, D.; Webb, E.; Janson, S. Burden and consequences of child maltreatment in high-income countries. Lancet 2009, 373, 68–81. [Google Scholar] [CrossRef]
- World Health Organization. World Report on Violence and Health. Available online: https://www.who.int/publications/i/item/9241545615 (accessed on 3 October 2022).
- Graham-Bermann, S.A. Child abuse in the context of domestic violence. In The APSAC Handbook on Child Maltreatment; Myers, J.E.B., Berliner, L., Briere, J., Hendrix, C.T., Jenny, C., Reid, T.A., Eds.; Sage Publications: Thousand Oakes, CA, USA, 2002; Volume 1, pp. 119–130. [Google Scholar]
- Kwon, M.; You, S. Gender and role associations between domestic violence during childhood and dating violence: Victimization among male college students mediated through violence justification beliefs. Child. Abuse Negl. 2023, 141, 106233. [Google Scholar] [CrossRef]
- Cirici, A.R.; Soler, A.R.; Cobo, J.; Soldevilla, A.J.M. Psychological consequences and daily life adjustment for victims of intimate partner violence. Int. J. Psychiatry Med. 2023, 58, 6–19. [Google Scholar] [CrossRef]
- Bussieres, A.; Hartvigsen, J.; Ferreira, M.L.; Ferreira, P.H.; Hancock, M.J.; Stone, L.S.; Wideman, T.H.; Boruff, J.; Elklit, A. Adverse childhood experience and adult persistent pain and disability: Protocol for a systematic review and meta-analysis. Syst. Rev. 2020, 9, 215. [Google Scholar] [CrossRef]
- Uvelli, A.; Ribaudo, C.; Gualtieri, G.; Coluccia, A.; Ferretti, F. The association between violence against women and chronic pain: A systematic review and meta-analysis. Res. Sq. 2023. under review. [Google Scholar] [CrossRef]
- Campbell, J.C. Health consequences of intimate partner violence. Lancet 2002, 359, 1331–1336. [Google Scholar] [CrossRef]
- Sutherland, C.A.; Bybee, D.I.; Sullivan, C.M. Beyond bruises and broken bones: The joint effects of stress and injuries on battered women’s health. Am. J. Community Psychol. 2002, 30, 609–636. [Google Scholar] [CrossRef]
- As-Sanie, S.; Clevenger, L.A.; Geisser, M.E.; Williams, D.A.; Roth, R.S. History of abuse and its relationship to pain experience and depression in women with chronic pelvic pain. Am. J. Obstet. Gynecol. 2014, 210, 317.e1–317.e8. [Google Scholar] [CrossRef]
- Chandan, J.S.; Thomas, T.; Raza, K.; Bradbury-Jones, C.; Taylor, J.; Bandyopadhyay, S.; Nirantharakumar, K. Intimate partner violence and the risk of developing fibromyalgia and chronic fatigue syndrome. J. Interpers. Violence 2021, 36, NP12279–NP12298. [Google Scholar] [CrossRef] [PubMed]
- Ringel, Y.; Whitehead, W.E.; Toner, B.B.; Diamant, N.E.; Hu, Y.; Jia, H.; Bangdiwala, S.I.; Drossman, D.A. Sexual and physical abuse are not associated with rectal hypersensitivity in patients with irritable bowel syndrome. Gut 2004, 53, 838–842. [Google Scholar] [CrossRef]
- Bo, M.; Canavese, A.; Magnano, L.; Rondana, A.; Castagna, P.; Gino, S. Violence against pregnant women in the experience of the rape centre of Turin: Clinical and forensic evaluation. J. Forensic Leg. Med. 2020, 76, 102071. [Google Scholar] [CrossRef]
- Cripe, S.M.; Sanchez, S.E.; Gelaye, B.; Sanchez, E.; Williams, M.A. Association between intimate partner violence, migraine, and probable migraine. Headache 2011, 51, 208–219. [Google Scholar] [CrossRef] [PubMed]
- Wuest, J.; Merritt-Gray, M.; Ford-Gilboe, M.; Lent, B.; Varcoe, C.; Campbell, J.C. Chronic pain in women survivors of intimate partner violence. J. Pain 2008, 9, 1049–1057. [Google Scholar] [CrossRef] [PubMed]
- Coll-Vinent, B.; Marti, G.; Calderon, S.; Martinez, B.; Cespedes, F.; Fuenzalida, C. La violencia de pareja en las pacientes que consultan pr dolor toracico en urgencias. Semergen 2018, 45, 23–29. [Google Scholar] [CrossRef]
- Shields, L.B.; Corey, T.S.; Weakley-Jones, B.; Stewart, D. Living victims of strangulation: A 10-year review of cases in a metropolitan community. Am. J. Forensic Med. Pathol. 2010, 31, 320–325. [Google Scholar] [CrossRef]
- .Melzack, R. Phantom limbs and the concept of a neuromatrix. Trends Neurosci. 1990, 13, 88–92. [Google Scholar] [CrossRef]
- Baliki, M.N.; Apkarian, A.V. Nociception, pain, negative moods, and behavior selection. Neuron 2015, 87, 474–491. [Google Scholar] [CrossRef]
- Garcia-Larrea, L.; Peyron, R. Pain matrices and neuropathic pain matrices: A review. Pain 2013, 154, S29–S43. [Google Scholar] [CrossRef]
- Raphael, K.G.; Janal, M.N.; Nayak, S.; Schwartz, J.E.; Gallagher, R.M. Psychiatric comorbidities in a community sample of women with fibromyalgia. Pain 2006, 124, 117–125. [Google Scholar] [CrossRef] [PubMed]
- Uguz, F.; Cicek, E.; Salli, A.; Karahan, A.Y.; Albayrak, I.; Kaya, N.; Ugurlu, H. Axis I and Axis II psychiatric disorders in patients with fibromyalgia. Gen. Hosp. Psychiatry 2010, 32, 105–107. [Google Scholar] [CrossRef] [PubMed]
- Kudlow, P.A.; Rosenblat, J.D.; Weissman, C.R.; Cha, D.S.; Kakar, R.; McIntyre, R.S.; Sharma, V. Prevalence of fibromyalgia and co-morbid bipolar disorder: A systematic review and meta-analysis. J. Affect. Disord. 2015, 188, 134–142. [Google Scholar] [CrossRef] [PubMed]
- Carroll, L.J.; Cassidy, J.D.; Cote, P. Factors associated with the onset of an episode of depressive symptoms in the general population. J. Clin. Epidemiol. 2003, 56, 651–658. [Google Scholar] [CrossRef] [PubMed]
- Currie, S.R.; Wang, J. Chronic back pain and major depression in the general Canadian population. Pain 2004, 107, 54–60. [Google Scholar] [CrossRef] [PubMed]
- Carroll, L.J.; Cassidy, J.D.; Cote, P. Depression as a risk factor for onset of an episode of troublesome neck and low back pain. Pain 2004, 107, 134–139. [Google Scholar] [CrossRef]
- Currie, S.R.; Wang, J. More data on major depression as an antecedent risk factors for first onset of chronic back pain. Psychol. Med. 2005, 35, 1275–1282. [Google Scholar] [CrossRef]
- Von Korff, M.; Crane, P.; Lane, M.; Miglioretti, D.L.; Simon, G.; Saunders, K.; Stang, P.; Brandenburg, N.; Kessler, R. Chronic spinal pain and physical-mental comorbidity in the United States: Results from the national comorbidity survey replication. Pain 2005, 113, 331–339. [Google Scholar] [CrossRef]
- Stang, P.E.; Brandenburg, N.A.; Lane, M.C.; Merikangas, K.R.; Von Korff, M.R.; Kessler, R.C. Mental and physical comorbid conditions and days in role among persons with arthritis. Psychosom. Med. 2006, 68, 152–158. [Google Scholar] [CrossRef]
- Demyttenaere, K.; Bruffaerts, R.; Lee, S.; Posada-Villa, J.; Kovess, V.; Angermeyer, M.C.; Levinson, D.; de Girolamo, G.; Nakane, H.; Mneimneh, Z.; et al. Mental disorders among persons with chronic back or neck pain: Results from the World Mental Health Survey. Pain 2007, 129, 332–342. [Google Scholar] [CrossRef]
- Arnold, L.M.; Hudson, J.I.; Keck, P.E.; Auchenbach, M.B.; Javaras, K.N.; Hess, E.V. Comorbidity of fibromyalgia and psychiatric disorders. J. Clin. Psychiatry 2006, 67, 1219–1225. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Liu, J.; Zhao, Y.; Thethi, T.; Fonseca, V.; Shi, L. Predictors of duloxetine versus other treatments among veterans with diabetic peripheral neuropathic pain: A retrospective study. Pain Pract. 2012, 12, 366–373. [Google Scholar] [CrossRef] [PubMed]
- Alonso-Moran, E.; Orueta, J.F.; Fraile Esteban, J.I.; Arteagoitia Axpe, J.M.; Marques Gonzalez, M.L.; Toro Polanco, N.; Ezkurra Loiola, P.; Gaztambide, S.; Nuno-Solinis, R. The prevalence of diabetes-related complications and multimorbidity in the population with type 2 diabetes mellitus in the Basque Country. BMC Public Health 2014, 14, 1059. [Google Scholar] [CrossRef] [PubMed]
- Cheatle, M.D.; Wasser, T.; Foster, C.; Olugbodi, A.; Bryan, J. Prevalence of suicidal ideation in patients with chronic non-cancer pain referred to a behaviorally based pain program. Pain Physician 2014, 17, E359–E367. [Google Scholar] [CrossRef]
- Trinanes, Y.; Gonzalez-Villar, A.; Gomez-Perretta, C.; Carrillo-de-la-Pena, M.T. Suicidality in chronic pain: Predictors of suicidal ideation in fibromyalgia. Pain Pract. 2015, 15, 323–332. [Google Scholar] [CrossRef] [PubMed]
- Chapman, C.R.; Tuckett, R.P.; Woo Song, C. Pain and stress in systems perspective: Reciprocal neural, endocrine and immune interactions. J. Pain 2008, 9, 122–145. [Google Scholar] [CrossRef]
- Blalock, J.E. The syntax of immune-neuroendocrine communication. Immunol. Today 1994, 15, 504–511. [Google Scholar] [CrossRef]
- Moreno-Ramos, O.A.; Lattig, M.C.; Barrios, A.F.G. Modeling of the hypothalamic-pituitary-adrenal axis-mediated interaction between the serotonin regulation pathway and the stress response using a Boolean Approximation: A novel study of depression. Theor. Biol. Med. Model. 2013, 10, 59. [Google Scholar] [CrossRef]
- Kendall-Tackett, K.; Marshall, A.R.; Ness, K.E. Victimization, healthcare use, and health maintenance. Fam. Viol. Sex. Assault Bull. 2000, 16, 18–21. [Google Scholar]
- Engel, G.L. The need for a new medical model: A challenge for biomedicine. Science 1977, 196, 129–136. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.; Horsley, T.; Weeks, L. Prisma extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0; The Cochrane Collaboration: London, UK, 2011. [Google Scholar]
- Horsley, S.; Dingwall, O.; Sampson, M. Checking reference lists to find additional studies for systematic reviews. Cochrane Database Syst. Rev. 2011, 8, MR000026. [Google Scholar] [CrossRef] [PubMed]
- Beynon, R.; Leeflang, M.M.G.; McDonald, S.; Eisinga, A.; Mitchell, R.L.; Whiting, P.; Glanville, J.M. Search strategies to identify diagnostic accuracy studies in MEDLINE and EMBASE. Cochrane Database Syst. Rev. 2013, 9, MR000022. [Google Scholar] [CrossRef] [PubMed]
- Moola, S.; Munn, Z.; Tufanaru, C.; Aromataris, E.; Sears, K.; Sfetc, R. Systematic reviews of etiology and risk. In JBI Manual for Evidence Synthesis; Aromataris., E., Munn, Z., Eds.; JBI: Adelaide, Australia, 2020; Available online: https://synthesismanual.jbi.global (accessed on 1 March 2023).
- Parish, W.L.; Wang, T.; Laumann, E.O.; Pan, S.; Luo, Y. Intimate partner violence in China: National prevalence, risk factors and associated health problems. Int. Fam. Plan Perspect. 2004, 30, 174–181. [Google Scholar] [CrossRef] [PubMed]
- Bonomi, A.E.; Anderson, M.L.; Rivara, F.P.; Thompson, R.S. Health outcomes in women with physical and sexual intimate partner violence exposure. J. Womens Health 2007, 16, 987–997. [Google Scholar] [CrossRef] [PubMed]
- Hegarty, K.; Gunn, J.; Chondros, P.; Taft, A. Physical and social predictors of partner abuse in women attending general practice: A cross-sectional study. Br. J. Gen. Pract. 2008, 58, 484–487. [Google Scholar] [CrossRef]
- Chartier, M.J.; Walker, J.R.; Naimark, B. Separate and cumulative effects of adverse childhood experiences in predicting adult health and health care utilization. Child. Abuse Negl. 2010, 34, 454–464. [Google Scholar] [CrossRef]
- Vives-Cases, C.; Ruiz-Cantero, M.T.; Escriba-Aguir, V.; Miralles, J.J. The effect of intimate partner violence and other forms of violence against women on health. J. Public Health 2011, 33, 15–21. [Google Scholar] [CrossRef]
- Williams, C.; Larsen, U.; McCloskey, L.A. The impact of childhood sexual abuse and intimate partner violence on sexually transmitted infections. Violence Vict. 2010, 25, 787–798. [Google Scholar] [CrossRef]
- Eslick, G.D.; Koloski, N.A.; Talley, N.J. Sexual, physical, verbal/emotional abuse and unexplained chest pain. Child. Abuse Negl. 2011, 35, 601–605. [Google Scholar] [CrossRef]
- Kelly, U.A.; Skelton, K.; Patel, M.; Bradley, B. More than military sexual trauma: Interpersonal violence, PTSD, and mental health in women veterans. Res. Nurs. Health 2011, 34, 457–467. [Google Scholar] [CrossRef] [PubMed]
- Young, R.A.; Benold, T.; Whitham, J.; Burge, S. Factors influencing work interference in patients with chronic low back pain: A Residency Research Network of Texas (RRNet) study. J. Am. Board. Fam. Med. 2011, 24, 503–510. [Google Scholar] [CrossRef] [PubMed]
- Gerber, M.R.; Fried, L.E.; Pineles, S.L.; Shipherd, J.C.; Bernstein, C.A. Posttraumatic stress disorder and intimate partner violence in a women’s headache center. Women Health 2012, 52, 454–471. [Google Scholar] [CrossRef]
- Saito, A.; Creedy, D.; Cooke, M.; Chaboyer, W. Effect of intimate partner violence on antenatal functional health status of childbearing women in Northeastern Thailand. Health Care Women Int. 2013, 34, 757–774. [Google Scholar] [CrossRef] [PubMed]
- Sutherland, M.A.; Fantasia, H.D.; McClain, N. Abuse experiences, substance use, and reproductive health in women seeking care at an emergency department. J. Emerg. Nurs. 2013, 39, 326–333. [Google Scholar] [CrossRef]
- Gelaye, B.; Do, N.; Avila, S.; Velez, J.C.; Zhong, Q.Y.; Sanchez, S.E.; Peterlin, B.L.; Williams, M.A. Childhood abuse, intimate partner violence and risk of migraine among pregnant women: An epidemiologic study. Headache 2016, 56, 976–986. [Google Scholar] [CrossRef]
- Halpern, L.R.; Shealer, M.L.; Cho, R.; McMichael, E.B.; Rogers, J.; Ferguson-Young, D.; Mouton, C.P.; Tabatabai, M.; Southerland, P.G.; Gangula, P. Influence of intimate partner violence (IPV) exposure on cardiovascular and salivary biosensors: Is there a relationship? J. Natl. Med. Assoc. 2017, 109, 252–261. [Google Scholar] [CrossRef]
- Lutgendorf, M.A.; Snipes, M.A.; O’Boyle, A.L. Prevalence and predictors of intimate partner violence in a military urogynecology clinic. Mil. Med. 2017, 182, e1634–e1638. [Google Scholar] [CrossRef][Green Version]
- England-Mason, G.; Casey, R.; Ferro, M.; MacMillan, H.L.; Tonmyr, L.; Gonzalez, A. Child maltreatment and adult multimorbidity: Results from the Canadian Community Health Survey. Can. J. Public. Health 2018, 109, 561–572. [Google Scholar] [CrossRef]
- Grossi, P.K.; Bueno, C.H.; de Abreu Silva, M.A.; Pellizzer, E.P.; Grossi, M.L. Evaluation of sexual, physical, and emotional abuse in women diagnosed with temporomandibular disorders: A case-control study. Int. J. Prosthodont. 2018, 31, 543–551. [Google Scholar] [CrossRef]
- Gucek, N.K.; Selic, P. Depression in intimate partner violence victims in Slovenia: A crippling pattern of factors identified in family practice attendees. Int. J. Environ. Res. Public Health 2018, 15, 210. [Google Scholar] [CrossRef] [PubMed]
- Gunduz, N.; Erzican, E.; Polat, A. The relationship of intimate partner violence with psychiatric disorders and severity of pain among female patients with fibromyalgia. Arch. Rheumatol. 2019, 34, 245–252. [Google Scholar] [CrossRef] [PubMed]
- Jovanovic, V.M.; Cankovic, S.; Milijasevic, D.; Ukropina, S.; Jovanovic, M.; Cankovic, D. Health consequences of domestic violence against women in Serbia. Vojnosanit. Pregl. 2020, 77, 14–21. [Google Scholar] [CrossRef]
- Ali, T.S.; Sami, N.; Saeed, A.A.; Ali, P. Gynaecological morbidities among married women and husband’s behaviour: Evidence from a community-based study. Nurs. Open 2021, 8, 553–561. [Google Scholar] [CrossRef] [PubMed]
- Al Kendi, A.; Al Shidhani, N.; Al Kiyumi, M. Domestic violence among Omani women: Prevalence, risk factors and help-seeking behaviour. East. Mediterr. Health J. 2021, 27, 242–249. [Google Scholar] [CrossRef] [PubMed]
- De Wet-Billings, N.; Godongwana, M. Exposure to intimate partner violence and hypertension outcomes among young women in South Africa. Int. J. Hypertens. 2021, 2021, 5519356. [Google Scholar] [CrossRef]
- FitzPatrick, K.M.; Brown, S.; Hegarty, K.; Mensah, F.; Gartland, D. Physical and emotional intimate partner violence and women’s health in the first year after childbirth: An Australian pregnancy cohort study. J. Interpers. Violence 2022, 37, NP2147–NP2176. [Google Scholar] [CrossRef]
- Raphael, E.; Van Den Eeden, S.K.; Gibson, C.J.; Tonner, C.; Thom, D.H.; Subak, L.; Huang, A.J. Interpersonal violence and painful bladder symptoms in community-dwelling midlife to older women. Am. J. Obstet. Gynecol. 2022, 226, 230.e1–230.e10. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, 71. [Google Scholar] [CrossRef]
- Hassam, T.; Kelso, E.; Chowdary, P.; Yisma, E.; Mol, B.W.; Han, A. Sexual assault as a risk factor for gynaecological morbidity: An exploratory systematic review and meta-analysis. Eur. J. Obstet. Gynecol. Reprod. Biol. 2020, 255, 222–230. [Google Scholar] [CrossRef]
- Matthews, K.A.; Woodall, K.L.; Allen, M.T. Cardiovascular reactivity to stress predicts future blood pressure status. Hypertension 1993, 22, 479–485. [Google Scholar] [CrossRef] [PubMed]
- Turner, A.I.; Smyth, N.; Hall, S.J.; Torres, S.J.; Hussein, M.; Jayasinghe, S.U.; Ball, K.; Clow, A.J. Psychological stress reactivity and future health and disease outcomes: A systematic review of prospective evidence. Psychoneuroendocrinology 2020, 114, 104599. [Google Scholar] [CrossRef] [PubMed]
- Lee, N.; Massetti, G.M.; Perry, E.W.; Self-Brown, S. Adverse childhood experiences and associated mental distress and suicide risk: Results from the Zambia violence against children survey. J. Interpers. Violence 2022, 37, NP21244–NP21265. [Google Scholar] [CrossRef]
- Themelis, K.; Gillett, J.L.; Karadag, P.; Cheatle, M.D.; Giordano, N.A.; Balasubramanian, S.; Singh, S.P.; Tang, N.K. Mental defeat and suicidality in chronic pain: A prospective analysis. J. Pain 2023, in press. [Google Scholar] [CrossRef] [PubMed]
- Cherrier, C.; Courtois, R.; Rusch, E.; Potard, C. Self-esteem, social problem solving and intimate partner violence victimization in emerging adulthood. Behav. Sci. 2023, 13, 327. [Google Scholar] [CrossRef] [PubMed]
- Bosch, J.; Weaver, T.L.; Arnold, L.D.; Clark, E.M. The impact of intimate partner violence on women’s physical health: Findings from the Missouri Behavioral Risk Factor Surveillance System. J. Interpers. Violence 2017, 32, 3402–3419. [Google Scholar] [CrossRef] [PubMed]
- Alhalal, E. Obesity in women who have experienced intimate partner violence. J. Adv. Nurs. 2018, 74, 2785–2797. [Google Scholar] [CrossRef]
- Lopresti, A.L.; Drummond, P.D. Obesity and psychiatric disorders: Commonalities in dysregulated biological pathways and their implications for treatment. Prog. Neuropsychopharmacol. Biol. Psychiatry 2013, 45, 92–99. [Google Scholar] [CrossRef]
- Wurtman, J.; Wurtman, R. The trajectory from mood to obesity. Curr. Obes. Rep. 2018, 7, 1–5. [Google Scholar] [CrossRef]
- Okifuji, A.; Hare, B.D. The association between chronic pain and obesity. J. Pain. Res. 2015, 8, 399–408. [Google Scholar] [CrossRef]
- Global Initiative for Asthma 2020. Available online: https://ginasthma.org/wp-content/uploads/2020/06/GINA-2020-report_20_06_04-1-wms.pdf (accessed on 5 April 2023).
- Haczku, A.; Panettieri, R.A. Social stress and asthma: The role of corticosteroid insensitivity. J. Allergy Clin. Inmmunol. 2010, 125, 550–558. [Google Scholar] [CrossRef] [PubMed]
- Subramanian, S.V.; Ackerson, L.K.; Subramanyam, M.A.; Wright, R.J. Domestic violence is associated with adult and childhood asthma prevalence in India. Int. J. Epidemiol. 2007, 36, 569–579. [Google Scholar] [CrossRef] [PubMed]
- Rosenberg, S.L.; Miller, G.E.; Brehm, J.M.; Celedon, J.C. Stress and asthma: Novel insights on genetic, epigenetic, and immunologic mechanism. J. Allergy Clin. Immunol. 2014, 134, 1009–1015. [Google Scholar] [CrossRef] [PubMed]
- Adler, E. Erkrankungen durch Storfelder im Trigeminusbereich; Fischer: Heidelberg, Germany, 1973. [Google Scholar]
- Nakagawa, Y.; Yamada, S. Alterations in brain neural network and stress system in atopic dermatitis: Novel therapeutic interventions. J. Pharmacol. Exp. Ther. 2023, 385, 78–87. [Google Scholar] [CrossRef] [PubMed]
- John, R.; Johnson, J.K.; Kukreja, S.; Found, M.; Lindow, S.W. Domestic violence: Prevalence and association with gynaecological symptoms. BJOG 2004, 111, 1128–1132. [Google Scholar] [CrossRef]
- Letourneau, E.J.; Holmes, M.; Chasedunn-Roark, J. Gynaecologic health consequences to victims of interpersonal violence. Womens Health Issues 1999, 9, 115–120. [Google Scholar] [CrossRef]
- Coker, A.L.; Smith, P.H.; Bethea, L.; King, M.R.; McKeown, R.E. Physical health consequences of physical and psychological intimate partner violence. Arch. Fam. Med. 2000, 9, 451–457. [Google Scholar] [CrossRef]
- McCauley, J.; Kern, D.E.; Kolodner, K.; Dill, L.; Schroeder, A.F.; DeChant, H.K.; Ryden, J.; Bass, E.B.; Derogatis, L.R. The “battering syndrome”: Prevalence and clinical characteristics of domestic violence in primary care internal medicine practices. Ann. Intern. Med. 1995, 123, 737–746. [Google Scholar] [CrossRef]
| Biological Risk Factors | Psycho-Social Risk Factors |
|---|---|
Weight condition
Acute upper/lower respiratory tract affection
Genitourinary conditions
Cardiovascular symptoms and conditions
Endocrine disease
Hormonal conditions
Gastrointestinal disorders
Skin problems
Specific inflammations
| Mental health disease
Use of psychoactive substances
Life events
Life quality
Personal characteristics
|
| Authors | Sample | Study Design | Pain | Risk Factors |
|---|---|---|---|---|
| Ali et al. (2021) Pakistan [69] | 945 F 15–49 y/o | Cross-sectional | Pelvic pain |
|
| Al Kendi et al. (2021) Oman [70] | 978 F 30.6 y/o | Cross-sectional | General chronic pain |
|
| Bonomi et al. (2007) USA [50] | 1928 F 18–64 y/o | Cross-sectional | General chronic pain |
|
| Chartier et al. (2010) Canada [52] | 9953 (5187 F—4766 M) 15–98 y/o | Cross-sectional | General chronic pain |
|
| De Wet-Billings & Godongwana (2021) South Africa [71] | 216 F 15–34 y/o | Cross-sectional | General chronic pain |
|
| England-Mason et al. (2018) Canada [64] | 23,846 (12,290 F—11,556 M) 18–64 y/o | Cross-sectional | General chronic pain |
|
| Eslick et al. (2011) Australia [55] | 87 (66 F—21 M) 47 y/o | Case-control | General chronic pain |
|
| FitzPatrick et al. (2022) Australia [72] | 1507 F 31 y/o | Cohort | Pelvic pain |
|
| Gelaye et al. (2016) USA [61] | 2970 F 28.1 y/o | Cross-sectional | General chronic pain |
|
| Gerber et al. (2017) USA [58] | 92 F 39 y/o | Cross-sectional | General chronic pain |
|
| Grossi et al. (2018) Brazil [65] | 80 F 33 y/o | Case-control | General chronic pain |
|
| Gucek & Selic (2018) Slovenia [66] | 161 F 51.1 y/o | Cross-sectional | General chronic pain |
|
| Gunduz et al. (2019) Turkey [67] | 136 F 40 y/o | Case-control | Fibromyalgia |
|
| Halpern et al. (2017) USA [62] | 37 F 19–63 y/o | Cross-sectional | General chronic pain |
|
| Hegarty et al. (2008) Australia [51] | 942 F 16–50 y/o | Cross-sectional | General chronic pain |
|
| Jovanovic et al. (2020) Serbia [68] | 6320 F 20–75 y/o | Cross-sectional | General chronic pain |
|
| Kelly et al. (2011) USA [56] | 135 F 40.3 y/o | Cross-sectional | General chronic pain |
|
| Lutgendorf et al. (2017) USA [63] | 188 F 18–64 y/o | Cross-sectional | Pelvic pain |
|
| Parish et al. (2004) USA [49] | 3323 (1662 F—1661 M) 20–64 y/o | Cross-sectional | General chronic pain |
|
| Raphael et al. (2022) USA [73] | 1974 F 60.2 y/o | Cross-sectional | Pelvic pain |
|
| Saito et al. (2013) Thailand [59] | 421 F 25.9 y/o | Cross-sectional | General chronic pain |
|
| Sutherland et al. (2013) USA [60] | 145 F 30.1 y/o | Cross-sectional | Pelvic pain |
|
| Vives-Cases et al. (2010) Spain [53] | 13,094 F 16–64 y/o | Cross-sectional | General chronic pain |
|
| Williams et al. (2010) USA [54] | 309 F 18–64 y/o | Case-control | Pelvic pain |
|
| Young et al. (2011) USA [57] | 360 (260 F—100 M) 53 y/o | Cohort | General chronic pain |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Uvelli, A.; Duranti, C.; Salvo, G.; Coluccia, A.; Gualtieri, G.; Ferretti, F. The Risk Factors of Chronic Pain in Victims of Violence: A Scoping Review. Healthcare 2023, 11, 2421. https://doi.org/10.3390/healthcare11172421
Uvelli A, Duranti C, Salvo G, Coluccia A, Gualtieri G, Ferretti F. The Risk Factors of Chronic Pain in Victims of Violence: A Scoping Review. Healthcare. 2023; 11(17):2421. https://doi.org/10.3390/healthcare11172421
Chicago/Turabian StyleUvelli, Allison, Cristina Duranti, Giulia Salvo, Anna Coluccia, Giacomo Gualtieri, and Fabio Ferretti. 2023. "The Risk Factors of Chronic Pain in Victims of Violence: A Scoping Review" Healthcare 11, no. 17: 2421. https://doi.org/10.3390/healthcare11172421
APA StyleUvelli, A., Duranti, C., Salvo, G., Coluccia, A., Gualtieri, G., & Ferretti, F. (2023). The Risk Factors of Chronic Pain in Victims of Violence: A Scoping Review. Healthcare, 11(17), 2421. https://doi.org/10.3390/healthcare11172421






