Psychological Toll of the COVID-19 Pandemic: An In-Depth Exploration of Anxiety, Depression, and Insomnia and the Influence of Quarantine Measures on Daily Life
Abstract
:1. Introduction
2. Hypotheses Development
2.1. Anxiety
2.2. Depression
2.3. Insomnia
3. Materials and Methods
3.1. Study Subjects
3.2. Research Design
3.3. Statistical Analysis
-Do you feel anxious about the spread of coronavirus? If yes, What makes you anxious about the spread of COVID-19?-Has the COVID-19 quarantine affected your life? If yes, please specify?
4. Results
4.1. Qualitative Results
4.1.1. Q1: What Makes You Anxious about the Spread of COVID-19?
- a.
- Life treats (death, life-threatening disease, highly infectious);
- b.
- Shortage of support (shortage/unavailability of vaccines, treatment, and inadequate healthcare);
- c.
- Economic impact (lockdown and quarantine, economic shutdown, unemployment);
- d.
- Family and social life (worries about family, disrupted social life).
4.1.2. Q2: Has the COVID-19 Quarantine Affected Your Life? If Yes, Please Specify?
4.2. Quantitative Analysis Results
4.2.1. Invariance Measurement
4.2.2. Measurement Model
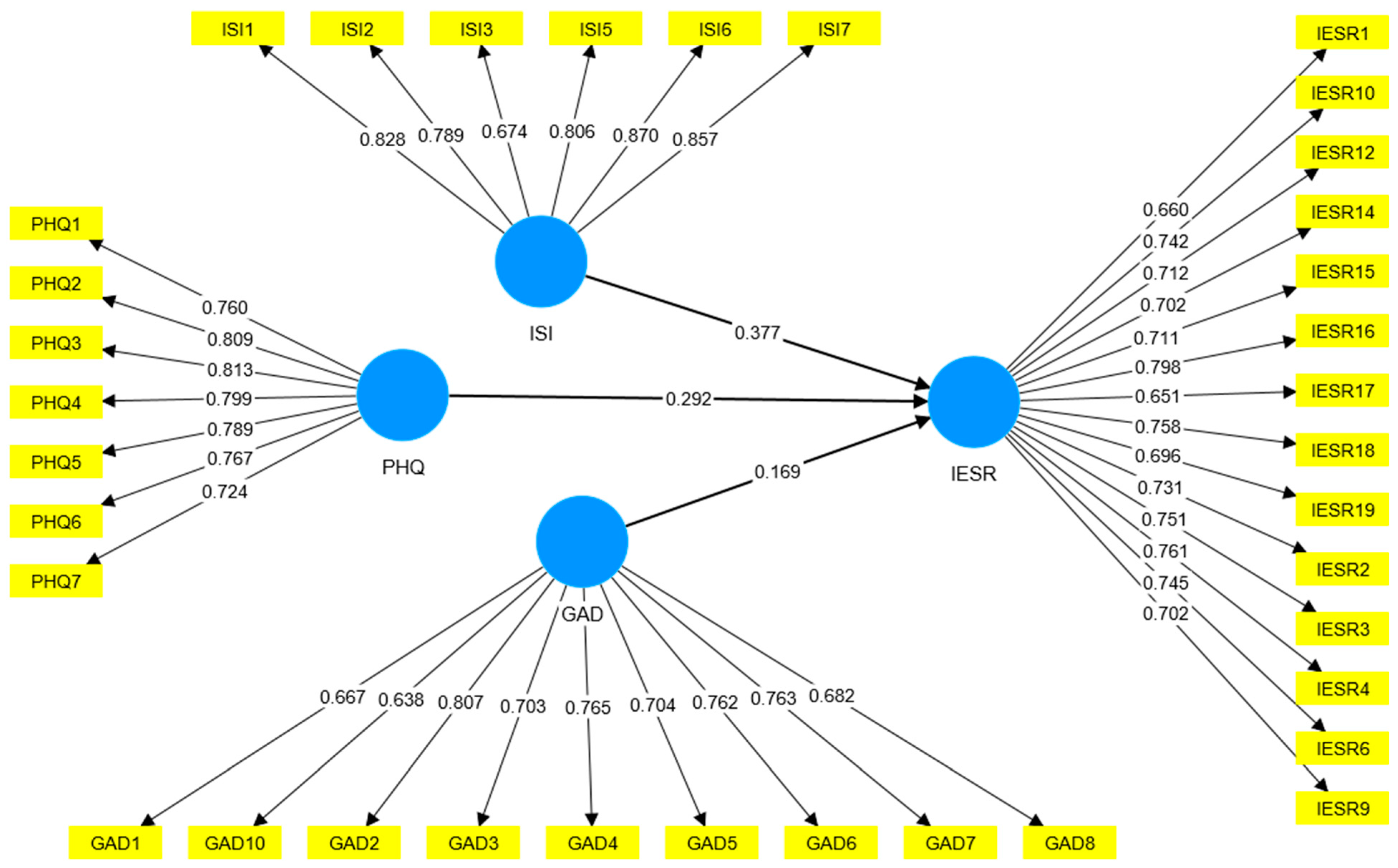
4.2.3. Structural Model
5. Discussion
5.1. Research Implications, Limitations, and Future Directions
5.1.1. Practical Implications
5.1.2. Theoretical Contributions
5.1.3. Limitations and Future Directions
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Martinelli, D.; Fortunato, F.; Mazzilli, S.; Bisceglia, L.; Lopalco, P.L.; Prato, R. Estimating the Proportion of Asymptomatic COVID-19 Cases in an Italian Region with Intermediate Incidence during the First Pandemic Wave: An Observational Retrospective Study. BioMed Res. Int. 2022, 2022, 3401566. [Google Scholar] [CrossRef] [PubMed]
- Mohapatra, R.K.; Tiwari, R.; Sarangi, A.K.; Sharma, S.K.; Khandia, R.; Saikumar, G.; Dhama, K. Twin combination of Omicron and Delta variants triggering a tsunami wave of ever high surges in COVID-19 cases: A challenging global threat with a special focus on the Indian subcontinent. J. Med. Virol. 2022, 94, 1761–1765. [Google Scholar] [CrossRef]
- WHO. WHO Coronavirus (COVID-19) Emergency Dashboard. Available online: https://covid19.who.int/ (accessed on 17 January 2023).
- Aljaberi, M.A.; Lee, K.-H.; Alareqe, N.A.; Qasem, M.A.; Alsalahi, A.; Abdallah, A.M.; Noman, S.; Al-Tammemi, A.A.B.; Mohamed Ibrahim, M.I.; Lin, C.-Y. Rasch Modeling and Multilevel Confirmatory Factor Analysis for the Usability of the Impact of Event Scale-Revised (IES-R) during the COVID-19 Pandemic. Healthcare 2022, 10, 1858. [Google Scholar] [CrossRef]
- Aljaberi, M.A.; Alareqe, N.A.; Alsalahi, A.; Qasem, M.A.; Noman, S.; Uzir, M.U.H.; Mohammed, L.A.; Fares, Z.E.A.; Lin, C.-Y.; Abdallah, A.M.; et al. A cross-sectional study on the impact of the COVID-19 pandemic on psychological outcomes: Multiple indicators and multiple causes modeling. PLoS ONE 2022, 17, e0277368. [Google Scholar] [CrossRef]
- Cascella, M.; Rajnik, M.; Aleem, A.; Dulebohn, S.C.; Di Napoli, R. Features, Evaluation, and Treatment of Coronavirus (COVID-19). In StatPearls; StatPearls Publishing LLC: Treasure Island, FL, USA, 2022. [Google Scholar]
- Millett, G.A.; Jones, A.T.; Benkeser, D.; Baral, S.; Mercer, L.; Beyrer, C.; Honermann, B.; Lankiewicz, E.; Mena, L.; Crowley, J.S.; et al. Assessing differential impacts of COVID-19 on black communities. Ann. Epidemiol. 2020, 47, 37–44. [Google Scholar] [CrossRef] [PubMed]
- Hooper, M.W.; Nápoles, A.M.; Pérez-Stable, E.J. COVID-19 and racial/ethnic disparities. JAMA 2020, 323, 2466–2467. [Google Scholar] [CrossRef] [PubMed]
- Mohammed, L.A.; Aljaberi, M.A.; Amidi, A.; Abdulsalam, R.; Lin, C.-Y.; Hamat, R.A.; Abdallah, A.M. Exploring Factors Affecting Graduate Students’ Satisfaction toward E-Learning in the Era of the COVID-19 Crisis. Eur. J. Investig. Health Psychol. Educ. 2022, 12, 1121–1142. [Google Scholar] [CrossRef]
- Abiddine, F.Z.E.; Aljaberi, M.A.; Gadelrab, H.F.; Lin, C.-Y.; Muhammed, A. Mediated effects of insomnia in the association between problematic social media use and subjective well-being among university students during COVID-19 pandemic. Sleep Epidemiol. 2022, 2, 100030. [Google Scholar] [CrossRef]
- Fares, Z.E.A.; Ala’a, B.; Gadelrab, H.F.; Lin, C.Y.; Aljaberi, M.A.; Alhuwailah, A.; Roubi, M.L. Arabic COVID-19 Psychological Distress Scale: Development and initial validation. BMJ Open 2021, 11, e046006. [Google Scholar] [CrossRef]
- Al-Tammemi, A.A.B.; Barakat, M.; Al Tamimi, D.a.; Alhallaq, S.A.; Al Hasan, D.M.; Khasawneh, G.M.; Naqera, K.A.; Jaradat, R.M.; Farah, F.W.; Al-Maqableh, H.O.; et al. Beliefs Toward Smoking and COVID-19, and the Pandemic Impact on Smoking Behavior and Quit Intention: Findings from a Community-Based Cross-Sectional Study in Jordan. Tob. Use Insights 2021, 14, 1179173X211053022. [Google Scholar] [CrossRef]
- Al-Tammemi, A.a.B.; Nheili, R.; Jibuaku, C.H.; Al Tamimi, D.a.; Aljaberi, M.A.; Khatatbeh, M.; Barakat, M.; Al-Maqableh, H.O.; Fakhouri, H.N. A qualitative exploration of university students’ perspectives on distance education in Jordan: An application of Moore’s theory of transactional distance. Front. Educ. 2022, 7, 960660. [Google Scholar] [CrossRef]
- Cuadra-Martínez, D.; Castro-Carrasco, P.J.; Sandoval-Díaz, J.; Pérez-Zapata, D.; Mora Dabancens, D. COVID-19 and psychological behavior: A systematic review of the psychological effects of 21st century pandemics. Rev. Med. Chile 2020, 148, 1139–1154. [Google Scholar] [CrossRef] [PubMed]
- Dominguez-Salas, S.; Gomez-Salgado, J.; Andres-Villas, M.; Díaz-Milanes, D.; Romero-Martin, M.; Ruiz-Frutos, C. Psycho-Emotional approach to the psychological distress related to the COVID-19 pandemic in Spain: A Cross-Sectional Observational Study. Healthcare 2020, 8, 190. [Google Scholar] [CrossRef]
- Gunnell, D.; Appleby, L.; Arensman, E.; Hawton, K.; John, A.; Kapur, N.; Khan, M.; O’Connor, R.C.; Pirkis, J.; Caine, E.D. Suicide risk and prevention during the COVID-19 pandemic. Lancet Psychiatry 2020, 7, 468–471. [Google Scholar] [CrossRef]
- Kang, L.; Li, Y.; Hu, S.; Chen, M.; Yang, C.; Yang, B.X.; Wang, Y.; Hu, J.; Lai, J.; Ma, X.; et al. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiatry 2020, 7, e14. [Google Scholar] [CrossRef]
- Pramukti, I.; Strong, C.; Sitthimongkol, Y.; Setiawan, A.; Pandin, M.G.R.; Yen, C.-F.; Lin, C.-Y.; Griffiths, M.D.; Ko, N.-Y. Anxiety and Suicidal Thoughts During the COVID-19 Pandemic: Cross-Country Comparative Study Among Indonesian, Taiwanese, and Thai University Students. J. Med. Internet Res. 2020, 22, e24487. [Google Scholar] [CrossRef]
- Acharya, B.; Subedi, K.; Acharya, P.; Ghimire, S. Association between COVID-19 pandemic and the suicide rates in Nepal. PLoS ONE 2022, 17, e0262958. [Google Scholar] [CrossRef] [PubMed]
- Morin, C.M.; Vézina-Im, L.-A.; Ivers, H.; Micoulaud-Franchi, J.-A.; Philip, P.; Lamy, M.; Savard, J. Prevalent, incident, and persistent insomnia in a population-based cohort tested before (2018) and during the first-wave of COVID-19 pandemic (2020). Sleep 2022, 45, zsab258. [Google Scholar] [CrossRef] [PubMed]
- Tang, S.; Xiang, M.; Cheung, T.; Xiang, Y.-T. Mental health and its correlates among children and adolescents during COVID-19 school closure: The importance of parent-child discussion. J. Affect. Disord. 2021, 279, 353–360. [Google Scholar] [CrossRef]
- Holmes, E.A.; O’Connor, R.C.; Perry, V.H.; Tracey, I.; Wessely, S.; Arseneault, L.; Ballard, C.; Christensen, H.; Cohen Silver, R.; Everall, I.; et al. Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. Lancet Psychiatry 2020, 7, 547–560. [Google Scholar] [CrossRef]
- Akour, A.; AlMuhaissen, S.A.; Nusair, M.B.; Al-Tammemi, A.A.B.; Mahmoud, N.N.; Jalouqa, S.; Alrawashdeh, M.N. The untold story of the COVID-19 pandemic: Perceptions and views towards social stigma and bullying in the shadow of COVID-19 illness in Jordan. SN Soc. Sci. 2021, 1, 240. [Google Scholar] [CrossRef] [PubMed]
- Al-Amer, R.; Malak, M.Z.; Burqan, H.M.R.; Stănculescu, E.; Nalubega, S.; Alkhamees, A.A.; Hendawy, A.O.; Ali, A.M. Emotional Reaction to the First Dose of COVID-19 Vaccine: Postvaccination Decline in Anxiety and Stress among Anxious Individuals and Increase among Individuals with Normal Prevaccination Anxiety Levels. J. Pers. Med. 2022, 12, 912. [Google Scholar] [CrossRef]
- Al-Tammemi, A.A.B.; Tarhini, Z. Beyond equity: Advocating theory-based health promotion in parallel with COVID-19 mass vaccination campaigns. Public Health Pract. 2021, 2, 100142. [Google Scholar] [CrossRef] [PubMed]
- Arinah, W.; Musheer, J.; Juni, M.H. Health Care Provision and Equity. Int. J. Public Health Clin. Sci. 2016, 3, 2289–7577. [Google Scholar]
- Strauß, B.; Berger, U.; Rosendahl, J. Indirect and direct psychosocial consequences of the corona pandemic—Part 1 of a (preliminary) review. Psychotherapeut 2021, 66, 175–185. [Google Scholar] [CrossRef]
- Ali, A.M.; Al-Dossary, S.A.; Almarwani, A.M.; Atout, M.; Al-Amer, R.; Alkhamees, A.A. The Impact of Event Scale—Revised: Examining its cutoff scores among Arab psychiatric patients and healthy adults within the context of COVID-19 as a collective traumatic event. Healthcare 2023, 11, 892. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, R.C.; Wetherall, K.; Cleare, S.; McClelland, H.; Melson, A.J.; Niedzwiedz, C.L.; O’Carroll, R.E.; O’Connor, D.B.; Platt, S.; Scowcroft, E.; et al. Mental health and well-being during the COVID-19 pandemic: Longitudinal analyses of adults in the UK COVID-19 Mental Health & Wellbeing study. Br. J. Psychiatry J. Ment. Sci. 2021, 218, 326–333. [Google Scholar] [CrossRef]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; McIntyre, R.S.; Choo, F.N.; Tran, B.; Ho, R.; Sharma, V.K.; et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav. Immun. 2020, 87, 40–48. [Google Scholar] [CrossRef]
- Ramlo, S.E. Divergent viewpoints about the statistical stage of a mixed method: Qualitative versus quantitative orientations. Int. J. Res. Method Educ. 2020, 43, 93–111. [Google Scholar] [CrossRef]
- Koh, D.; Lim, M.K.; Chia, S.E.; Ko, S.M.; Qian, F.; Ng, V.; Tan, B.H.; Wong, K.S.; Chew, W.M.; Tang, H.K. Risk Perception and Impact of Severe Acute Respiratory Syndrome (SARS) on Work and Personal Lives of Healthcare Workers in Singapore What Can We Learn? Med. Care 2005, 43, 676–682. [Google Scholar] [CrossRef]
- Sim, K.; Chan, Y.H.; Chong, P.N.; Chua, H.C.; Soon, S.W. Psychosocial and coping responses within the community health care setting towards a national outbreak of an infectious disease. J. Psychosom. Res. 2010, 68, 195–202. [Google Scholar] [CrossRef] [PubMed]
- Odriozola-Gonzalez, P.; Planchuelo-Gómez, A.; Irurtia, M.J.; de Luis-Garcia, R. Psychological effects of the COVID-19 outbreak and lockdown among students and workers of a Spanish university. Psychiatry Res. 2020, 290, 113108. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; Ho, C.S.; Ho, R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health 2020, 17, 1705–1729. [Google Scholar] [CrossRef]
- Ho, C.S.; Chee, C.Y.; Ho, R.C. Mental Health Strategies to Combat the Psychological Impact of Coronavirus Disease 2019 (COVID-19) Beyond Paranoia and Panic. Ann. Acad. Med. Singap. 2020, 49, 155–160. [Google Scholar] [CrossRef]
- Li, Z.; Ge, J.; Yang, M.; Feng, J.; Qiao, M.; Jiang, R.; Bi, J.; Zhan, G.; Xu, X.; Wang, L.; et al. Vicarious traumatization in the general public, members, and non-members of medical teams aiding in COVID-19 control. Brain Behav. Immun. 2020, 88, 916–919. [Google Scholar] [CrossRef]
- Powell-Jackson, T.; King, J.J.C.; Makungu, C.; Spieker, N.; Woodd, S.; Risha, P.; Goodman, C. Infection prevention and control compliance in Tanzanian outpatient facilities: A cross-sectional study with implications for the control of COVID-19. Lancet Glob. Health 2020, 8, e780–e789. [Google Scholar] [CrossRef] [PubMed]
- Sun, N.; Wei, L.; Shi, S.; Jiao, D.; Song, R.; Ma, L.; Wang, H.; Wang, C.; Wang, Z.; You, Y.; et al. A qualitative study on the psychological experience of caregivers of COVID-19 patients. Am. J. Infect. Control. 2020, 48, 592–598. [Google Scholar] [CrossRef]
- Gabarrell-Pascuet, A.; García-Mieres, H.; Giné-Vázquez, I.; Moneta, M.V.; Koyanagi, A.; Haro, J.M.; Domènech-Abella, J. The Association of Social Support and Loneliness with Symptoms of Depression, Anxiety, and Posttraumatic Stress during the COVID-19 Pandemic: A Meta-Analysis. Int. J. Environ. Res. Public Health 2023, 20, 2765. [Google Scholar] [CrossRef]
- Warwicker, S.; Sant, D.; Richard, A.; Cutajar, J.; Bellizzi, A.; Micallef, G.; Refalo, D.; Camilleri, L.; Grech, A. A Retrospective Longitudinal Analysis of Mental Health Admissions: Measuring the Fallout of the Pandemic. Int. J. Environ. Res. Public Health 2023, 20, 1194. [Google Scholar] [CrossRef]
- Narita, Z.; Okubo, R.; Sasaki, Y.; Takeda, K.; Ohmagari, N.; Yamaguchi, K.; Morisaki, N.; Sampei, M.; Ishitsuka, K.; Kojima, M.; et al. Association of COVID-19-related discrimination with subsequent depression and suicidal ideation in healthcare workers. J. Psychiatr. Res. 2023, 159, 153–158. [Google Scholar] [CrossRef]
- Lenzi, S.; Sádaba, J.; Lindborg, P. Soundscape in Times of Change: Case Study of a City Neighbourhood During the COVID-19 Lockdown. Front. Psychol. 2021, 12, 570741. [Google Scholar] [CrossRef]
- Roy, D.; Tripathy, S.; Kar, S.K.; Sharma, N.; Verma, S.K.; Kaushal, V. Study of knowledge, attitude, anxiety & perceived mental healthcare need in Indian population during COVID-19 pandemic. Asian J. Psychiatry 2020, 51, 102083. [Google Scholar]
- Pinar Kiymet, K. Anxiety of Dental Professionals during COVID-19 Pandemic. In Anxiety, Uncertainty, and Resilience during the Pandemic Period; Fabio, G., Floriana, I., Eds.; IntechOpen: Rijeka, Croatia, 2021; p. Ch. 29. [Google Scholar]
- Lasheras, I.; Gracia-García, P.; Lipnicki, D.M.; Bueno-Notivol, J.; López-Antón, R.; de la Cámara, C.; Lobo, A.; Santabárbara, J. Prevalence of Anxiety in Medical Students during the COVID-19 Pandemic: A Rapid Systematic Review with Meta-Analysis. Int. J. Environ. Res. Public Health 2020, 17, 6603. [Google Scholar] [CrossRef]
- Usher, K.; Durkin, J.; Bhullar, N. The COVID-19 pandemic and mental health impacts. Int. J. Ment. Health Nurs. 2020, 29, 315. [Google Scholar] [CrossRef]
- Santabárbara, J.; Bueno-Notivol, J.; Lipnicki, D.M.; Olaya, B.; Pérez-Moreno, M.; Gracia-García, P.; Idoiaga-Mondragon, N.; Ozamiz-Etxebarria, N. Prevalence of anxiety in health care professionals during the COVID-19 pandemic: A rapid systematic review (on published articles in Medline) with meta-analysis. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2021, 107, 110244. [Google Scholar] [CrossRef]
- Liu, C.-Y.; Yang, Y.-Z.; Zhang, X.-M.; Xu, X.; Dou, Q.-L.; Zhang, W.-W.; Cheng, A.S. The prevalence and influencing factors in anxiety in medical workers fighting COVID-19 in China: A cross-sectional survey. Epidemiol. Infect. 2020, 148, e98. [Google Scholar] [CrossRef] [PubMed]
- Cag, Y.; Erdem, H.; Gormez, A.; Ankarali, H.; Hargreaves, S.; Ferreira-Coimbra, J.; Rubulotta, F.; Belliato, M.; Berger-Estilita, J.; Pelosi, P. Anxiety among front-line health-care workers supporting patients with COVID-19: A global survey. Gen. Hosp. Psychiatry 2021, 68, 90–96. [Google Scholar] [CrossRef]
- Sorokin, M.Y.; Kasyanov, E.D.; Rukavishnikov, G.V.; Makarevich, O.V.; Neznanov, N.G.; Lutova, N.B.; Mazo, G.E. Structure of anxiety associated with the COVID-19 pandemic in the Russian-speaking sample: Results from on-line survey. MedRxiv 2020. [Google Scholar] [CrossRef]
- Sunday-Nweke, N.A.; Igwe, M.; Obasi, A. Assessing anxiety levels amongst surgeons during COVID-19 pandemic. Consultant 2020, 3, 28–31. [Google Scholar]
- Lahav, Y. Psychological distress related to COVID-19–the contribution of continuous traumatic stress. J. Affect. Disord. 2020, 277, 129–137. [Google Scholar] [CrossRef] [PubMed]
- Ali, A.M.; Alkhamees, A.A.; Abd Elhay, E.S.; Taha, S.M.; Hendawy, A.O. COVID-19-related psychological trauma and psychological distress among community-dwelling psychiatric patients: People struck by depression and sleep disorders endure the greatest burden. Front. Public Health 2022, 9, 2141. [Google Scholar] [CrossRef]
- Shevlin, M.; Nolan, E.; Owczarek, M.; McBride, O.; Murphy, J.; Gibson Miller, J.; Hartman, T.K.; Levita, L.; Mason, L.; Martinez, A.P. COVID-19-related anxiety predicts somatic symptoms in the UK population. Br. J. Health Psychol. 2020, 25, 875–882. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.H.; Zhang, E.; Wong, G.T.F.; Hyun, S. Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: Clinical implications for US young adult mental health. Psychiatry Res. 2020, 290, 113172. [Google Scholar] [CrossRef] [PubMed]
- Rettie, H.; Daniels, J. Coping and tolerance of uncertainty: Predictors and mediators of mental health during the COVID-19 pandemic. Am. Psychol. 2021, 76, 427. [Google Scholar] [CrossRef] [PubMed]
- Özmete, E.; Pak, M. The relationship between anxiety levels and perceived social support during the pandemic of COVID-19 in Turkey. Soc. Work. Public Health 2020, 35, 603–616. [Google Scholar] [CrossRef]
- Santabárbara, J.; Lasheras, I.; Lipnicki, D.M.; Bueno-Notivol, J.; Pérez-Moreno, M.; López-Antón, R.; De la Cámara, C.; Lobo, A.; Gracia-García, P. Prevalence of anxiety in the COVID-19 pandemic: An updated meta-analysis of community-based studies. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2021, 109, 110207. [Google Scholar] [CrossRef]
- Del Valle, M.V.; Andrés, M.L.; Urquijo, S.; Yerro-Avincetto, M.; López-Morales, H.; Canet-Juric, L. Intolerance of uncertainty over COVID-19 pandemic and its effect on anxiety and depressive symptoms. Rev. Interam. De Psicol./Interam. J. Psychol. 2020, 54, e1335. [Google Scholar] [CrossRef]
- Vignesh, D.; Lokesh, S. Systamatic review on the relationship among COVID-19 and anxiety. Eur. J. Mol. Clin. Med. 2020, 7, 5687–5693. [Google Scholar]
- Soetikno, N. Descriptive Study of Adolescent Depression in COVID-19 Pandemic. In Proceedings of the 2nd Tarumanagara International Conference on the Applications of Social Sciences and Humanities (TICASH 2020), Jakarta, Indonesia, 3–4 August 2020; pp. 588–592. [Google Scholar]
- Dange, H.; Gurav, A.; Naik, P. To assess basic knowledge of COVID-19 and impact of COVID-19 on mental health status of nursing staff working in COVID-19 hospital atmosphere. Int. J. Adv. Res. Nurs. 2020, 3, 121–123. [Google Scholar] [CrossRef]
- Yasir, S.; Fatima, G.; Umar, Z.; Tahir, Z.; Malik, Q.; Maqsood, A.; Muhammad, S. Assessment of Severity of Anxiety and Depression in COVID-19 Patients Admitted to Rawalpindi Medical University and Allied Hospitals Rawalpindi Pakistan. Pak. J. Med. Health Sci. 2022, 16, 296. [Google Scholar]
- Ali Shah, S.A.; Zubair, U.B.; Nadeem, M.S.; Faheem Qasim, M.; Azhar Ali, S.S.; Yasmeen, R. Depression and Anxiety among patients suffering from mild to moderate COVID-19 Disease. Pak. J. Med. Health Sci. 2021, 15, 3322–3324. [Google Scholar] [CrossRef]
- Rajkumar, R.P. COVID-19 and mental health: A review of the existing literature. Asian J. Psychiatry 2020, 52, 102066. [Google Scholar] [CrossRef]
- Liu, X.; Zhu, M.; Zhang, R.; Zhang, J.; Zhang, C.; Liu, P.; Feng, Z.; Chen, Z. Public mental health problems during COVID-19 pandemic: A large-scale meta-analysis of the evidence. Transl. Psychiatry 2021, 11, 384. [Google Scholar] [CrossRef] [PubMed]
- Vindegaard, N.; Benros, M.E. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain Behav. Immun. 2020, 89, 531–542. [Google Scholar] [CrossRef] [PubMed]
- Lakhan, R.; Agrawal, A.; Sharma, M. Prevalence of depression, anxiety, and stress during COVID-19 pandemic. J. Neurosci. Rural. Pract. 2020, 11, 519–525. [Google Scholar] [CrossRef] [PubMed]
- Canet-Juric, L.; Andrés, M.L.; Del Valle, M.; López-Morales, H.; Poó, F.; Galli, J.I.; Yerro, M.; Urquijo, S. A longitudinal study on the emotional impact cause by the COVID-19 pandemic quarantine on general population. Front. Psychol. 2020, 11, 2431. [Google Scholar] [CrossRef]
- Paolini, M.; Mazza, M.G.; Palladini, M.; Dallaspezia, S.; Vai, B.; Poletti, S.; Benedetti, F.P. 0279 Neural underpinnings of depressive and post-traumatic symptomatology in COVID-19 survivors: A voxel-based morphometry study. Eur. Neuropsychopharmacol. 2021, 53, S201–S202. [Google Scholar] [CrossRef]
- da Silva, F.C.T.; Neto, M.L.R. Psychiatric symptomatology associated with depression, anxiety, distress, and insomnia in health professionals working in patients affected by COVID-19: A systematic review with meta-analysis. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2021, 104, 110057. [Google Scholar] [CrossRef]
- Sinha, K.; Ish, P. Insomnia During COVID-19 Pandemic: Few Points to Ponder. Sleep Vigil. 2021, 5, 323–324. [Google Scholar] [CrossRef] [PubMed]
- Pizzonia, K.L.; Koscinski, B.; Suhr, J.A.; Accorso, C.; Allan, D.M.; Allan, N.P. Insomnia during the COVID-19 pandemic: The role of depression and COVID-19-related risk factors. Cogn. Behav. Ther. 2021, 50, 246–260. [Google Scholar] [CrossRef]
- Li, Y.; Chen, B.; Hong, Z.; Sun, Q.; Dai, Y.; Basta, M.; Tang, X.; Qin, Q. Insomnia symptoms during the early and late stages of the COVID-19 pandemic in China: A systematic review and meta-analysis. Sleep Med. 2022, 91, 262–272. [Google Scholar] [CrossRef] [PubMed]
- Kokou-Kpolou, C.K.; Megalakaki, O.; Laimou, D.; Kousouri, M. Insomnia during COVID-19 pandemic and lockdown: Prevalence, severity, and associated risk factors in French population. Psychiatry Res. 2020, 290, 113128. [Google Scholar] [CrossRef] [PubMed]
- Lin, L.-Y.; Wang, J.; Ou-yang, X.-Y.; Miao, Q.; Chen, R.; Liang, F.-X.; Zhang, Y.-P.; Tang, Q.; Wang, T. The immediate impact of the 2019 novel coronavirus (COVID-19) outbreak on subjective sleep status. Sleep Med. 2021, 77, 348–354. [Google Scholar] [CrossRef]
- Xu, F.; Wang, X.; Yang, Y.; Zhang, K.; Shi, Y.; Xia, L.; Hu, X.; Liu, H. Depression and insomnia in COVID-19 survivors: A cross-sectional survey from Chinese rehabilitation centers in Anhui province. Sleep Med. 2022, 91, 161–165. [Google Scholar] [CrossRef] [PubMed]
- Serrano-Ripoll, M.J.; Zamanillo-Campos, R.; Castro, A.; Fiol-de Roque, M.A.; Ricci-Cabello, I. Insomnia and sleep quality in healthcare workers fighting against COVID-19: A systematic review of the literature and meta-analysis. Actas Esp. Psiquiatr. 2021, 49, 155–179. [Google Scholar]
- Melehin, A. Sleep disorders during the COVID-19 pandemic: Specifics and psychological diagnostic. Arch. Neurol. Neurosci. 2021, 9, 17–25. [Google Scholar] [CrossRef]
- Wang, Y.; Zhu, L.-Y.; Ma, Y.-F.; Bo, H.-X.; Deng, H.-B.; Cao, J.; Wang, Y.; Wang, X.-J.; Xu, Y.; Lu, Q.-D.; et al. Association of insomnia disorder with sociodemographic factors and poor mental health in COVID-19 inpatients in China. Sleep Med. 2020, 75, 282–286. [Google Scholar] [CrossRef]
- Voitsidis, P.; Gliatas, I.; Bairachtari, V.; Papadopoulou, K.; Papageorgiou, G.; Parlapani, E.; Syngelakis, M.; Holeva, V.; Diakogiannis, I. Insomnia during the COVID-19 pandemic in a Greek population. Psychiatry Res. 2020, 289, 113076. [Google Scholar] [CrossRef]
- Budiarti, T.N.; Puspitasari, A.D.; Rosyid, A.N.; Indriani, D.; Melaniani, S.; Satryo, F.Z.O.; Aina, L.; Ardianto, N.; Rachman, M.P.A.; Meiliani, F. Insomnia Among COVID-19 Patients During Isolation Treatment in Inpatient Room of Indonesian Health Care Facilities. Media Kesehat. Masy. Indones. 2022, 18, 18–25. [Google Scholar] [CrossRef]
- Creswell, J.W.; Creswell, J.D. Research Design: Qualitative, Quantitative, and Mixed Methods Approaches; Sage Publications: Newbury Park, CA, USA, 2017. [Google Scholar]
- Greene, J.C. Is mixed methods social inquiry a distinctive methodology? J. Mix. Methods Res. 2008, 2, 7–22. [Google Scholar] [CrossRef]
- Morgan, D.L. Practical strategies for combining qualitative and quantitative methods: Applications to health research. Qual. Health Res. 1998, 8, 362–376. [Google Scholar] [CrossRef] [PubMed]
- Weiss, D.S.; Marmar, C. The Impact of Event Scale—Revised. In Assessing Psychological Trauma and PTSD: A Handbook for Practitioners; Wilson, J.P., Tang, S.-K., Catherine, C., Eds.; Guilford Press: New York, NY, USA, 1997; Volume 19, pp. 399–411. [Google Scholar]
- Zhang, M.W.; Ho, C.S.; Fang, P.; Lu, Y.; Ho, R.C. Usage of social media and smartphone application in assessment of physical and psychological well-being of individuals in times of a major air pollution crisis. JMIR Mhealth Uhealth 2014, 2, e16. [Google Scholar] [CrossRef]
- Chin, W.Y.; Chan, K.T.; Lam, C.L.; Wong, S.Y.; Fong, D.Y.; Lo, Y.Y.; Lam, T.P.; Chiu, B.C. Detection and management of depression in adult primary care patients in Hong Kong: A cross-sectional survey conducted by a primary care practice-based research network. BMC Fam. Pract. 2014, 15, 30. [Google Scholar] [CrossRef]
- Manea, L.; Gilbody, S.; McMillan, D. Optimal cut-off score for diagnosing depression with the Patient Health Questionnaire (PHQ-9): A meta-analysis. CMAJ 2012, 184, E191–E196. [Google Scholar] [CrossRef]
- Dhingra, S.S.; Kroenke, K.; Zack, M.M.; Strine, T.W.; Balluz, L.S. PHQ-8 Days: A measurement option for DSM-5 Major Depressive Disorder (MDD) severity. Popul. Health Metr. 2011, 9, 11. [Google Scholar] [CrossRef] [PubMed]
- Bianchi, R.; Verkuilen, J.; Toker, S.; Schonfeld, I.S.; Gerber, M.; Brähler, E.; Kroenke, K. Is the PHQ-9 a unidimensional measure of depression? A 58,272-participant study. Psychological Assessment 2022, 34, 595–603. [Google Scholar] [CrossRef] [PubMed]
- Chiu, B.; Chin, W. Systematic review and meta-analysis on the patient health questionnare-9 (PHQ-9) for depression screening in Chinese primary care patients. Fam. Med. 2018. [Google Scholar] [CrossRef]
- Fekadu, A.; Demissie, M.; Birhane, R.; Medhin, G.; Bitew, T.; Hailemariam, M.; Minaye, A.; Habtamu, K.; Milkias, B.; Petersen, I.; et al. Under detection of depression in primary care settings in low and middle-income countries: A systematic review and meta-analysis. Syst. Rev. 2022, 11, 21. [Google Scholar] [CrossRef]
- Hu, T.; Zhao, X.; Wu, M.; Li, Z.; Luo, L.; Yang, C.; Yang, F. Prevalence of depression in older adults: A systematic review and meta-analysis. Psychiatry Res. 2022, 311, 114511. [Google Scholar] [CrossRef]
- Yin, L.; Teklu, S.; Pham, H.; Li, R.; Tahir, P.; Garcia, M.E. Validity of the Chinese Language Patient Health Questionnaire 2 and 9: A Systematic Review. Health Equity 2022, 6, 574–594. [Google Scholar] [CrossRef]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.; Löwe, B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef]
- Bastien, C.H.; Vallières, A.; Morin, C.M. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001, 2, 297–307. [Google Scholar] [CrossRef]
- Liang, M.; Li, Y.; Chen, Q.; Tan, H.; He, L.; Sheng, C.; Cai, Y.; Li, X.; Zhang, Z.; Wang, J.; et al. The Difficulties and Mental Health Intervention Need of Doctors and Nurses in Biological Emergencies: A Qualitative Study. Front. Psychiatry 2021, 12, 696823. [Google Scholar] [CrossRef]
- Morrow, R.; Rodriguez, A.; King, N. Colaizzi’s descriptive phenomenological method. Psychologist 2015, 28, 643–644. [Google Scholar]
- Edward, K.-L.; Welch, T. The extension of Colaizzi’s method of phenomenological enquiry. Contemp. Nurse 2011, 39, 163–171. [Google Scholar] [CrossRef] [PubMed]
- Wirihana, L.; Welch, A.; Williamson, M.; Christensen, M.; Bakon, S.; Craft, J. Using Colaizzi’s method of data analysis to explore the experiences of nurse academics teaching on satellite campuses. Nurse Res. 2018, 25, 30–34. [Google Scholar] [CrossRef]
- Neal, J.W.; Neal, Z.P.; VanDyke, E.; Kornbluh, M. Expediting the analysis of qualitative data in evaluation: A procedure for the rapid identification of themes from audio recordings (RITA). Am. J. Eval. 2015, 36, 118–132. [Google Scholar] [CrossRef]
- Cohen, J. Eta-Squared and Partial Eta-Squared in Fixed Factor Anova Designs. Educ. Psychol. Meas. 1973, 33, 107–112. [Google Scholar] [CrossRef]
- Hajji, J.; Sabah, A.; Aljaberi, M.A.; Lin, C.-Y.; Huang, L.-Y. The Effect of Ramadan Fasting on the Coping Strategies Used by Male Footballers Affiliated with the Tunisian First Professional League. Healthcare 2023, 11, 1053. [Google Scholar] [CrossRef] [PubMed]
- Lakens, D. Calculating and reporting effect sizes to facilitate cumulative science: A practical primer for t-tests and ANOVAs. Front. Psychol. 2013, 4, 863. [Google Scholar] [CrossRef] [PubMed]
- Musheer Abdulwahid, A.; Muhamad Hanafiah, J.; Rasheed Addulsalam, A.-M.; Munn Sann, L.; Murad Abdu, S.; Sami Abdo Radman, A.-D.; Hayati Kadir, S. Relationships among perceived quality of healthcare services, satisfaction and behavioural intentions of international students in Kuala Lumpur, Malaysia: A cross-sectional study. BMJ Open 2018, 8, e021180. [Google Scholar] [CrossRef]
- Hair, J.F., Jr.; Matthews, L.M.; Matthews, R.L.; Sarstedt, M. PLS-SEM or CB-SEM: Updated guidelines on which method to use. Int. J. Multivar. Data Anal. 2017, 1, 107–123. [Google Scholar] [CrossRef]
- Hair, J.F.; Anderson, R.E.; Babin, B.J.; Black, W.C. Multivariate Data Analysis: A Global Perspective; Pearson: Upper Saddle River, NJ, USA, 2010; Volume 7. [Google Scholar]
- Al-Matari, A.S.; Amiruddin, R.; Aziz, K.A.; Al-Sharafi, M.A. The Impact of Dynamic Accounting Information System on Organizational Resilience: The Mediating Role of Business Processes Capabilities. Sustainability 2022, 14, 4967. [Google Scholar] [CrossRef]
- Hair, J.F.; Hult, G.T.M.; Ringle, C.M.; Sarstedt, M.; Danks, N.P.; Ray, S. Evaluation of the Structural Model. In Partial Least Squares Structural Equation Modeling (PLS-SEM) Using R: A Workbook; Springer International Publishing: Cham, Swithzerland, 2021; pp. 115–138. [Google Scholar]
- Hair, J.F., Jr.; Hult, G.T.M.; Ringle, C.; Sarstedt, M. A primer on Partial Least Squares Structural Equation Modeling (PLS-SEM), 2nd ed.; Sage Publications: Newbury Park, CA, USA, 2016. [Google Scholar]
- Uzir, M.U.H.; Al Halbusi, H.; Thurasamy, R.; Thiam Hock, R.L.; Aljaberi, M.A.; Hasan, N.; Hamid, M. The effects of service quality, perceived value and trust in home delivery service personnel on customer satisfaction: Evidence from a developing country. J. Retail. Consum. Serv. 2021, 63, 102721. [Google Scholar] [CrossRef]
- Ramayah, T.; Cheah, J.; Chuah, F.; Ting, H.; Memon, M.A. Partial Least Squares Structural Equation Modeling (PLS-SEM) using SmartPLS 3.0: An Updated Guide and Practical Guide to Statistical Analysis, 2nd ed.; Pearson: Kuala Lumpur, Malaysia; Upper Saddle River, NJ, USA, 2018. [Google Scholar]
- Al-Emran, M.; Mezhuyev, V.; Kamaludin, A. PLS-SEM in Information Systems Research: A Comprehensive Methodological Reference. In Proceedings of the International Conference on Advanced Intelligent Systems and Informatics, Cairo, Egypt, 1–3 September 2018; Springer: Cham, Swithzerland, 2019; pp. 644–653. [Google Scholar]
- Streukens, S.; Leroi-Werelds, S. Bootstrapping and PLS-SEM: A step-by-step guide to get more out of your bootstrap results. Eur. Manag. J. 2016, 34, 618–632. [Google Scholar] [CrossRef]
- Kock, N. Should Bootstrapping Be Used in PLS-SEM? Toward Stable P-Value Calculation Methods. J. Appl. Struct. Equ. Model. 2018, 1, 2590–42211. [Google Scholar] [CrossRef] [PubMed]
- Al-Emran, M.; AlQudah, A.A.; Abbasi, G.A.; Al-Sharafi, M.A.; Iranmanesh, M. Determinants of using AI-based chatbots for knowledge sharing: Evidence from PLS-SEM and fuzzy sets (fsQCA). IEEE Trans. Eng. Manag. 2023, 1–15. [Google Scholar] [CrossRef]
- Mohd Rahim, N.I.; Iahad, N.A.; Yusof, A.F.; A. Al-Sharafi, M. AI-Based Chatbots Adoption Model for Higher-Education Institutions: A Hybrid PLS-SEM-Neural Network Modelling Approach. Sustainability 2022, 14, 12726. [Google Scholar] [CrossRef]
- Arpaci, I.; Masrek, M.N.; Al-Sharafi, M.A.; Al-Emran, M. Evaluating the actual use of cloud computing in higher education through information management factors: A cross-cultural comparison. Educ. Inf. Technol. 2023, 1–21. [Google Scholar] [CrossRef]
- Ayyash, M.M.; Herzallah, F.A.; Al-Sharafi, M.A. Arab cultural dimensions model for e-government services adoption in public sector organisations: An empirical examination. Electron. Gov. Int. J. 2022, 18, 9–44. [Google Scholar] [CrossRef]
- Al-Sharafi, M.A.; Al-Emran, M.; Arpaci, I.; Marques, G.; Namoun, A.; Iahad, N.A. Examining the impact of psychological, social, and quality factors on the continuous intention to use virtual meeting platforms during and beyond COVID-19 pandemic: A hybrid SEM-ANN approach. Int. J. Hum.–Comput. Interact. 2022, 39, 2673–2685. [Google Scholar] [CrossRef]
- Chin, W.W. The partial least squares approach to structural equation modeling. Mod. Methods Bus. Res. 1998, 295, 295–336. [Google Scholar]
- Hair, J.F.; Black, W.C.; Babin, B.J.; Anderson, R.E.; Tatham, R.L. Multivariate Data Analysis, 6th ed.; Pearson Prentice Hall: Upper Saddle River, NJ, USA, 2006. [Google Scholar]
- Al-Sharafi, M.A.; Al-Emran, M.; Arpaci, I.; Iahad, N.A.; AlQudah, A.A.; Iranmanesh, M.; Al-Qaysi, N. Generation Z use of artificial intelligence products and its impact on environmental sustainability: A cross-cultural comparison. Comput. Hum. Behav. 2023, 143, 107708. [Google Scholar] [CrossRef]
- Franke, G.; Sarstedt, M. Heuristics versus statistics in discriminant validity testing: A comparison of four procedures. Internet Res. 2019, 29, 430–447. [Google Scholar] [CrossRef]
- Henseler, J.; Ringle, C.M.; Sarstedt, M. A new criterion for assessing discriminant validity in variance-based structural equation modeling. J. Acad. Mark. Sci. 2015, 43, 115–135. [Google Scholar] [CrossRef]
- Alareqe, N.A.; Hassan, S.A.; Kamarudin, E.M.E.; Aljaberi, M.A.; Nordin, M.S.; Ashureay, N.M.; Mohammed, L.A. Validity of Adult Psychopathology Model Using Psychiatric Patient Sample from a Developing Country: Confirmatory Factor Analysis. Ment. Illn. 2022, 2022, 9594914. [Google Scholar] [CrossRef]
- Gupta, S.; Hayek, S.S.; Wang, W.; Chan, L.; Mathews, K.S.; Melamed, M.L.; Brenner, S.K.; Leonberg-Yoo, A.; Schenck, E.J.; Radbel, J. Factors Associated With Death in Critically Ill Patients With Coronavirus Disease 2019 in the US. JAMA Intern. Med. 2020, 180, 1436–1446. [Google Scholar] [CrossRef]
- Mizumoto, K.; Chowell, G. Estimating risk for death from coronavirus disease, China, january–february 2020. Emerg. Infect. Dis. 2020, 26, 1251–1256. [Google Scholar] [CrossRef]
- Wu, C.; Chen, X.; Cai, Y.; Xia, J.; Zhou, X.; Xu, S.; Huang, H.; Zhang, L.; Zhou, X.; Du, C.; et al. Risk Factors Associated With Acute Respiratory Distress Syndrome and Death in Patients With Coronavirus Disease 2019 Pneumonia in Wuhan, China. JAMA Intern. Med. 2020, 180, 934–943. [Google Scholar] [CrossRef]
- Zivot, J. Coronavirus Disease 2019 Triage Teams: Death by Numbers. Crit. Care Med. 2020, 48, 1241–1242. [Google Scholar] [CrossRef]
- Le, T.T.; Cramer, J.P.; Chen, R.; Mayhew, S. Evolution of the COVID-19 vaccine development landscape. Nat. Rev. Drug Discov. 2020, 19, 667–668. [Google Scholar] [CrossRef]
- Barmparis, G.D.; Tsironis, G. Estimating the infection horizon of COVID-19 in eight countries with a data-driven approach. Chaos Solitons Fractals 2020, 135, 109842. [Google Scholar] [CrossRef] [PubMed]
- De Natale, G.; Ricciardi, V.; De Luca, G.; De Natale, D.; Di Meglio, G.; Ferragamo, A.; Marchitelli, V.; Piccolo, A.; Scala, A.; Somma, R. The COVID-19 Infection in Italy: A Statistical Study of an Abnormally Severe Disease. J. Clin. Med. 2020, 9, 1564. [Google Scholar] [CrossRef] [PubMed]
- Azar, K.M.; Shen, Z.; Romanelli, R.J.; Lockhart, S.H.; Smits, K.; Robinson, S.; Brown, S.; Pressman, A.R. Disparities In Outcomes Among COVID-19 Patients In A Large Health Care System In California: Study estimates the COVID-19 infection fatality rate at the US county level. Health Aff. 2020, 39, 1253–1262. [Google Scholar] [CrossRef] [PubMed]
- Ibarra-Vega, D. Lockdown, one, two, none, or smart. Modeling containing COVID-19 infection. A conceptual model. Sci. Total Environ. 2020, 730, 138917. [Google Scholar] [CrossRef]
- Panda, P.K.; Gupta, J.; Chowdhury, S.R.; Kumar, R.; Meena, A.K.; Madaan, P.; Sharawat, I.K.; Gulati, S. Psychological and Behavioral Impact of Lockdown and Quarantine Measures for COVID-19 Pandemic on Children, Adolescents and Caregivers: A Systematic Review and Meta-Analysis. J. Trop. Pediatr. 2021, 67, fmaa122. [Google Scholar] [CrossRef]
- Shah, J.N.; Shah, J.; Shah, J. Quarantine, isolation and lockdown: In context of COVID-19. J. Patan Acad. Health Sci. 2020, 7, 48–57. [Google Scholar] [CrossRef]
- Sjodin, H.; Wilder-Smith, A.; Osman, S.; Farooq, Z.; Rocklöv, J. Only strict quarantine measures can curb the coronavirus disease (COVID-19) outbreak in Italy, 2020. Eurosurveillance 2020, 25, 2000280. [Google Scholar] [CrossRef]
- Zhang, H. The Influence of the Ongoing COVID-19 Pandemic on Family Violence in China. J. Fam. Violence 2020, 37, 733–743. [Google Scholar] [CrossRef]
- Asanov, I.; Flores, F.; McKenzie, D.; Mensmann, M.; Schulte, M. Remote-learning, time-use, and mental health of Ecuadorian high-school students during the COVID-19 quarantine. World Dev. 2021, 138, 105225. [Google Scholar] [CrossRef]
- Farre, L.; Fawaz, Y.; Gonzalez, L.; Graves, J. How the COVID-19 Lockdown Affected Gender Inequality in Paid and Unpaid Work in Spain; IZA Discussion Paper 13434; IZA: Bonn, Germany, 2020. [Google Scholar]
- Gostin, L.O.; Wiley, L.F. Governmental public health powers during the COVID-19 pandemic: Stay-at-home orders, business closures, and travel restrictions. JAMA 2020, 323, 2137–2138. [Google Scholar] [CrossRef] [PubMed]
- Khan, N.; Fahad, S.; Faisal, S.; Naushad, M. Quarantine role in the control of corona virus in the world and its impact on the world economy. SSRN Electron. J. 2020. [Google Scholar] [CrossRef]
- Verma, S.; Gustafsson, A. Investigating the emerging COVID-19 research trends in the field of business and management: A bibliometric analysis approach. J. Bus. Res. 2020, 118, 253–261. [Google Scholar] [CrossRef]
- Koçak, O.; Koçak, Ö.E.; Younis, M.Z. The psychological consequences of COVID-19 fear and the moderator effects of individuals’ underlying illness and witnessing infected friends and family. Int. J. Environ. Res. Public Health 2021, 18, 1836. [Google Scholar] [CrossRef] [PubMed]
- Mumbardo-Adam, C.; Barnet-Lopez, S.; Balboni, G. How have youth with Autism Spectrum Disorder managed quarantine derived from COVID-19 pandemic? An approach to families perspectives. Res. Dev. Disabil. 2021, 110, 103860. [Google Scholar] [CrossRef] [PubMed]
- Kołodziejczyk, A.; Misiak, B.; Szcześniak, D.; Maciaszek, J.; Ciułkowicz, M.; Łuc, D.; Wieczorek, T.; Fila-Witecka, K.; Chladzinska-Kiejna, S.; Rymaszewska, J. Coping Styles, Mental Health, and the COVID-19 Quarantine: A Nationwide Survey in Poland. Front. Psychiatry 2021, 12, 106. [Google Scholar] [CrossRef]
- Maciaszek, J.; Ciulkowicz, M.; Misiak, B.; Szczesniak, D.; Luc, D.; Wieczorek, T.; Fila-Witecka, K.; Gawlowski, P.; Rymaszewska, J. Mental Health of Medical and Non-Medical Professionals during the Peak of the COVID-19 Pandemic: A Cross-Sectional Nationwide Study. J. Clin. Med. 2020, 9, 2527. [Google Scholar] [CrossRef]
- Marin, F.-X.; Rusinol, J.; Gallifa, J. Pseudoscientific beliefs and psychopathological risks increase after COVID-19 social quarantine. Glob. Health 2020, 16, 72. [Google Scholar] [CrossRef]
- Martinotti, G.; Alessi, M.C.; Di Natale, C.; Sociali, A.; Ceci, F.; Lucidi, L.; Picutti, E.; Di Carlo, F.; Corbo, M.; Vellante, F.; et al. Psychopathological Burden and Quality of Life in Substance Users During the COVID-19 Lockdown Period in Italy. Front. Psychiatry 2020, 11, 572245. [Google Scholar] [CrossRef]
- Orgiles, M.; Morales, A.; Delvecchio, E.; Francisco, R.; Mazzeschi, C.; Pedro, M.; Espada, J.P. Coping behaviors and psychological disturbances in youth affected by the COVID-19 health crisis. Front. Psychol. 2021, 12, 565657. [Google Scholar] [CrossRef]
- Al-Khanini, M.b.A. Impact of COVID-19 on the management of household income and consumption spending in Saudi Arabia. Int. J. Manag. 2021, 12, 938–951. [Google Scholar]
- Chung, S.J.; Tan, E.K.; Kee, T.; Krishnamoorthy, T.L.; Phua, G.C.; Sewa, D.W.; Ong, B.-H.; Tan, T.E.; Sivathasan, C.; Gan, H.L.V. Practical considerations for solid organ transplantation during the COVID-19 global outbreak: The experience from Singapore. Transplant. Direct 2020, 6, e554. [Google Scholar] [CrossRef] [PubMed]
- Lombardi, A.; Bozzi, G.; Mangioni, D.; Muscatello, A.; Peri, A.M.; Taramasso, L.; Ungaro, R.; Bandera, A.; Gori, A. Duration of quarantine in hospitalized patients with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection: A question needing an answer. J. Hosp. Infect. 2020, 105, 404–405. [Google Scholar] [CrossRef]
- Ali, I.; Alharbi, O.M. COVID-19: Disease, management, treatment, and social impact. Sci. Total Environ. 2020, 728, 138861. [Google Scholar] [CrossRef]
- Garcovich, S.; Bersani, F.; Chiricozzi, A.; De Simone, C. Mass quarantine measures in the time of COVID-19 pandemic: Psychosocial implications for chronic skin conditions and a call for qualitative studies. J. Eur. Acad. Dermatol. Venereol. 2020, 34, e293–e294. [Google Scholar] [CrossRef]
- Ilyas, S.; Srivastava, R.R.; Kim, H. Disinfection technology and strategies for COVID-19 hospital and bio-medical waste management. Sci. Total Environ. 2020, 749, 141652. [Google Scholar] [CrossRef] [PubMed]

| Main Themes | Sub-Themes | Frequency | Percent |
|---|---|---|---|
| Life threats | Death (increasing number of deaths) | 123 | 12.31% |
| Life-threatening disease | 32 | 3.20% | |
| Highly infectious | 269 | 26.93% | |
| Shortage of support | Shortage of vaccine/treatment | 52 | 5.21% |
| Unavailability of enough healthcare | 29 | 2.90% | |
| Economic impact | Lockdown and quarantine | 31 | 3.10% |
| Economic shutdown | 52 | 5.21% | |
| Joblessness | 47 | 4.70% | |
| Family and social life | Anxious about family | 19 | 1.90% |
| Imbalance in social life | 32 | 3.20% | |
| Total | 686 | 68.67% |
| Main Theme | Sub-Themes | Frequency | Percent | Cumulative Percent |
|---|---|---|---|---|
| Effects associated with the quarantine | Academic and schooling life interruption | 190 | 19.0% | 19.0% |
| Family life and friendship interruption | 29 | 2.9% | 21.9% | |
| Job/work and business interruption | 95 | 9.5% | 31.4% | |
| Mixed issues (miscellaneous) | 198 | 19.8% | 51.2% | |
| Psychopathological pressure | 102 | 10.2% | 61.4% | |
| Movement restrictions | 35 | 3.5% | 64.9% | |
| Idly staying at home | 51 | 5.1% | 70.0% | |
| Income loss or no income | 39 | 3.9% | 73.9% | |
| Time management | 12 | 1.2% | 75.1% | |
| No travel or tour | 15 | 1.5% | 76.6% |
| Sum of Squares | df | Mean Square | F | Sig. | Eta Value | Eta Square Value | ||
|---|---|---|---|---|---|---|---|---|
| Mean_PHQ | Between groups | 33.155 | 56 | 0.592 | 1.251 | 0.106 | 0.263 | 0.069 |
| Within groups | 445.673 | 942 | 0.473 | |||||
| Total | 478.828 | 998 | ||||||
| MeanGAD | Between groups | 31.891 | 56 | 0.569 | 1.329 | 0.057 | 0.271 | 0.073 |
| Within groups | 403.620 | 942 | 0.428 | |||||
| Total | 435.511 | 998 | ||||||
| Mean_ISI | Between groups | 24.959 | 56 | 0.446 | 0.934 | 0.614 | 0.229 | 0.053 |
| Within groups | 449.646 | 942 | 0.477 | |||||
| Total | 474.606 | 998 | ||||||
| Mean_IESR | Between groups | 32.379 | 56 | 0.578 | 1.056 | 0.366 | 0.243 | 0.059 |
| Within groups | 515.578 | 942 | 0.547 | |||||
| Total | 547.958 | 998 |
| Construct/Items | Factor Loadings | Alpha | CR | AVE | R Square |
|---|---|---|---|---|---|
| GAD1 | 0.667 | 0.89 | 0.91 | 0.52 | 0.54 |
| GAD2 | 0.807 | ||||
| GAD3 | 0.703 | ||||
| GAD4 | 0.765 | ||||
| GAD5 | 0.704 | ||||
| GAD6 | 0.762 | ||||
| GAD7 | 0.763 | ||||
| GAD8 | 0.682 | ||||
| GAD10 | 0.638 | ||||
| GAD1 | 0.667 | ||||
| IESR1 | 0.660 | 0.93 | 0.94 | 0.52 | |
| IESR2 | 0.731 | ||||
| IESR3 | 0.751 | ||||
| IESR4 | 0.761 | ||||
| IESR6 | 0.745 | ||||
| IESR9 | 0.702 | ||||
| IESR10 | 0.742 | ||||
| IESR12 | 0.712 | ||||
| IESR14 | 0.702 | ||||
| IESR15 | 0.711 | ||||
| IESR16 | 0.798 | ||||
| IESR17 | 0.651 | ||||
| IESR18 | 0.758 | ||||
| IESR19 | 0.696 | ||||
| ISI1 | 0.828 | 0.89 | 0.91 | 0.65 | |
| ISI2 | 0.789 | ||||
| ISI3 | 0.674 | ||||
| ISI5 | 0.806 | ||||
| ISI6 | 0.870 | ||||
| ISI7 | 0.857 | ||||
| PHQ1 | 0.760 | 0.89 | 0.92 | 0.61 | |
| PHQ2 | 0.809 | ||||
| PHQ3 | 0.813 | ||||
| PHQ4 | 0.799 | ||||
| PHQ5 | 0.789 | ||||
| PHQ6 | 0.767 | ||||
| PHQ7 | 0.724 |
| Fornell-Larcker Criterion | Heterotrait-Monotrait Ratio (HTMT) | |||||||
|---|---|---|---|---|---|---|---|---|
| GAD | IES-R | ISI | PHQ | GAD | IES-R | ISI | PHQ | |
| GAD | 0.723 | |||||||
| IESR | 0.643 | 0.724 | 0.686 | |||||
| ISI | 0.709 | 0.663 | 0.806 | 0.797 | 0.698 | |||
| PHQ | 0.708 | 0.627 | 0.570 | 0.781 | 0.792 | 0.675 | 0.636 | |
| Hypotheses | Path Coefficient | Standard Deviation | T Statistics | p-Values | VIF | Lower Limit | Upper Limit | Decision |
|---|---|---|---|---|---|---|---|---|
| GAD -> IESR | 0.168 | 0.040 | 4.100 | <0.001 | 2.057 | 0.096 | 0.246 | Accepted |
| ISI -> IESR | 0.381 | 0.032 | 11.19 | <0.001 | 2.793 | 0.306 | 0.437 | Accepted |
| PHQ -> IESR | 0.290 | 0.034 | 8.11 | <0.001 | 2.002 | 0.222 | 0.355 | Accepted |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aljaberi, M.A.; Al-Sharafi, M.A.; Uzir, M.U.H.; Sabah, A.; Ali, A.M.; Lee, K.-H.; Alsalahi, A.; Noman, S.; Lin, C.-Y. Psychological Toll of the COVID-19 Pandemic: An In-Depth Exploration of Anxiety, Depression, and Insomnia and the Influence of Quarantine Measures on Daily Life. Healthcare 2023, 11, 2418. https://doi.org/10.3390/healthcare11172418
Aljaberi MA, Al-Sharafi MA, Uzir MUH, Sabah A, Ali AM, Lee K-H, Alsalahi A, Noman S, Lin C-Y. Psychological Toll of the COVID-19 Pandemic: An In-Depth Exploration of Anxiety, Depression, and Insomnia and the Influence of Quarantine Measures on Daily Life. Healthcare. 2023; 11(17):2418. https://doi.org/10.3390/healthcare11172418
Chicago/Turabian StyleAljaberi, Musheer A., Mohammed A. Al-Sharafi, Md. Uzir Hossain Uzir, Aiche Sabah, Amira Mohammed Ali, Kuo-Hsin Lee, Abdulsamad Alsalahi, Sarah Noman, and Chung-Ying Lin. 2023. "Psychological Toll of the COVID-19 Pandemic: An In-Depth Exploration of Anxiety, Depression, and Insomnia and the Influence of Quarantine Measures on Daily Life" Healthcare 11, no. 17: 2418. https://doi.org/10.3390/healthcare11172418
APA StyleAljaberi, M. A., Al-Sharafi, M. A., Uzir, M. U. H., Sabah, A., Ali, A. M., Lee, K.-H., Alsalahi, A., Noman, S., & Lin, C.-Y. (2023). Psychological Toll of the COVID-19 Pandemic: An In-Depth Exploration of Anxiety, Depression, and Insomnia and the Influence of Quarantine Measures on Daily Life. Healthcare, 11(17), 2418. https://doi.org/10.3390/healthcare11172418











