Clinical Efficiency and Acceptability of EMDR and MOSAIC Therapy for PTSD
Abstract
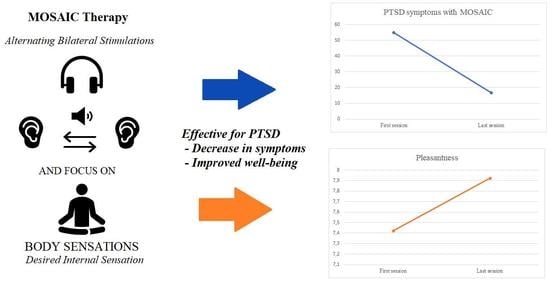
1. Clinical Efficiency and Acceptability of EMDR and MOSAIC Therapy for PTSD
2. Materials and Methods
2.1. Participants
2.2. Psychometric Scales
2.3. Procedure
2.4. Statistical Analysis
3. Results
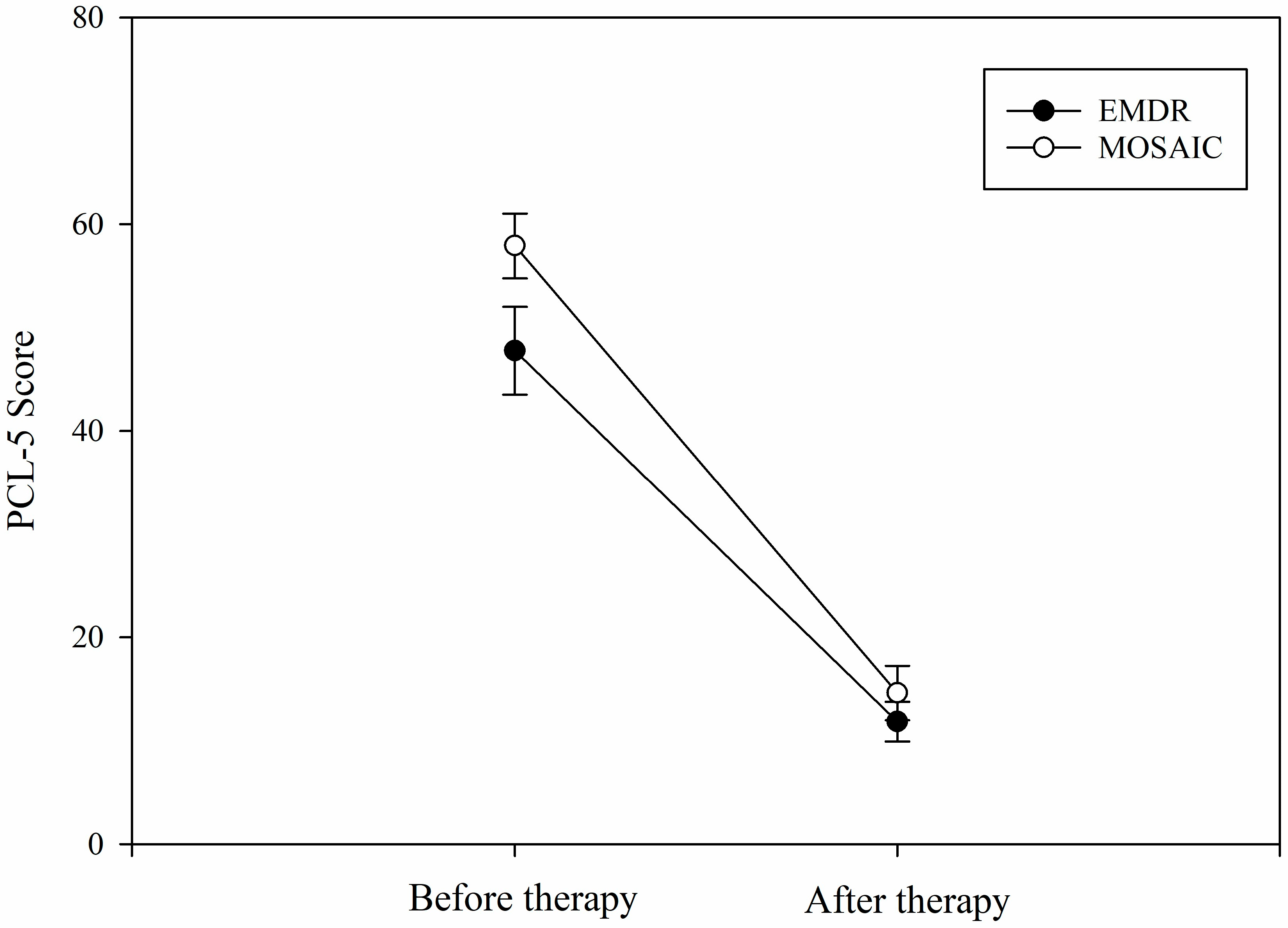
3.1. PCL-5
3.2. Number of Sessions
3.3. Pleasantness Scale
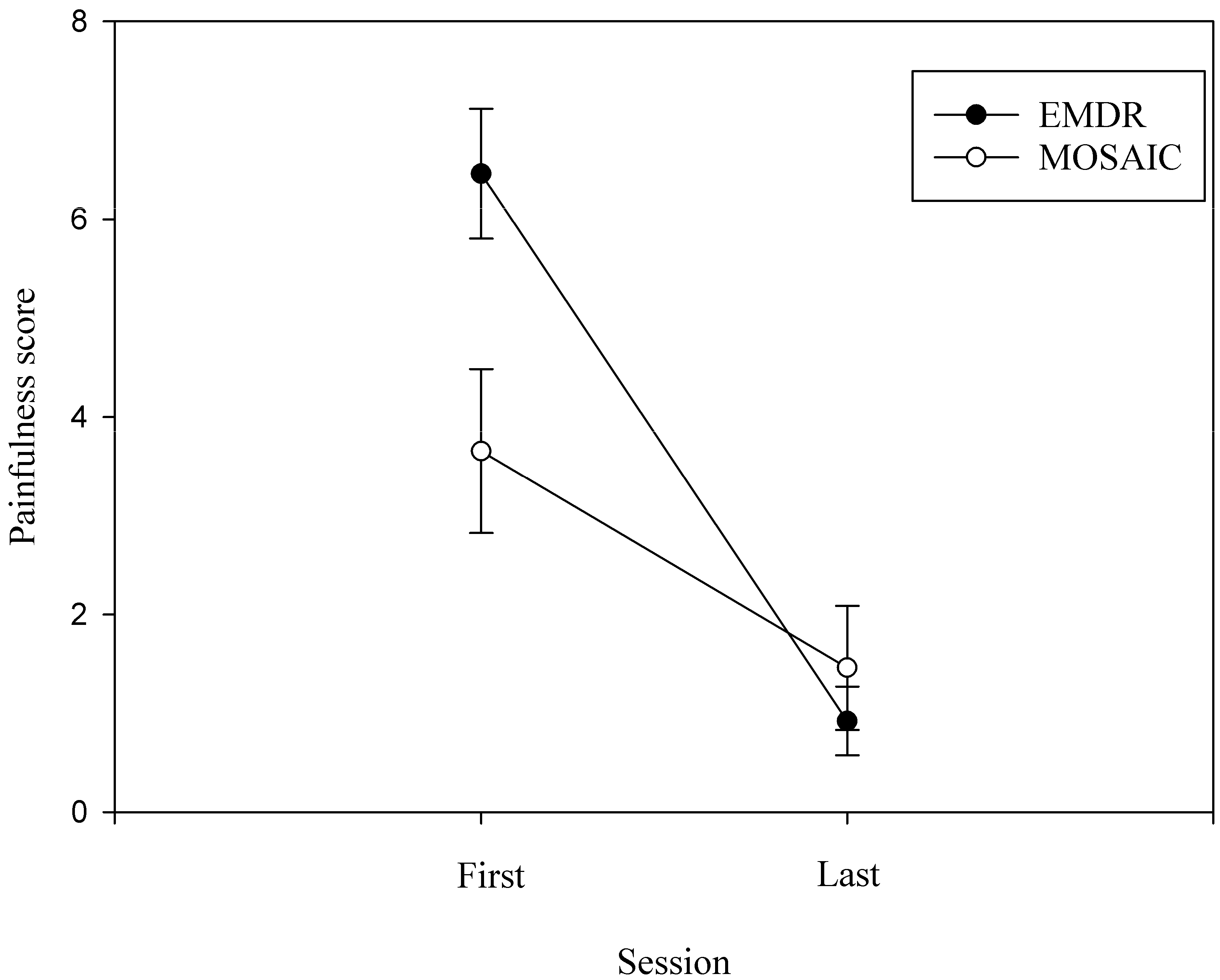
3.4. Painfulness Scale
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association Publishing: Arlington, VA, USA, 2013. [Google Scholar] [CrossRef]
- Kessler, R.C.; Sonnega, A.; Bromet, E.; Hughes, M.; Nelson, C.B. Posttraumatic Stress Disorder in the National Comorbidity Survey. Arch. Gen. Psychiatry 1995, 52, 1048–1060. [Google Scholar] [CrossRef] [PubMed]
- Klein Breteler, J.; Ikani, N.; Becker, E.; Spijker, J.; Hendriks, G. Comorbid depression and treatment of anxiety disorders, OCD, and PTSD: Diagnosis versus severity. J. Affect. Disord. 2021, 295, 1005–1011. [Google Scholar] [CrossRef] [PubMed]
- Perkonigg, A.; Kessler, R.C.; Storz, S.; Wittchen, H.-U. Traumatic events and post-traumatic stress disorder in the community: Prevalence, risk factors and comorbidity. Acta Psychiatr. Scand. 2000, 101, 46–59. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Guidelines for the Management of Conditions Specifically Related to Stress. 2013. Available online: https://apps.who.int/iris/bitstream/handle/10665/85119/9789241505406_eng.pdf (accessed on 31 January 2022).
- El-Hage, W. Prise en charge des troubles post-traumatiques. Rhizome 2018, 69–70, 10–11. [Google Scholar] [CrossRef]
- Foa, E.B.; Hembree, E.; Rothbaum, B.O. Prolonged Exposure Therapy for PTSD—Therapist Guide; Oxford University Press: Oxford, UK, 2007. [Google Scholar]
- Foa, E.B.; Kozak, M.J. Emotional processing of fear: Exposure to corrective information. Psychol. Bull. 1986, 99, 20–35. [Google Scholar] [CrossRef]
- Cohen, J.A.; Mannarino, A.P.; Deblinger, E. Treating Trauma and Traumatic Grief in Children and Adolescents, 2nd ed.; Guilford Press: New York, NY, USA, 2017. [Google Scholar]
- Resick, P.A.; Monson, C.M.; Chard, K.M. Cognitive Processing Therapy for PTSD: A Comprehensive Manual; Guilford Press: New York, NY, USA, 2016. [Google Scholar]
- Lecomte, C.; Servant, D. Les Thérapies Comportementales, Cognitives et Emotionnelles en 150 Fiches; Elsevier Masson: Issy-les-Moulineaux, France, 2020. [Google Scholar] [CrossRef]
- Shapiro, F. Eye movement desensitization and reprocessing (EMDR): Evaluation of controlled PTSD research. J. Behav. Ther. Exp. Psychiatry 1996, 27, 209–218. [Google Scholar] [CrossRef]
- Servan-Schreiber, D.; Schooler, J.; Dew, M.A.; Carter, C.; Bartone, P. Eye movement desensitization and reprocessing for posttraumatic stress disorder: A pilot blinded, randomized study of stimulation type. Psychother. Psychosom. 2006, 75, 290–297. [Google Scholar] [CrossRef]
- Shapiro, F. Eye Movement Desensitization and Reprocessing (EMDR) Therapy: Basic Principles, Protocols, and Procedures, 3rd ed.; Guilford Press: New York, NY, USA, 2001; Available online: https://www.guilford.com/books/Eye-Movement-Desensitization-and-Reprocessing-EMDR-Therapy/Francine-Shapiro/9781462532766 (accessed on 17 October 2022).
- Shapiro, F. Manuel d’EMDR (Intégration Neuro-Emotionnelle par les Mouvements Oculaires) Principes, Protocoles, Procédures; Dunod: Paris, France, 2007. [Google Scholar]
- Shapiro, F. The Role of Eye Movement Desensitization and Reprocessing (EMDR) Therapy in Medicine: Addressing the Psychological and Physical Symptoms Stemming from Adverse Life Experiences. Perm. J. 2014, 18, 71–77. [Google Scholar] [CrossRef]
- Lewis, C.; Roberts, N.P.; Gibson, S.; Bisson, J.I. Dropout from psychological therapies for post-traumatic stress disorder (PTSD) in adults: Systematic review and meta-analysis. Eur. J. Psychotraumatology 2020, 11, 1709709. [Google Scholar] [CrossRef]
- Mavranezouli, I.; Megnin-Viggars, O.; Daly, C.; Dias, S.; Welton, N.J.; Stockton, S.; Bhutani, G.; Grey, N.; Leach, J.; Greenberg, N.; et al. Psychological treatments for post-traumatic stress disorder in adults: A network meta-analysis. Psychol. Med. 2020, 50, 542–555. [Google Scholar] [CrossRef]
- Hembree, E.A.; Foa, E.B.; Dorfan, N.M.; Street, G.P.; Kowalski, J.; Tu, X. Do patients drop out prematurely from exposure therapy for PTSD? J. Trauma. Stress 2003, 16, 555–562. [Google Scholar] [CrossRef]
- Varker, T.; Jones, K.A.; Arjmand, H.-A.; Hinton, M.; Hiles, S.A.; Freijah, I.; Forbes, D.; Kartal, D.; Phelps, A.; Bryant, R.A.; et al. Dropout from guideline-recommended psychological treatments for posttraumatic stress disorder: A systematic review and meta-analysis. J. Affect. Disord. Rep. 2021, 4, 100093. [Google Scholar] [CrossRef]
- Pearlman, L.A.; Saakvitne, K.W. Trauma and the Therapist: Countertransference and Vicarious Traumatization in Psychotherapy with Incest Survivors; Norton: New York, NY, USA, 1995. [Google Scholar]
- Boyd, J.E.; Lanius, R.A.; McKinnon, M.C. Mindfulness-based treatments for posttraumatic stress disorder: A review of the treatment literature and neurobiological evidence. J. Psychiatry Neurosci. 2018, 43, 7–25. [Google Scholar] [CrossRef]
- Shea, M.T.; Krupnick, J.L.; Belsher, B.E.; Schnurr, P.P. Non-Trauma-Focused Psychotherapies for the Treatment of PTSD: A Descriptive Review. Curr. Treat. Options Psychiatry 2020, 7, 242–257. [Google Scholar] [CrossRef]
- Simpson, T.L.; Goldberg, S.B.; Louden, D.K.; Blakey, S.M.; Hawn, S.E.; Lott, A.; Browne, K.C.; Lehavot, K.; Kaysen, D. Efficacy and acceptability of interventions for co-occurring PTSD and SUD: A meta-analysis. J. Anxiety Disord. 2021, 84, 102490. [Google Scholar] [CrossRef]
- Yager, J. Non-Trauma-Focused Therapies for Posttraumatic Stress Disorder. Focus 2018, 16, 7s. [Google Scholar] [CrossRef] [PubMed]
- Scheel, M.J.; Hanson, W.E.; Razzhavaikina, T.I. The Process of Recommending Homework in Psychotherapy: A Review of Therapist Delivery Methods, Client Acceptability, and Factors That Affect Compliance. Psychotherapy 2004, 41, 38–55. [Google Scholar] [CrossRef]
- Jericho, B.; Luo, A.; Berle, D. Trauma-focused psychotherapies for post-traumatic stress disorder: A systematic review and network meta-analysis. Acta Psychiatr. Scand. 2021, 145, 132–155. [Google Scholar] [CrossRef]
- Khalfa, S. De l’EMDR à la Thérapie MOSAIC. Guérir Sans Douleur les Traumatismes Psychologiques; Independently Published: Paris, France, 2021. [Google Scholar]
- Khalfa, S.; Poupard, G. MOSAIC: A New Pain-Free Psychotherapy for Psychological Trauma. Am. J. Psychother. 2021, 74, 40–43. [Google Scholar] [CrossRef]
- Corcoran, J.; Pillai, V. A Review of the Research on Solution-Focused Therapy. Br. J. Soc. Work. 2007, 39, 234–242. [Google Scholar] [CrossRef]
- Hendricks, M.N. Focusing-Oriented Experiential Psychotherapy: How To Do It. Am. J. Psychother. 2007, 61, 271–284. [Google Scholar] [CrossRef]
- Khalfa, S.; Touzet, C.F. EMDR therapy mechanisms explained by the theory of neural cognition. J. Trauma. Stress Disord. Treat. 2017, 4, 2. [Google Scholar] [CrossRef]
- McDonnell, M.D.; Abbott, D. What is stochastic resonance? Definitions, misconceptions, debates, and its relevance to biology. PLoS Comput. Biol. 2009, 5, e1000348. [Google Scholar] [CrossRef] [PubMed]
- Rousseau, P.-F.; Boukezzi, S.; Garcia, R.; Chaminade, T.; Khalfa, S. Cracking the EMDR code: Recruitment of sensory, memory and emotional networks during bilateral alternating auditory stimulation. Aust. N. Z. J. Psychiatry 2020, 54, 818–831. [Google Scholar] [CrossRef] [PubMed]
- Ward, L.M.; MacLean, S.E.; Kirschner, A. Stochastic resonance modulates neural synchronization within and between cortical sources. PLoS ONE 2010, 5, e14371. [Google Scholar] [CrossRef] [PubMed]
- Miller, P.W.; McGowan, I.W.; Bergmann, U.; Farrell, D.; McLaughlin, D.F. Stochastic resonance as a proposed neurobiological model for Eye Movement Desensitization and Reprocessing (EMDR) therapy. Med. Hypotheses 2018, 121, 106–111. [Google Scholar] [CrossRef]
- Johansen, J.P.; Diaz-Mataix, L.; Hamanaka, H.; Ozawa, T.; Ycu, E.; Koivumaa, J.; Kumar, A.; Hou, M.; Deisseroth, K.; Boyden, E.S.; et al. Hebbian and neuromodulatory mechanisms interact to trigger associative memory formation. Proc. Natl. Acad. Sci. USA 2014, 111, E5584–E5592. [Google Scholar] [CrossRef]
- Khalfa, S. Prise en charge du traumatisme psychique par la thérapie EMDR et mécanismes cérébraux impliqués. Rev. de Neuropsychol. 2019, 4, 267–272. [Google Scholar] [CrossRef]
- Gunter, R.W.; Bodner, G.E. How eye movements affect unpleasant memories: Support for a working-memory account. Behav. Res. Ther. 2008, 46, 913–931. [Google Scholar] [CrossRef]
- Landin-Romero, R.; Moreno-Alcazar, A.; Pagani, M.; Amann, B.L. How Does Eye Movement Desensitization and Reprocessing Therapy Work? A Systematic Review on Suggested Mechanisms of Action. Front. Psychol. 2018, 9, 1395. [Google Scholar] [CrossRef]
- Van den Hout, M.A.; Engelhard, I.M. How does EMDR work? J. Exp. Psychopathol. 2012, 3, 724–738. [Google Scholar] [CrossRef]
- Ashbaugh, A.R.; Houle-Johnson, S.A.; Herbert, C.; El-Hage, W.; Brunet, A. Psychometric Validation of the English and French Versions of the Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5). PLoS ONE 2016, 11, e0161645. [Google Scholar] [CrossRef] [PubMed]
- Bovin, M.J.; Marx, B.P.; Weathers, F.W.; Gallagher, M.W.; Rodriguez, P.; Schnurr, P.P.; Keane, T.M. Psychometric properties of the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders–Fifth Edition (PCL-5) in veterans. Psychol. Assess. 2016, 28, 1379–1391. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Releases New International Classification of Diseases (ICD 11). 2018. Available online: http://www.who.int/news-room/detail/18-06-2018-who-releases-new-international-classification-of-diseases-(icd-11) (accessed on 14 September 2022).
- Flatot-Blin. Clinical Efficiency and Pleasantness of EMDR and MOSAIC Therapy for PTSD. Available online: https://osf.io/x8gu4/ (accessed on 3 November 2022). [CrossRef]
- Abdi, H. Bonferroni and Šidák corrections for multiple comparisons. Encycl. Meas. Stat. 2017, 3, 103–107. [Google Scholar]
- Elton, J.; Stage, K.; Nielsen, A.B.S.; Svendsen, A.L.H. The experience of Basic Body Awareness Therapy and its transfer to daily life amongst Danish military veterans with PTSD. J. Bodyw. Mov. Ther. 2021, 28, 202–211. [Google Scholar] [CrossRef] [PubMed]
- Gibert, L.; El Hage, W.; Verdonk, C.; Levy, B.; Falissard, B.; Trousselard, M. The negative association between trait mindfulness and post-traumatic stress disorder: A 4.5-year prospective cohort study. Brain Behav. 2021, 11, e02163. [Google Scholar] [CrossRef]
- Hildebrand, M.W.O.; Host, H.H.; Binder, E.F.; Carpenter, B.; Freedland, K.E.; Morrow-Howell, N.; Baum, C.M.; Doré, P.M.; Lenze, E.J. Measuring Treatment Fidelity in a Rehabilitation Intervention Study. Am. J. Phys. Med. Rehabil. 2012, 91, 715–724. [Google Scholar] [CrossRef]

| EMDR | MOSAIC | p-Value | |
|---|---|---|---|
| Socio-demographic characteristics | |||
| Male | n = 6 | n = 3 | |
| Female | n = 7 | n = 10 | |
| Age (years) | 38.2 (12) | 37.4 (13.7) | ns |
| Education level (years) | 12.9 (2.3) | 13.5 (2) | ns |
| Psychometric scores | |||
| Number of sessions | 3.1 (1.7) | 5.4 (2.4) | 0.008 |
| Delay between traumatic event and therapy (days) | 533.3 (511) | 924.7 (1435) | ns |
| Duration of therapy (days) | 17.3 (10.8) | 51.6 (35.7) | 0.005 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Flatot-Blin, D.; Rey, A.; Derynck, F.; Fossard, O.; Khalfa, S. Clinical Efficiency and Acceptability of EMDR and MOSAIC Therapy for PTSD. Healthcare 2023, 11, 2226. https://doi.org/10.3390/healthcare11152226
Flatot-Blin D, Rey A, Derynck F, Fossard O, Khalfa S. Clinical Efficiency and Acceptability of EMDR and MOSAIC Therapy for PTSD. Healthcare. 2023; 11(15):2226. https://doi.org/10.3390/healthcare11152226
Chicago/Turabian StyleFlatot-Blin, Deborah, Arnaud Rey, Flavie Derynck, Olivier Fossard, and Stephanie Khalfa. 2023. "Clinical Efficiency and Acceptability of EMDR and MOSAIC Therapy for PTSD" Healthcare 11, no. 15: 2226. https://doi.org/10.3390/healthcare11152226
APA StyleFlatot-Blin, D., Rey, A., Derynck, F., Fossard, O., & Khalfa, S. (2023). Clinical Efficiency and Acceptability of EMDR and MOSAIC Therapy for PTSD. Healthcare, 11(15), 2226. https://doi.org/10.3390/healthcare11152226