Assistive Technology Involving Postural Control and Gait Performance for Adults with Stroke: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Review Design
2.2. Eligibility Criteria
2.3. Information Sources and Search Strategy
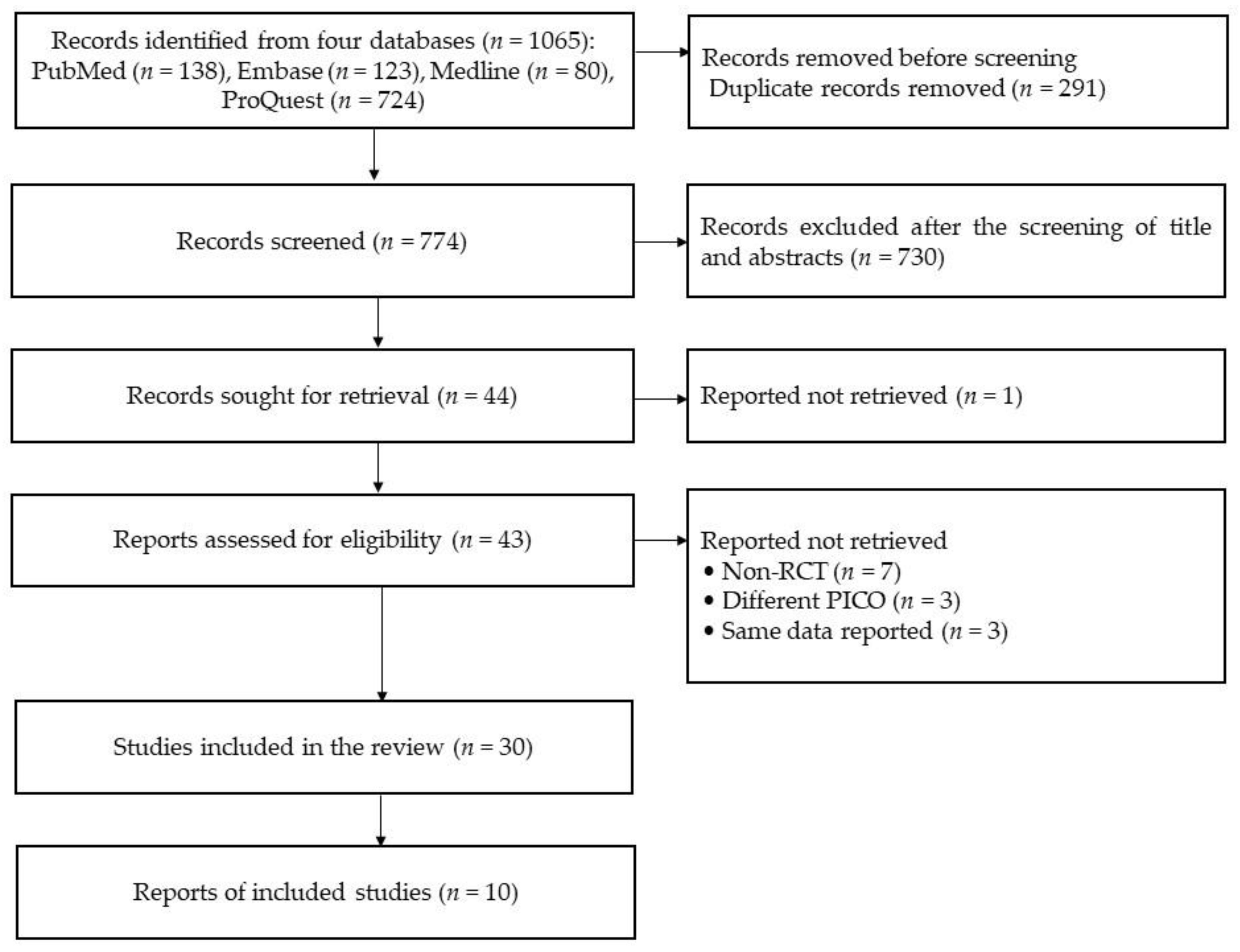
2.4. Screening of Searched Studies
2.5. Data Extraction
2.6. Data Analysis
3. Results
3.1. Literature Characteristics of Included RCTs
3.2. Qualitative Synthesis of Selected RCTs to Review Postural Control and Gait Performance in Stroke Survivors
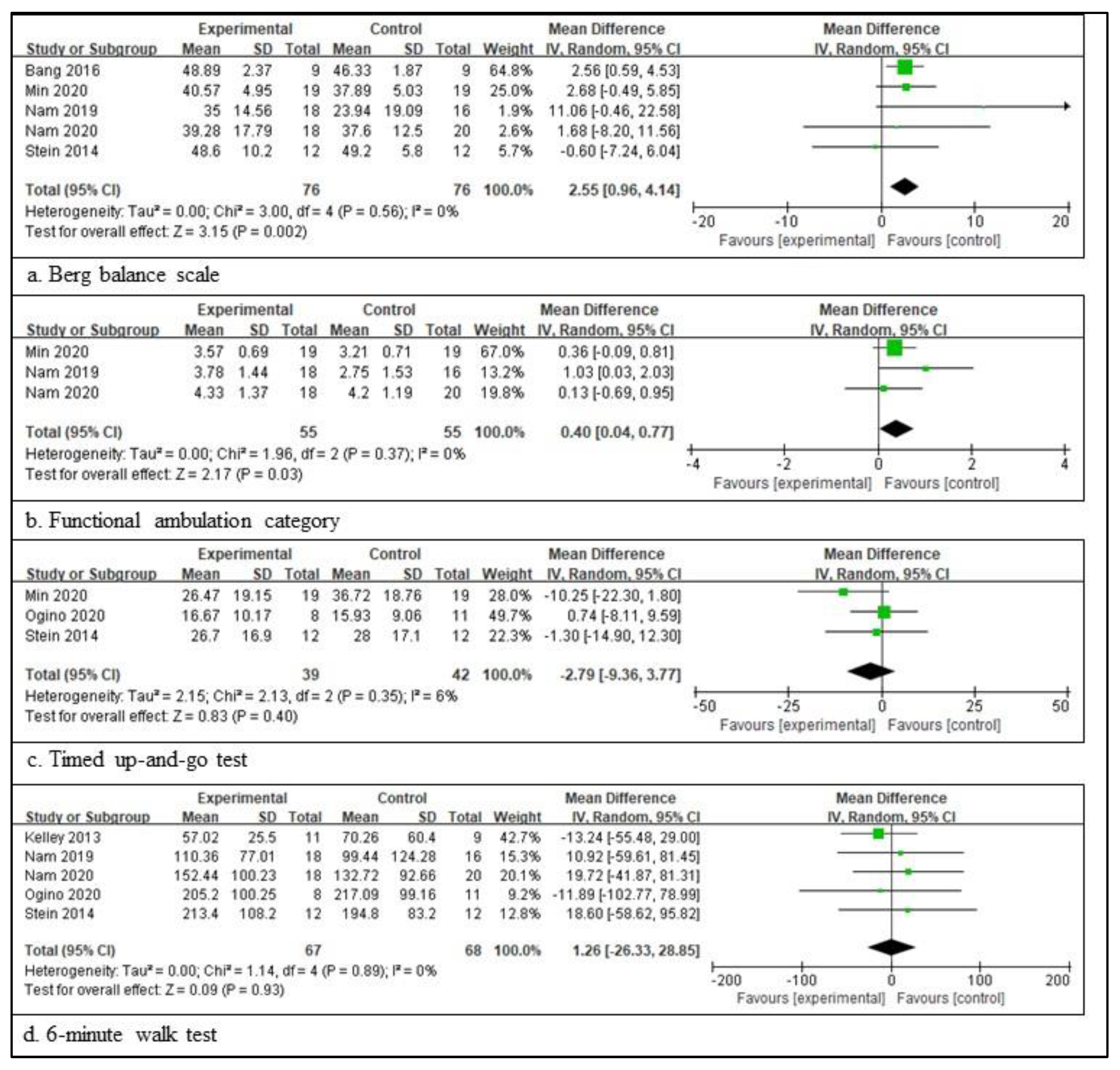
3.3. Effectiveness of Assistive Technology Device on Postural Control and Gait Performance in the RCT Studies
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Li, S.; Francisco, G.E.; Zhou, P. Post-Stroke Hemiplegic Gait: New Perspective and Insights. Front. Physiol. 2018, 9, 1021. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Selves, C.; Stoquart, G.; Lejeune, T. Gait Rehabilitation after Stroke: Review of the Evidence of Predictors, Clinical Outcomes and Timing for Interventions. Acta Neurol. Belg. 2020, 120, 783–790. [Google Scholar] [CrossRef] [PubMed]
- Bizovičar, N.; Matjačić, Z.; Stanonik, I.; Goljar, N. Overground Gait Training Using a Motorized Assistive Device in Patients with Severe Disabilities after Stroke. Int. J. Rehabil. Res. 2017, 40, 46–52. [Google Scholar] [CrossRef]
- Mohan, D.M.; Khandoker, A.H.; Wasti, S.A.; Ismail Ibrahim Ismail Alali, S.; Jelinek, H.F.; Khalaf, K. Assessment Methods of Post-Stroke Gait: A Scoping Review of Technology-Driven Approaches to Gait Characterization and Analysis. Front. Neurol. 2021, 12, 650024. [Google Scholar] [CrossRef]
- Cirstea, C.M. Gait Rehabilitation after Stroke. Stroke 2020, 51, 2892–2894. [Google Scholar] [CrossRef]
- Perry, J.; Burnfield, J. Gait Analysis: Normal and Pathological Function, 2nd ed.; Slack Incorporated: West Deptford, NJ, USA, 2010; ISBN 9781556427664. [Google Scholar]
- Karakkattil, P.S.; Trudelle-Jackson, E.; Medley, A.; Swank, C. Effects of Two Different Types of Ankle–Foot Orthoses on Gait Outcomes in Patients with Subacute Stroke: A Randomized Crossover Trial. Clin. Rehabil. 2020, 34, 1094–1102. [Google Scholar] [CrossRef]
- Huizenga, D.; Rashford, L.; Darcy, B.; Lundin, E.; Medas, R.; Shultz, S.T.; DuBose, E.; Reed, K.B. Wearable Gait Device for Stroke Gait Rehabilitation at Home. Top. Stroke Rehabil. 2021, 28, 443–455. [Google Scholar] [CrossRef]
- Caro, C.C.; Costa, J.D.; Cruz, D.M.C.d. The Use of Mobility Assistive Devices and the Functional Independence in Stroke Patients. Cad. Bras. Ter. Ocup. 2018, 26, 558–568. [Google Scholar] [CrossRef] [Green Version]
- Tyson, S.F.; Rogerson, L. Assistive Walking Devices in Nonambulant Patients Undergoing Rehabilitation after Stroke: The Effects on Functional Mobility, Walking Impairments, and Patients’ Opinion. Arch. Phys. Med. Rehabil. 2009, 90, 475–479. [Google Scholar] [CrossRef]
- Morris, L.; Cramp, M.; Turton, A. User Perspectives on the Future of Mobility Assistive Devices: Understanding Users’ Assistive Device Experiences and Needs. J. Rehabil. Assist. Technol. Eng. 2022, 9, 205566832211147. [Google Scholar] [CrossRef]
- Jutai, J.; Coulson, S.; Teasell, R.; Bayley, M.; Garland, J.; Mayo, N.; Wood-Dauphinee, S. Mobility Assistive Device Utilization in a Prospective Study of Patients with First-Ever Stroke. Arch. Phys. Med. Rehabil. 2007, 88, 1268–1275. [Google Scholar] [CrossRef]
- S⊘rensen, H.V.; Lendal, S.; Schultz-Larsen, K.; Uhrskov, T. Stroke Rehabilitation: Assistive Technology Devices and Environmental Modifications Following Primary Rehabilitation in Hospital—A Therapeutic Perspective. Assist. Technol. 2003, 15, 39–48. [Google Scholar] [CrossRef] [PubMed]
- Taki, S.; Imura, T.; Iwamoto, Y.; Imada, N.; Tanaka, R.; Araki, H.; Araki, O. Effects of Exoskeletal Lower Limb Robot Training on the Activities of Daily Living in Stroke Patients: Retrospective Pre-Post Comparison Using Propensity Score Matched Analysis. J. Stroke Cerebrovasc. Dis. 2020, 29, 105176. [Google Scholar] [CrossRef] [PubMed]
- Forrester, L.W.; Roy, A.; Hafer-Macko, C.; Krebs, H.I.; Macko, R.F. Task-Specific Ankle Robotics Gait Training after Stroke: A Randomized Pilot Study. J. Neuroeng. Rehabil. 2016, 13, 51. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Nunen, M.P.M.; Gerrits, K.H.L.; Konijnenbelt, M.; Janssen, T.W.J.; De Haan, A. Recovery of Walking Ability Using a Robotic Device in Subacute Stroke Patients: A Randomized Controlled Study. Disabil. Rehabil. Assist. Technol. 2015, 10, 141–148. [Google Scholar] [CrossRef]
- Mate, K.K.V.; Abou-Sharkh, A.; Mansoubi, M.; Alosaimi, A.; Dawes, H.; Michael, W.; Stanwood, O.; Harding, S.; Gorenko, D.; Mayo, N.E. Evidence for the Efficacy of Commercially Available Wearable Biofeedback Gait Devices: Consumer-Centered Review. JMIR Rehabil. Assist. Technol. 2023, 10, e40680. [Google Scholar] [CrossRef]
- Eng, J.J.; Tang, P.-F. Gait Training Strategies to Optimize Walking Ability in People with Stroke: A Synthesis of the Evidence. Expert Rev. Neurother. 2007, 7, 1417–1436. [Google Scholar] [CrossRef] [Green Version]
- Mikolajczyk, T.; Ciobanu, I.; Badea, D.I.; Iliescu, A.; Pizzamiglio, S.; Schauer, T.; Seel, T.; Seiciu, P.L.; Turner, D.L.; Berteanu, M. Advanced Technology for Gait Rehabilitation: An Overview. Adv. Mech. Eng. 2018, 10, 168781401878362. [Google Scholar] [CrossRef]
- Stevenson, A.J.; Mrachacz-Kersting, N.; van Asseldonk, E.; Turner, D.L.; Spaich, E.G. Spinal Plasticity in Robot-Mediated Therapy for the Lower Limbs. J. Neuroeng. Rehabil. 2015, 12, 81. [Google Scholar] [CrossRef] [Green Version]
- Jezernik, S.; Colombo, G.; Keller, T.; Frueh, H.; Morari, M. Robotic Orthosis Lokomat: A Rehabilitation and Research Tool. Neuromodulation Technol. Neural Interface 2003, 6, 108–115. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Higgins, J.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.; Welck, V. Cochrane Handbook for Systematic Reviews of Interventions, 2nd ed.; John Wiley & Sons: Chichester, UK, 2019. [Google Scholar]
- Luo, D.; Wan, X.; Liu, J.; Tong, T. Optimally Estimating the Sample Mean from the Sample Size, Median, Mid-Range, and/or Mid-Quartile Range. Stat. Methods Med. Res. 2018, 27, 1785–1805. [Google Scholar] [CrossRef] [Green Version]
- Wan, X.; Wang, W.; Liu, J.; Tong, T. Estimating the Sample Mean and Standard Deviation from the Sample Size, Median, Range and/or Interquartile Range. BMC Med. Res. Methodol. 2014, 14, 135. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hozo, S.P.; Djulbegovic, B.; Hozo, I. Estimating the Mean and Variance from the Median, Range, and the Size of a Sample. BMC Med. Res. Methodol. 2005, 5, 13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nedergård, H.; Arumugam, A.; Sandlund, M.; Bråndal, A.; Häger, C.K. Effect of Robotic-Assisted Gait Training on Objective Biomechanical Measures of Gait in Persons Post-Stroke: A Systematic Review and Meta-Analysis. J. Neuroeng. Rehabil. 2021, 18, 64. [Google Scholar] [CrossRef]
- Alingh, J.F.; Fleerkotte, B.M.; Groen, B.E.; Rietman, J.S.; Weerdesteyn, V.; van Asseldonk, E.H.F.; Geurts, A.C.H.; Buurke, J.H. Effect of Assist-as-Needed Robotic Gait Training on the Gait Pattern Post Stroke: A Randomized Controlled Trial. J. Neuroeng. Rehabil. 2021, 18, 26. [Google Scholar] [CrossRef] [PubMed]
- Choi, Y.H.; Kim, N.H.; Son, S.M.; Cha, Y.J. Effects of Trunk Stabilization Exercise While Wearing a Pelvic Compression Belt on Walking and Balancing Abilities in Patients with Stroke. Am. J. Phys. Med. Rehabil. 2020, 99, 1048–1055. [Google Scholar] [CrossRef] [PubMed]
- De Sèze, M.P.; Bonhomme, C.; Daviet, J.C.; Burguete, E.; MacHat, H.; Rousseaux, M.; Mazaux, J.M. Effect of Early Compensation of Distal Motor Deficiency by the Chignon Ankle-Foot Orthosis on Gait in Hemiplegic Patients: A Randomized Pilot Study. Clin. Rehabil. 2011, 25, 989–998. [Google Scholar] [CrossRef]
- Forrester, L.W.; Roy, A.; Krywonis, A.; Kehs, G.; Krebs, H.I.; Macko, R.F. Modular Ankle Robotics Training in Early Subacute Stroke: A Randomized Controlled Pilot Study. Neurorehabil. Neural Repair 2014, 28, 678–687. [Google Scholar] [CrossRef] [Green Version]
- Han, E.Y.; Im, S.H.; Kim, B.R.; Seo, M.J.; Kim, M.O. Robot-Assisted Gait Training Improves Brachial-Ankle Pulse Wave Velocity and Peak Aerobic Capacity in Subacute Stroke Patients with Totally Dependent Ambulation Randomized Controlled Trial. Medicine 2016, 95, e5078. [Google Scholar] [CrossRef]
- Kim, J.Y.; Kim, D.Y.; Chun, M.H.; Kim, S.W.; Jeon, H.R.; Hwang, C.H.; Choi, J.K.; Bae, S. Effects of Robot-(Morning Walk®) Assisted Gait Training for Patients after Stroke: A Randomized Controlled Trial. Clin. Rehabil. 2019, 33, 516–523. [Google Scholar] [CrossRef] [PubMed]
- Monticone, M.; Ambrosini, E.; Ferrante, S.; Colombo, R. “Regent Suit” Training Improves Recovery of Motor and Daily Living Activities in Subjects with Subacute Stroke: A Randomized Controlled Trial. Clin. Rehabil. 2013, 27, 792–802. [Google Scholar] [CrossRef] [PubMed]
- Morone, G.; Annicchiarico, R.; Iosa, M.; Federici, A.; Paolucci, S.; Cortés, U.; Caltagirone, C. Overground Walking Training with the I-Walker, a Robotic Servo-Assistive Device, Enhances Balance in Patients with Subacute Stroke: A Randomized Controlled Trial. J. Neuroeng. Rehabil. 2016, 13, 47. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nikamp, C.D.M.; Buurke, J.H.; van der Palen, J.; Hermens, H.J.; Rietman, J.S. Six-Month Effects of Early or Delayed Provision of an Ankle-Foot Orthosis in Patients with (Sub)Acute Stroke: A Randomized Controlled Trial. Clin. Rehabil. 2017, 31, 1616–1624. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, S.; Tanaka, S.; Motojima, N. Comparison of Ankle–Foot Orthoses with Plantar Flexion Stop and Plantar Flexion Resistance in the Gait of Stroke Patients: A Randomized Controlled Trial. Prosthet. Orthot. Int. 2018, 42, 544–553. [Google Scholar] [CrossRef]
- Bang, D.H.; Shin, W.S. Effects of Robot-Assisted Gait Training on Spatiotemporal Gait Parameters and Balance in Patients with Chronic Stroke: A Randomized Controlled Pilot Trial. Neurorehabilitation 2016, 38, 343–349. [Google Scholar] [CrossRef]
- Calabrò, R.S.; Naro, A.; Russo, M.; Bramanti, P.; Carioti, L.; Balletta, T.; Buda, A.; Manuli, A.; Filoni, S.; Bramanti, A. Shaping Neuroplasticity by Using Powered Exoskeletons in Patients with Stroke: A Randomized Clinical Trial. J. Neuroeng. Rehabil. 2018, 15, 35. [Google Scholar] [CrossRef] [Green Version]
- Chiong, Y.; Tay, S.S.; Lim, P.A.C.; Tan, D.M.L. The Effects of Toe Spreader in People with Overactive Toe Flexors Post Stroke: A Randomized Controlled Pilot Study. Clin. Rehabil. 2013, 27, 90–95. [Google Scholar] [CrossRef]
- Cho, J.E.; Shin, J.H.; Kim, H. Does Electrical Stimulation Synchronized with Ankle Movements Better Improve Ankle Proprioception and Gait Kinematics in Chronic Stroke? A Randomized Controlled Study. Neurorehabilitation 2022, 51, 259–269. [Google Scholar] [CrossRef]
- Erbil, D.; Tugba, G.; Murat, T.H.; Melike, A.; Merve, A.; Cagla, K.; Mehmetali, Ç.C.; Akay, Ö.; Nigar, D. Effects of Robot-Assisted Gait Training in Chronic Stroke Patients Treated by Botulinum Toxin-a: A Pivotal Study. Physiother. Res. Int. 2018, 23, e1718. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, L.A.B.; Cimolin, V.; Neto, H.P.; Grecco, L.A.C.; Lazzari, R.D.; Dumont, A.J.L.; Galli, M.; Oliveira, C.S. Effect of Postural Insoles on Gait Pattern in Individuals with Hemiparesis: A Randomized Controlled Clinical Trial. J. Bodyw. Mov. Ther. 2018, 22, 792–797. [Google Scholar] [CrossRef]
- Kelley, C.P.; Childress, J.; Boake, C.; Noser, E.A. Over-Ground and Robotic-Assisted Locomotor Training in Adults with Chronic Stroke: A Blinded Randomized Clinical Trial. Disabil. Rehabil. Assist. Technol. 2013, 8, 161–168. [Google Scholar] [CrossRef]
- Kluding, P.M.; Dunning, K.; O’Dell, M.W.; Wu, S.S.; Ginosian, J.; Feld, J.; McBride, K. Foot Drop Stimulation versus Ankle Foot Orthosis after Stroke: 30-Week Outcomes. Stroke 2013, 44, 1660–1669. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, H.J.; Lee, S.H.; Seo, K.; Lee, M.; Chang, W.H.; Choi, B.O.; Ryu, G.H.; Kim, Y.H. Training for Walking Efficiency with a Wearable Hip-Assist Robot in Patients with Stroke a Pilot Randomized Controlled Trial. Stroke 2019, 50, 3545–3552. [Google Scholar] [CrossRef] [PubMed]
- Min, J.H.; Seong, H.Y.; Ko, S.H.; Jo, W.R.; Sohn, H.J.; Ahn, Y.H.; Son, J.H.; Seo, H.Y.; Son, Y.R.; Mun, S.J.; et al. Effects of Trunk Stabilization Training Robot on Postural Control and Gait in Patients with Chronic Stroke: A Randomized Controlled Trial. Int. J. Rehabil. Res. 2020, 43, 159–166. [Google Scholar] [CrossRef]
- Nam, Y.G.; Lee, J.W.; Park, J.W.; Lee, H.J.; Nam, K.Y.; Park, J.H.; Yu, C.S.; Choi, M.R.; Kwon, B.S. Effects of Electromechanical Exoskeleton-Assisted Gait Training on Walking Ability of Stroke Patients: A Randomized Controlled Trial. Arch. Phys. Med. Rehabil. 2019, 100, 26–31. [Google Scholar] [CrossRef]
- Nam, Y.G.; Park, J.W.; Lee, H.J.; Nam, K.Y.; Choi, M.R.; Yu, C.S.; Zhu, L.; Zhang, X.; Lee, J.W.; Kwon, B.S. Further Effects of Electromechanically Assisted Gait Trainer (Exowalk®) in Patients with Chronic Stroke: A Randomized Controlled Trial. J. Rehabil. Med. 2020, 52, jrm00097. [Google Scholar] [CrossRef] [PubMed]
- Ogino, T.; Kanata, Y.; Uegaki, R.; Yamaguchi, T.; Morisaki, K.; Nakano, S.; Domen, K. Effects of Gait Exercise Assist Robot (GEAR) on Subjects with Chronic Stroke: A Randomized Controlled Pilot Trial. J. Stroke Cerebrovasc. Dis. 2020, 29, 104886. [Google Scholar] [CrossRef]
- Rodrigues, T.A.; Goroso, D.G.; Westgate, P.M.; Carrico, C.; Batistella, L.R.; Sawaki, L. Slow Versus Fast Robot-Assisted Locomotor Training after Severe Stroke: A Randomized Controlled Trial. Am. J. Phys. Med. Rehabil. 2017, 96, S165–S170. [Google Scholar] [CrossRef]
- Stein, J.; Bishop, L.; Stein, D.J.; Wong, C.K. Gait Training with a Robotic Leg Brace after Stroke: A Randomized Controlled Pilot Study. Am. J. Phys. Med. Rehabil. 2014, 93, 987–994. [Google Scholar] [CrossRef]
- Wang, R.Y.; Lin, C.Y.; Chen, J.L.; Lee, C.S.; Chen, Y.J.; Yang, Y.R. Adjunct Non-Elastic Hip Taping Improves Gait Stability in Cane-Assisted Individuals with Chronic Stroke: A Randomized Controlled Trial. J. Clin. Med. 2022, 11, 1553. [Google Scholar] [CrossRef] [PubMed]
- Wu, M.; Landry, J.M.; Kim, J.; Schmit, B.D.; Yen, S.C.; Macdonald, J. Robotic Resistance/Assistance Training Improves Locomotor Function in Individuals Poststroke: A Randomized Controlled Study. Arch. Phys. Med. Rehabil. 2014, 95, 799–806. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yoo, D.; Son, Y.; Kim, D.H.; Seo, K.H.; Lee, B.C. Technology-Assisted Ankle Rehabilitation Improves Balance and Gait Performance in Stroke Survivors: A Randomized Controlled Study with 1-Month Follow-Up. IEEE Trans. Neural Syst. Rehabil. Eng. 2018, 26, 2315–2323. [Google Scholar] [CrossRef]
- Kim, H.Y.; Shin, J.H.; Yang, S.P.; Shin, M.A.; Lee, S.H. Robot-Assisted Gait Training for Balance and Lower Extremity Function in Patients with Infratentorial Stroke: A Single-Blinded Randomized Controlled Trial. J. Neuroeng. Rehabil. 2019, 16, 99. [Google Scholar] [CrossRef]
- Mehrholz, J.; Thomas, S.; Werner, C.; Kugler, J.; Pohl, M.; Elsner, B. Electromechanical-Assisted Training for Walking after Stroke. Cochrane Database Syst. Rev. 2017, 5, CD006185. [Google Scholar] [CrossRef] [PubMed]
- Bruni, M.F.; Melegari, C.; De Cola, M.C.; Bramanti, A.; Bramanti, P.; Calabrò, R.S. What Does Best Evidence Tell Us about Robotic Gait Rehabilitation in Stroke Patients: A Systematic Review and Meta-Analysis. J. Clin. Neurosci. 2018, 48, 11–17. [Google Scholar] [CrossRef]
- Hesse, S.; Waldner, A.; Tomelleri, C. Innovative Gait Robot for the Repetitive Practice of Floor Walking and Stair Climbing up and down in Stroke Patients. J. Neuroeng. Rehabil. 2010, 7, 30. [Google Scholar] [CrossRef] [Green Version]
- Schmidt, H.; Hesse, S.; Bernhardt, R.; Krüger, J. HapticWalker---A Novel Haptic Foot Device. ACM Trans. Appl. Percept. 2005, 2, 166–180. [Google Scholar] [CrossRef]
- Halmi, Z.; Stone, T.W.; Dinya, E.; Málly, J. Postural Instability Years after Stroke. J. Stroke Cerebrovasc. Dis. 2020, 29, 105038. [Google Scholar] [CrossRef]
- Krebs, H.I.; Ferraro, M.; Buerger, S.P.; Newbery, M.J.; Makiyama, A.; Sandmann, M.; Lynch, D.; Volpe, B.T.; Hogan, N. Rehabilitation Robotics: Pilot Trial of a Spatial Extension for MIT-Manus. J. Neuroeng. Rehabil. 2004, 1, 5. [Google Scholar] [CrossRef] [Green Version]

| Author; Year; Nation | Participants; Age | Intervention | Device Type | Intensity | Comparison | Outcome | Additional Therapy | Summary of Findings |
|---|---|---|---|---|---|---|---|---|
| Alingh; 2021; the Netherlands [28] | 32 (female, 12) EG: 60.6 ± 9.3 CG: 56.8 ± 9.8 | Robot-assisted gait training with BWSS | MOOG BV | 30 min/session 18 sessions | Conventional gait training | Gait speed, step width, step length, single-support time, 10MWT, 6mWT, FGA, TUG, FMA-LE, MI | Conventional gait training 30 min 12 sessions | EG = CG |
| Bizovičar; 2017; Slovenia [3] | 19 (female, 11) EG: 52 ± 8 CG: 60 ± 10 | Walking training with an E-go device | E-go device (motorized wheels) | 45 min/session 15 sessions | Conventional physiotherapy | Walking speed, walking distance BBS, FMA-LE, FAC | Standard physiotherapy training | EG = CG |
| Forrester; 2014; USA [31] | 34 (female, NR) EG: 63.3 ± 2.3 CG: 60.0 ± 3.1 | Robot training | Anklebot | 60 min | Manual stretching | FIM, gait velocity, BBS, AROM, MMT, STG parameters, PAV, MAV, normalized jerk, target success | Usual physical therapy | EG > CG |
| Han; 2016; South Korea [32] | 56 (female, 24) EG: 67.89 ± 14.96 CG: 63.20 ± 10.62 | Robot-assistive gait training | Lokomat | 30 min/session 20 sessions | Conventional therapy | K-MBI, BBS, FAC, FMA-LE, baPWV | Rehabilitation therapy 30 min | EG = CG, except for baPWV (EG > CG) |
| Kim; 2019; South Korea [33] | 48 (female, 15) EG: 57.7 ± 12.9 CG: 60.4 ± 13.2 | Robot-assisted gait training | Morning Walk® | 30 min 15 sessions | Conventional therapy | FAC, MI, 10MWT, MBI, RMI, BBS | Conventional therapy 60 min | EG > CG on affected lower limb’s strength and postural balance |
| Monticone; 2013; Italy [34] | 60 (female, 26) EG: 62.1 ± 9.7 CG: 60.2 ± 6.1 | Robot training | Regent Suit | 30 min 20 sessions | Usual care | Gait speed, cadence, step length, symmetry index FIM, BI | Neuromotor rehabilitation 60 min/session 20 sessions | EG > CG |
| Morone; 2016; Italy [35] | 44 (female, 14) EG: 61.50 ± 10.97 CG: 64.09 ± 16.27 | Conventional walking training using a servo-assistive robotic walker | i-Walker | 40 min 20 sessions | Conventional walking-oriented therapy | 6mWT, 10MWT, Tinetti’s scale, MAS, BI, CNS | Hand therapy | EG > CG |
| van Nunen; 2015; the Netherlands [16] | 30 (female, 14) EG: 50.0 ± 9.6 CG: 56.0 ± 8.7 | Robot-assisted treadmill training | Lokomat | 2 h per week/8 weeks | Conventional therapy | Walking speed, FAC, BBS, RMI, FMA-LE, TUG | Conventional therapy 1.5 h per week/8 weeks | EG = CG |
| Author; Year; Nation | Participants; Age | Intervention | Device Type | Intensity | Comparison | Outcome | Additional Therapy | Summary of Findings |
|---|---|---|---|---|---|---|---|---|
| Choi; 2020; South Korea [29] | 36 (female, 16) EG1: 64.1 ± 10.5 EG2: 62.4 ± 12.1 CG: 67.4 ± 12.9 | Trunk stabilization exercise with pelvic compressor belt | Compressor belt | 30 min/session 30 sessions | Comprehensive rehabilitation therapy | PASS, TUG, COL, LOS | Neurodevelopmental therapy 60 min/session 30 sessions | EG1 > EG2 = CG |
| de Seze; 2011; France [30] | 28 (female, 10) EG: 56.4 ± 8 CG: 53 ± 13 | Ankle–foot orthosis | Chignon ankle–foot orthosis | 30 days | Standard ankle–foot orthosis | 10MWT, FAC, PASS, FIM | Not available | EG > CG |
| Nikamp; 2017; the Netherlands [36] | 33 (female, 13) EG: 56.9 ± 9.6 CG: 57.5 ± 9.1 | Early provision | Ankle–foot orthosis: polyethylene, semi-rigid, and rigid | 26 weeks | Delayed provision | 10MWT, BBS, FAC, 6mWT, TUG, RMI, BI, MI, stairs test | Not available | EG = CG |
| Yamamoto; 2018; Japan [37] | 40 (female, 4) EG: 59.2 ± 9.8 CG: 60.2 ± 12.3 | Gait training with ankle–foot orthosis | Ankle–foot orthosis with plantar flexion stop | 1 h/session 14 sessions | Ankle–foot orthosis with plantar flexion resistance | Gait velocity, loading response times, single-stance times, pre-swing time, swing time, ground reaction forces, COP progression, joint angle, moment, and power at ankle, knee, and hip Pelvic tilt, thoracic tilt | Not available | EG = CG |
| Author; Year; Nation | Participants; Age | Intervention | Device Type | Intensity | Comparison | Outcome | Additional Therapy | Summary of Findings |
|---|---|---|---|---|---|---|---|---|
| Bang; 2016; South Korea [38] | 18 (female, 9) EG: 53.56 ± 3.94 CG: 53.67 ± 2.83 | Robot-assisted gait training | Lokomat | 60 min/session 20 sessions | Treadmill training | ABC, BBS, gait velocity, cadence step length, double-support period | Not available | EG > CG |
| Calabro; 2018; Italy [39] | 40 (female, 17) EG: 69 ± 4 CG: 67 ± 6 | Robot-assisted gait training | EksoTM | 45 min/session 40 sessions | Overground gait training | 10MWT, RMI, TUG, GQI, GCD, cadence, stance/swing ratio, sEMG (RF, BF, S, TA), EEG | Conventional physiotherapy training 60min/day | EG > CG |
| Erbil; 2018; Turkey [42] | 43 (female, 27) EG: 50.1 ± 11.8 CG: 48.7 ± 10.4 | Robot-assisted gait training | RoboGait® | 30 min/session | Physical therapy | BBS, TUG, RVGA, MAS, Tardieu scale | Physical therapy 60 min/day | EG > CG |
| Kelley; 2013; USA [44] | 20 (female, 7) EG: 66.91 ± 8.50 CG: 64.33 ± 10.91 | Robotic-assisted locomotor training | Locomat® | 60 min/session 40 sessions | Overground training | 10MWT, 6MWT, FIM-LE, Barthel index, SIS | Not available | EG = CG |
| Lee; 2019; South Korea [46] | 26 (female, 12) EG: 61.85 ± 7.87 CG: 62.25 ± 6.36 | Gait enhancing and motivating system on five treadmill sessions and five overground sessions | Wearable hip-assistance robot | 45 min/session 10 sessions | Non-robot on five treadmill sessions and five overground sessions | MAS, K-MoCA, FAC, gait velocity, cadence, stride length, temporal symmetry ratio, spatial step symmetry ratio, muscle effort symmetry ratio | Not available | EG > CG |
| Min; 2020; South Korea [47] | 38 (female, 14) EG: 61.47 ± 11.15 CG: 56.36 ± 9.16 | Robot training | Trunk stability rehabilitation robot trainer (3DBT-33) | 30 min/session 20 sessions | Conventional physical therapy | BBS, TUG, FMA-LE, FAC, K-MBI | Conventional physical therapy 30 min/day | EG > CG |
| Ogino; 2020; Japan [50] | 19 (female, 4) EG: 66.1 ± 9.6 CG: 65.0 ± 7.7 | Robot-assisted gait training | GEAR system (gait exercise assistive robot) | 40 min/session 20 sessions | Treadmill training | 10MWT, TUG, SF-8, 6mWT, GRC | Conventional therapy 20 min/day | EG > CG |
| Rodrigues; 2017; USA [51] | 18 (female, 8) EG: 50.6 ± 14.4 CG: 59.3 ± 13.8 | Robot-assisted BWSTT | Robot-assisted (slow) | 30 min/session | Robot-assisted (fast) | FAC, TUG, 6mWT, 10MWT, BBS, FMA-LE | Not available | EG > CG |
| Stein; 2014; USA [52] | 24 (female) EG: 57.6 ± 10.7 CG: 56.6 ± 15.1 | Robot training | Bionic leg device | 60 min/session 18 sessions | Group exercise | 10MWT, 6mWT, 5XSST, TUG, BBS, CAFÉ 40, EFAP, Romberg | Not available | EG = CG |
| Wu; 2014; USA [54] | 28 (female, 10) EG: 53.6 ± 8.9 CG: 57.4 ± 9.8 | Robotic gait training applied to the paretic leg to assist with leg swing | Custom-designed, cable-driven robotic gait training system | 45 min/session 18 sessions | Robotic gait training applied to the paretic leg to assist with leg swing | SLS, step length, step asymmetry, cadence ABC, SF-36, MAS | Not available | EG = CG |
| Author; Year; Nation | Participants; Age | Intervention | Device Type | Intensity | Comparison | Outcome | Additional Therapy | Summary of Findings |
|---|---|---|---|---|---|---|---|---|
| Chiong; 2013; Singapore [40] | 9 (female, 4) 48 (34–61) | Toe flexor stretches with toe spreader | Rolyan Ezemix elastomer putty with sports sandals | Ambulated during the 6-month study period | Toe flexor stretches | Gait velocity, stride length, step length, plantar surface contact area, MAS, BBS, VAS | Not available | EG = CG |
| Cho; 2022; South Korea [41] | 30 (female, 7) EG: 51.8 ± 12.0 CG: 55.0 ± 10.9 | Passive biaxial ankle movement training with electrical stimulation therapy | Ankle movement system | 40 min/session 20 sessions | Electrical stimulation therapy | Proprioception, pROM, strength, FMA-LE, BBS, TUG, FES, walking speed, step length, step time, step width, ROM | Inpatient rehabilitation program | EG > CG on pROM and strength |
| Ferreira; 2017; Brazil [43] | 20 (female, 4) EG: 59.2 ± 10.4 CG: 60.3 ± 13.3 | Postural insoles for equinovarus foot | Postural insoles | 3 months | Placebo insoles without corrective elements | Stance phase, swing phase, double support, step length, stride length, mean velocity, cadence, sagittal kinematic plots | Conventional physical therapy | EG > CG on dorsiflexion and knee flexion at post-training |
| Kluding; 2012; USA [45] | 197 (female, 79) EG: 60.71 ± 12.24 CG: 61.58 ± 10.98 | Gait training with foot drop stimulator | NESS L300 Foot Drop System | 30 weeks | Gait training with ankle–foot orthosis | Walking speed, FMA, 6mWT, FRT, SIS, BBS, FAC | Gait training and home exercise program Eight sessions | EG > CG on user satisfaction |
| Nam; 2019; South Korea [48] | 34 (female, 17) EG: 48.33 ± 15.56 CG: 68.56 ± 17.35 | Electromechanical-assisted gait training | Exowalk, an electromechanical exoskeleton | 30 min/session 20 sessions | Physical therapy-assisted gait training | FAC, RMI, 10MWT, 6mWT, MI, BBS, MBI | Physical therapy | EG = CG |
| Nam; 2020; South Korea [49] | 38 (female, 16) EG: 60.00 ± 11.48 CG: 57.30 ± 8.71 | Electromechanical-assisted gait training | Exowalk, an electromechanical exoskeleton | 60 min/session 20 sessions | Physical therapy-assisted gait training | FAC, RMI, 10MWT, 6mWT, MI, BBS, MBI | Physical therapy | EG = CG |
| Wang; 2022; Taiwan [53] | 21 (female, 6) EG: 62.27 ± 10.10 CG: 63.30 ± 7.05 | Non-elastic hip taping combined with gait training | Non-elastic taping | 50 min/session 12 sessions | Sham | Gait velocity, double-support time, spatial symmetry index, temporal symmetry index, BBS, 6mWT, FES | Not available | EG = CG |
| Yoo; 2018; South Korea [55] | 16 (female, 5) EG: 58.5 ± 9.4 CG: 53.9 ± 6.0 | Ankle stretching exercise | Motorized ankle stretcher | Seven sessions | Stretching board exercise | Ankle ROM, SOT, walking speed, cadence, step length | Not available | EG > CG |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hwang, S.; Song, C.-S. Assistive Technology Involving Postural Control and Gait Performance for Adults with Stroke: A Systematic Review and Meta-Analysis. Healthcare 2023, 11, 2225. https://doi.org/10.3390/healthcare11152225
Hwang S, Song C-S. Assistive Technology Involving Postural Control and Gait Performance for Adults with Stroke: A Systematic Review and Meta-Analysis. Healthcare. 2023; 11(15):2225. https://doi.org/10.3390/healthcare11152225
Chicago/Turabian StyleHwang, Sujin, and Chiang-Soon Song. 2023. "Assistive Technology Involving Postural Control and Gait Performance for Adults with Stroke: A Systematic Review and Meta-Analysis" Healthcare 11, no. 15: 2225. https://doi.org/10.3390/healthcare11152225
APA StyleHwang, S., & Song, C.-S. (2023). Assistive Technology Involving Postural Control and Gait Performance for Adults with Stroke: A Systematic Review and Meta-Analysis. Healthcare, 11(15), 2225. https://doi.org/10.3390/healthcare11152225







