Sleep Profiles in Eating Disorders: A Scientometric Study on 50 Years of Clinical Research
Abstract
1. Introduction
The Current Study
2. Materials and Methods
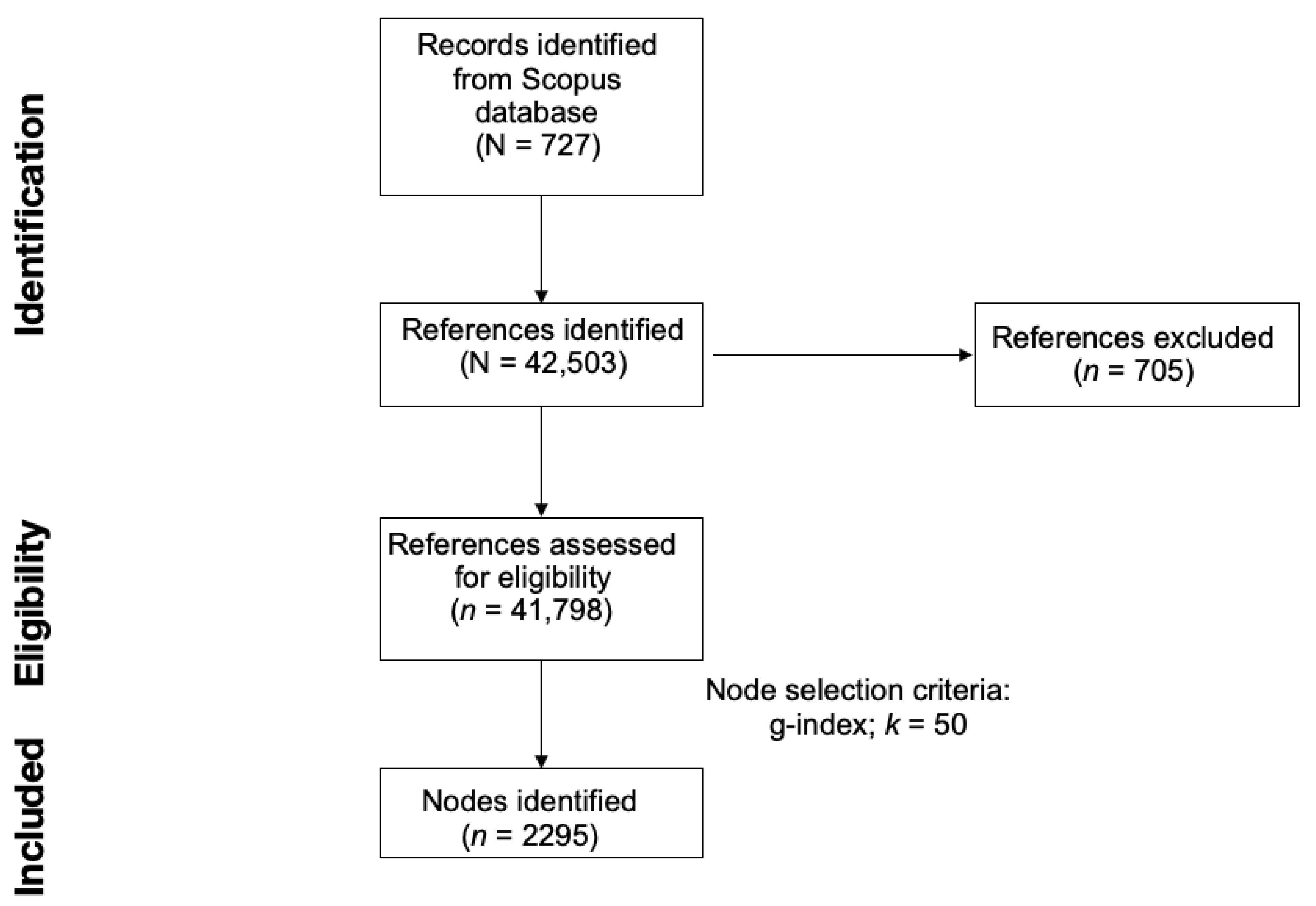
2.1. Data Collection from Scopus
2.2. Data Import on CiteSpace
2.3. Document Co-Citation Analysis (DCA)
2.4. DCA Network Evaluation Metrics
3. Results
3.1. Bibliometric Analysis on the Citing Documents
3.2. Document Co-Citation Analysis
3.3. Impactful Documents
4. Discussion
4.1. Cluster #9: Sleep-Related Eating Disorder
4.2. Cluster #3: Nocturnal Eating
4.3. Cluster #46: Ghrelin
4.4. Cluster #4: Comorbidities
4.5. Cluster #22: Mental Disorders in Sport
4.6. Cluster #1: Sleep Quality in Anorexia Nervosa
4.7. Cluster #17: Bidirectional Relationship
4.8. Limitations of the Study
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| DCA | Document Co-Citation Analysis |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| LLR | Log-Likelihood Ratio |
| GCS | Global Citing Score |
References
- Lauer, C.J.; Krieg, J.C. Sleep in eating disorders. Sleep Med. Rev. 2004, 8, 109–118. [Google Scholar] [CrossRef] [PubMed]
- Allison, K.C.; Spaeth, A.; Hopkins, C.M. Sleep and eating disorders. Curr. Psychiatry Rep. 2016, 18, 1–8. [Google Scholar] [CrossRef]
- Galmiche, M.; Déchelotte, P.; Lambert, G.; Tavolacci, M.P. Prevalence of eating disorders over the 2000–2018 period: A systematic literature review. Am. J. Clin. Nutr. 2019, 109, 1402–1413. [Google Scholar] [CrossRef]
- Van Eeden, A.E.; van Hoeken, D.; Hoek, H.W. Incidence, prevalence and mortality of anorexia nervosa and bulimia nervosa. Curr. Opin. Psychiatry 2021, 34, 515. [Google Scholar] [CrossRef] [PubMed]
- Strother, E.; Lemberg, R.; Stanford, S.C.; Turberville, D. Eating disorders in men: Underdiagnosed, undertreated, and misunderstood. Eat. Disord. 2012, 20, 346–355. [Google Scholar] [CrossRef] [PubMed]
- Cho, J.; Lee, J.H.; Hong, S.C. Sleep-Related Eating Disorder and Nocturnal Eating Syndrome. Sleep Med. Res. 2020, 11, 65–69. [Google Scholar] [CrossRef]
- Knudsen, H.K.; Ducharme, L.J.; Roman, P.M. Job stress and poor sleep quality: Data from an American sample of full-time workers. Soc. Sci. Med. 2007, 64, 1997–2007. [Google Scholar] [CrossRef]
- Karna, B.; Sankari, A.; Tatikonda, G. Sleep Disorder; StatPearls: Tampa, FL, USA, 2023. [Google Scholar]
- Cooper, A.R.; Loeb, K.L.; McGlinchey, E.L. Sleep and eating disorders: Current research and future directions. Curr. Opin. Psychol. 2020, 34, 89–94. [Google Scholar] [CrossRef]
- Lundgren, J.D.; O’Reardon, J.P.; Allison, K.C.; Spresser, C.D. Sleep and quality of life in eating disorders. In Sleep and Quality of Life in Clinical Medicine; Humana Press: Totowa, NJ, USA, 2008; pp. 281–289. [Google Scholar]
- Nakagawa, S.; Samarasinghe, G.; Haddaway, N.R.; Westgate, M.J.; O’Dea, R.E.; Noble, D.W.; Lagisz, M. Research weaving: Visualizing the future of research synthesis. Trends Ecol. Evol. 2019, 34, 224–238. [Google Scholar] [CrossRef]
- Sabe, M.; Pillinger, T.; Kaiser, S.; Chen, C.; Taipale, H.; Tanskanen, A.; Tiihonen, J.; Leucht, S.; Correll, C.U.; Solmi, M. Half a century of research on antipsychotics and schizophrenia: A scientometric study of hotspots, nodes, bursts, and trends. Neurosci. Biobehav. Rev. 2022, 136, 104608. [Google Scholar] [CrossRef]
- Börner, K.; Chen, C.; Boyack, K.W. Visualizing knowledge domains. Annu. Rev. Inf. Sci. Technol. 2003, 37, 179–255. [Google Scholar] [CrossRef]
- Goldenberg, D. Scientometrics and its positive consequences. Rev. Bras. Cir. Plástica (RBCP)—Braz. J. Plast. Sugery 2017, 32, 471. [Google Scholar] [CrossRef]
- Bonacina, G.; Carollo, A.; Esposito, G. The Genetic Side of the Mood: A Scientometric Review of the Genetic Basis of Mood Disorders. Genes 2023, 14, 352. [Google Scholar] [CrossRef]
- Lim, M.; Carollo, A.; Neoh, M.J.Y.; Sacchiero, M.; Azhari, A.; Balboni, G.; Marschik, P.; Nordahl-Hansen, A.; Dimitriou, D.; Esposito, G. Developmental disabilities in Africa: A scientometric review. Res. Dev. Disabil. 2023, 133, 104395. [Google Scholar] [CrossRef] [PubMed]
- Carollo, A.; Balagtas, J.P.M.; Neoh, M.J.Y.; Esposito, G. A scientometric approach to review the role of the medial preoptic area (MPOA) in parental behavior. Brain Sci. 2021, 11, 393. [Google Scholar] [CrossRef]
- Carollo, A.; Lim, M.; Aryadoust, V.; Esposito, G. Interpersonal synchrony in the context of caregiver-child interactions: A document co-citation analysis. Front. Psychol. 2021, 12, 701824. [Google Scholar] [CrossRef]
- Neoh, M.J.Y.; Carollo, A.; Lim, M.; Dimitriou, D.; Esposito, G. A Scientometric Review of Obstructive Sleep Apnea and Obesity. Appl. Sci. 2023, 13, 753. [Google Scholar] [CrossRef]
- Chen, C. The citespace manual. Coll. Comput. Inform. 2014, 1, 1–84. [Google Scholar]
- Falagas, M.E.; Pitsouni, E.I.; Malietzis, G.A.; Pappas, G. Comparison of PubMed, Scopus, web of science, and Google scholar: Strengths and weaknesses. FASEB J. 2008, 22, 338–342. [Google Scholar] [CrossRef]
- Carollo, A.; Bonassi, A.; Lim, M.; Gabrieli, G.; Setoh, P.; Dimitriou, D.; Aryadoust, V.; Esposito, G. Developmental disabilities across the world: A scientometric review from 1936 to 2020. Res. Dev. Disabil. 2021, 117, 104031. [Google Scholar] [CrossRef]
- Aria, M.; Cuccurullo, C. bibliometrix: An R-tool for comprehensive science mapping analysis. J. Inf. 2017, 11, 959–975. [Google Scholar] [CrossRef]
- Chen, C. CiteSpace II: Detecting and visualizing emerging trends and transient patterns in scientific literature. J. Am. Soc. Inf. Sci. Technol. 2006, 57, 359–377. [Google Scholar] [CrossRef]
- Chen, C. CiteSpace: A Practical Guide for Mapping Scientific Literature; Nova Science Publishers: Hauppauge, NY, USA, 2016. [Google Scholar]
- Trujillo, C.M.; Long, T.M. Document co-citation analysis to enhance transdisciplinary research. Sci. Adv. 2018, 4, e1701130. [Google Scholar] [CrossRef] [PubMed]
- Small, H. Co-citation in the scientific literature: A new measure of the relationship between two documents. J. Am. Soc. Inf. Sci. 1973, 24, 265–269. [Google Scholar] [CrossRef]
- Egghe, L. Theory and practise of the g-index. Scientometrics 2006, 69, 131–152. [Google Scholar] [CrossRef]
- Carollo, A.; Fong, S.; Gabrieli, G.; Mulatti, C.; Esposito, G. To wine or not to wine? A scientometric approach to 65+ years of wine preference and selection studies. Br. Food J. 2022, 124, 409–431. [Google Scholar] [CrossRef]
- Chen, C.; Hu, Z.; Liu, S.; Tseng, H. Emerging trends in regenerative medicine: A scientometric analysis in CiteSpace. Expert Opin. Biol. Ther. 2012, 12, 593–608. [Google Scholar] [CrossRef]
- Aryadoust, V.; Tan, H.A.H.; Ng, L.Y. A Scientometric review of Rasch measurement: The rise and progress of a specialty. Front. Psychol. 2019, 10, 2197. [Google Scholar] [CrossRef]
- Muff, S.; Rao, F.; Caflisch, A. Local modularity measure for network clusterizations. Phys. Rev. E 2005, 72, 056107. [Google Scholar] [CrossRef]
- Chen, C.; Ibekwe-SanJuan, F.; Hou, J. The structure and dynamics of cocitation clusters: A multiple-perspective cocitation analysis. J. Am. Soc. Inf. Sci. Technol. 2010, 61, 1386–1409. [Google Scholar] [CrossRef]
- Aryadoust, V.; Ang, B.H. Exploring the frontiers of eye tracking research in language studies: A novel co-citation scientometric review. Comput. Assist. Lang. Learn. 2021, 34, 898–933. [Google Scholar] [CrossRef]
- Rousseeuw, P.J. Silhouettes: A graphical aid to the interpretation and validation of cluster analysis. J. Comput. Appl. Math. 1987, 20, 53–65. [Google Scholar] [CrossRef]
- Freeman, L.C. A set of measures of centrality based on betweenness. Sociometry 1977, 40, 35–41. [Google Scholar] [CrossRef]
- Kleinberg, J. Bursty and hierarchical structure in streams. In Proceedings of the Eighth ACM SIGKDD International Conference on Knowledge Discovery and Data Mining, Edmonton, AB, Canada, 23–26 July 2002; pp. 91–101. [Google Scholar]
- Chen, C. Science mapping: A systematic review of the literature. J. Data Inf. Sci. 2017, 2, 1–40. [Google Scholar] [CrossRef]
- Chen, C.; Chen, Y.; Horowitz, M.; Hou, H.; Liu, Z.; Pellegrino, D. Towards an explanatory and computational theory of scientific discovery. J. Inf. 2009, 3, 191–209. [Google Scholar] [CrossRef]
- Hofmann, S.G.; Asnaani, A.; Vonk, I.J.; Sawyer, A.T.; Fang, A. The efficacy of cognitive behavioral therapy: A review of meta-analyses. Cogn. Ther. Res. 2012, 36, 427–440. [Google Scholar] [CrossRef] [PubMed]
- Gustavsson, A.; Svensson, M.; Jacobi, F.; Allgulander, C.; Alonso, J.; Beghi, E.; Dodel, R.; Ekman, M.; Faravelli, C.; Fratiglioni, L.; et al. Cost of disorders of the brain in Europe 2010. Eur. Neuropsychopharmacol. 2011, 21, 718–779. [Google Scholar] [CrossRef]
- Lim, M.; Carollo, A.; Neoh, M.J.Y.; Esposito, G. Mapping miRNA Research in Schizophrenia: A Scientometric Review. Int. J. Mol. Sci. 2023, 24, 436. [Google Scholar] [CrossRef]
- Vetrugno, R.; Manconi, M.; Ferini-Strambi, L.; Provini, F.; Plazzi, G.; Montagna, P. Nocturnal eating: Sleep-related eating disorder or night eating syndrome? A videopolysomnographic study. Sleep 2006, 29, 949–954. [Google Scholar] [CrossRef]
- Morgenthaler, T.I.; Silber, M.H. Amnestic sleep-related eating disorder associated with zolpidem. Sleep Med. 2002, 3, 323–327. [Google Scholar] [CrossRef]
- Howell, M.J.; Schenck, C.H.; Crow, S.J. A review of nighttime eating disorders. Sleep Med. Rev. 2009, 13, 23–34. [Google Scholar] [CrossRef]
- Winkelman, J.; Herzog, D.; Fava, M. The prevalence of sleep-related eating disorder in psychiatric and non-psychiatric populations. Psychol. Med. 1999, 29, 1461–1466. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Winkelman, J.W. Sleep-related eating disorder and night eating syndrome: Sleep disorders, eating disorders, or both? Sleep 2006, 29, 876–877. [Google Scholar] [CrossRef] [PubMed]
- Provini, F.; Albani, F.; Vetrugno, R.; Vignatelli, L.; Lombardi, C.; Plazzi, G.; Montagna, P. A pilot double-blind placebo-controlled trial of low-dose pramipexole in sleep-related eating disorder. Eur. J. Neurol. 2005, 12, 432–436. [Google Scholar] [CrossRef] [PubMed]
- Winkelman, J.W. Treatment of nocturnal eating syndrome and sleep-related eating disorder with topiramate. Sleep Med. 2003, 4, 243–246. [Google Scholar] [CrossRef] [PubMed]
- Tzischinsky, O.; Vinai, P.; Howell, M.J.; Latzer, Y. Sleep-Related Eating Disorders: A Separate Entity or Part of the NES Clinical Spectrum? In Parasomnias: Clinical Characteristics and Treatment; Springer: New York, NY, USA, 2013; pp. 303–325. [Google Scholar]
- Howell, M.J. Sleep-Related Eating Disorder. In Encyclopedia of Sleep; Elsevier Inc.: Amsterdam, The Netherlands, 2013; pp. 243–247. [Google Scholar]
- Benca, R.M.; Schenck, C.H. Sleep and eating disorders. In Principles and Practice of Sleep Medicine; ScienceDirect: Amsterdam, The Netherlands, 2005; pp. 1337–1344. [Google Scholar]
- Inoue, Y. Sleep-related eating disorder and its associated conditions. Psychiatry Clin. Neurosci. 2015, 69, 309–320. [Google Scholar] [CrossRef]
- Winkelman, J.W. Efficacy and tolerability of open-label topiramate in the treatment of sleep-related eating disorder: A retrospective case series. J. Clin. Psychiatry 2006, 67, 1729–1734. [Google Scholar] [CrossRef]
- Allison, K.C.; Wadden, T.A.; Sarwer, D.B.; Fabricatore, A.N.; Crerand, C.E.; Gibbons, L.M.; Stack, R.M.; Stunkard, A.J.; Williams, N.N. Night eating syndrome and binge eating disorder among persons seeking bariatric surgery: Prevalence and related features. Surg. Obes. Relat. Dis. 2006, 2, 153–158. [Google Scholar] [CrossRef]
- Allison, K.C.; Grilo, C.M.; Masheb, R.M.; Stunkard, A.J. High self-reported rates of neglect and emotional abuse, by persons with binge eating disorder and night eating syndrome. Behav. Res. Ther. 2007, 45, 2874–2883. [Google Scholar] [CrossRef]
- Allison, K.C.; Lundgren, J.D.; O’Reardon, J.P.; Geliebter, A.; Gluck, M.E.; Vinai, P.; Mitchell, J.E.; Schenck, C.H.; Howell, M.J.; Crow, S.J.; et al. Proposed diagnostic criteria for night eating syndrome. Int. J. Eat. Disord. 2010, 43, 241–247. [Google Scholar] [CrossRef]
- Allison, K.C.; Tarves, E.P. Treatment of night eating syndrome. Psychiatr. Clin. 2011, 34, 785–796. [Google Scholar] [CrossRef]
- Howell, M.J. Parasomnias: An updated review. Neurotherapeutics 2012, 9, 753–775. [Google Scholar] [CrossRef]
- Howell, M.J.; Schenck, C.H. Restless nocturnal eating: A common feature of Willis-Ekbom Syndrome (RLS). J. Clin. Sleep Med. 2012, 8, 413–419. [Google Scholar] [CrossRef]
- Schenck, C.H.; Mahowald, M.W. Therapeutics for parasomnias in adults. Sleep Med. Clin. 2010, 5, 689–700. [Google Scholar] [CrossRef]
- Boeve, B.F.; Silber, M.H.; Ferman, T.J. Melatonin for treatment of REM sleep behavior disorder in neurologic disorders: Results in 14 patients. Sleep Med. 2003, 4, 281–284. [Google Scholar] [CrossRef] [PubMed]
- Boeve, B.F.; Silber, M.; Saper, C.; Ferman, T.; Dickson, D.; Parisi, J.; Benarroch, E.; Ahlskog, J.; Smith, G.; Caselli, R.; et al. Pathophysiology of REM sleep behaviour disorder and relevance to neurodegenerative disease. Brain 2007, 130, 2770–2788. [Google Scholar] [CrossRef] [PubMed]
- Hobson, J.A. REM sleep and dreaming: Towards a theory of protoconsciousness. Nat. Rev. Neurosci. 2009, 10, 803–813. [Google Scholar] [CrossRef] [PubMed]
- Spaggiari, M.C.; Granella, F.; Parrino, L.; Marchesi, C.; Melli, I.; Terzano, M.G. Nocturnal eating syndrome in adults. Sleep 1994, 17, 339–344. [Google Scholar] [CrossRef]
- Chiang, A.; Krystal, A. Report of two cases where sleep related eating behavior occurred with the extended-release formulation but not the immediate-release formulation of a sedative-hypnotic agent. J. Clin. Sleep Med. 2008, 4, 155–156. [Google Scholar] [CrossRef]
- Dang, A.; Garg, G.; Rataboli, P.V. Zolpidem induced nocturnal sleep-related eating disorder (NSRED) in a male patient. Int. J. Eat. Disord. 2009, 42, 385–386. [Google Scholar] [CrossRef]
- Yun, C.H.; Ji, K.H. Zolpidem-induced sleep-related eating disorder. J. Neurol. Sci. 2010, 288, 200–201. [Google Scholar] [CrossRef]
- Allen, R.P.; Walters, A.S.; Montplaisir, J.; Hening, W.; Myers, A.; Bell, T.J.; Ferini-Strambi, L. Restless legs syndrome prevalence and impact: REST general population study. Arch. Intern. Med. 2005, 165, 1286–1292. [Google Scholar] [CrossRef] [PubMed]
- Mahowald, M.W.; Bornemann, M.A.C.; Schenck, C.H. A case of reversible restless legs syndrome (RLS) and sleep-related eating disorder relapse triggered by acute right leg herpes zoster infection: Literature review of spinal cord and peripheral nervous system contributions to RLS. Sleep Med. 2010, 11, 583–585. [Google Scholar] [CrossRef]
- Nirenberg, M.J.; Waters, C. Nocturnal eating in restless legs syndrome. Mov. Disord. 2010, 25, 126–127. [Google Scholar] [CrossRef]
- Provini, F.; Antelmi, E.; Vignatelli, L.; Zaniboni, A.; Naldi, G.; Calandra-Buonaura, G.; Vetrugno, R.; Plazzi, G.; Montagna, P. Association of restless legs syndrome with nocturnal eating: A case-control study. Mov. Disord. Off. J. Mov. Disord. Soc. 2009, 24, 871–877. [Google Scholar] [CrossRef] [PubMed]
- Provini, F.; Antelmi, E.; Vignatelli, L.; Zaniboni, A.; Naldi, G.; Calandra-Buonaura, G.; Vetrugno, R.; Plazzi, G.; Pizza, F.; Montagna, P. Increased prevalence of nocturnal smoking in restless legs syndrome (RLS). Sleep Med. 2010, 11, 218–220. [Google Scholar] [CrossRef] [PubMed]
- Wittekind, D.A.; Kluge, M. Ghrelin in psychiatric disorders—A review. Psychoneuroendocrinology 2015, 52, 176–194. [Google Scholar] [CrossRef] [PubMed]
- Atalayer, D.; Gibson, C.; Konopacka, A.; Geliebter, A. Ghrelin and eating disorders. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2013, 40, 70–82. [Google Scholar] [CrossRef]
- Otto, B.; Cuntz, U.; Fruehauf, E.a.; Wawarta, R.; Folwaczny, C.; Riepl, R.; Heiman, M.; Lehnert, P.; Fichter, M.; Tschop, M. Weight gain decreases elevated plasma ghrelin concentrations of patients with anorexia nervosa. Eur. J. Endocrinol. 2001, 145, R5–R9. [Google Scholar] [CrossRef]
- Schur, E.A.; Cummings, D.E.; Callahan, H.S.; Foster-Schubert, K.E. Association of cognitive restraint with ghrelin, leptin, and insulin levels in subjects who are not weight-reduced. Physiol. Behav. 2008, 93, 706–712. [Google Scholar] [CrossRef]
- Schüssler, P.; Kluge, M.; Yassouridis, A.; Dresler, M.; Uhr, M.; Steiger, A. Ghrelin levels increase after pictures showing food. Obesity 2012, 20, 1212–1217. [Google Scholar] [CrossRef]
- Kojima, S.; Nakahara, T.; Nagai, N.; Muranaga, T.; Tanaka, M.; Yasuhara, D.; Masuda, A.; Date, Y.; Ueno, H.; Nakazato, M.; et al. Altered ghrelin and peptide YY responses to meals in bulimia nervosa. Clin. Endocrinol. 2005, 62, 74–78. [Google Scholar] [CrossRef]
- Monteleone, P.; Serritella, C.; Martiadis, V.; Scognamiglio, P.; Maj, M. Plasma obestatin, ghrelin, and ghrelin/obestatin ratio are increased in underweight patients with anorexia nervosa but not in symptomatic patients with bulimia nervosa. J. Clin. Endocrinol. Metab. 2008, 93, 4418–4421. [Google Scholar] [CrossRef]
- Monteleone, P.; Serritella, C.; Scognamiglio, P.; Maj, M. Enhanced ghrelin secretion in the cephalic phase of food ingestion in women with bulimia nervosa. Psychoneuroendocrinology 2010, 35, 284–288. [Google Scholar] [CrossRef]
- Geliebter, A.; Gluck, M.E.; Hashim, S.A. Plasma ghrelin concentrations are lower in binge-eating disorder. J. Nutr. 2005, 135, 1326–1330. [Google Scholar] [CrossRef]
- Motivala, S.J.; Tomiyama, A.J.; Ziegler, M.; Khandrika, S.; Irwin, M.R. Nocturnal levels of ghrelin and leptin and sleep in chronic insomnia. Psychoneuroendocrinology 2009, 34, 540–545. [Google Scholar] [CrossRef]
- Kucukgoncu, S.; Tek, C.; Bestepe, E.; Musket, C.; Guloksuz, S. Clinical features of night eating syndrome among depressed patients. Eur. Eat. Disord. Rev. 2014, 22, 102–108. [Google Scholar] [CrossRef]
- Aspen, V.; Weisman, H.; Vannucci, A.; Nafiz, N.; Gredysa, D.; Kass, A.E.; Trockel, M.; Jacobi, C.; Wilfley, D.E.; Taylor, C.B. Psychiatric co-morbidity in women presenting across the continuum of disordered eating. Eat. Behav. 2014, 15, 686–693. [Google Scholar] [CrossRef]
- Bos, S.C.; Soares, M.J.; Marques, M.; Maia, B.; Pereira, A.T.; Nogueira, V.; Valente, J.; Macedo, A. Disordered eating behaviors and sleep disturbances. Eat. Behav. 2013, 14, 192–198. [Google Scholar] [CrossRef]
- Kim, K.R.; Jung, Y.C.; Shin, M.Y.; Namkoong, K.; Kim, J.K.; Lee, J.H. Sleep disturbance in women with eating disorder: Prevalence and clinical characteristics. Psychiatry Res. 2010, 176, 88–90. [Google Scholar] [CrossRef]
- Nolan, L.J.; Geliebter, A. Night eating is associated with emotional and external eating in college students. Eat. Behav. 2012, 13, 202–206. [Google Scholar] [CrossRef]
- Antelmi, E.; Vinai, P.; Pizza, F.; Marcatelli, M.; Speciale, M.; Provini, F. Nocturnal eating is part of the clinical spectrum of restless legs syndrome and an underestimated risk factor for increased body mass index. Sleep Med. 2014, 15, 168–172. [Google Scholar] [CrossRef] [PubMed]
- Gouttebarge, V.; Jonkers, R.; Moen, M.; Verhagen, E.; Wylleman, P.; Kerkhoffs, G. A prospective cohort study on symptoms of common mental disorders among Dutch elite athletes. Physician Sportsmed. 2017, 45, 426–432. [Google Scholar] [CrossRef] [PubMed]
- Gouttebarge, V.; Kerkhoffs, G.M. A prospective cohort study on symptoms of common mental disorders among current and retired professional ice hockey players. Physician Sportsmed. 2017, 45, 252–258. [Google Scholar] [CrossRef] [PubMed]
- Gouttebarge, V.; Johnson, U.; Rochcongar, P.; Rosier, P.; Kerkhoffs, G. Symptoms of common mental disorders among professional football referees: A one-season prospective study across Europe. Physician Sportsmed. 2017, 45, 11–16. [Google Scholar] [CrossRef]
- Gouttebarge, V.; Tol, J.L.; Kerkhoffs, G.M. Epidemiology of symptoms of common mental disorders among elite Gaelic athletes: A prospective cohort study. Physician Sportsmed. 2016, 44, 283–289. [Google Scholar] [CrossRef]
- Gouttebarge, V.; Kerkhoffs, G.; Lambert, M. Prevalence and determinants of symptoms of common mental disorders in retired professional Rugby Union players. Eur. J. Sport Sci. 2016, 16, 595–602. [Google Scholar] [CrossRef]
- Gouttebarge, V.; Aoki, H.; Verhagen, E.A.; Kerkhoffs, G.M. A 12-month prospective cohort study of symptoms of common mental disorders among European professional footballers. Clin. J. Sport Med. 2017, 27, 487–492. [Google Scholar] [CrossRef]
- Arnold, R.D.F. A research synthesis and taxonomic classification of the organizational stressors encountered by sport performers. J. Sport Exerc. Psychol. 2012, 34, 397–429. [Google Scholar] [CrossRef]
- Gulliver, A.; Griffiths, K.M.; Christensen, H. Barriers and facilitators to mental health help-seeking for young elite athletes: A qualitative study. BMC Psychiatry 2012, 12, 157. [Google Scholar] [CrossRef]
- Vinai, P.; Ferri, R.; Anelli, M.; Ferini-Strambi, L.; Zucconi, M.; Oldani, A.; Manconi, M. New data on psychological traits and sleep profiles of patients affected by nocturnal eating. Sleep Med. 2015, 16, 746–753. [Google Scholar] [CrossRef]
- Nagata, J.M.; Thurston, I.B.; Karazsia, B.T.; Woolridge, D.; Buckelew, S.M.; Murray, S.B.; Calzo, J.P. Self-reported eating disorders and sleep disturbances in young adults: A prospective cohort study. Eat. Weight Disord.-Stud. Anorex. Bulim. Obes. 2021, 26, 695–702. [Google Scholar] [CrossRef]
- Ralph-Nearman, C.; Williams, B.M.; Ortiz, A.M.L.; Smith, A.R.; Levinson, C.A. Pinpointing core and pathway symptoms among sleep disturbance, anxiety, worry, and eating disorder symptoms in anorexia nervosa and atypical anorexia nervosa. J. Affect. Disord. 2021, 294, 24–32. [Google Scholar] [CrossRef]
- Abdou, T.A.; Esawy, H.I.; Mohamed, G.A.R.; Ahmed, H.H.; Elhabiby, M.M.; Khalil, S.A.; El-Hawary, Y.A. Sleep profile in anorexia and bulimia nervosa female patients. Sleep Med. 2018, 48, 113–116. [Google Scholar] [CrossRef]
- Lombardo, C.; Battagliese, G.; Venezia, C.; Salvemini, V. Persistence of poor sleep predicts the severity of the clinical condition after 6 months of standard treatment in patients with eating disorders. Eat. Behav. 2015, 18, 16–19. [Google Scholar] [CrossRef]
- Allison, K.C.; Crow, S.J.; Reeves, R.R.; West, D.S.; Foreyt, J.P.; DiLillo, V.G.; Wadden, T.A.; Jeffery, R.W.; Van Dorsten, B.; Stunkard, A.J.; et al. Binge eating disorder and night eating syndrome in adults with type 2 diabetes. Obesity 2007, 15, 1287–1293. [Google Scholar] [CrossRef]
- Allison, K.C.; Lundgren, J.D.; Moore, R.H.; O’Reardon, J.P.; Stunkard, A.J. Cognitive behavior therapy for night eating syndrome: A pilot study. Am. J. Psychother. 2010, 64, 91–106. [Google Scholar] [CrossRef]
- Allison, K.C.; Studt, S.K.; Berkowitz, R.I.; Hesson, L.A.; Moore, R.H.; Dubroff, J.G.; Newberg, A.; Stunkard, A.J. An open-label efficacy trial of escitalopram for night eating syndrome. Eat. Behav. 2013, 14, 199–203. [Google Scholar] [CrossRef]
- Goel, N.; Stunkard, A.J.; Rogers, N.L.; Van Dongen, H.P.; Allison, K.C.; O’Reardon, J.P.; Ahima, R.S.; Cummings, D.E.; Heo, M.; Dinges, D.F. Circadian rhythm profiles in women with night eating syndrome. J. Biol. Rhythm. 2009, 24, 85–94. [Google Scholar] [CrossRef]
- Vander Wal, J.S.; Gang, C.H.; Griffing, G.T.; Gadde, K.M. Escitalopram for treatment of night eating syndrome: A 12-week, randomized, placebo-controlled trial. J. Clin. Psychopharmacol. 2012, 32, 341–345. [Google Scholar] [CrossRef]
- Buelow, M. Risky Decision Making in Psychological Disorders; Academic Press: Cambridge, MA, USA, 2020. [Google Scholar]
- Christensen, K.A.; Short, N.A. The case for investigating a bidirectional association between insomnia symptoms and eating disorder pathology. Int. J. Eat. Disord. 2021, 54, 701–707. [Google Scholar] [CrossRef]
- Christensen, K.A.; Forbush, K.T.; Elliott, B.T.; Jarmolowicz, D.P. A single-case multiple baseline design for treating insomnia in eating disorders: The TIRED study. Int. J. Eat. Disord. 2021, 54, 652–659. [Google Scholar] [CrossRef]
- Cousineau, H.; Marchand, A.; Bouchard, S.; Bélanger, C.; Gosselin, P.; Langlois, F.; Labrecque, J.; Dugas, M.J. Belleville, G. Insomnia Symptoms Following Treatment for Comorbid Panic Disorder With Agoraphobia and Generalized Anxiety Disorder. J. Nerv. Ment. Dis. 2016, 204, 267–273. [Google Scholar] [CrossRef]
- Chen, P.J.; Huang, C.L.C.; Weng, S.F.; Wu, M.P.; Ho, C.H.; Wang, J.J.; Tsai, W.C.; Hsu, Y.W. Relapse insomnia increases greater risk of anxiety and depression: Evidence from a population-based 4-year cohort study. Sleep Med. 2017, 38, 122–129. [Google Scholar] [CrossRef]
- Kenny, T.E.; Van Wijk, M.; Singleton, C.; Carter, J.C. An examination of the relationship between binge eating disorder and insomnia symptoms. Eur. Eat. Disord. Rev. 2018, 26, 186–196. [Google Scholar] [CrossRef]
- Hertenstein, E.; Feige, B.; Gmeiner, T.; Kienzler, C.; Spiegelhalder, K.; Johann, A.; Jansson-Fröjmark, M.; Palagini, L.; Rücker, G.; Riemann, D.; et al. Insomnia as a predictor of mental disorders: A systematic review and meta-analysis. Sleep Med. Rev. 2019, 43, 96–105. [Google Scholar] [CrossRef]
- Van Straten, A.; van der Zweerde, T.; Kleiboer, A.; Cuijpers, P.; Morin, C.M.; Lancee, J. Cognitive and behavioral therapies in the treatment of insomnia: A meta-analysis. Sleep Med. Rev. 2018, 38, 3–16. [Google Scholar] [CrossRef]
- Aarstad-Martin, S.; Boyraz, G. Posttraumatic stress, risky drinking, and prescription drug misuse in trauma-exposed college students. J. Loss Trauma 2017, 22, 599–612. [Google Scholar] [CrossRef]
- Babson, K.A.; Boden, M.T.; Harris, A.H.; Stickle, T.R.; Bonn-Miller, M.O. Poor sleep quality as a risk factor for lapse following a cannabis quit attempt. J. Subst. Abus. Treat. 2013, 44, 438–443. [Google Scholar] [CrossRef]
- Short, N.A.; Mathes, B.M.; Gibby, B.; Oglesby, M.E.; Zvolensky, M.J.; Schmidt, N.B. Insomnia symptoms as a risk factor for cessation failure following smoking cessation treatment. Addict. Res. Theory 2017, 25, 17–23. [Google Scholar] [CrossRef]
- Cortese, S.; Sabé, M.; Chen, C.; Perroud, N.; Solmi, M. Half a century of research on Attention-Deficit/Hyperactivity Disorder: A scientometric study. Neurosci. Biobehav. Rev. 2022, 140, 104769. [Google Scholar] [CrossRef] [PubMed]
- Sabe, M.; Chen, C.; Perez, N.; Solmi, M.; Mucci, A.; Galderisi, S.; Strauss, G.P.; Kaiser, S. Thirty years of research on negative symptoms of schizophrenia: A scientometric analysis of hotspots, bursts, and research trends. Neurosci. Biobehav. Rev. 2022, 144, 104979. [Google Scholar] [CrossRef] [PubMed]
- Zakaria, A.; Aryadoust, V. A scientometric analysis of applied linguistics research (1970–2022): Methodology and future directions. Appl. Linguist. Rev. 2023. [Google Scholar] [CrossRef]
- Hicks, D.; Wouters, P.; Waltman, L.; De Rijcke, S.; Rafols, I. Bibliometrics: The Leiden Manifesto for research metrics. Nature 2015, 520, 429–431. [Google Scholar] [CrossRef]

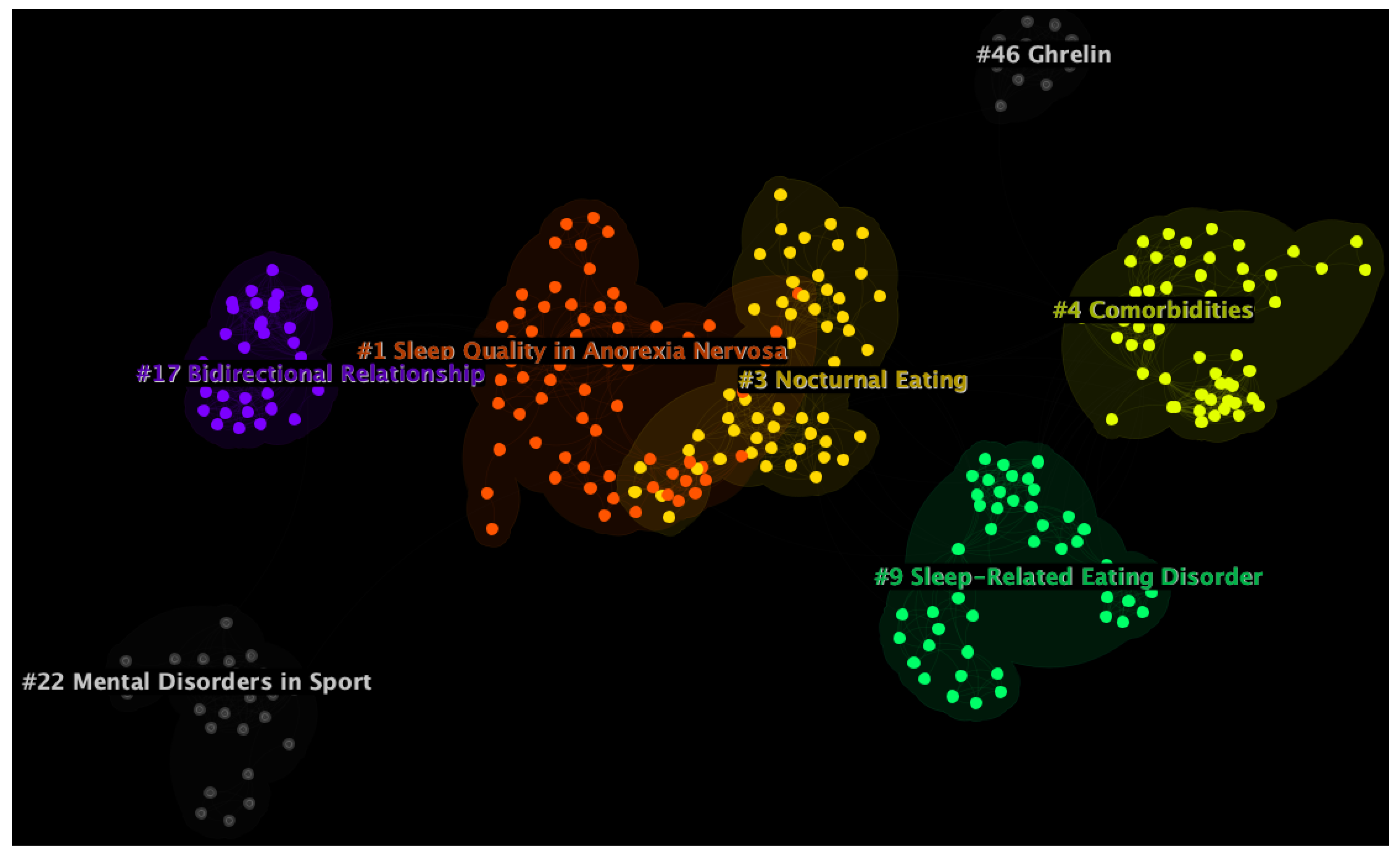
| Cluster ID | Size | Silhouette | Mean Year | LLR Label | Suggested Label |
|---|---|---|---|---|---|
| 1 | 69 | 0.956 | 2014 | sleep-related eating disorder | Sleep Quality in Anorexia Nervosa |
| 3 | 57 | 0.970 | 2007 | restless nocturnal eating | Nocturnal Eating |
| 4 | 56 | 0.973 | 2010 | depressed patient | Comorbidities |
| 9 | 48 | 0.991 | 2005 | sleep-related eating disorder | Sleep-Related Eating Disorder |
| 17 | 34 | 1.000 | 2015 | psychological disorder | Bidirectional Relationship |
| 22 | 25 | 0.995 | 2013 | common mental disorder | Mental Disorders in Sport |
| 46 | 11 | 0.999 | 2010 | psychiatric disorder | Ghrelin |
| References | Citation Burstness | Publication Year | Burst Begin | Burst End | Duration | Centrality | Sigma |
|---|---|---|---|---|---|---|---|
| Vetrugno et al. [43] | 8.3575 | 2006 | 2007 | 2012 | 5 | 0.00 | 1.03 |
| Morgenthaler and Silber [44] | 6.7376 | 2002 | 2005 | 2009 | 4 | 0.00 | 1.03 |
| Howell et al. [45] | 5.9064 | 2009 | 2010 | 2012 | 2 | 0.00 | 1.01 |
| Winkelman et al. [46] | 5.155 | 1999 | 2002 | 2006 | 4 | 0.00 | 1.00 |
| Allison et al. [2] | 4.7939 | 2016 | 2017 | 2021 | 4 | 0.01 | 1.04 |
| American Psychiatric Association [47] | 4.577 | 2013 | 2018 | 2021 | 3 | 1.01 | 1.04 |
| Winkelman [48] | 4.4768 | 2006 | 2009 | 2012 | 3 | 0.00 | 1.00 |
| Provini et al. [49] | 4.1406 | 2005 | 2011 | 2013 | 2 | 0.00 | 1.00 |
| Winkelman [50] | 3.9927 | 2003 | 2005 | 2011 | 6 | 0.00 | 1.00 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Carollo, A.; Zhang, P.; Yin, P.; Jawed, A.; Dimitriou, D.; Esposito, G.; Mangar, S. Sleep Profiles in Eating Disorders: A Scientometric Study on 50 Years of Clinical Research. Healthcare 2023, 11, 2090. https://doi.org/10.3390/healthcare11142090
Carollo A, Zhang P, Yin P, Jawed A, Dimitriou D, Esposito G, Mangar S. Sleep Profiles in Eating Disorders: A Scientometric Study on 50 Years of Clinical Research. Healthcare. 2023; 11(14):2090. https://doi.org/10.3390/healthcare11142090
Chicago/Turabian StyleCarollo, Alessandro, Pengyue Zhang, Peiying Yin, Aisha Jawed, Dagmara Dimitriou, Gianluca Esposito, and Stephen Mangar. 2023. "Sleep Profiles in Eating Disorders: A Scientometric Study on 50 Years of Clinical Research" Healthcare 11, no. 14: 2090. https://doi.org/10.3390/healthcare11142090
APA StyleCarollo, A., Zhang, P., Yin, P., Jawed, A., Dimitriou, D., Esposito, G., & Mangar, S. (2023). Sleep Profiles in Eating Disorders: A Scientometric Study on 50 Years of Clinical Research. Healthcare, 11(14), 2090. https://doi.org/10.3390/healthcare11142090






