High Levels of Anxiety, Depression, Risk of Suicide, and Implications for Treatment in Patients with Lamellar Ichthyosis
Abstract
1. Introduction
2. Materials and Methods
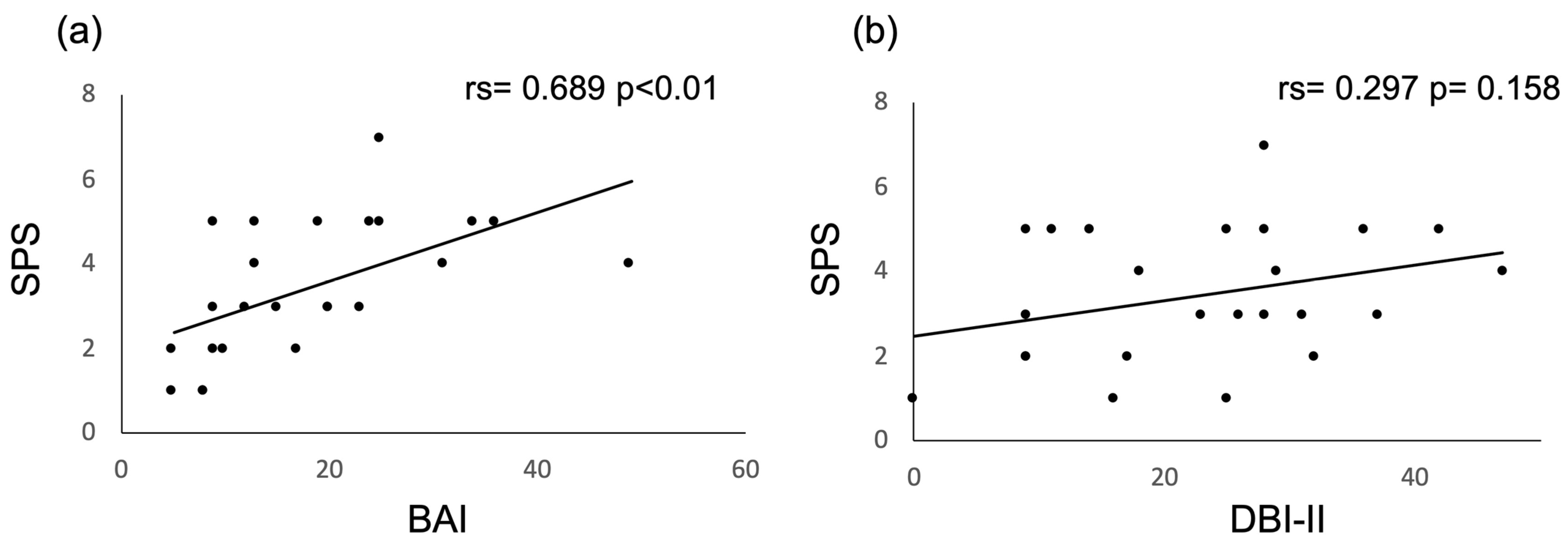
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Vahlquist, A.; Gånemo, A.; Virtanen, M. Congenital ichthyosis: An overview of current and emerging therapies. Acta Derm. Venereol. 2008, 88, 4–14. [Google Scholar] [CrossRef]
- Schmuth, M.; Gruber, R.; Elias, P.M.; Williams, M.L. Ichthyosis update: Towards a function-driven model of pathogenesis of the disorders of cornification and the role of corneocyte proteins in these disorders. Adv. Dermatol. 2007, 23, 231–256. [Google Scholar] [CrossRef]
- González-Del Carmen, M.; Montaño, S.; Reyes-Hernández, O.D.; Vizcaíno-Dorado, P.A.; Leyva-García, N.; Morales-Morfín, J.C.; Diaz-Beltran, W.; Quinto-Santiago, E.; Msc, L.C.; Magaña, J.J.; et al. High prevalence of autosomal recessive congenital ichthyosis in a Mexican population caused by a new mutation in the TGM1 gene: Epidemiological evidence of a founder effect. Int. J. Dermatol. 2020, 59, 969–977. [Google Scholar] [CrossRef]
- Rodríguez-Pazos, L.; Ginarte, M.; Fachal, L.; Toribio, J.; Carracedo, A.; Vega, A. Analysis of TGM1, ALOX12B, ALOXE3, NIPAL4 and CYP4F22 in autosomal recessive congenital ichthyosis from Galicia (NW Spain): Evidence of founder effects. Br. J. Dermatol. 2011, 165, 906–911. [Google Scholar] [CrossRef] [PubMed]
- Hernández-Martín, A.; Garcia-Doval, I.; Aranegui, B.; De Unamuno, P.; Rodríguez-Pazos, L.; González-Enseñat, M.A.; Vicente, A.; Martín-Santiago, A.; Garcia-Bravo, B.; Feito, M.; et al. Prevalence of autosomal recessive congenital ichthyosis: A population-based study using the capture-recapture method in Spain. J. Am. Acad. Dermatol. 2012, 67, 240–244. [Google Scholar] [CrossRef] [PubMed]
- Kurosawa, M.; Uehara, R.; Takagi, A.; Aoyama, Y.; Iwatsuki, K.; Amagai, M.; Nagai, M.; Nakamura, Y.; Inaba, Y.; Yokoyama, K.; et al. Results of a nationwide epidemiologic survey of autosomal recessive congenital ichthyosis and ichthyosis syndromes in Japan. J. Am. Acad. Dermatol. 2019, 81, 1086–1092. [Google Scholar] [CrossRef] [PubMed]
- Guo, F.; Yu, Q.; Liu, Z.; Zhang, C.; Li, P.; Xu, Y.; Zuo, Y.; Zhang, G.; Li, Y.; Liu, H. Evaluation of life quality, anxiety, and depression in patients with skin diseases. Medicine 2020, 99, e22983. [Google Scholar] [CrossRef] [PubMed]
- Sun, Q.; Ren, I.; Zaki, T.; Maciejewski, K.; Choate, K. Ichthyosis affects mental health in adults and children: A cross-sectional study. J. Am. Acad. Dermatol. 2020, 83, 951–954. [Google Scholar] [CrossRef]
- Wren, G.H.; Humby, T.; Thompson, A.R.; Davies, W. Mood symptoms, neurodevelopmental traits, and their contributory factors in X-linked ichthyosis, ichthyosis vulgaris and psoriasis. Clin. Exp. Dermatol. 2022, 47, 1097–1108. [Google Scholar] [CrossRef] [PubMed]
- Showraki, M.; Showraki, T.; Brown, K. Generalized Anxiety Disorder: Revisited. Psychiatr. Q. 2020, 91, 905–914. [Google Scholar] [CrossRef] [PubMed]
- Fried, R.G.; Gupta, M.A.; Gupta, A.K. Depression and skin disease. Dermatol. Clin. 2005, 23, 657–664. [Google Scholar] [CrossRef] [PubMed]
- Bentley, K.H.; Franklin, J.C.; Ribeiro, J.D.; Kleiman, E.M.; Fox, K.R.; Nock, M.K. Anxiety and its disorders as risk factors for suicidal thoughts and behaviors: A meta-analytic review. Clin. Psychol. Rev. 2016, 43, 30–46. [Google Scholar] [CrossRef] [PubMed]
- Norton, P.J.; Temple, S.R.; Pettit, J.W. Suicidal ideation and anxiety disorders: Elevated risk or artifact of comorbid depression? J. Behav. Ther. Exp. Psychiatry 2008, 39, 515–525. [Google Scholar] [CrossRef]
- World Health Organization Suicide: Key Facts. 2021. Available online: https://www.who.int/news-room/fact-sheets/detail/suicide (accessed on 7 July 2022).
- Picardi, A.; Lega, I.; Tarolla, E. Suicide risk in skin disorders. Clin. Dermatol. 2013, 31, 47–56. [Google Scholar] [CrossRef] [PubMed]
- Dieris-Hirche, J.; Gieler, U.; Petrak, F.; Milch, W.; te Wildt, B.; Dieris, B.; Herpertz, S. Suicidal ideation in adult patients with atopic dermatitis: A German cross-sectional study. Acta Derm. Venereol. 2017, 97, 1189–1195. [Google Scholar] [CrossRef]
- Pompili, M.; Bonanni, L.; Gualtieri, F.; Trovini, G.; Persechino, S.; Baldessarini, R.J. Suicidal risks with psoriasis and atopic dermatitis: Systematic review and meta-analysis. J. Psychosom Res. 2021, 141, 110347. [Google Scholar] [CrossRef] [PubMed]
- Sandhu, J.K.; Wu, K.K.; Bui, T.L.; Armstrong, A.W. Association between Atopic Dermatitis and Suicidality: A Systematic Review and Meta-analysis. JAMA Dermatol. 2019, 155, 178–187. [Google Scholar] [CrossRef]
- Cortés, H.; Rojas-Márquez, M.; Reyes-Hernández, O.D.; Morales-Morfín, J.C.; Guapillo-Vargas, M.R.B.; Varela-Cardoso, M.; Magaña, J.J.; Leyva-Gómez, G.; González-del Carmen, M. Increased risk of depression and impairment in quality of life in patients with lamellar ichthyosis. Dermatol. Ther. 2021, 34, e14628. [Google Scholar] [CrossRef]
- Wang, Y.-P.; Gorenstein, C. Psychometric properties of the Beck Depression Inventory-II: A comprehensive review. Rev. Bras Psiquiatr. 2013, 35, 416–431. [Google Scholar] [CrossRef] [PubMed]
- Sanz, J. Recomendaciones para la utilizacion de la adaptacion espanola del Inventario de Ansiedad de Beck (BAI) en la practica clinica. Clin. Salud 2014, 25, 39–48. [Google Scholar] [CrossRef]
- Hockberger, R.S.; Rothstein, R.J. Assessment of suicide potential by nonpsychiatrists using the SAD PERSONS score. J. Emerg. Med. 1988, 6, 99–107. [Google Scholar] [CrossRef] [PubMed]
- Chandramouleeswaran, S.; Edwin, N.C.; Victor, P.J.; Tharyan, P. The emergency physician’s assessment of suicide risk in intentional self-poisoning using the modified SAD PERSONS scale versus standard psychiatric evaluation in a general hospital in South India: A cross-sectional study. Trop. Doct. 2015, 45, 21–26. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.-Y.; Huang, H.-C.; Wu, S.-I.; Sun, F.-J.; Huang, C.-R.; Liu, S.-I. Validation of the Chinese SAD PERSONS Scale to predict repeated self-harm in emergency attendees in Taiwan. BMC Psychiatry 2014, 14, 44. [Google Scholar] [CrossRef] [PubMed]
- Kamalpour, L.; Rice, Z.P.; Pavlis, M.; Veledar, E.; Chen, S.C. Reliable methods to evaluate the clinical severity of ichthyosis. Pediatr. Dermatol. 2010, 27, 148–153. [Google Scholar] [CrossRef]
- Cortés, H.; Magaña, J.J.; Reyes-Hernández, O.D.; Zacaula-Juárez, N.; González-Torres, M.; Diaz-Beltrán, W.; León-Trejo, M.C.; Cariño-Calvo, L.; Leyva-Gómez, G.; Carmen, M.G. Non-invasive analysis of skin mechanical properties in patients with lamellar ichthyosis. Skin Res. Technol. 2019, 25, 375–381. [Google Scholar] [CrossRef] [PubMed]
- Cortés, H.; Rojas-Márquez, M.; Del Prado-Audelo, M.L.; Reyes-Hernández, O.D.; González-Del Carmen, M.; Leyva-Gómez, G. Alterations in mental health and quality of life in patients with skin disorders: A narrative review. Int. J. Dermatol. 2022, 61, 783–791. [Google Scholar] [CrossRef]
- Keefner, T.P.; Stenvig, T. Suicidality: An Evolutionary Concept Analysis. Issues Ment. Health Nurs. 2021, 42, 227–238. [Google Scholar] [CrossRef] [PubMed]
- Gupta, M.A.; Pur, D.R.; Vujcic, B.; Gupta, A.K. Suicidal behaviors in the dermatology patient. Clin. Dermatol. 2017, 35, 302–311. [Google Scholar] [CrossRef]
- Thyssen, J.P.; Hamann, C.R.; Linneberg, A.; Dantoft, T.M.; Skov, L.; Gislason, G.H.; Wu, J.J.; Egeberg, A. Atopic dermatitis is associated with anxiety, depression, and suicidal ideation, but not with psychiatric hospitalization or suicide. Allergy Eur. J. Allergy Clin. Immunol. 2018, 73, 214–220. [Google Scholar] [CrossRef]
- Rønnstad, A.T.M.; Halling-Overgaard, A.S.; Hamann, C.R.; Skov, L.; Egeberg, A.; Thyssen, J.P. Association of atopic dermatitis with depression, anxiety, and suicidal ideation in children and adults: A systematic review and meta-analysis. J. Am. Acad. Dermatol. 2018, 79, 448–456. [Google Scholar] [CrossRef]
- Kelly, K.A.; Balogh, E.A.; Kaplan, S.G.; Feldman, S.R. Skin Disease in Children: Effects on Quality of Life, Stigmatization, Bullying, and Suicide Risk in Pediatric Acne, Atopic Dermatitis, and Psoriasis Patients. Child 2021, 8, 1057. [Google Scholar] [CrossRef] [PubMed]
- Picardi, A.; Mazzotti, E.; Pasquini, P. Prevalence and correlates of suicidal ideation among patients with skin disease. J. Am. Acad. Dermatol. 2006, 54, 420–426. [Google Scholar] [CrossRef] [PubMed]
- Xu, S.; Zhu, Y.; Hu, H.; Liu, X.; Li, L.; Yang, B.; Wu, W.; Liang, Z.; Deng, D. The analysis of acne increasing suicide risk. Medicine 2021, 100, e26035. [Google Scholar] [CrossRef] [PubMed]
- Lukaviciute, L.; Navickas, P.; Navickas, A.; Grigaitiene, J.; Ganceviciene, R.; Zouboulis, C.C. Quality of life, anxiety prevalence, depression symptomatology and suicidal ideation among acne patients in Lithuania. J. Eur. Acad. Dermatol. Venereol. 2017, 31, 1900–1906. [Google Scholar] [CrossRef] [PubMed]
- Pavon Blanco, A.; Turner, M.A.; Petrof, G.; Weinman, J. To what extent do disease severity and illness perceptions explain depression, anxiety and quality of life in hidradenitis suppurativa? Br. J. Dermatol. 2019, 180, 338–345. [Google Scholar] [CrossRef] [PubMed]
- Thorlacius, L.; Cohen, A.D.; Gislason, G.H.; Jemec, G.B.E.; Egeberg, A. Increased Suicide Risk in Patients with Hidradenitis Suppurativa. J. Investig. Dermatol. 2018, 138, 52–57. [Google Scholar] [CrossRef] [PubMed]
- Cavenagh, A.; Chatterjee, S.; Davies, W. Behavioural and psychiatric phenotypes in female carriers of genetic mutations associated with X-linked ichthyosis. PLoS ONE 2019, 14, e0212330. [Google Scholar] [CrossRef]
- Lang, U.E.; Borgwardt, S. Molecular mechanisms of depression: Perspectives on new treatment strategies. Cell Physiol. Biochem. 2013, 31, 761–777. [Google Scholar] [CrossRef]
- Cortés, H.; Del Prado-Audelo, M.L.; Urbán-Morlán, Z.; Alcalá-Alcalá, S.; González-Torres, M.; Reyes-Hernández, O.D.; Carmen, M.G.-D.; Leyva-Gómez, G. Pharmacological treatments for cutaneous manifestations of inherited ichthyoses. Arch. Dermatol. Res. 2020, 312, 237–248. [Google Scholar] [CrossRef]
- Zaenglein, A.L.; Levy, M.L.; Stefanko, N.S.; Benjamin, L.T.; Bruckner, A.L.; Choate, K.; Craiglow, B.G.; DiGiovanna, J.J.; Eichenfield, L.F.; Elias, P.; et al. Consensus recommendations for the use of retinoids in ichthyosis and other disorders of cornification in children and adolescents. Pediatr. Dermatol. 2021, 38, 164–180. [Google Scholar] [CrossRef]
- Paljarvi, T.; McPherson, T.; Luciano, S.; Herttua, K.; Fazel, S. Isotretinoin and adverse neuropsychiatric outcomes: Retrospective cohort study using routine data. Br. J. Dermatol. 2022, 187, 64–72. [Google Scholar] [CrossRef] [PubMed]
- Abdelmaksoud, A.; Vojvodic, A.; Ayhan, E.; Dönmezdil, S.; Jovicevic, T.V.; Vojvodic, P.; Lotti, T.; Vestita, M. Depression, isotretinoin, and folic acid: A practical review. Dermatol. Ther. 2019, 32, e13104. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Kim, J.; Lee, Y.I.; Suk, J.; Lee, D.; Lee, J.H. A pilot study evaluating the efficacy and safety of retinaldehyde-loaded niosomes against mild-to-moderate acne. J. Cosmet Dermatol. 2021, 20, 3586–3592. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Zheng, A.; Peng, B.; Xu, Y.; Zhang, N. Size-Dependent Absorption through Stratum Corneum by Drug-Loaded Liposomes. Pharm. Res. 2021, 38, 1429–1437. [Google Scholar] [CrossRef]
- Samadi, A.; Sartipi, Z.; Ahmad Nasrollahi, S.; Sheikholeslami, B.; Kashani, M.N.; Rouini, M.R.; Dinarvand, R.; Firooz, A. Efficacy assessments of tretinoin-loaded nano lipid carriers in acne vulgaris: A double blind, split-face randomized clinical study. Arch. Dermatol. Res. 2022, 314, 553–561. [Google Scholar] [CrossRef] [PubMed]
- Marathe, K.; Teng, J.M.C.; Guenthner, S.; Bunick, C.G.; Kempers, S.; Eads, K.; Castelo-Soccio, L.; Mendelsohn, A.M.; Raiz, J.; Murrell, D.F. Topical Isotretinoin (TMB-001) Treatment for 12 Weeks Did Not Result in Clinically Relevant Laboratory Abnormalities in Participants with Congenital Ichthyosis in the Phase 2b CONTROL Study. Dermatol. Ther. 2023, 13, 1255–1264. [Google Scholar] [CrossRef]
- Wincewicz, K.; Nasierowski, T. Electrodermal activity and suicide risk assessment in patients with affective disorders. Psychiatr. Pol. 2020, 54, 1137–1147. [Google Scholar] [CrossRef]

| Clinical Features | n (%) |
|---|---|
| Collodion membrane a | 24 (100) |
| Brown plate-like scales b | 24 (100) |
| Palmoplantar hyperkeratosis b | 24 (100) |
| Palmoplantar hyperlinearity b | 21 (87) |
| Hypohidrosis a | 21 (87) |
| Pruritus a | 21 (87) |
| Ectropion b | 20 (83) |
| Scarring alopecia b | 19 (79) |
| Digital contractures b | 15 (62) |
| Subungual hyperkeratosis b | 7 (29) |
| Onychogryphosis b | 4 (16) |
| Malformation of the nose and ear cartilage b | 2 (8) |
| Keratosis pilaris b | 2 (8) |
| N (%) | p-Value * | Cramer’s V | |||||
|---|---|---|---|---|---|---|---|
| Anxiety | |||||||
| Minimum | Mild | Moderate | Severe | ||||
| LI | 24 (100) | 2 (8) | 10 (41) | 8 (33) | 4 (16) | 0.028 | 0.429 |
| Control | 24 (100) | 11 (45) | 5 (20) | 6 (25) | 2 (8) | ||
| Depression | |||||||
| Minimum | Mild | Moderate | Severe | ||||
| LI | 24 (100) | 5 (20) | 5 (20) | 7 (29) | 7 (29) | 0.001 | 0.594 |
| Control | 24 (100) | 19 (79) | 1 (4) | 3 (12) | 1 (4) | ||
| Suicide risk | |||||||
| No risk | Low | Medium | High | ||||
| LI | 24 (100) | 7 (29) | 9 (37) | 7 (29) | 1 (4) | 0.011 | 0.462 |
| Control | 24 (100) | 17 (70) | 6 (25) | 1 (4) | 0 (0) | ||
| N | Median a (Range) | p-Value b | OR c | |
|---|---|---|---|---|
| BAI | ||||
| LI | 24 | 16 (5–49) | 0.011 | 9.3 (1.778, 48.723) |
| Control | 24 | 10 (0–34) | ||
| DBI-II | ||||
| LI | 24 | 25 (0–47) | <0.001 | 14.4 (3.58, 58.15) |
| Control | 24 | 8.5 (2–33) | ||
| SAD PERSONS | ||||
| LI | 24 | 3 (1–7) | 0.001 | 5.8 (1.699, 20.48) |
| Control | 24 | 2 (0–6) |
| N | Median a (Range) | p-Value b | OR c | |
|---|---|---|---|---|
| LI | ||||
| Comorbidity of anxiety and depression | 17 | 4 (1–7) | 0.02 | 18.7 (2.06, 170.2) |
| Only depression or anxiety | 7 | 2 (1–5) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cortés, H.; Cariño-Calvo, L.; Reyes-Hernández, O.D.; Rojas-Márquez, M.; Magaña, J.J.; Vizcaino-Dorado, P.A.; Villegas-Vazquez, E.Y.; Quintas-Granados, L.I.; Jiménez-Islas, E.; Cortés-Mollinedo, V.A.; et al. High Levels of Anxiety, Depression, Risk of Suicide, and Implications for Treatment in Patients with Lamellar Ichthyosis. Healthcare 2023, 11, 2071. https://doi.org/10.3390/healthcare11142071
Cortés H, Cariño-Calvo L, Reyes-Hernández OD, Rojas-Márquez M, Magaña JJ, Vizcaino-Dorado PA, Villegas-Vazquez EY, Quintas-Granados LI, Jiménez-Islas E, Cortés-Mollinedo VA, et al. High Levels of Anxiety, Depression, Risk of Suicide, and Implications for Treatment in Patients with Lamellar Ichthyosis. Healthcare. 2023; 11(14):2071. https://doi.org/10.3390/healthcare11142071
Chicago/Turabian StyleCortés, Hernán, Lizbeth Cariño-Calvo, Octavio D. Reyes-Hernández, Martín Rojas-Márquez, Jonathan J. Magaña, Pablo A. Vizcaino-Dorado, Edgar Y. Villegas-Vazquez, Laura Itzel Quintas-Granados, Elizabeth Jiménez-Islas, Valeria A. Cortés-Mollinedo, and et al. 2023. "High Levels of Anxiety, Depression, Risk of Suicide, and Implications for Treatment in Patients with Lamellar Ichthyosis" Healthcare 11, no. 14: 2071. https://doi.org/10.3390/healthcare11142071
APA StyleCortés, H., Cariño-Calvo, L., Reyes-Hernández, O. D., Rojas-Márquez, M., Magaña, J. J., Vizcaino-Dorado, P. A., Villegas-Vazquez, E. Y., Quintas-Granados, L. I., Jiménez-Islas, E., Cortés-Mollinedo, V. A., Leyva-Gómez, G., & González-Del Carmen, M. (2023). High Levels of Anxiety, Depression, Risk of Suicide, and Implications for Treatment in Patients with Lamellar Ichthyosis. Healthcare, 11(14), 2071. https://doi.org/10.3390/healthcare11142071








