Systematic Review and Meta-Analysis of the Correlation Coefficients between Nomophobia and Anxiety, Smartphone Addiction, and Insomnia Symptoms
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria
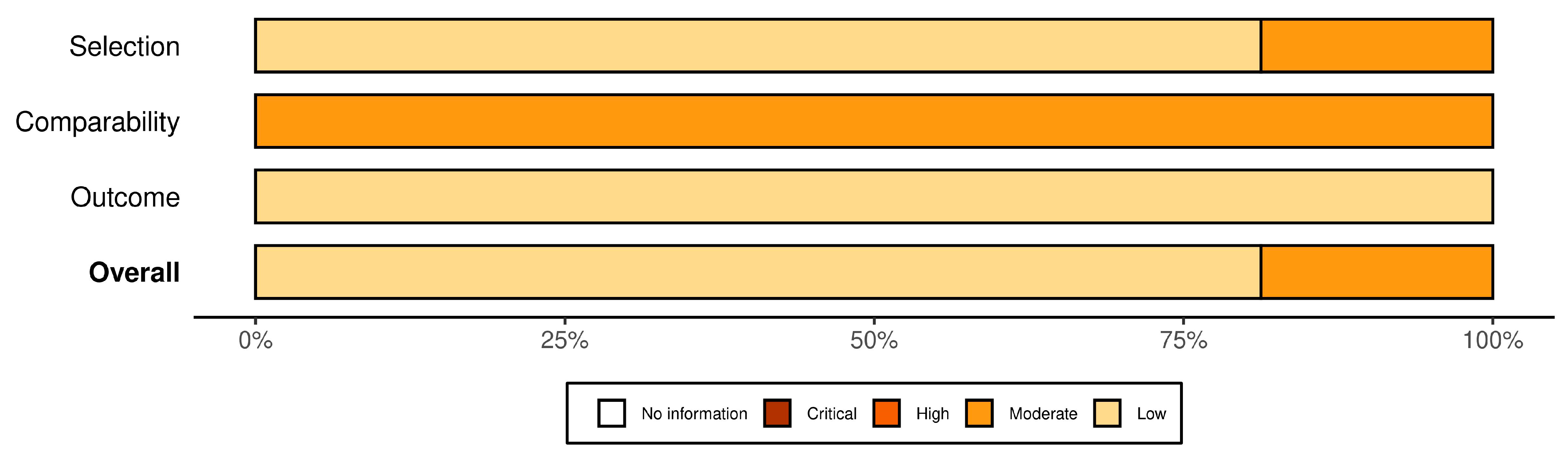
2.3. Data Extraction and Quality Assessment
2.4. Measures
2.4.1. Anxiety Outcomes
2.4.2. Smartphone Addiction Outcomes
2.4.3. Insomnia Outcomes
2.5. Statistical Analysis
3. Results
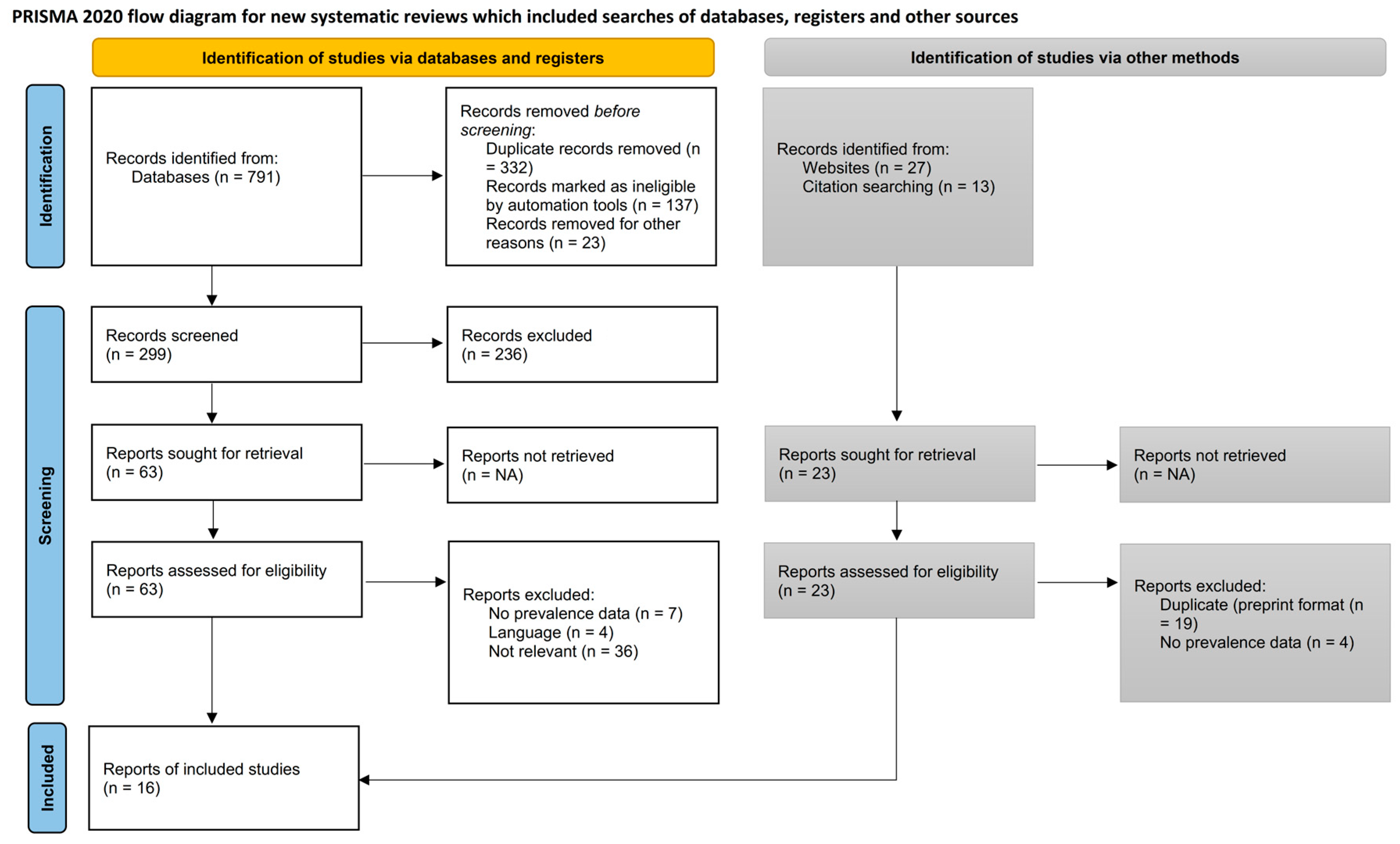
3.1. Study Identification
3.2. Characteristics of the Included Studies
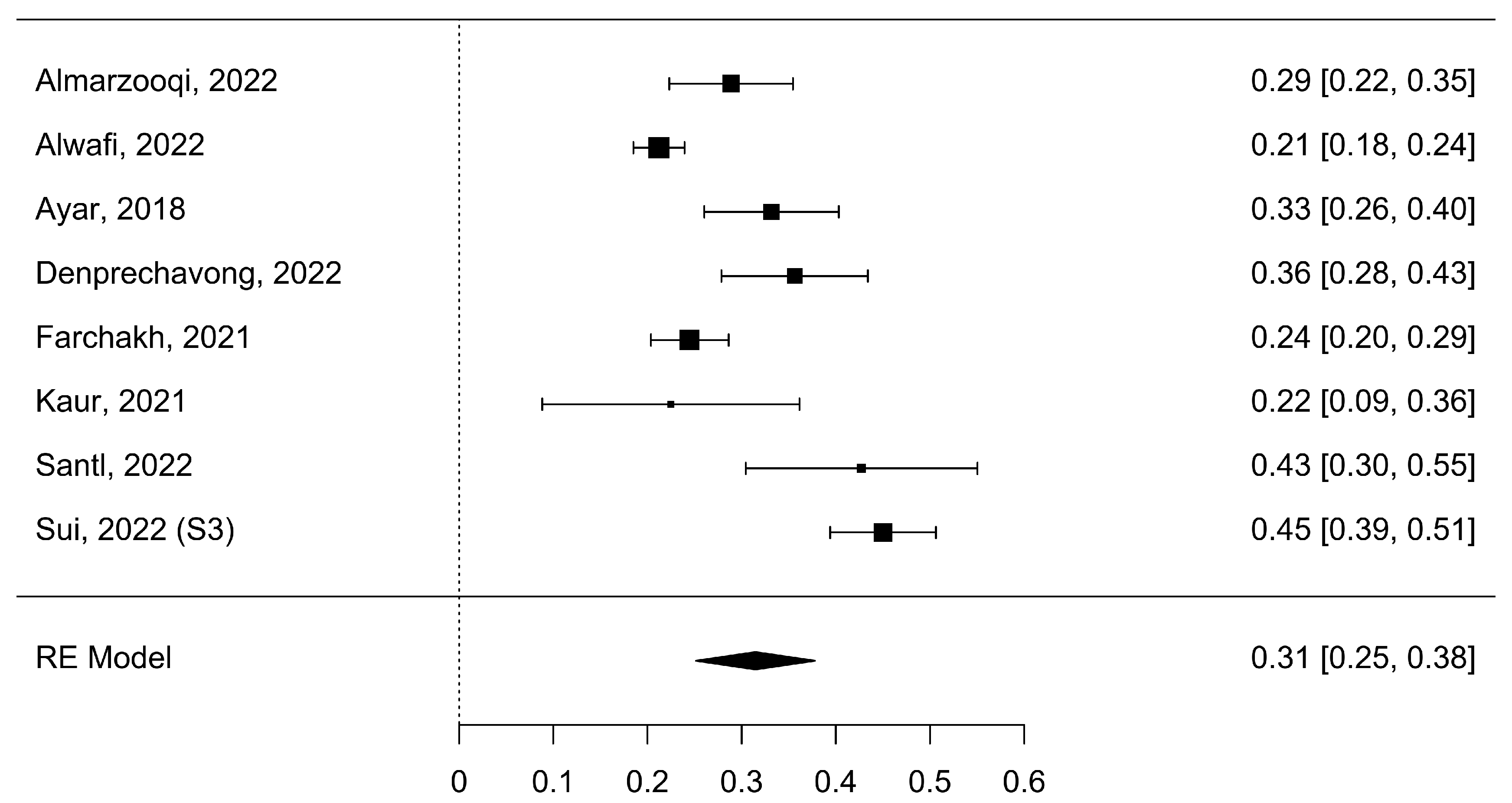
3.3. Nomophobia Symptoms with Anxiety (NSA)
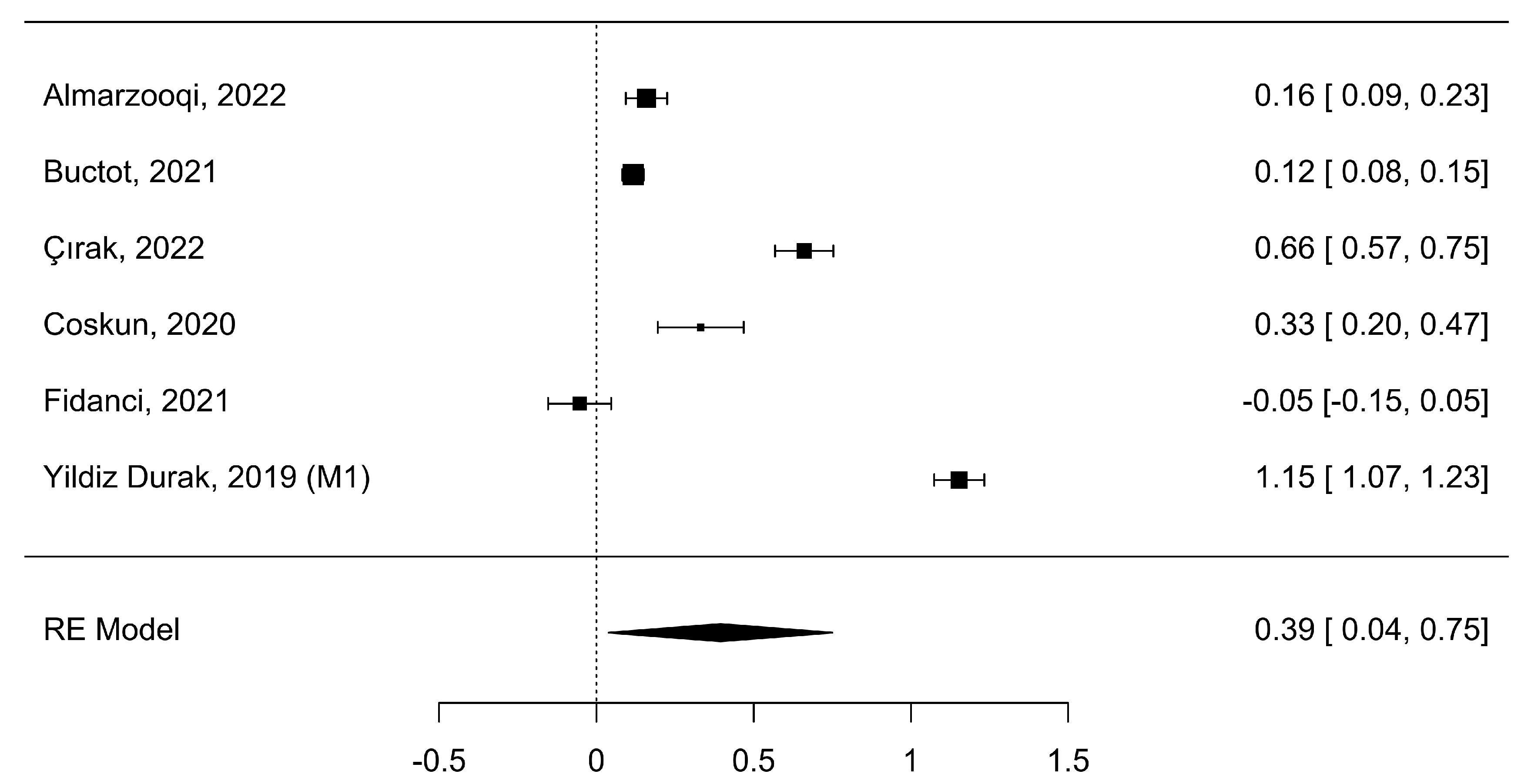
3.4. Nomophobia Symptoms with Smartphone Addiction (NSSA)
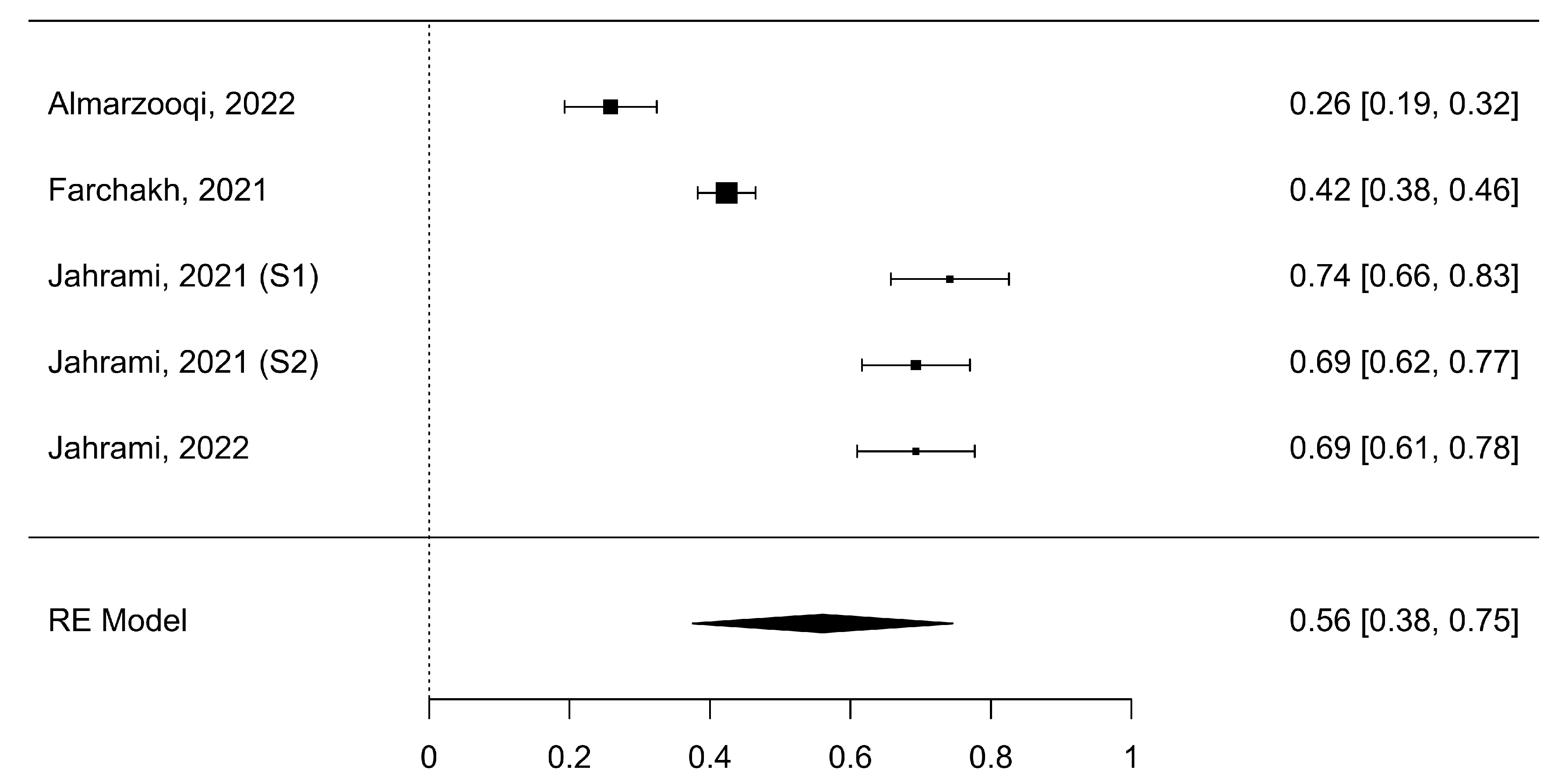
3.5. Nomophobia Symptoms with Insomnia (NSI)
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ayar, D.; Gerçeker, G.Ö.; Özdemir, E.Z.; Bektas, M. The effect of problematic internet use, social appearance anxiety, and social media use on nursing students’ nomophobia levels. CIN Comput. Inform. Nurs. 2018, 36, 589–595. [Google Scholar] [CrossRef] [PubMed]
- Jahrami, H.; Abdelaziz, A.; Binsanad, L.; Alhaj, O.A.; Buheji, M.; Bragazzi, N.L.; Saif, Z.; BaHammam, A.S.; Vitiello, M.V. The association between symptoms of nomophobia, insomnia and food addiction among young adults: Findings of an exploratory cross-sectional survey. Int. J. Environ. Res. Public Health 2021, 18, 711. [Google Scholar] [CrossRef] [PubMed]
- Jahrami, H.; Trabelsi, K.; Boukhris, O.; Hussain, J.H.; Alenezi, A.F.; Humood, A.; Saif, Z.; Pandi-Perumal, S.R.; Seeman, M.V. The Prevalence of Mild, Moderate, and Severe Nomophobia Symptoms: A Systematic Review, Meta-Analysis, and Meta-Regression. Behav. Sci. 2022, 13, 35. [Google Scholar] [CrossRef]
- Farchakh, Y.; Hallit, R.; Akel, M.; Chalhoub, C.; Hachem, M.; Hallit, S.; Obeid, S. Nomophobia in Lebanon: Scale validation and association with psychological aspects. PLoS ONE 2021, 16, e0249890. [Google Scholar] [CrossRef] [PubMed]
- ÇIRAK, M.; Dost, M.T. Nomophobia in university students: The roles of digital addiction, social connectedness, and life satisfaction. Turk. Psychol. Couns. Guid. J. 2022, 12, 35–52. [Google Scholar] [CrossRef]
- Jahrami, H.; Saif, Z.; Trabelsi, K.; Bragazzi, N.L.; Vitiello, M.V. Internal consistency and structural validity of the nomophobia questionnaire (NMP-Q) and its translations: A systematic review with meta-analysis. Heliyon 2023, 9, e15464. [Google Scholar] [CrossRef]
- Jahrami, H. The Relationship between Nomophobia, Insomnia, Chronotype, Phone in Proximity, Screen Time, and Sleep Duration in Adults: A Mobile Phone App-Assisted Cross-Sectional Study. Healthcare 2023, 11, 1503. [Google Scholar] [CrossRef]
- Arnold, E. Anxiety DSM-5 Diagnostic Criteria and Treatment Overview. Available online: https://pro.psycom.net/assessment-diagnosis-adherence/anxiety (accessed on 21 April 2023).
- Buctot, D.B.; Kim, N.; Kim, S.H. The role of nomophobia and smartphone addiction in the lifestyle profiles of junior and senior high school students in the Philippines. Soc. Sci. Humanit. Open 2020, 2, 100035. [Google Scholar]
- Taft, T. DSM-5 Criteria for Insomnia. Available online: https://psychcentral.com/disorders/insomnia-symptoms (accessed on 21 April 2023).
- AlMarzooqi, M.A.; Alhaj, O.A.; Alrasheed, M.M.; Helmy, M.; Trabelsi, K.; Ebrahim, A.; Hattab, S.; Jahrami, H.A.; Ben Saad, H. Symptoms of Nomophobia, Psychological Aspects, Insomnia and Physical Activity: A Cross-Sectional Study of ESports Players in Saudi Arabia. Healthcare 2022, 10, 257. [Google Scholar] [CrossRef]
- Jahrami, H.; Fekih-Romdhane, F.; Saif, Z.; Bragazzi, N.L.; Pandi-Perumal, S.R.; BaHammam, A.S.; Vitiello, M.V. A social media outage was associated with a surge in nomophobia, and the magnitude of change in nomophobia during the outage was associated with baseline insomnia. Clocks Sleep 2022, 4, 508–519. [Google Scholar] [CrossRef]
- Lin, C.-Y.; Potenza, M.N.; Ulander, M.; Broström, A.; Ohayon, M.M.; Chattu, V.K.; Pakpour, A.H. Longitudinal relationships between nomophobia, addictive use of social media, and insomnia in adolescents. Healthcare 2021, 9, 1201. [Google Scholar] [CrossRef] [PubMed]
- Stang, A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur. J. Epidemiol. 2010, 25, 603–605. [Google Scholar] [CrossRef] [PubMed]
- Löwe, B.; Decker, O.; Müller, S.; Brähler, E.; Schellberg, D.; Herzog, W.; Herzberg, P.Y. Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Med. Care 2008, 46, 266–274. [Google Scholar] [CrossRef] [PubMed]
- Hart, T.A.; Flora, D.B.; Palyo, S.A.; Fresco, D.M.; Holle, C.; Heimberg, R.G. Development and examination of the social appearance anxiety scale. Assessment 2008, 15, 48–59. [Google Scholar] [CrossRef]
- Nilchaikovit, T. Development of Thai version of hospital anxiety and depression scale in cancer patients. J. Psychiatr. Assoc. Thail. 1996, 4, 18–30. [Google Scholar]
- Hamilton, M. The assessment of anxiety states by rating. Br. J. Med. Psychol. 1959, 32, 50–55. [Google Scholar] [CrossRef]
- Mattick, R.P.; Clarke, J.C. Development and validation of measures of social phobia scrutiny fear and social interaction anxiety. Behav. Res. Ther. 1998, 36, 455–470. [Google Scholar] [CrossRef]
- Lovibond, P.F.; Lovibond, S.H. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav. Res. Ther. 1995, 33, 335–343. [Google Scholar] [CrossRef]
- Spielberger, C. Manual for the State-Trait Anxiety Inventory (Form Y). 121; Consulting Psychologists Press: Palo Alto, CA, USA, 1983. [Google Scholar]
- Nichols, L.A.; Nicki, R. Development of a psychometrically sound internet addiction scale: A preliminary step. Psychol. Addict. Behav. 2004, 18, 381. [Google Scholar] [CrossRef]
- Kwon, M.; Lee, J.-Y.; Won, W.-Y.; Park, J.-W.; Min, J.-A.; Hahn, C.; Gu, X.; Choi, J.-H.; Kim, D.-J. Development and validation of a smartphone addiction scale (SAS). PLoS ONE 2013, 8, e56936. [Google Scholar] [CrossRef]
- Şahin, C.; Yağcı, M. Social media addiction scale-adult form: The reliability and validity study. J. Ahi Evran Univ. Kırşehir Fac. Educ. 2017, 18, 523–538. [Google Scholar]
- Morin, C.M.; Belleville, G.; Bélanger, L.; Ivers, H. The Insomnia Severity Index: Psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep 2011, 34, 601–608. [Google Scholar] [CrossRef] [PubMed]
- Hallit, S.; Sacre, H.; Haddad, C.; Malaeb, D.; Al Karaki, G.; Kheir, N.; Hajj, A.; Hallit, R.; Salameh, P. Development of the Lebanese insomnia scale (LIS-18): A new scale to assess insomnia in adult patients. BMC Psychiatry 2019, 19, 421. [Google Scholar] [CrossRef] [PubMed]
- Laliberté, E.; Laliberté, M.E. Package ‘Metacor’, Version 1.0-2.1; The R Foundation: Vienna, Austria, 2009. [Google Scholar]
- Biggerstaff, B.J.; Tweedie, R.L. Incorporating variability in estimates of heterogeneity in the random effects model in meta-analysis. Stat. Med. 1997, 16, 753–768. [Google Scholar] [CrossRef]
- Higgins, J.P.; Thompson, S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef]
- Egger, M.; Davey Smith, G.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997, 315, 629–634. [Google Scholar] [CrossRef]
- Lin, L.; Chu, H. Quantifying publication bias in meta-analysis. Biometrics 2018, 74, 785–794. [Google Scholar] [CrossRef]
- Shi, L.; Lin, L. The trim-and-fill method for publication bias: Practical guidelines and recommendations based on a large database of meta-analyses. Medicine 2019, 98, e15987. [Google Scholar] [CrossRef]
- McGuinness, L.A.; Higgins, J.P.T. Risk-of-bias VISualization (robvis): An R package and Shiny web app for visualizing risk-of-bias assessments. Res. Synth. Methods 2021, 12, 55–61. [Google Scholar] [CrossRef]
- Alwafi, H.; Naser, A.Y.; Aldhahir, A.M.; Fatani, A.I.; Alharbi, R.A.; Alharbi, K.G.; Almutwakkil, B.A.; Salawati, E.; Ekram, R.; Samannodi, M. Prevalence and predictors of nomophobia among the general population in two middle eastern countries. BMC Psychiatry 2022, 22, 520. [Google Scholar] [CrossRef]
- Karademir Coskun, T.; Kaya, O. The Distribution of Variables That Affect Nomophobia in Adults’ Profiles. Int. J. Res. Educ. Sci. 2020, 6, 534–550. [Google Scholar] [CrossRef]
- Denprechavong, V.; Ngamchaliew, P.; Buathong, N. Prevalence of Nomophobia and Relationship with Anxiety and Depression among University Students in Southern Thailand. J. Med. Assoc. Thail. 2022, 105, 359–367. [Google Scholar]
- Fidancı, İ.; Aksoy, H.; Ayhan Başer, D.; Yengil Taci, D.; Cankurtaran, M. Evaluation of Nomophobia and Smartphone Addiction Levels among University Students in terms of Alcohol and Drug Abuse Risk. Anatol. J. Fam. Med. 2021, 4, 159–164. [Google Scholar]
- Kaur, A.; Ani, A.; Sharma, A.; Kumari, V. Nomophobia and social interaction anxiety among university students. Int. J. Afr. Nurs. Sci. 2021, 15, 100352. [Google Scholar] [CrossRef]
- Santl, L.; Brajkovic, L.; Kopilaš, V. Relationship between Nomophobia, Various Emotional Difficulties, and Distress Factors among Students. Eur. J. Investig. Health Psychol. Educ. 2022, 12, 716–730. [Google Scholar] [CrossRef]
- Sui, A.; Sui, W.; Irwin, J. Exploring the prevalence of nomophobia in a Canadian university: An environmental scan. J. Am. Coll. Health 2022, 1–8. [Google Scholar] [CrossRef]
- Durak, H.Y. Investigation of nomophobia and smartphone addiction predictors among adolescents in Turkey: Demographic variables and academic performance. Soc. Sci. J. 2019, 56, 492–517. [Google Scholar] [CrossRef]
- Sharma, M.; Mathur, D.M.; Jeenger, J. Nomophobia and its relationship with depression, anxiety, and quality of life in adolescents. Ind. Psychiatry J. 2019, 28, 231. [Google Scholar]
- Bano, N.; Khan, M.A.; Asif, U.; de Beer, J.; Rawass, H. Effects of nomophobia on anxiety, stress and depression among Saudi medical students in Jeddah, Saudi Arabia. J. Pak. Med. Assoc. 2021, 71, 854–858. [Google Scholar]
- Çobanoğlu, A.; Bahadir-Yilmaz, E.; Kiziltan, B. The relationship between nursing students’ digital and smartphone addiction levels and nomophobia: A descriptive, correlational study. Perspect. Psychiatr. Care 2021, 57, 1727–1734. [Google Scholar] [CrossRef]
- Kurnia, E.A.; Satiadarma, M.P.; Wati, L. The Relationship Between Nomophobia and Poorer Sleep Among College Students. In Proceedings of the International Conference on Economics, Business, Social, and Humanities (ICEBSH 2021), Jakarta, Indonesia, 17–18 February 2021; Atlantis Press: Amsterdam, The Netherlands, 2021; pp. 1254–1261. [Google Scholar]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
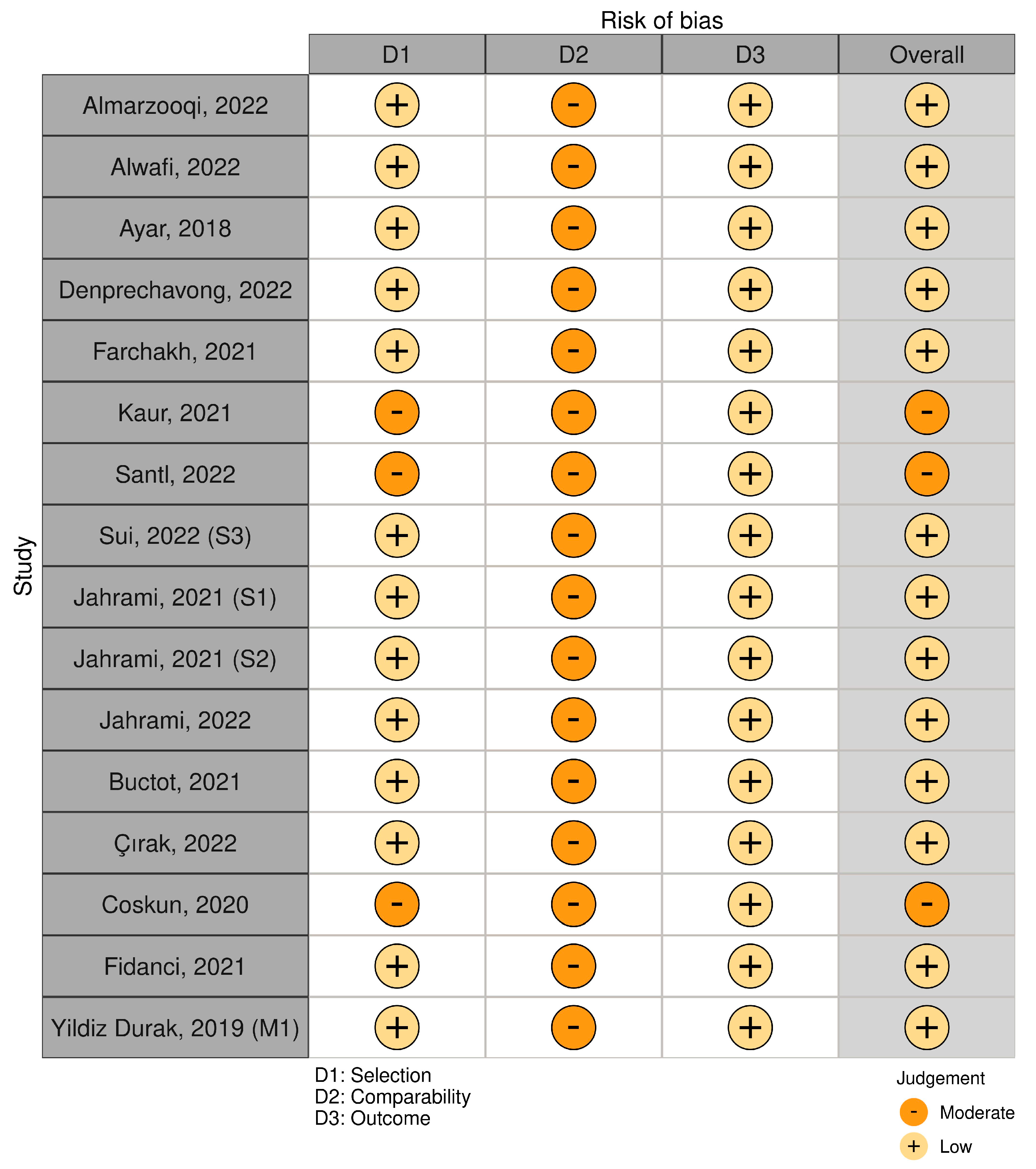
| SN | Ref. | Study | Country | Population Sample | Sample Size | Age (Years) | Insomnia | Smartphone Addiction | Anxiety | Insomnia’s Tool | Smartphone Addiction’s Tool | Anxiety’s Tool | Risk of Bias (NOS) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | [11] | Almarzooqi et al., 2022 | Saudi Arabia | General population | 893 | 24 | r = 0.253 p = 0.001 | r = 0.158 p = 0.001 | r = 0.281 p = 0.001 | ISI | IAS | GAD-7 | 8 (low) |
| 2 | [34] | Alwafi et al., 2022 | Saudi Arabia | General population | 5191 | 24 | NR | NR | r = 0.209 p = 0.001 | NR | NR | RD | 7 (low) |
| 3 | [1] | Ayar et al., 2018 | Turkey | University students | 755 | 21 | NR | NR | r = 0.320 p = 0.001 | NR | NR | SAAS | 8 (low) |
| 4 | [9] | Buctot et al., 2021 | Philippines | Adolescents | 3374 | 15 | NR | r = 0.116 p = 0.010 | NR | NR | SAS-SV | NR | 8 (low) |
| 5 | [5] | Çırak et al., 2022 | Turkey | University students | 451 | 20 | NR | r = 0.579 p = 0.010 | NR | NR | DAS | NR | 8 (low) |
| 6 | [35] | Coskun et al., 2020 | Turkey | General population | 210 | 33 | NR | r = NR p = 0.050 | NR | NR | Scale of Social Media Addiction—Adult Form | NR | 6 (moderate) |
| 7 | [36] | Denprechavong et al., 2022 | Thailand | University students | 638 | 20 | NR | NR | r = 0.342 p = 0.001 | NR | NR | HADS | 8 (low) |
| 8 | [4] | Farchakh et al., 2021 | Lebanon | General population | 2260 | 28 | r = 0.400 p = 0.001 | NR | r = 0.240 p = 0.001 | LIS-18 | NR | HAM-A | 8 (low) |
| 9 | [37] | Fidanci et al., 2021 | Turkey | University students | 386 | 22 | NR | r = −0.053 p = 0.296 | NR | NR | SAS-SV | NR | 8 (low) |
| 10 | [2] | Jahrami et al., 2021 (S1) | Bahrain | General population | 549 | 27 | r = 0.630 p = 0.001 | NR | NR | ISI | NR | NR | 8 (low) |
| 11 | [2] | Jahrami et al., 2021 (S2) | Bahrain | General population | 654 | 27 | r = 0.600 p = 0.001 | NR | NR | ISI | NR | NR | 8 (low) |
| 12 | [12] | Jahrami et al., 2022 | Bahrain | General population | 549 | 27 | r = 0.600 p = 0.001 | NR | NR | ISI | NR | NR | 8 (low) |
| 13 | [38] | Kaur et al., 2021 | Pakistan | University students | 209 | 21 | NR | NR | r = 0.221 p = 0.001 | NR | NR | SIAS | 6 (moderate) |
| 14 | [39] | Santl et al., 2022 | Croatia | Adolescents | 257 | 22 | NR | NR | r = 0.403 p = 0.010 | NR | NR | DASS | 6 (moderate) |
| 15 | [40] | Sui et al., 2022 (S3) | Canada | University students | 1221 | 23 | NR | NR | r = 0.422 p = 0.001 | NR | NR | STAI | 8 (low) |
| 16 | [41] | Yildiz Durak et al., 2019 (M1) | Turkey | Adolescents | 612 | 13 | NR | r = 0.819 p = 0.001 | NR | NR | SAS | NR | 7 (low) |
| Analysis | Descriptive | Random-Effects Meta-Analysis | Prediction Intervals | Visual Results | Heterogeneity | Publication Bias | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| K | N | Pooled Results [95%CI] | PI [95%CI] | Forest Plot | τ2 | τ | I2 | H | df | Q | p | Egger’s Test | Rank Test | |
| NSA | 8 | 11,424 | 0.31 [0.25; 0.38] | [0.14; 0.49] | Figure 4 | 0.01 | 0.08 | 88.92% | 9.02 | 7 | 72.93 | <0.001 | 0.46 | 0.28 |
| NSSA | 6 | 5926 | 0.39 [0.04; 0.75] | [−0.54; 1.33] | Figure 5 | 0.20 | 0.44 | 99.32% | 146.49 | 5 | 675.17 | <0.001 | 0.86 | 0.72 |
| NSI | 5 | 4905 | 0.56 [0.38; 0.75] | [0.11; 1.01] | Figure 6 | 0.04 | 0.21 | 97.41% | 38.58 | 4 | 141.37 | <0.001 | 0.20 | 0.21 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Daraj, L.R.; AlGhareeb, M.; Almutawa, Y.M.; Trabelsi, K.; Jahrami, H. Systematic Review and Meta-Analysis of the Correlation Coefficients between Nomophobia and Anxiety, Smartphone Addiction, and Insomnia Symptoms. Healthcare 2023, 11, 2066. https://doi.org/10.3390/healthcare11142066
Daraj LR, AlGhareeb M, Almutawa YM, Trabelsi K, Jahrami H. Systematic Review and Meta-Analysis of the Correlation Coefficients between Nomophobia and Anxiety, Smartphone Addiction, and Insomnia Symptoms. Healthcare. 2023; 11(14):2066. https://doi.org/10.3390/healthcare11142066
Chicago/Turabian StyleDaraj, Lateefa Rashed, Muneera AlGhareeb, Yaser Mansoor Almutawa, Khaled Trabelsi, and Haitham Jahrami. 2023. "Systematic Review and Meta-Analysis of the Correlation Coefficients between Nomophobia and Anxiety, Smartphone Addiction, and Insomnia Symptoms" Healthcare 11, no. 14: 2066. https://doi.org/10.3390/healthcare11142066
APA StyleDaraj, L. R., AlGhareeb, M., Almutawa, Y. M., Trabelsi, K., & Jahrami, H. (2023). Systematic Review and Meta-Analysis of the Correlation Coefficients between Nomophobia and Anxiety, Smartphone Addiction, and Insomnia Symptoms. Healthcare, 11(14), 2066. https://doi.org/10.3390/healthcare11142066