The Importance of the Kinematic Evaluation Methods of the Upper Limbs in Women with Breast Cancer Mastectomy: A Literature Review
Abstract
1. Introduction
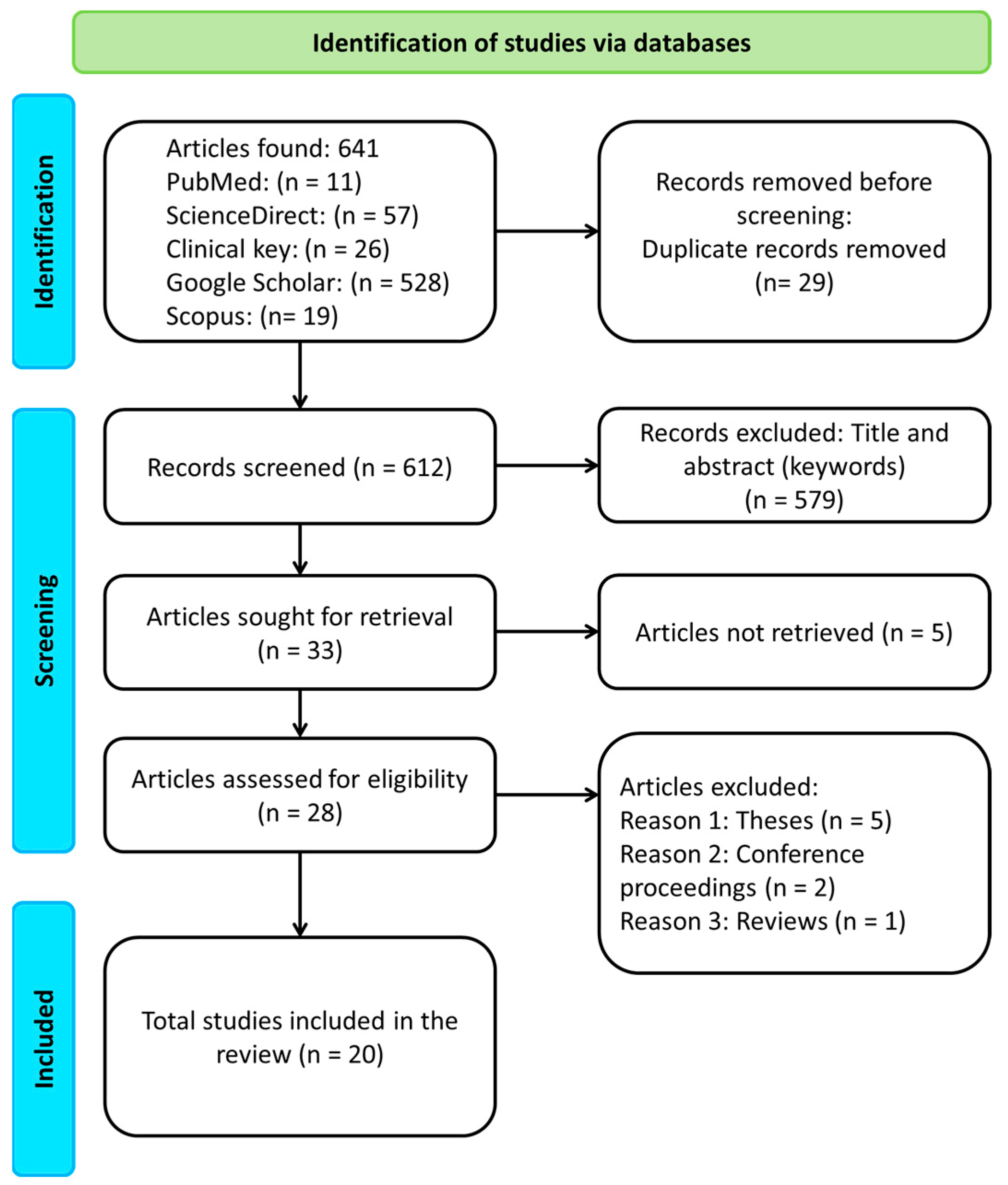
2. Materials and Methods
2.1. Inclusion Criteria
2.2. Search Strategies
2.3. Selection Criteria for Scientific Manuscripts
2.4. Data Collection and Extraction
3. Results
3.1. Methodologies for Motion Capture System (MoCS), and Study Designs to Measure Kinematic Movements of the Upper Extremity in BC Survivors
3.1.1. The Optoelectronic System (Vicon Motion System)
3.1.2. Electromagnetic System to Evaluate Kinematic Movements of the Upper Extremity in BC Survivors
3.1.3. Other Optoelectronic Systems to Measure the Kinematics Movements of the Upper Extremity in BC Survivors
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lang, A.E.; Dickerson, C.R.; Kim, S.Y.; Stobart, J.; Milosavljevic, S. Impingement pain affects kinematics of breast cancer survivors in work-related functional tasks. Clin. Biomech. 2019, 70, 223–230. [Google Scholar] [CrossRef] [PubMed]
- Crosbie, J.; Kilbreath, S.L.; Dylke, E.; Refshauge, K.M.; Nicholson, L.L.; Beith, J.M.; Spillane, A.J.; White, K. Effects of mastectomy on shoulder and spinal kinematics during bilateral upper-limb movement. Phys. Ther. 2010, 90, 679–692. [Google Scholar] [CrossRef] [PubMed]
- Borstad, J.D.; Szucs, K.A. Three-dimensional scapula kinematics and shoulder function examined before and after surgical treatment for breast cancer. Hum. Mov. Sci. 2012, 31, 408–418. [Google Scholar] [CrossRef]
- Brookham, R.L.; Cudlip, A.C.; Dickerson, C.R. Examining upper limb kinematics and dysfunction of breast cancer survivors in functional dynamic tasks. Clin. Biomech. 2018, 55, 86–93. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, I.L.; Camargo, P.R.; Alburquerque-Sendín, F.; Ferrari, A.V.; Arrais, C.L.; Salvini, T.F. Three-dimensional scapular kinematics, shoulder outcome measures and quality of life following treatment for breast cancer—A case control study. Musculoskelet. Sci. Pract. 2019, 40, 72–79. [Google Scholar] [CrossRef] [PubMed]
- Baran, E.; Yildiz, T.İ.; Gursen, C.; Üzelpasaci, E.; Özgül, S.; Düzgün, İ.; Akbayrak, T. The association of breast cancer-related lymphedema after unilateral mastectomy with shoulder girdle kinematics and upper extremity function. J. Biomech. 2021, 121, 110432. [Google Scholar] [CrossRef] [PubMed]
- Lang, A.E.; Card, A.; Barden, J.; Kim, S.Y. Effect of breast reconstruction on kinematics and performance during upper limb-focused functional tasks. Plast. Reconstr. Surg. 2022, 150, 747E–756E. [Google Scholar] [CrossRef]
- Lang, A.E.; Milosavljevic, S.; Dickerson, C.R.; Trask, C.M.; Kim, S.Y. Evidence of rotator cuff disease after breast cancer treatment: Scapular kinematics of post-mastectomy and post-reconstruction breast cancer survivors. Ann. Med. 2022, 54, 1058–1066. [Google Scholar] [CrossRef]
- García-González, S.B.; Huerta-Franco, M.R.; Miguel-Andrés, I.; de Jesús Mayagoitia-Vázquez, J.; León-Rodríguez, M.; Barrera-Beltrán, K.; Espinoza-Macías, G. Differences in the glenohumeral joint before and after unilateral breast cancer surgery: Motion capture analysis. Healthcare 2022, 10, 707. [Google Scholar] [CrossRef]
- Miguel-Andrés, I.; García-González, S.B.; Mayagoitia-Vázquez, J.d.J.; Barrera-Beltrán, K.; Samayoa-Ochoa, D.; León-Rodríguez, M.; García-García, L.A. Effect of the unilateral breast cancer surgery on the shoulder movement: Electromyographic and motion. Mex. J. Biomed. Eng. 2022, 43, 40–51. [Google Scholar] [CrossRef]
- Shamley, D.; Srinaganathan, R.; Oskrochi, R.; Lascurain-Aguirrebeña, I.; Sugden, E. Three-dimensional scapulothoracic motion following treatment for breast cancer. Breast Cancer Res. Treat. 2009, 118, 315–322. [Google Scholar] [CrossRef] [PubMed]
- Lang, A.E.; Milosavljevic, S.; Dickerson, C.R.; Kim, S.Y. Examining assessment methods of scapular motion: Comparing results from planar elevations and functional task performance. Clin. Biomech. 2020, 80, 105203. [Google Scholar] [CrossRef] [PubMed]
- Wu, G.; van der Helm, F.C.T.; Veeger, H.E.J.D.; Makhsous, M.; Van Roy, P.; Anglin, C.; Nagels, J.; Karduna, A.R.; McQuade, K.; Wang, X.; et al. ISB recommendation on definitions of joint coordinate systems of various joints for the reporting of human joint motion—Part II: Shoulder, elbow, wrist and hand. J. Biomech. 2005, 38, 981–992. [Google Scholar] [CrossRef] [PubMed]
- Cunha, N.d.S.; Sinhorim, L.; Schleip, R.; Zomkowski, K.; Santos, G.M.; Sperandio, F.F. Effects of myofascial reorganization associated with kinesiotherapy on chronic pain and functionality of breast cancer survivors: Development of a study protocol. Fisioter. Mov. 2022, 35, e35609. [Google Scholar] [CrossRef]
- Rett, M.T.; Moura, D.P.; de Oliveira, F.B.; Domingos, H.Y.B.; de Oliveira, M.M.F.; Gallo, R.B.S.; da Silva Junior, W.M. Physical therapy after breast cancer surgery improves range of motion and pain over time. Fisioter. Pesqui. 2022, 29, 46–52. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Lang, A.E.; Kim, S.Y.; Milosavljevic, S.; Dickerson, C.R. The utility of the acromion marker cluster (AMC) in a clinical population. J. Electromyogr. Kinesiol. 2022, 62, 102298. [Google Scholar] [CrossRef]
- Balzarini, A.; Lualdi, P.; Lucarini, C.; Ferla, S.; Galli, M.; Crivellini, M.; DeConno, F. Biochemical evaluation of scapular girdle in patients with chronic arm lymphedema. Lymphology 2006, 39, 132–140. [Google Scholar]
- Rundquist, P.J.; Behrens, B.A.; Happel, A.S.; Kennedy, K.; Biggers, L. Shoulder kinematics and function in breast cancer survivors with unilateral lymphedema: An observational study. Rehabil. Oncol. 2015, 33, 41–46. [Google Scholar] [CrossRef]
- Corrado, B.; Ciardi, G.; Iammarrone, C.S.; Arpino, G. Home exercise program is an effective tool in improving upper limb function and quality of life in breast cancer survivors: A retrospective observational study. J. Hum. Sport. Exerc. 2018, 13, 926–939. [Google Scholar] [CrossRef]
- Braudy, R.; Atoms, B.; Coghlan, J.; Staples, M.; Moga, D.; Tollefsrud, R.; Lawrence, R.L.; Ludewig, P.; Koehler, L. Shoulder kinematics of axillary web syndrome in women treated for breast cancer. Arch. Phys. Med. Rehabil. 2022, 104, 403–409. [Google Scholar] [CrossRef] [PubMed]
- Maciukiewicz, J.M.; Hussein, A.T.S.; Mourtzakis, M.; Dickerson, C.R. An evaluation of upper limb strength and range of motion of breast cancer survivors immediately following treatment. Clin. Biomech. 2022, 96, 105666. [Google Scholar] [CrossRef] [PubMed]
- Lopot, F.; Rawnik, D.; Koudelkova, K.; Kubovy, P.; Stastny, P. The influence of woman’s mastectomy on breathing kinematics. In Proceedings of the International Conference of the Polish Society of Biomechanics, Zielona Góra, Poland, 5–7 September 2018; Springer: Berlin/Heidelberg, Germany, 2019; Volume 831, pp. 36–44. [Google Scholar] [CrossRef]
- Shamley, D.; Lascurain-Aguirrebeña, I.; Oskrochi, R. Clinical anatomy of the shoulder after treatment for breast cancer. Clin. Anat. 2014, 27, 467–477. [Google Scholar] [CrossRef]
- Shamley, D.; Lascurain-Aguirrebeña, I.; Oskrochi, R.; Srinaganathan, R. Shoulder morbidity after treatment for breast cancer is bilateral and greater after mastectomy. Acta Oncol. (Madr.) 2012, 51, 1045–1053. [Google Scholar] [CrossRef]
- Spinelli, B.A.; Silfies, S.; Jacobs, L.A.; Brooks, A.D.; Ebaugh, D. Scapulothoracic and glenohumeral motions during functional reaching tasks in women with a history of breast cancer and healthy age-matched controls. Rehabil. Oncol. 2016, 34, 127–136. [Google Scholar] [CrossRef]
| Study design | Clinical studies, and observational trials (cross-sectional or longitudinal) |
| Target population | Women with mastectomy for breast cancer |
| Treatment | Mastectomy |
| Variables analyzed | Kinematics of the glenohumeral joint, scapula, or shoulder girdle |
| Comparison | Control group (healthy women, contralateral side). Pre and post-test measurement |
| Database | Search Equation | Search Date | Outcomes | Selected |
|---|---|---|---|---|
| PubMed | “kinematics” AND “breast cancer” AND “mastectomy” | 4 March 2023 | 11 | 9 |
| ScienceDirect | “kinematics” AND “breast cancer” AND “mastectomy” | 2 March 2023 | 57 | 8 |
| Clinical Key | “kinematics” AND “breast cancer” AND “mastectomy” | 3 March 2023 | 26 | 8 |
| Google Scholar | “kinematics” AND “breast cancer” AND “mastectomy” | 17 February 2023 | 528 | 27 |
| Scopus | “kinematics” AND “breast cancer” AND “mastectomy” | 5 March 2023 | 19 | 15 |
| Total | 641 | 67 |
| Articles | Objective | MoCS and Kinematics (Movements) | Reference System | Time (Days or Months) | Age and Sample Size | Surgery | Region of the Body | Comparison |
|---|---|---|---|---|---|---|---|---|
| Lang et al., 2022 [8] | Scapular kinematics and impingement pain during an overhead reach task | Vicon motion System (optoelectronic system) Functional movement (overhead reaching task) | Recommendations of the International Society of Biomechanics (ISB) (torso cluster) | >6 months after surgery | 35–65 years old n = 95 | Mastectomy and reconstruction post-mastectomy | Scapula (internal/external rotation, upward/downward rotation and anterior/posterior tilt) | Control healthy group; Mastectomy group; Reconstruction group |
| Crosbie et al., 2010 [2] | Shoulder girdle kinematics and control group | Motion star wireless (electromagnetic system) Forward flexion, abduction, movement in the scapular plane | Local coordinate system, 6-degree-of-freedom | >12 months after surgery | 44–88 years old n = 75 | Mastectomy | Scapulothoracic (upward/downward rotation, internal/external rotation, anterior/posterior tilt). Trunk (flexion, extension, lateral flexion, axial rotation of thoracic and lumbar region) | Control healthy group; Mastectomy dominant side; Mastectomy nondominant side |
| Shamley et al., 2012 [26] | Impact of a mastectomy vs. a wide local excision | 3 Space Fastrak (electromagnetic system) Elevation and depression arm in the scapular plane | ISB standard (thorax, scapula, humerus) | 1143.81 (534.77) days after surgery | 61.6 (9.1) years old n = 176 | Mastectomy and wide local excision | Scapula (internal/external rotation, upward/downward rotation and anterior/posterior tilt) | Mastectomy group; Wide local excision group (Both left and right affected sides) |
| García-González et al., 2022 [9] | Shoulder kinematics before and after mastectomy | Vicon Nexus System (optoelectronic system) Flexion-extension and abduction-adduction movement | Three orthogonal coordinate axes systems (torso, left and right arms) | <15 days before surgery 60 days after surgery | 46.7 (8.2) years old n = 15 | Mastectomy and axillary lymph node dissection | Glenohumeral joint (flexion/extension and abduction/adduction) | Mastectomy group before and after surgery |
| Corrado et al., 2018 [21] | Effects of home exercise program on upper limb function | SMART-DX (optoelectronic system) Functional task (hand-to-mouth, reaching-arm, hand-to-head) ROM task (shoulder flexion/extension, abduction/adduction, elbow flexión/extension) | International shoulder groups (ISB) protocol | 1 and 3 months after surgery | 55.8 mean age n = 30 | Modified radical mastectomy and axillary lymph node dissection | Shoulder and elbow (movement duration and angular velocity) | Patients without home exercise program; Patients with home exercise program |
| Shamley et al., 2009 [11] | Scapulothoracic kinematics between affected and unaffected side | The Polhemus Fastrak (electromagnetic system) Humeral elevation and depression in the scapular plane | ISB protocol (orientation of the scapula relative to the trunk) | 1144 (537) mean days after surgery | 61.8 (8.9) mean years n = 152 | Mastectomy and wide local excision | Scapula (protaction/retraction, lateral/medial rotation, anterior/posterior tilt) | Affected side left and right; Unaffected side left and right |
| Balzarini et al., 2006 [19] | Alterations in postural strategies due to increased weight and volume of the arm due to lymphedema | ELITE 2002 (optoelectronic system) Shoulder retroposition and abduction movements | Global coordinate system, trajectories (X, Y, Z) of the markers | The evaluation time after the mastectomy is not clear. | 58.9 mean age n = 17 | Quadrantectomy and modified radical mastectomy | ROM of the shoulder girdle and the affected arm. | Unaffected side in the mastectomy group |
| Baran et al., 2021 [6] | Breast cancer-related lymphedema on shoulder girdle kinematics | Flock of birds (Electromagnetic system) Elevation in the scapular plane | Recommendations of the International Society of Biomechanics (ISB) | 32.5 (26.8) mean months since surgery | 50.9 (7.3) mean age n = 67 | Modified radical or radical mastectomy and axillary lymph node dissection | Scapula (internal-external rotation, upward-downward rotation and anterior-posterior tilt) | Non lymphedema group; Moderate lymphedema group; Severe lymphedema group |
| Braudy et al., 2022 [22] | Kinematics between women with and without axillary web syndrome | Polhemus 3Space FASTRAK (electromagnetic system) Arm forward flexion, scapular plane abduction, coronal plane abduction | ISB recommendations | >5 years after surgery | 54 (10) Mean age at surgery n = 25 | Lumpectomy, mastectomy, and axillary surgery | Scapulothoracic (internal and upward rotation and posterior tilt) Humerothoracic (elevation, elevation plane, and axial rotation) | Axillary web syndrome; Non-axillary web syndrome |
| Lang et al., 2020 [12] | Scapular upward rotation and scapulohumeral rhythm during arm elevation | Vicon Motion System (Optoelectronic system) Three elevations in frontal, scapular, and sagittal plane. Functional task (overhead reach, overhead lift, and fingertip dexterity) | Recommendations of the International Society of Biomechanics (ISB) | 50.9 (45.7) mean months since surgery | 53.1 (5.5) mean age n = 50 | Mastectomy and lymph node removal | Scapula (upward rotation) and Scapulohumeral rhythm | Non-cancer controls group; Breast cancer survivors group (pain and no pain) |
| Lang et al., 2019 [1] | Torso and shoulder kinematics during common task | Vicon Motion System (Optoelectronic system) Work-related functional task (overhead reach, repetitive reach, fingertip dexterity, hand and forearm dexterity, waist to overhead lift, overhead work) | Recommendations of the International Society of Biomechanics (ISB) | 42.5 (41.6) months since surgery | 52.8 (5.4) mean age n = 50 | Mastectomy and lymph node removal | Torso (flexion/extension, lateral flexion/extension, axial rotation) Thoracohumeral (abduction/adduction, flexion/extension, internal/external rotation) Scapula (protraction/retraction, upward/downward rotation, anterior/posterior tilt) | Breast cancer survivors (with and without impingement pain) group; Control group |
| Lang et al., 2022 [18] | Accuracy of the AMC (acromion marker cluster) for scapula motion tracking | Vicon Motion System (Optoelectronic system) Humeral elevation in frontal plane | Recommendations of the International Society of Biomechanics (ISB) | 56.8 (4.7) months since mastectomy | 54.1 (5.2) mean age n = 50 | Mastectomy | Scapula (protraction, rotation, and tilt) | Breast cancer survivors group; Control group |
| Brookham et al., 2018 [4] | Humerothoracic, scapulothoracic kinematics in functional dynamic task | Vicon Motion System (Optoelectronic system) Task of shoulder ROM, ADL task (personal body care activities), and work task (reaching task with and without loads) | Recommendations of the International Society of Biomechanics (ISB) | >3 months after completing treatment | 59.4 (9.7) mean age n = 50 | Mastectomy, lumpectomy, axillar node dissection | Scapulothoracic (upward/downward rotation, anterior/posterior tilt, retraction/protraction) Humerothoracic angle (elevation angle; plane of elevation: flexion, abduction; external/internal rotation) | Affected side group; Unaffected side group |
| Maciukiewicz et al., 2022 [23] | Range of motion and strength follow breast cancer treatment | Vicon Motion System (Optoelectronic system) Arm flexion, extension, abduction, adduction, scapular abduction, and internal–external rotation | Recommendations of the International Society of Biomechanics | >1 year after surgery | 53.9 (10.3) mean age n = 29 | Any form of surgical procedure for breast tumor removal | Humerothoracic joint range of motion (flexion, extension, scapular abduction, abduction, internal and external rotation) | One year of treatment ending group; Between one and two years after treatment ended group |
| Ribeiro et al., 2019 [5] | Scapular kinematics during elevation of the arm | Flock of birds (Electromagnetic system) Elevation of the arm in the scapular plane | Recommendations of the International Society of Biomechanics | 24.2 (20.5) median months since surgery | 50.2 (9.8) mean age n = 42 | Conserving surgery or mastectomy | Scapula (internal/external rotation, upward rotation, anterior/posterior tilt) | Control group; Surgery group |
| Lang et al., 2022 [7] | Breast reconstruction on kinematics during functional task | Vicon Motion System (Optoelectronic system) Maximum arm abduction and extension. Additionally, functional task (right and left repetitive reach, right and left fingertip dexterity, overhead lift, and overhead work) | Recommendations of the International Society of Biomechanics (ISB) | 56.8 (42.1) mean months after surgery | 54.0 (5.1) mean age n = 95 | Mastectomy, reconstruction post-mastectomy, and lymph node removal | Shoulder range of motion (abduction and extension). Thoracohumeral (abduction, horizontal flexion, axial rotation). Additionally, scapular (protraction/retraction, upward/downward rotation, anterior/posterior tilt) | Control group; Mastectomy-only group; Mastectomy with reconstruction |
| Lopot et al., 2019 [24] | Extent of breathing movements of the thoracic and abdominal wall | Qualisys (Optoelectronic kinematic analyzer) Mild and deep breath | Global coordinate system, trajectories (X, Y, Z) | >5 years after surgery | 64.5 average age n = 12 | Total breast mastectomy | Thoracic and abdominal wall | Control health group; Mastectomy group |
| Spinelli et al., 2016 [27] | Range of motion during functional task | Liberty Polhemus (electromagnetic system) Functional task (unweighted and weighted overhead reaching, and simulated hair combing) | Recommendations of the International Society of Biomechanics | 29.4 (10.8) mean months since surgery | 53.8 (10.9) mean age n = 60 | Lumpectomy, mastectomy, and lymph node surgery | Scapulothoracic range of motion (elevation, internal/external rotation, clavicular elevation/retraction, upward rotation, posterior til) Glenohumeral range of motion (adduction, external rotation) | Control group; Breast cancer treatment group |
| Rundquist et al., 2015 [20] | Lymphedema and decreased range of motion | The Motion Monitor 3D (electromagnetic system) Shoulder flexion, abduction, external and internal rotation | Local coordinate system. | 72.3 (64.3) mean months from surgery | 57.8 (10.1) mean age n = 30 | Mastectomy | Shoulder range of motion (flexion, abduction, external and internal rotation) | Involved upper extremity; Uninvolved upper extremity |
| Shamley et al., 2014 [25] | Muscle activity and movement deviations | The 3 Space Fastrak (electromagnetic system) Arm elevation and depression in the scapular plane | International Shoulder Group (ISG) protocol | 1143.8 (534.7) mean days after surgery | 61.6 (9.1) mean age n = 176 | Mastectomy and wide local excision | Scapula (internal/external rotation, upward/downward rotation, anterior/posterior tilt) | Affected side left and right; Unaffected side left and right |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Miguel-Andrés, I.; Huerta-Franco, M.R.; García-González, S.B.; León-Rodríguez, M.; Barrera-Beltrán, K.; Ortiz-Lango, L.A. The Importance of the Kinematic Evaluation Methods of the Upper Limbs in Women with Breast Cancer Mastectomy: A Literature Review. Healthcare 2023, 11, 2064. https://doi.org/10.3390/healthcare11142064
Miguel-Andrés I, Huerta-Franco MR, García-González SB, León-Rodríguez M, Barrera-Beltrán K, Ortiz-Lango LA. The Importance of the Kinematic Evaluation Methods of the Upper Limbs in Women with Breast Cancer Mastectomy: A Literature Review. Healthcare. 2023; 11(14):2064. https://doi.org/10.3390/healthcare11142064
Chicago/Turabian StyleMiguel-Andrés, Israel, María Raquel Huerta-Franco, Silvia Beatríz García-González, Miguel León-Rodríguez, Karla Barrera-Beltrán, and Luis Angel Ortiz-Lango. 2023. "The Importance of the Kinematic Evaluation Methods of the Upper Limbs in Women with Breast Cancer Mastectomy: A Literature Review" Healthcare 11, no. 14: 2064. https://doi.org/10.3390/healthcare11142064
APA StyleMiguel-Andrés, I., Huerta-Franco, M. R., García-González, S. B., León-Rodríguez, M., Barrera-Beltrán, K., & Ortiz-Lango, L. A. (2023). The Importance of the Kinematic Evaluation Methods of the Upper Limbs in Women with Breast Cancer Mastectomy: A Literature Review. Healthcare, 11(14), 2064. https://doi.org/10.3390/healthcare11142064










