Unmet Supportive Care Needs after Non-Small Cell Lung Cancer Resection at a Tertiary Hospital in Seoul, South Korea
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design, Setting, and Population
2.2. Data Collection
2.3. Measurement of Unmet Need
2.4. Other Measures
2.5. Statistical Analysis
3. Results
3.1. General Characteristics of Study Participants
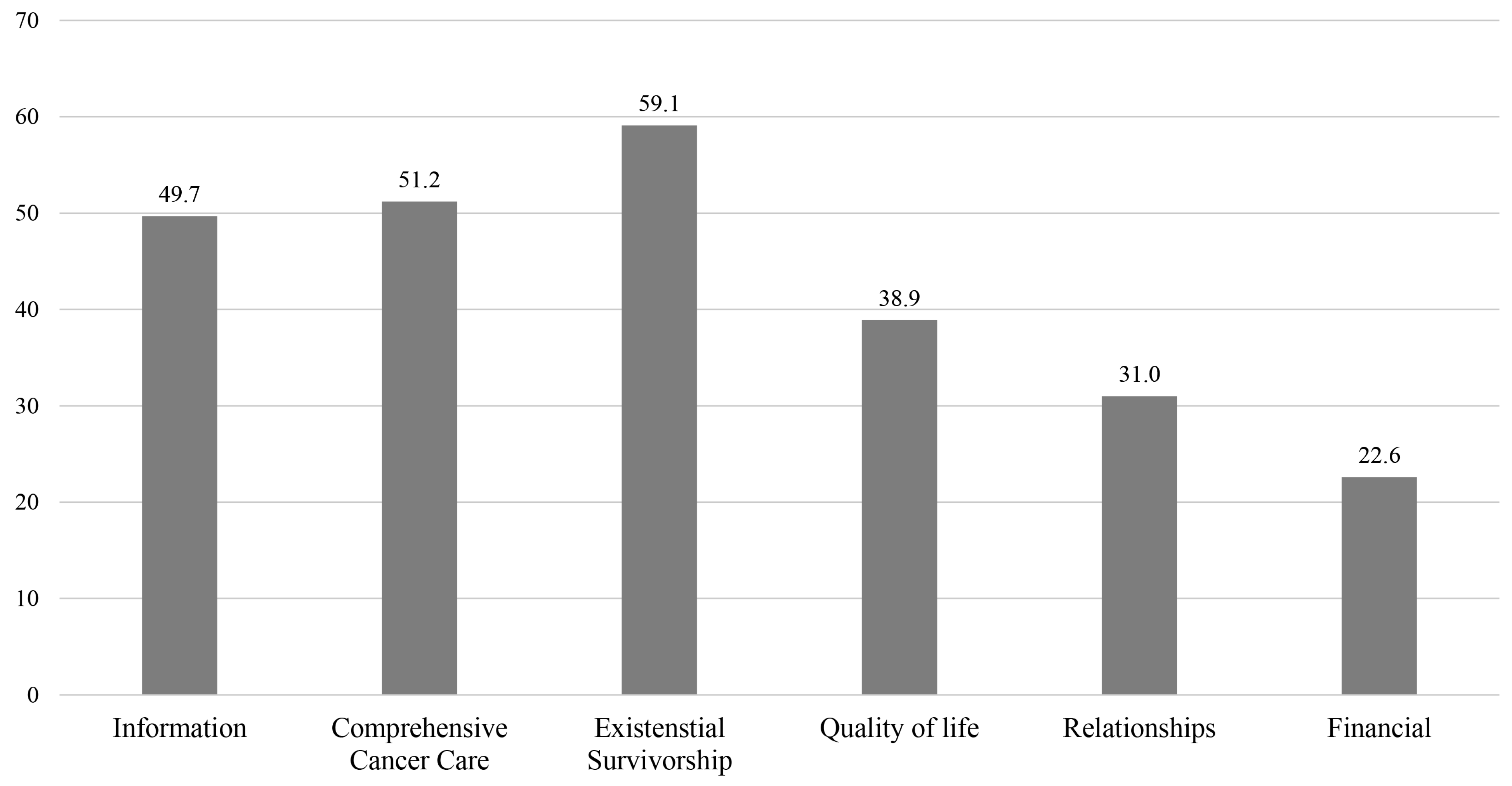
3.2. Prevalence of Unmet Needs
4. Discussion
4.1. Correlates of Unmet Needs
4.2. Clinical Implications
4.3. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Usman Ali, M.; Miller, J.; Peirson, L.; Fitzpatrick-Lewis, D.; Kenny, M.; Sherifali, D.; Raina, P. Screening for lung cancer: A systematic review and meta-analysis. Prev. Med. 2016, 89, 301–314. [Google Scholar] [CrossRef] [PubMed]
- de Koning, H.J.; van der Aalst, C.M.; de Jong, P.A.; Scholten, E.T.; Nackaerts, K.; Heuvelmans, M.A.; Lammers, J.J.; Weenink, C.; Yousaf-Khan, U.; Horeweg, N.; et al. Reduced Lung-Cancer Mortality with Volume CT Screening in a Randomized Trial. N. Engl. J. Med. 2020, 382, 503–513. [Google Scholar] [CrossRef] [PubMed]
- Wao, H.; Mhaskar, R.; Kumar, A.; Miladinovic, B.; Djulbegovic, B. Survival of patients with non-small cell lung cancer without treatment: A systematic review and meta-analysis. Syst. Rev. 2013, 2, 10. [Google Scholar] [CrossRef] [PubMed]
- Vijayvergia, N.; Shah, P.C.; Denlinger, C.S. Survivorship in Non-Small Cell Lung Cancer: Challenges Faced and Steps Forward. J. Natl. Compr. Cancer Netw. 2015, 13, 1151–1161. [Google Scholar] [CrossRef]
- Stein, K.D.; Syrjala, K.L.; Andrykowski, M.A. Physical and psychological long-term and late effects of cancer. Cancer 2008, 112, 2577–2592. [Google Scholar] [CrossRef]
- Jarrett, N.; Scott, I.; Addington-Hall, J.; Amir, Z.; Brearley, S.; Hodges, L.; Richardson, A.; Sharpe, M.; Stamataki, Z.; Stark, D.; et al. Informing future research priorities into the psychological and social problems faced by cancer survivors: A rapid review and synthesis of the literature. Eur. J. Oncol. Nurs. 2013, 17, 510–520. [Google Scholar] [CrossRef]
- Maguire, R.; Papadopoulou, C.; Kotronoulas, G.; Simpson, M.F.; McPhelim, J.; Irvine, L. A systematic review of supportive care needs of people living with lung cancer. Eur. J. Oncol. Nurs. 2013, 17, 449–464. [Google Scholar] [CrossRef]
- Moghaddam, N.; Coxon, H.; Nabarro, S.; Hardy, B.; Cox, K. Unmet care needs in people living with advanced cancer: A systematic review. Support. Care Cancer 2016, 24, 3609–3622. [Google Scholar] [CrossRef]
- Molassiotis, A.; Uyterlinde, W.; Hollen, P.J.; Sarna, L.; Palmer, P.; Krishnasamy, M. Supportive care in lung cancer: Milestones over the past 40 years. J. Thorac. Oncol. 2015, 10, 10–18. [Google Scholar] [CrossRef]
- Li, J.; Girgis, A. Supportive care needs: Are patients with lung cancer a neglected population? Psycho-Oncology 2006, 15, 509–516. [Google Scholar] [CrossRef]
- Giuliani, M.E.; Milne, R.A.; Puts, M.; Sampson, L.R.; Kwan, J.Y.; Le, L.W.; Alibhai, S.M.; Howell, D.; Abdelmutti, N.; Liu, G.; et al. The prevalence and nature of supportive care needs in lung cancer patients. Curr. Oncol. 2016, 23, 258–265. [Google Scholar] [CrossRef]
- Cochrane, A.; Woods, S.; Dunne, S.; Gallagher, P. Unmet supportive care needs associated with quality of life for people with lung cancer: A systematic review of the evidence 2007–2020. Eur. J. Cancer Care 2022, 31, e13525. [Google Scholar] [CrossRef]
- Molassiotis, A.; Yates, P.; Li, Q.; So, W.K.W.; Pongthavornkamol, K.; Pittayapan, P.; Komatsu, H.; Thandar, M.; Yi, M.; Titus Chacko, S.; et al. Mapping unmet supportive care needs, quality-of-life perceptions and current symptoms in cancer survivors across the Asia-Pacific region: Results from the International STEP Study. Ann. Oncol. 2017, 28, 2552–2558. [Google Scholar] [CrossRef]
- Yun, Y.H.; Shon, E.J.; Yang, A.J.; Kim, S.H.; Kim, Y.A.; Chang, Y.J.; Lee, J.; Kim, M.S.; Lee, H.S.; Zo, J.I.; et al. Needs regarding care and factors associated with unmet needs in disease-free survivors of surgically treated lung cancer. Ann. Oncol. 2013, 24, 1552–1559. [Google Scholar] [CrossRef]
- Hodgkinson, K.; Butow, P.; Hunt, G.E.; Pendlebury, S.; Hobbs, K.M.; Lo, S.K.; Wain, G. The development and evaluation of a measure to assess cancer survivors’ unmet supportive care needs: The CaSUN (Cancer Survivors’ Unmet Needs measure). Psycho-Oncology 2007, 16, 796–804. [Google Scholar] [CrossRef]
- Li, Q.; Lin, Y.; Zhou, H.; Xu, Y.; Xu, Y. Supportive care needs and associated factors among Chinese cancer survivors: A cross-sectional study. Support. Care Cancer 2019, 27, 287–295. [Google Scholar] [CrossRef]
- Mazariego, C.G.; Juraskova, I.; Campbell, R.; Smith, D.P. Long-term unmet supportive care needs of prostate cancer survivors: 15-year follow-up from the NSW Prostate Cancer Care and Outcomes Study. Support. Care Cancer 2020, 28, 5511–5520. [Google Scholar] [CrossRef]
- Miroševič, Š.; Prins, J.; Borštnar, S.; Besić, N.; Homar, V.; Selič-Zupančič, P.; Smrdel, A.; Klemenc-Ketiš, Z. Factors associated with a high level of unmet needs and their prevalence in the breast cancer survivors 1–5 years after post local treatment and (neo)adjuvant chemotherapy during the COVID-19: A cross-sectional study. Front. Psychol. 2022, 13, 969918. [Google Scholar] [CrossRef]
- Kang, D.; Lee, G.; Kim, S.; Nam, H.; Kong, S.; Shim, S.; Lee, J.K.; Jung, W.; Shin, S.; Kim, H.K.; et al. Psychometric Validation of the Korean Version of the Cancer Survivors’ Unmet Needs (CaSUN) Scale Among Korean Non-Small Cell Lung Cancer (NSCLC) Survivors. Cancer Res. Treat. 2022, 55, 61–72. [Google Scholar] [CrossRef]
- Shin, J.; Goo, A.; Ko, H.; Kim, J.-H.; Lim, S.-U.; Lee, H.-K.; Simard, S.; Song, Y.-M. Validation Study for the Korean Version of Fear of Cancer Recurrence Inventory. J. Korean Med. Sci. 2017, 32, 1792–1799. [Google Scholar] [CrossRef] [PubMed]
- Jung, W.; Park, J.; Jeong, A.; Cho, J.H.; Jeon, Y.J.; Shin, D.W. Fear of cancer recurrence and its predictors among patients with non-small cell lung cancer (NSCLC). J. Cancer Surviv. 2023. [Google Scholar] [CrossRef] [PubMed]
- Simard, S.; Savard, J. Screening and comorbidity of clinical levels of fear of cancer recurrence. J. Cancer Surviv. 2015, 9, 481–491. [Google Scholar] [CrossRef] [PubMed]
- Yun, Y.H.; Park, Y.S.; Lee, E.S.; Bang, S.M.; Heo, D.S.; Park, S.Y.; You, C.H.; West, K. Validation of the Korean version of the EORTC QLQ-C30. Qual. Life Res. 2004, 13, 863–868. [Google Scholar] [CrossRef]
- Ahn, S.H.; Park, B.W.; Noh, D.Y.; Nam, S.J.; Lee, E.S.; Lee, M.K.; Kim, S.H.; Lee, K.M.; Park, S.M.; Yun, Y.H. Health-related quality of life in disease-free survivors of breast cancer with the general population. Ann. Oncol. 2007, 18, 173–182. [Google Scholar] [CrossRef]
- Fayers, P.M. Interpreting quality of life data: Population-based reference data for the EORTC QLQ-C30. Eur. J. Cancer 2001, 37, 1331–1334. [Google Scholar] [CrossRef]
- Clinical Oncology Network for Unifying Electronic Medical Data. Available online: https://bigdata-cancer.kr/ncc/lungInfo.do (accessed on 1 July 2023).
- Chen, S.C.; Chiou, S.C.; Yu, C.J.; Lee, Y.H.; Liao, W.Y.; Hsieh, P.Y.; Jhang, S.Y.; Lai, Y.H. The unmet supportive care needs-what advanced lung cancer patients’ caregivers need and related factors. Support. Care Cancer 2016, 24, 2999–3009. [Google Scholar] [CrossRef]
- Herschbach, P.; Dinkel, A. Fear of progression. Recent Results Cancer Res. 2014, 197, 11–29. [Google Scholar]
- Simard, S.; Thewes, B.; Humphris, G.; Dixon, M.; Hayden, C.; Mireskandari, S.; Ozakinci, G. Fear of cancer recurrence in adult cancer survivors: A systematic review of quantitative studies. J. Cancer Surviv. 2013, 7, 300–322. [Google Scholar] [CrossRef]
- Liao, Y.C.; Liao, W.Y.; Shun, S.C.; Yu, C.J.; Yang, P.C.; Lai, Y.H. Symptoms, psychological distress, and supportive care needs in lung cancer patients. Support. Care Cancer 2011, 19, 1743–1751. [Google Scholar] [CrossRef]
- Afiyanti, Y.; Besral, B.; Haryani, H.; Milanti, A.; Nasution, L.A.; Wahidi, K.R.; Gayatri, D. The relationships of unmet needs with quality of life and characteristics of Indonesian gynecologic cancer survivors. Can. Oncol. Nurs. J. 2021, 31, 298–305. [Google Scholar] [CrossRef]
- Rha, S.Y.; Lee, H.J.; Lee, J. Unmet needs in the physical and daily living domain mediates the influence of symptom experience on the quality of life of gastric cancer patients. Support. Care Cancer 2020, 28, 1419–1431. [Google Scholar] [CrossRef]
- Willems, R.A.; Bolman, C.A.; Mesters, I.; Kanera, I.M.; Beaulen, A.A.; Lechner, L. Cancer survivors in the first year after treatment: The prevalence and correlates of unmet needs in different domains. Psycho-Oncology 2016, 25, 51–57. [Google Scholar] [CrossRef]
- Smith, A.B.; Butow, P.; Olver, I.; Luckett, T.; Grimison, P.; Toner, G.C.; Stockler, M.R.; Hovey, E.; Stubbs, J.; Turner, S.; et al. The prevalence, severity, and correlates of psychological distress and impaired health-related quality of life following treatment for testicular cancer: A survivorship study. J. Cancer Surviv. 2016, 10, 223–233. [Google Scholar] [CrossRef]
- Amiri, P.; Mohammadi, A.; Bahaadinbeigy, K.; Kalantari Khandani, B.; Maazed, V. Identifying unmet information needs of advanced cancer patients in Iran: An in-depth qualitative study. Health Sci. Rep. 2022, 5, e914. [Google Scholar] [CrossRef]
- Kim, H.W.; Kim, Y.H.; Kang, S.Y.; Lee, E.J.; Lee, J.L.; Kim, Y. Gender Differences in Sexual Information Needs and Relating Factors in Cancer Patients: A Cross-Sectional Survey. Int. J. Environ. Res. Public Health 2021, 18, 3752. [Google Scholar] [CrossRef]
- Park, B.W.; Hwang, S.Y. Unmet needs of breast cancer patients relative to survival duration. Yonsei Med. J. 2012, 53, 118–125. [Google Scholar] [CrossRef]
- Nicklasson, M.; Bergman, B. Validity, reliability and clinical relevance of EORTC QLQ-C30 and LC13 in patients with chest malignancies in a palliative setting. Qual. Life Res. 2007, 16, 1019–1028. [Google Scholar] [CrossRef]
- Holm, L.V.; Hansen, D.G.; Johansen, C.; Vedsted, P.; Larsen, P.V.; Kragstrup, J.; Søndergaard, J. Participation in cancer rehabilitation and unmet needs: A population-based cohort study. Support. Care Cancer 2012, 20, 2913–2924. [Google Scholar] [CrossRef]
- Kim, J.Y.; Chun, M.; Kim, S.W.; Song, J. Identification of Korean cancer survivors’ unmet needs and desired psychosocial assistance: A focus group study. PLoS ONE 2020, 15, e0228054. [Google Scholar] [CrossRef]
| Characteristics | Total Study Population (n = 949) |
|---|---|
| Number (%) | |
| Sociodemographic characteristics | |
| Mean age, years * | 63.4 ± 8.8 |
| <65 | 510 (53.7) |
| ≥65 | 439 (46.3) |
| Sex | |
| Male | 529 (55.7) |
| Female | 420 (44.3) |
| Smoking status | |
| Never smoker | 464 (48.9) |
| Ex- or current smoker | 485 (51.1) |
| Education level | |
| ≥University | 353 (37.2) |
| High school | 328 (34.6) |
| ≤Middle school | 267 (28.1) |
| Unknown | 1 (0.1) |
| Marital status | |
| Married | 820 (86.4) |
| Working status | |
| Unemployed | 551 (58.1) |
| Employed | 398 (41.9) |
| Household monthly income | |
| <USD$3000 | 335 (35.3) |
| ≥USD$3000 | 536 (56.5) |
| Unknown | 78 (8.2) |
| Disease-related characteristics | |
| Comorbidity | |
| No | 239 (25.2) |
| Yes | 710 (74.8) |
| Pathologic stage | |
| 0 | 12 (1.3) |
| I | 697 (73.4) |
| II | 140 (14.8) |
| III ** | 100 (10.5) |
| Time since the end of active treatment | |
| <18 months | 461 (48.6) |
| ≥18 months | 488 (51.4) |
| Psychological characteristics | |
| Fear of cancer recurrence (FCR) | |
| Low FCR (<13) | 419 (44.2) |
| High FCR (≥13) | 530 (55.8) |
| Function domain of EORTC-QoL-C30 | |
| Poor Physical Function | 168 (17.7) |
| Poor Role Function | 384 (40.5) |
| Poor Emotional Function | 293 (30.9) |
| Poor Cognitive Function | 244 (25.7) |
| Poor Social Function | 332 (35.0) |
| CaSUN-K’s Survey Items | Question Number | No Need | Met Need | Unmet Need, Weak | Unmet Need, Moderate | Unmet Need, Strong | Unmet Need Moderate-to-Strong |
|---|---|---|---|---|---|---|---|
| Number (%) | Number (%) | Number (%) | Number (%) | Number (%) | Number (%) | ||
| Information | |||||||
| Up-to-date information | 1 | 178 (18.8) | 135 (14.2) | 239 (25.2) | 178 (18.8) | 219 (23.1) | 397 (41.8) |
| Information for others | 2 | 221 (23.3) | 108 (11.4) | 256 (27.0) | 177 (18.7) | 187(19.7) | 364 (38.4) |
| Understandable information | 3 | 176 (18.5) | 98 (10.3) | 255 (26.9) | 188 (19.8) | 232 (24.4) | 420 (44.3) |
| Comprehensive cancer care | |||||||
| Best medical care | 4 | 238 (25.1) | 154 (16.2) | 175 (18.4) | 172 (18.1) | 210 (22.1) | 382 (40.3) |
| Local healthcare services | 5 | 228 (24.0) | 124 (13.1) | 175 (18.4) | 192 (20.2) | 230 (24.2) | 422 (44.5) |
| Manage health with team | 6 | 144 (15.2) | 143 (15.1) | 203 (21.4) | 193 (20.3) | 266 (28.0) | 459 (48.4) |
| Communication among doctors | 7 | 145 (15.3) | 131 (13.8) | 200 (21.1) | 200 (21.1) | 273 (28.8) | 473 (49.8) |
| Complaints are addressed | 8 | 236 (24.9) | 127 (13.4) | 176 (18.5) | 185 (19.5) | 225 (23.7) | 410 (43.2) |
| Complimentary therapy * | 9 | 405 (42.7) | 80 (8.4) | 199 (21.0) | 134 (14.1) | 131 (13.8) | 265 (27.9) |
| Accessible hospital parking | 18 | 557 (58.7) | 95 (10.0) | 95 (10.0) | 66 (7.0) | 136 (14.3) | 202 (21.3) |
| Existential survivorship | |||||||
| Reduce stress in my life | 10 | 274 (28.9) | 142 (15.0) | 262 (27.6) | 150 (15.8) | 121 (12.8) | 271 (28.6) |
| Concerns about cancer coming back | 19 | 155 (16.3) | 71 (7.5) | 234 (24.7) | 159 (16.8) | 330 (34.8) | 489 (51.5) |
| Emotional support for me | 20 | 352 (37.1) | 102 (10.7) | 218 (23.0) | 166 (17.5) | 111 (11.7) | 277 (29.2) |
| New relationships | 23 | 470 (49.5) | 107 (11.3) | 184 (19.4) | 102 (10.7) | 86 (9.1) | 188 (19.8) |
| Talk to others | 24 | 355 (37.4) | 110 (11.6) | 230 (24.2) | 138 (14.5) | 116 (12.2) | 254 (26.8) |
| Handle social/work situations | 25 | 462 (48.7) | 100 (10.5) | 196 (20.7) | 109 (11.5) | 82 (8.6) | 191 (20.1) |
| Changes to my body | 26 | 371 (39.1) | 113 (11.9) | 234 (24.7) | 142 (15.0) | 89 (9.4) | 231 (24.3) |
| Ongoing case manager * | 28 | 490 (51.6) | 68 (7.2) | 167 (17.6) | 110 (11.6) | 114 (12.0) | 224 (23.6) |
| Move on with my life | 29 | 424 (44.7) | 124 (13.1) | 216 (22.8) | 105 (11.1) | 80 (8.4) | 185 (19.5) |
| Changes to beliefs | 30 | 422 (44.5) | 111 (11.7) | 228 (24.0) | 114 (12.0) | 74 (7.8) | 188 (19.8) |
| Acknowledging the impact | 31 | 518 (54.6) | 121 (12.8) | 165 (17.4) | 85 (9.0) | 60 (6.3) | 145 (15.3) |
| Survivor expectations | 32 | 415 (43.7) | 140 (14.8) | 209 (22.0) | 101 (10.6) | 84 (8.9) | 185 (19.5) |
| Decisions about my life | 33 | 467 (49.2) | 110 (11.6) | 192 (20.2) | 103 (10.9) | 77 (8.1) | 180 (19.0) |
| Spiritual beliefs | 34 | 546 (57.5) | 136 (14.3) | 134 (14.1) | 82 (8.6) | 51 (5.4) | 133 (14.0) |
| Make my life count | 35 | 476 (50.2) | 117 (12.3) | 189 (19.9) | 96 (10.1) | 71 (7.5) | 167 (17.6) |
| Quality of life | |||||||
| Manage side effects | 11 | 352 (37.1) | 83 (8.7) | 201 (21.2) | 136 (14.3) | 177 (18.7) | 313 (33.0) |
| Changes to quality of life | 12 | 300 (31.6) | 112 (11.8) | 235 (24.8) | 143 (15.1) | 159 (16.8) | 302 (31.8) |
| Relationships | |||||||
| Support partner/family | 21 | 410 (43.2) | 100 (10.5) | 203 (21.4) | 133 (14.0) | 103 (10.9) | 236 (24.9) |
| Impact on my relationship | 22 | 450 (47.4) | 92 (9.7) | 188 (19.8) | 122 (12.9) | 97 (10.2) | 219 (23.1) |
| Changes to partner’s life * | 13 | 900 (94.8) | 23 (2.4) | 11 (1.2) | 6 (0.6) | 9 (0.9) | 15 (1.6) |
| Problems with sex life | 27 | 707 (74.5) | 66 (7.0) | 109 (11.5) | 44 (4.6) | 23 (2.4) | 67 (7.1) |
| Financial issues (new dimension) | |||||||
| Impact on my working life * | 14 | 729 (76.8) | 59 (6.2) | 78 (8.2) | 37 (3.9) | 46 (4.8) | 83 (8.7) |
| Financial support * | 15 | 502 (52.9) | 77 (8.1) | 141 (14.9) | 104 (11.0) | 125 (13.2) | 229 (24.1) |
| Life/travel insurance * | 16 | 584 (61.5) | 73 (7.7) | 139 (14.6) | 71 (7.5) | 82 (8.6) | 153 (16.1) |
| Legal services * | 17 | 600 (63.2) | 53 (5.6) | 118 (12.4) | 92 (9.7) | 86 (9.1) | 178 (18.8) |
| Information | Comprehensive Cancer Care | Existential Survivorship | Quality of Life | Relationship | Financial Issues | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | aOR * (95% CI) | OR (95% CI) | aOR * (95% CI) | OR (95% CI) | aOR * (95% CI) | OR (95% CI) | aOR * (95% CI) | OR (95% CI) | aOR * (95% CI) | OR (95% CI) | aOR * (95% CI) | |
| Sociodemographic characteristics | ||||||||||||
| Age | ||||||||||||
| ≥65 years | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| <65 years | 1.09 (0.85, 1.41) | 1.09 (0.84, 1.40) | 1.20 (0.93, 1.56) | 1.19 (0.91, 1.55) | 1.17 (0.89, 1.55) | 1.48 (1.09, 2.02) | 1.54 (1.09, 2.18) | |||||
| Sex | ||||||||||||
| Female | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| Male | 0.88 (0.67, 1.13) | 1.11 (0.86, 1.43) | 1.37 (1.01, 1.85) | 0.77 (0.59, 1.00) | 0.83 (0.63, 1.07) | 1.00 (0.76, 1.32) | 0.92 (0.68, 1.25) | |||||
| Marital status | ||||||||||||
| Non-married | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| Married | 0.81 (0.56, 1.18) | 1.24 (0.86, 1.80) | 0.61 (0.41, 0.91) | 0.75 (0.51, 1.09) | 1.04 (0.70, 1.56) | 0.40 (0.27, 0.59) | ||||||
| Education level | ||||||||||||
| ≥University | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| High school | 1.00 (0.74, 1.35) | 1.10 (0.82, 1.49) | 1.08 (0.80, 1.47) | 1.01 (0.74, 1.38) | 0.92 (0.67, 1.28) | 1.02 (0.71, 1.45) | ||||||
| ≤Middle school | 1.09 (0.79, 1.50) | 1.05 (0.77, 1.45) | 1.04 (0.75, 1.44) | 1.06 (0.76, 1.46) | 0.86 (0.61, 1.21) | 0.86 (0.59, 1.27) | ||||||
| Employment status | ||||||||||||
| Employed | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| Unemployed | 1.07 (0.83, 1.39) | 0.90 (0.69, 1.16) | 1.29 (0.99, 1.68) | 1.09 (0.84, 1.42) | 1.16 (0.88, 1.54) | 0.97 (0.71, 1.32) | ||||||
| Household monthly income | ||||||||||||
| <USD$3000 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| ≥USD$3000 | 0.91 (0.69, 1.19) | 1.03 (0.78, 1.35) | 0.79 (0.60, 1.05) | 0.92 (0.70, 1.22) | 0.90 (0.67, 1.20) | 0.76 (0.55, 1.05) | ||||||
| Disease-related characteristics | ||||||||||||
| Comorbidity | ||||||||||||
| No | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| Yes | 1.12 (0.83, 1.50) | 1.21 (0.90, 1.62) | 1.13 (0.84, 1.52) | 1.27 (0.93, 1.72) | 1.06 (0.77, 1.45) | 0.80 (0.57, 1.13) | ||||||
| Pathologic stage | ||||||||||||
| 0–I | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| II | 1.25 (0.87, 1.79) | 1.09 (0.76, 1.56) | 1.23 (0.85, 1.79) | 1.37 (0.95, 1.97) | 1.47 (1.01, 2.14) | 1.32 (0.87, 2.01) | ||||||
| III | 1.37 (0.80, 1.07) | 1.38 (0.90, 2.10) | 1.67 (1.07, 2.62) | 1.92 (1.26, 2.92) | 1.19 (0.76, 1.86) | 1.72 (1.08, 2.72) | ||||||
| Lapse after active treatment | ||||||||||||
| ≥18 months | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| <18 months | 1.49 (1.16, 1.93) | 1.58 (1.22, 2.04) | 1.50 (1.11, 2.02) | 1.65 (1.27, 2.14) | 1.55 (1.12, 2.14) | 1.70 (1.31, 2.21) | 1.59 (1.17, 2.15) | 1.43 (1.09, 1.89) | 1.55 (1.14, 2.11) | |||
| Psychological characteristics | ||||||||||||
| Fear of Cancer Recurrence | ||||||||||||
| Low FCR (<13) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| High FCR (≥13) | 4.64 (3.52, 6.12) | 4.13 (3.02, 5.64) | 4.29 (3.26, 5.64) | 3.87 (2.83, 5.30) | 7.05 (5.28, 9.41) | 5.99 (4.32, 8.30) | 4.97 (3.69, 6.68) | 3.90 (2.79, 5.46) | 5.44 (3.90, 7.57) | 4.39 (3.02, 6.39) | 3.89 (2.72, 5.57) | 2.77 (1.85, 4.15) |
| EORTC-QoL-C30 | ||||||||||||
| Poor Physical Function | 2.27 (1.60, 3.21) | 1.92 (1.36, 2.71) | 3.13 (2.10, 4.67) | 1.64 (1.01, 2.65) | 2.14 (1.53, 3.00) | 1.78 (1.26, 2.50) | 1.71 (1.18, 2.48) | |||||
| Poor Role Function | 2.22 (1.71, 2.90) | 2.05 (1.57, 2.67) | 2.19 (1.66, 2.88) | 2.19 (1.68, 2.86) | 2.30 (1.74, 3.04) | 2.45 (1.80, 3.35) | 1.56 (1.09, 2.24) | |||||
| Poor Emotional Function | 3.47 (2.58, 4.66) | 1.93 (1.35, 2.77) | 3.11 (2.32, 4.17) | 1.70 (1.18, 2.44) | 3.99 (2.89, 5.52) | 1.65 (1.09, 2.49) | 3.53 (2.65, 4.71) | 1.86 (1.30, 2.65) | 3.65 (2.72, 4.89) | 1.87 (1.31, 2.68) | 3.73 (2.72, 5.13) | 2.31 (1.60, 3.35) |
| Poor Cognitive Function | 2.64 (1.95, 3.59) | 1.65 (1.18, 2.31) | 2.38 (1.75, 3.23) | 2.67 (1.92, 3.70) | 2.17 (1.62, 2.92) | 2.32 (1.72, 3.15) | 2.39 (1.72, 3.30) | |||||
| Poor Social Function | 2.73 (2.07, 3.61) | 2.87 (2.17, 3.80) | 1.89 (1.34, 2.66) | 4.18 (3.07, 5.70) | 2.34 (1.59, 3.44) | 3.27 (2.48, 4.33) | 2.00 (1.42, 2.80) | 3.01 (2.26, 4.01) | 1.79 (1.26, 2.53) | 2.57 (1.88, 3.51) | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, J.; Jung, W.; Lee, G.; Kang, D.; Shim, Y.M.; Kim, H.K.; Jeong, A.; Cho, J.; Shin, D.W. Unmet Supportive Care Needs after Non-Small Cell Lung Cancer Resection at a Tertiary Hospital in Seoul, South Korea. Healthcare 2023, 11, 2012. https://doi.org/10.3390/healthcare11142012
Park J, Jung W, Lee G, Kang D, Shim YM, Kim HK, Jeong A, Cho J, Shin DW. Unmet Supportive Care Needs after Non-Small Cell Lung Cancer Resection at a Tertiary Hospital in Seoul, South Korea. Healthcare. 2023; 11(14):2012. https://doi.org/10.3390/healthcare11142012
Chicago/Turabian StylePark, Junhee, Wonyoung Jung, Genehee Lee, Danbee Kang, Young Mog Shim, Hong Kwan Kim, Ansuk Jeong, Juhee Cho, and Dong Wook Shin. 2023. "Unmet Supportive Care Needs after Non-Small Cell Lung Cancer Resection at a Tertiary Hospital in Seoul, South Korea" Healthcare 11, no. 14: 2012. https://doi.org/10.3390/healthcare11142012
APA StylePark, J., Jung, W., Lee, G., Kang, D., Shim, Y. M., Kim, H. K., Jeong, A., Cho, J., & Shin, D. W. (2023). Unmet Supportive Care Needs after Non-Small Cell Lung Cancer Resection at a Tertiary Hospital in Seoul, South Korea. Healthcare, 11(14), 2012. https://doi.org/10.3390/healthcare11142012






