Abstract
Long COVID syndrome has been recognized as a public health problem. Digital physiotherapy practice is an alternative that can better meet the needs of patients. The aim of this review was to synthesize the evidence of digital physiotherapy practice in Long COVID patients. A systematic review was carried out until December 2022. The review was complemented by an assessment of the risk of bias and methodological quality. A narrative synthesis of results was conducted, including subgroup analyses by intervention and clinical outcomes. Six articles, including 540 participants, were selected. Five articles were considered of high enough methodological quality. Parallel-group, single-blind, randomized controlled trials were the most commonly used research design. Tele-supervised home-based exercise training was the most commonly used intervention. Great heterogeneity in clinical outcomes and measurement tools was found. A subgroup analysis showed that digital physiotherapy is effective in improving clinical outcomes. Significant differences in favor of digital interventions over usual care were reported. Nevertheless, discrepancies regarding effectiveness were found. Improvements in clinical outcomes with digital physiotherapy were found to be at least non-inferior to usual care. This review provides new evidence that digital physiotherapy practice is an appropriate intervention for Long COVID patients, despite the inherent limitations of the review. Registration: CRD42022379004.
1. Introduction
The syndrome known as Long COVID or persistent COVID has been defined by the World Health Organization (WHO) as a condition that occurs in people with probable or confirmed SARS-CoV-2 infection with symptoms lasting at least 2 months and that cannot be explained by an alternative diagnosis [1,2]. Symptoms are wide-ranging and fluctuating [3,4] and can include fatigue and shortness of breath dysfunction. Over 200 different reported symptoms present against daily functions, job position, health perception, and mood, among others [5,6,7,8]. A very similar definition was provided by The National Health Service in England (NHS), who defined Long COVID as the signs and symptoms that develop during or after COVID-19 and continue for more than 12 weeks and are not explained by an alternative diagnosis [9]. To add more information, we include the definition of The National Research Action Plan on Long COVID and the Services and Supports for the Longer-term Impacts of COVID-19 from the United States government, which defined Long COVID as signs, symptoms, and conditions that continue or develop after initial COVID-19 or SARS-CoV-2 infection. The signs, symptoms, and conditions are present four weeks or more after the initial phase of infection; may be multisystemic; and may present with a relapsing–remitting pattern and progression or worsening over time, with the possibility of severe and life-threatening events even months or years after infection. It represents many potentially overlapping entities, likely with different biological causes and different sets of risk factors and outcomes [10].
Long COVID has been recognized as a public health problem; therefore, interventions that support patient management are critical to reducing the disease burden [11]. Symptoms persisted for more than six months with at least one sequela, requiring ongoing rehabilitation and evaluation, as has been stated [12], with a significant impact on reduced quality of life, capacity to work, and performance of usual daily activities [13]. The long-term effects of the disease are not related to the severity of the initial infection; they can affect young and adult fit patients and those who did not visit the hospital with COVID symptoms [9].
A clinical guideline for Long COVID patients was developed, including the recommendation of physiotherapy interventions and strongly advocating a multidisciplinary rehabilitation approach [14]. Digital physiotherapy practices, are methods and protocols for carrying out the rehabilitation process remotely, with or without supervision, and may also be referred to as telehealth, telemedicine or telerehabilitation [15]. The digital physiotherapy practice has been suggested as an innovative strategy in the management of COVID-19 disease [16] and its sequelae [17], aiming to increase accessibility and improve continuity of care [18]. Recent research showed that digital physiotherapy interventions could improve functional capacity and exercise perception and could be applied with minimal adverse impacts [19]. Traditional rehabilitation interventions seemed to improve muscle strength, dyspnea, walking capacity, functional capacity and quality of life; nevertheless, results on pulmonary function were inconsistent [20]. Notwithstanding, a recent meta-analysis states that telerehabilitation may be an effective and safe solution for survivors of COVID-19 [21]. However, to date, the evidence of digital interventions is limited, with low certainty of evidence [22], and systematic reviews have pointed out that clinical and economic effectiveness are still lacking [23].
In view of the increasing publication of randomized controlled trials that have not been reviewed to date, a thorough and rigorous review of methodological quality is recommended. On the basis of the diverse nature of digital physiotherapy interventions [24], more research is needed to improve our understanding of why particular interventions are or are not successful [25].
As such, the primary aim of this systematic review was to explore the effectiveness of digital physiotherapy practice interventions compared to usual care for adult patients with Long COVID by reporting the main changes in outcomes. Secondary aims were to describe the characteristics of the digital interventions.
2. Materials and Methods
2.1. Identification Data Sources and Search Strategy
This systematic review was performed following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [26] statement, as well as a synthesis of the findings of all evidence published following the methodological recommendations of the Cochrane Collaboration Handbook. The PRISMA checklist is detailed in Appendix A, Figure A1.
A systematic search in the following databases was conducted: PubMed/MEDLINE, Cochrane Library, PeDro (Physiotherapy Evidence Database), Embase, CINAHL database, Scopus, EBSCO, Prospero, Google Scholar, Tryp database, and NICE. Search was conducted in Title, Abstract, and Keywords. The search strategy combines terms included in MeSH related to the population and intervention used: “Long COVID” OR “persistent COVID syndrome” AND “Digital Physiotherapy Practice” OR “Telemedicine” OR “Telerehabilitation”. The search strategy with keywords is reported in Appendix A, Table A1.
Search includes publication dates from 2019 to 2022 in any language. For trials published in lesser-used languages, a translated version was sourced. Abstracts and articles were screened for further eligibility. In addition, a search was performed on the ClinicalTrials.gov registry website in order to locate ongoing and unpublished trials. A hand search of references was also performed for further relevant bibliographies.
2.2. Study Selection
In line with the PRISMA guidelines, the inclusion and exclusion criteria were established through the definition of the PICO (population, intervention, comparison, and assessment) strategy. The PICO acronym (Patient/Population–Intervention–Comparison/Comparator–Outcome) [27] was used with the intention to answer the research question: Is the practice of digital physiotherapy effective to improve clinical outcomes in patients with Long COVID compared to usual care?
- Patients:
Adults [≥18 years] with a diagnosis of Long COVID syndrome. ICD-10 (U09) e ICD-11 (RA02) [28]. Since the beginning of the pandemic, the classification and terminologies have been progressively activating emergency codes for COVID-19 in ICD-10 and ICD-11. A set of additional codes were activated to document flag conditions that occur in the context of COVID-19 [28].
- Intervention:
Any treatment intervention, synchronous or asynchronous, provided via digital physiotherapy practice or rehabilitation services at a distance. The intervention must have been a practice in any area of physical therapy, as defined by the World Confederation for Physical Therapy [29], remotely or outside of a regular session by a physiotherapist thanks to new technologies.
- Comparison:
Digital physiotherapy practice compared with usual face-to-face rehabilitation treatments, center-based rehabilitation treatments, or usual care and educational care for Long COVID symptoms.
- Outcomes:
As primary outcomes, any clinical outcome measure (pulmonary capacity, dyspnea, daily life activities, functional capacity, health-related quality of life, muscle strength, balance, cardiovascular parameters). Secondary outcomes may include satisfaction with care, participant experience, adherence, and adverse effects.
- Study Design:
Only Randomized clinical trials [RCTs] were included.
The exclusion criteria were:
Telehealth interventions for monitoring symptoms or physiological parameters only (i.e., telemonitoring). Studies where the comparison group received no usual care, no treatment, or no rehabilitation (waiting list) will be excluded.
2.3. Data Extraction
Titles and abstracts were screened by two reviewers. If an article appeared to be potentially relevant, it was retrieved as a full-text article and assessed to see if it fulfilled the criteria for inclusion/exclusion. If a consensus could not be reached, a third or fourth reviewer was consulted. The reviewers identified and excluded duplicates. Following the full-text analysis, a decision was made as to which articles must be included in the final review. Study characteristics and outcomes data were collected, including eligibility criteria, sample size, age and country of recruitment, type of intervention, session frequency, program duration, delivery format, outcomes measures, assessment time points and follow-up.
2.4. Evaluation of Methodological Quality and Risk of Bias
PeDro scale, based on the Delphi list, was used to evaluate methodological quality and risk of bias was evaluated using the Cochrane risk-of-bias tool for randomized trials (RoB 2) [30]. The PeDro scale is made up of 11 criteria that assess internal validity. The PeDro scale scores 10 items (the eligibility criteria do not contribute to the total score). Articles are rated present (1) or absent (0), and each trial is given a total PeDro score ranging from 0 to 10 [31]. It will be considered a low-risk study with high methodological quality with scores equal to or greater than 5 [32].
Assessment of the risk of bias in individual studies was performed as recommended by the Cochrane Collaboration Handbook. Version 2 of the Cochrane risk-of-bias tool for randomized trials (RoB 2) is a recommended instrument to assess the risk of bias in randomized trials included in a systematic review [33]. RoB 2 is structured into a fixed set of bias domains, focusing on different aspects of trial design and reflecting current understanding of how causes of bias may influence study results and the most appropriate ways to assess this risk. Each domain was classified as “low risk of bias”, “some concerns” or “high risk of bias” [34,35].
2.5. Data Synthesis and Analysis
The results of the included studies were analyzed through separate narrative syntheses. The data was organized in an Excel spreadsheet and was described as follows: authors/year, design study, risk of bias, intervention characteristics and duration, outcome measures, follow-up and results. Results include all available data.
3. Results
The review was conducted according to the registered protocol: CRD42022379004. Figure 1 presents this study’s selection process in a Flowchart, as recommended in the PRISMA statement [36], which shows the total number of retrieved references and the number of included and excluded studies.
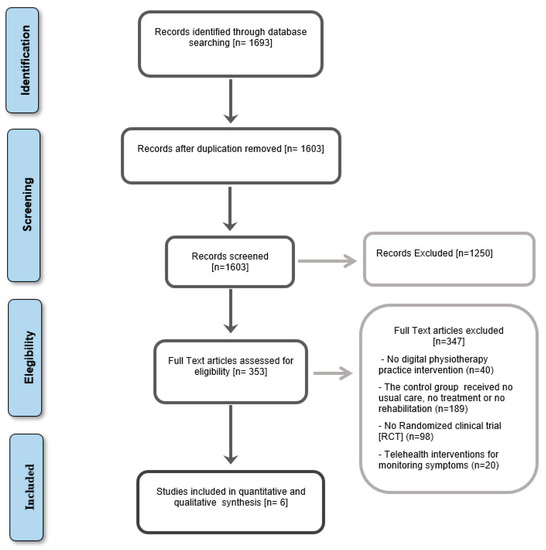
Figure 1.
PRISMA Flowchart.
The electronic search strategy identified a total of 1693 records from the selected databases. After screening titles, abstracts and reference lists, 353 potentially relevant records underwent full-text review. Of these, six randomized controlled trials were included [37,38,39,40,41,42]. Full-text articles excluded did not meet the eligibility criteria and were excluded due to an ineligible study design, population, intervention, or comparator. Data was extracted from all the study’s reports wherever possible.
3.1. Risk of Bias and Methodological Quality
Table 1 shows an evaluation of the methodological quality using the PeDro scale. Studies included in the review had scores of two to nine. High enough methodological quality was considered if they had a score of at least five [43]. We found one study with a PeDro score of nine [40], which is considered “excellent”, three studies with scores between six and eight [37,38,42], which are considered “good”, one study with a score of five [39], considered “fair”, and one study with a score < six, considered ‘poor’ [41].

Table 1.
Evaluation of the Methodological Quality of the Selected Studies.
Figure 2 shows a risk of bias summary using the Cochrane Risk of Bias. A risk of bias graph is shown in Figure 3. A low risk of bias was found in four studies [37,38,40,42], some concerns of bias were found in one [39], and a high risk of bias was found in one study [41].
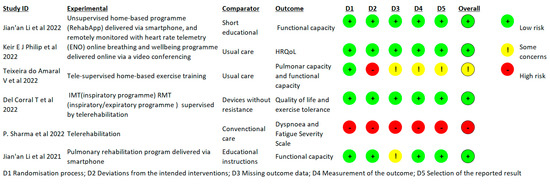
Figure 2.
Risk of bias summary [37,38,39,40,41,42].
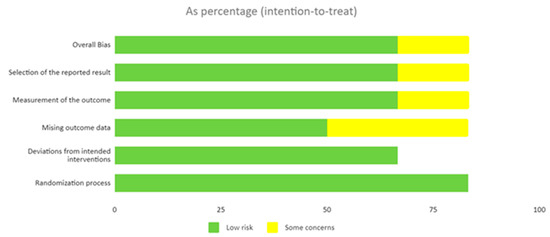
Figure 3.
Risk of bias graph.
3.2. Characteristics of the Included Trials
Table 2 shows the synthesized findings. Six RCTs with a total of 540 participants met the inclusion criteria and were considered. All studies included patients with Long COVID Syndrome aged from 18 to 75 years. All participants were assigned from their home hospital and complied with ICD-10 Diagnosis. The results of this review cover a wide geographical diversity of participants from China [37,42], the United Kingdom [38], Brazil [39], Spain [40] and India [41].

Table 2.
Characteristics of Studies.
The results of the articles included in the review show great heterogeneity in terms of interventions, effect sizes reported, clinical outcomes and instruments used. As examples, the studies that evaluate lung capacity reveal differences in the intervention approach as well as in the measurement instruments used. Heterogeneity occurs when there are methodological discordances among the trials included in the review: when the patient populations and the disease or symptoms are not exactly the same in their characteristics; when the outcome variables used are not defined exactly the same, nor are they measured in exactly the same way; when the interventions applied to the patients are not exactly the same, although they bear the same name; and when some of the included trials present some bias in their results, as has been previously stated [44].
Regarding the sample size, four of the articles [37,38,40,42] included a population of more than eighty subjects. In two of the studies [39,41] intervention groups did not exceed fifteen subjects. Parallel-group, single-blind, randomized controlled trials were the most commonly used research designs. Only one study included four arms [40].
3.2.1. Interventions
Regarding interventions, tele-supervised home-based exercise training was the most commonly used method in four studies [37,38,39,40], including 233 participants. A group-guided session was found with semi-structured participant discussion [38]. Two studies opted for an unsupervised program with one weekly teleconsultation, including a total of 74 participants [41,42]. Control groups received short educational instructions at baseline [37,42] or usual care [38,39,41] by continuing their clinical management and any other clinical services, or online supervised respiratory muscle training [40]. A subgroup analysis by intervention is presented in Table 3.

Table 3.
Subgroup Analysis by Intervention.
3.2.2. Outcomes
With reference to clinical outcomes and measurement, we found great heterogeneity in pulmonary capacity, quality of life, dyspnea, functional capacity, cognitive and psychological status, exercise tolerance, fatigue, cardiovascular function, and participants’ experiences. A subgroup analysis by outcomes is presented in Table 4.

Table 4.
Subgroup Analysis by Outcomes.
3.2.3. Results of Articles
A subgroup analysis of the results from the digital physiotherapy intervention showed that five studies stated positive effects on pulmonary capacity [37,38,39,40,42], but only three studies showed significant differences compared to the control group [38,39,40]. Improvements in quality of life were found [37,38,40,42], and mental components in the two articles improved without significant differences from the control group [37,42]. Digital physiotherapy practice has also shown improvement in dyspnea in four articles [37,38,41,42]. In one of the studies, the results of the intervention showed significant differences compared to the control group [41]. In studies without significant differences in improvements [37,38,42], only short-term effects were found. Improvements in functional capacity were found in four studies [37,39,40,42], and significant differences with the control group were found in three of them [37,40,42].
From a cognitive and psychological standpoint [38,40], improvements were observed in the intervention group, although differences were not statistically significant.
Fatigue improvement was reported in one of the studies, with significant results compared to the control group [41]. Exercise tolerance was superior over the control group, but between time and group factors, there were no statistically significant interactions [40]. Cardiovascular function improvements due to digital physiotherapy intervention were found in one study with significant differences from the control group [39]. And finally, participants’ positive experiences [38] were reported, suggesting that participants had improvements that were meaningful to them and even small improvements in measured Quality of life. The level of significance was set at p < 0.05. A subgroup analysis of the results is shown in Table 5.

Table 5.
Subgroup Analysis by Results.
4. Discussion
Our systematic review was carried out to analyze the effectiveness of digital physiotherapy practice to improve clinical outcomes in patients with Long COVID compared to usual care. The results of our review are in line with those shown in previous investigations, adding improvements in pulmonary capacity and function. The authors want to highlight the existence of significant improvements versus control groups in three studies, which provides important new knowledge for Long COVID patients.
Regarding the results of rehabilitation interventions, a previous meta-analysis [20] synthesized the effects in COVID-19 patients, concluding that standard rehabilitation seemed to improve dyspnea, anxiety, kinesiophobia, muscle strength, walking capacity, sit-to-stand performance, and quality of life; however, results on pulmonary function were inconsistent. Another systematic review in 2022 focused on telerehabilitation interventions [45], where COVID-19 and post-COVID-19 patients were included and pooled, and concluded that telerehabilitation effects on pulmonary function remain very uncertain with very low certainty of evidence.
Digital physiotherapy practice and synonymous terms have been positioned as a viable alternative intervention for COVID-19 patients and their sequelae; nevertheless, the authors feel it is necessary to discuss some key points identified during this review.
Firstly, this systematic review is focused on Long COVID patients based on the WHO definition of inclusion criteria. This allows us to align with the most current definitions of persistent symptoms and to minimize heterogeneity in the participants of the included studies, which represents an important differentiation with respect to previous reviews [19,20,45].
Secondly, our review includes as an inclusion criterion the existence of control groups receiving usual face-to-face rehabilitation treatments, center-based rehabilitation treatments, or usual care and educational care at least, avoiding statements of the effects of digital physiotherapy practice versus non-interventions that have been included in previous reviews [38]. Furthermore, reviews that combined face-to-face, home exercise programs, and digital interventions as experimental groups imply some limitations of the evidence available for each intervention. In our review, only physiotherapy digital interventions in any area defined by the World Confederation for Physical Therapy were included.
With regard to methodological quality, internal validity and the risk of bias have been assessed through validated tools. Evidence-based practice encourages the integration of high-quality evidence into clinical decision-making for patient care. In turn, low-quality clinical trials can lead to misinterpretations in the systematic reviews that combine them [5,46]. Nevertheless, the authors wish to emphasize that the inclusion of low-quality studies in this systematic review is essential to avoid bias and noted that one of the included studies [41] has a high risk of bias and low internal validity, so results should be interpreted as such, avoiding selection and interpretation biases.
Numerous feasibility studies and clinical trials are currently ongoing, including preliminary results in Long COVID patients [47], which require a continuous review of updated knowledge. Research priorities from WHO and the Long COVID Forum Group with respect to Long COVID involve improving clinical characterization and research and development of therapies [48]. Clinical characterization of patients with Long COVID is essential to providing appropriate treatment options [49]. In this sense, the inclusion criteria regarding digital physiotherapy interventions and clinical outcomes in our review allow us to contribute new, specific knowledge to the scientific demands.
With regard to quality of life, this review shows improvements due to digital interventions; however, in some studies, the improvements compared to the control group are minimal or nonexistent in physical or mental components, which can be interpreted in line with the results published in previous reviews. Some authors have noted that, interestingly, the affective component has improved substantially, suggesting the emotional impact it had [38].
Another aspect we would like to point out is the use of qualitative criteria. In a qualitative interview study in the United Kingdom, online peer support helped patients overcome feelings of inadequate care from healthcare professionals. Furthermore, patients reported feeling less alone and more validated after using online peer support [50]. According to studies indicating that the role of social support for Long COVID patients seems relevant, given that many of them do not feel that they are treated or cared for seriously [51]. Tele-supervised interventions allow more contact with the patient, which may be a clear explanation, as has been previously stated [52].
With regard to the variety and modalities of digital interventions, and despite the variety and quantity of available alternative models implemented globally [53], this review shows scarce intervention alternatives. Tele-supervised home-based exercise training was the most commonly used method. No other digital physiotherapy practices, such as artificial intelligence, virtual reality or video games, currently in common use met the inclusion criteria for this review [54,55,56].
Our review confirms improvements and significant differences from usual care when digital physiotherapy practice is used in Dyspnea, Functional capacity, Cognitive and psychological status, Fatigue, Exercise Tolerance, Cardiovascular function, and Participants’ experiences. These results are in line with the results published in previous reviews on different COVID patients and bring updated knowledge to Long COVID patients.
A previous meta-analysis, including COVID-19 survivors [21], states the superiority of telerehabilitation over no treatment or usual care for dyspnea, limb muscle strength, ambulation capacity, and depression. No significant difference was found in anxiety or quality of life, and no dates were included about pulmonary capacity. No severe adverse events were reported in any of the included studies in this meta-analysis. The authors stated moderate to very low-quality evidence [21]. In our review, we excluded studies where the comparison group received no usual care, no treatment or no rehabilitation (waiting list).
Only randomized clinical trials were included. The methodological analysis of the selected articles showed one study considered “excellent”, three studies considered “good”, one study considered “fair” and one study considered “poor”.
With regard to the adherence of the intervention in this review, it was reported as satisfactory in four articles [37,38,40,42]. In one article [38], program adherence was monitored by a registry, including emails and telephone calls. In one article [40], it was observed that remote supervision could have the potential to improve access to rehabilitation programs, which could increase the motivation of participants. In two articles [39,41], adherence was not evaluated.
On the other side, the absence of adverse effects is common to all included studies and confirms, once again, the positive effects of digital practices on different pathologies already mentioned in previous reviews.
Concerning possible gender differences, which have been previously addressed in some studies [57], the only issue to be highlighted in our findings is that one of the studies showed that females were more fatigued than males and therefore benefited more from the digital physiotherapy practice [41].
Finally, we would like to highlight the use of remote assessment by a telephone call in one article [37]. Furthermore, outcome measures were collected using a self-completed online form in one article [38]. Online assessment may become relevant and effective, as has been stated in previous research during COVID-19 pandemic restrictions [58], but in our results, no other study used digital technology to assess patients.
Notwithstanding, the results of our systematic review should be interpreted in the context of its unique context and PICO criteria, showing differences from previous reviews, as has been highlighted.
Limitations
Important limitations have been identified in this review. First, limitations due to inclusion criteria mean that only Long COVID adult patients were selected; therefore, under-18-year-old participants are not subject to the review.
Five articles were considered to be of sufficiently high methodological quality; in addition, a low risk of bias was found in four of them. Given the nature of the intervention, only one article [40] used double blinding; therefore, excellent internal validity was limited. The inclusion of very low methodological quality and a high risk of bias in one study [41] limits the overall findings of this review.
The limited scope of the published trials in patients with Long COVID may have led to the conclusion that some studies were simply underpowered to detect a clinically relevant difference. Also, the limited information available on effect size is an important limitation to consider. Moreover, the information regarding dropout rates is limited and should be addressed in depth [39].
5. Conclusions
The results of the present review showed that digital physiotherapy practices could be a real opportunity to improve clinical outcomes, including pulmonary, functional, and cardiovascular capacities, quality of life, dyspnea and fatigue in Long COVID patients.
In line with previous findings in various conditions [59], the effectiveness of digital physiotherapy interventions has been proven, and their results have been shown to be no less inferior to those achieved with usual care for Long COVID patients. Therefore, digital physiotherapy could be an effective alternative to usual care and a viable option for providing a safe way of delivering rehabilitation.
This review provides new evidence that digital physiotherapy practice is an appropriate intervention for Long COVID patients and should be recommended in clinical practice guidelines, despite the inherent limitations of the review.
A robust, comprehensive meta-analysis on the effectiveness of digital physiotherapy practice for patients with Long COVID could be available in the future based on the findings.
Author Contributions
All authors have made significant contributions to the article. M.-J.E.-P., R.M.-V., M.J.V.-G. and J.-M.P.-B. coordinated the project, contributed to the conception and design of this study and drafted the manuscript. As well as being responsible for methodological guidance and contributing to coordinating intervention protocols, patient acquisition and spelling review. All authors have read and agreed to the published version of the manuscript.
Funding
This study received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
All data relevant to this study are included in the article.
Acknowledgments
The University of Malaga, the University of Granada, the University of Cadiz, and, especially, the Long COVID Andalucia Association which initiated it all.
Conflicts of Interest
The authors declare no conflict of interest.
Appendix A
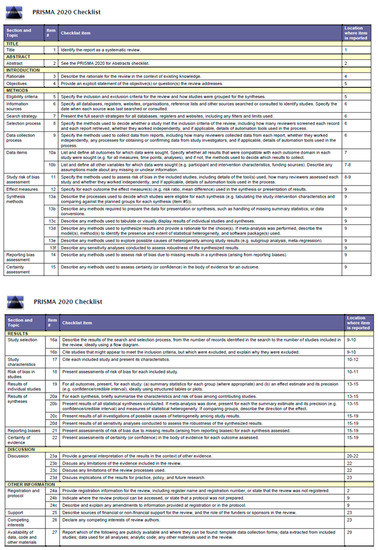
Figure A1.
Prisma Checklist.

Table A1.
The search strategy with keywords.
Table A1.
The search strategy with keywords.
| Database | Search Terms |
|---|---|
| MEDLINE (n = 1648); PeDro (n = 2); Trip database (n = 0); Cochrane (n = 28) Google Schollar (n = 3); Embase (n = 6); CINAHL/EBSCO (n = 1); Scopus (n = 5) NICE (n = 0) Prospero (n = 0) | (“Long COVID” or “post COVID-19” or “persistent COVID syndrome”) AND (“Telemedicine” OR “Telerehabilitation” OR Digital Physiotherapy Practice”) |
References
- Coronavirus Disease (COVID-19): Post COVID-19 Condition. Available online: https://www.who.int/news-room/questions-and-answers/item/coronavirus-disease-(covid-19)-post-covid-19-condition (accessed on 15 June 2023).
- NHS England. National Commissioning Guidance for Post COVID Services. Available online: https://www.england.nhs.uk/publication/national-commissioning-guidance-for-post-covid-services/ (accessed on 15 June 2023).
- Afecciones Persistentes Al COVID-19 Y Afecciones Posteriores Al COVID-19|CDC. Available online: https://espanol.cdc.gov/coronavirus/2019-ncov/long-term-effects/index.html (accessed on 11 January 2023).
- Long COVID or Post-COVID Conditions|CDC. Available online: https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects/index.html (accessed on 11 January 2023).
- Titler, M.G. The Evidence for Evidence-Based Practice Implementation. In Patient Safety and Quality: An Evidence-Based Handbook for Nurses; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2008. [Google Scholar]
- Matriz-Eisenhower.Jpg (560 × 397). Available online: https://images.squarespace-cdn.com/content/v1/5538a145e4b0a3d5e6f58f96/1519291451739-RCFXNB5TFUGUSNBHOV9O/ke17ZwdGBToddI8pDm48kF4-X2XhqtJN7c5IlWAn_IRZw-zPPgdn4jUwVcJE1ZvWQUxwkmyExglNqGp0IvTJZUJFbgE-7XRK3dMEBRBhUpxctm9o8f6K7MioOda3A72qPDwAxCSbfak35Bet1U2ds-JcwNCOzjT0vX_uiFCjGD4/matriz-eisenhower.jpg?format=750w (accessed on 4 December 2020).
- Clinical Management of Severe Acute Respiratory Infection when Novel Coronavirus (2019-nCoV) Infection is Suspected: Interim Guidance. 28 January 2020. Available online: https://apps.who.int/iris/handle/10665/330893 (accessed on 5 May 2022).
- WHO. Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19). Available online: https://www.Who.Int/Publications-Detail/Report-of-the-Who-China-Joint-Mission-on-Coronavirus-Disease-2019-(Covid-19) (accessed on 21 May 2020).
- Coronavirus » Post-COVID Syndrome (Long COVID). Available online: https://www.england.nhs.uk/coronavirus/post-covid-syndrome-long-covid/ (accessed on 14 June 2023).
- COVID.gov—What Is Long COVID. Available online: https://www.covid.gov/longcovid/definitions (accessed on 14 June 2023).
- Prevalence of Ongoing Symptoms Following Coronavirus (COVID-19) Infection in the UK—Office for National Statistics. Available online: https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/prevalenceofongoingsymptomsfollowingcoronaviruscovid19infectionintheuk/1april2021 (accessed on 23 August 2022).
- Hama Amin, B.J.; Kakamad, F.H.; Ahmed, G.S.; Ahmed, S.F.; Abdulla, B.A.; Mohammed, S.H.; Mikael, T.M.; Salih, R.Q.; Ali, R.K.; Salh, A.M.; et al. Post COVID-19 Pulmonary Fibrosis; a Meta-Analysis Study. Ann. Med. Surg. 2022, 77, 103590. [Google Scholar] [CrossRef] [PubMed]
- Harenwall, S.; Heywood-Everett, S.; Henderson, R.; Godsell, S.; Jordan, S.; Moore, A.; Philpot, U.; Shepherd, K.; Smith, J.; Bland, A.R. Post-COVID-19 Syndrome: Improvements in Health-Related Quality of Life Following Psychology-Led Interdisciplinary Virtual Rehabilitation. J. Prim. Care Community Health 2021, 12, 215013192110676. [Google Scholar] [CrossRef] [PubMed]
- Sivan, M.; Taylor, S. NICE Guideline on Long Covid. BMJ 2020, 371, m4938. [Google Scholar] [CrossRef] [PubMed]
- Report of The Wcpt/Inptra Digital Physical Therapy Practice Task Force; WCPT: Chicago, IL, USA, 2020.
- Turan, Z.; Topaloglu, M.; Ozyemisci Taskiran, O. Is Tele-Rehabilitation Superior to Home Exercise Program in COVID-19 Survivors Following Discharge from Intensive Care Unit?—A Study Protocol of a Randomized Controlled Trial. Physiother. Res. Int. 2021, 26, e1920. [Google Scholar] [CrossRef]
- Besnier, F.; Bérubé, B.; Malo, J.; Gagnon, C.; Grégoire, C.-A.A.; Juneau, M.; Simard, F.; L’Allier, P.; Nigam, A.; Iglésies-Grau, J.; et al. Cardiopulmonary Rehabilitation in Long-COVID-19 Patients with Persistent Breathlessness and Fatigue: The COVID-Rehab Study. Int. J. Environ. Res. Public Health 2022, 19, 4133. [Google Scholar] [CrossRef]
- Rogante, M.; Grigioni, M.; Cordella, D.; Giacomozzi, C. Ten Years of Telerehabilitation: A Literature Overview of Technologies and Clinical Applications. NeuroRehabilitation 2010, 27, 287–304. [Google Scholar] [CrossRef]
- Seid, A.A.; Aychiluhm, S.B.; Mohammed, A.A. Effectiveness and Feasibility of Telerehabilitation in Patients with COVID-19: A Systematic Review and Meta-Analysis. BMJ Open 2022, 12, e063961. [Google Scholar] [CrossRef]
- Fugazzaro, S.; Contri, A.; Esseroukh, O.; Kaleci, S.; Croci, S.; Massari, M.; Facciolongo, N.C.; Besutti, G.; Iori, M.; Salvarani, C.; et al. Rehabilitation Interventions for Post-Acute COVID-19 Syndrome: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 5185. [Google Scholar] [CrossRef]
- Huang, J.; Fan, Y.; Zhao, K.; Yang, C.; Zhao, Z.; Chen, Y.; Yang, J.; Wang, T.; Qu, Y. Do Patients with and Survivors of COVID-19 Benefit from Telerehabilitation? A Meta-Analysis of Randomized Controlled Trials. Front. Public Health 2022, 10, 954754. [Google Scholar] [CrossRef]
- Janjua, S.; Banchoff, E.; Threapleton, C.J.D.; Prigmore, S.; Fletcher, J.; Disler, R.T. Digital Interventions for the Management of Chronic Obstructive Pulmonary Disease. Cochrane Database Syst. Rev. 2021, 4, CD013246. [Google Scholar] [CrossRef]
- Zischke, C.; Simas, V.; Hing, W.; Milne, N.; Spittle, A.; Pope, R. The Utility of Physiotherapy Assessments Delivered by Telehealth: A Systematic Review. J. Glob. Health 2021, 11, 04072. [Google Scholar] [CrossRef]
- Handbook Integrated Care; Amelung, V., Stein, V., Goodwin, N., Balicer, R., Nolte, E., Suter, E., Eds.; Springer International Publishing: Cham, Switzerland, 2017. [Google Scholar] [CrossRef]
- McLean, S.; Nurmatov, U.; Liu, J.L.Y.; Pagliari, C.; Car, J.; Sheikh, A. Telehealthcare for Chronic Obstructive Pulmonary Disease: Cochrane Review and Meta-Analysis. Br. J. Gen. Pract. 2012, 62, e739–e749. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA Statement for Reporting Systematic Reviews and Meta-Analyses of Studies That Evaluate Health Care Interventions: Explanation and Elaboration. PLoS Med. 2009, 6, e1000100. [Google Scholar] [CrossRef]
- Thomas, J.; Kneale, D.; McKenzie, J.E.; Brennan, S.E.; Bhaumik, S. Determining the Scope of the Review and the Questions It Will Address. In Cochrane Handbook for Systematic Reviews of Interventions; Wiley: Hoboken, NJ, USA, 2019; pp. 13–31. [Google Scholar] [CrossRef]
- Emergency Use ICD Codes for COVID-19 Disease Outbreak. Available online: https://www.who.int/standards/classifications/classification-of-diseases/emergency-use-icd-codes-for-covid-19-disease-outbreak (accessed on 11 January 2023).
- Policy Statement: Description of Physical Therapy|World Physiotherapy. Available online: https://world.physio/policy/ps-descriptionPT (accessed on 11 January 2023).
- Verhagen, E.; Engbers, L. The Physical Therapist’s Role in Physical Activity Promotion. Br. J. Sports Med. 2008, 43, 99–101. [Google Scholar] [CrossRef]
- de Morton, N.A. The PEDro Scale Is a Valid Measure of the Methodological Quality of Clinical Trials: A Demographic Study. Aust. J. Physiother. 2009, 55, 129–133. [Google Scholar] [CrossRef]
- Escala PEDro—PEDro. Available online: https://pedro.org.au/spanish/resources/pedro-scale/ (accessed on 11 January 2023).
- Manual Cochrane de Revisiones Sistemáticas de Intervenciones|Cochrane Training. Available online: https://training.cochrane.org/es/manual-cochrane-de-revisiones-sistemáticas-de-intervenciones (accessed on 26 January 2023).
- Cumpston, M.; Li, T.; Page, M.J.; Chandler, J.; Welch, V.A.; Higgins, J.P.; Thomas, J. Updated Guidance for Trusted Systematic Reviews: A New Edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst. Rev. 2019, 10, ED000142. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A Revised Tool for Assessing Risk of Bias in Randomised Trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef]
- Yepes-Nuñez, J.J.; Urrútia, G.; Romero-García, M.; Alonso-Fernández, S. Declaración PRISMA 2020: Una Guía Actualizada Para La Publicación de Revisiones Sistemáticas. Rev. Española Cardiol. 2021, 74, 790–799. [Google Scholar] [CrossRef]
- Li, J.; Xia, W.; Zhan, C.; Liu, S.; Yin, Z.; Wang, J.; Chong, Y.; Zheng, C.; Fang, X.; Cheng, W.; et al. A Telerehabilitation Programme in Post-Discharge COVID-19 Patients (TERECO): A Randomised Controlled Trial. Thorax 2022, 77, 697–706. [Google Scholar] [CrossRef]
- Philip, K.E.J.; Owles, H.; McVey, S.; Pagnuco, T.; Bruce, K.; Brunjes, H.; Banya, W.; Mollica, J.; Lound, A.; Zumpe, S.; et al. An Online Breathing and Wellbeing Programme (ENO Breathe) for People with Persistent Symptoms Following COVID-19: A Parallel-Group, Single-Blind, Randomised Controlled Trial. Lancet Respir. Med. 2022, 10, 851–862. [Google Scholar] [CrossRef]
- Teixeira Do Amaral, V.; Viana, A.A.; Heubel, A.D.; Linares, S.N.; Martinelli, B.; Witzler, P.H.C.; Orikassa de Oliveira, G.Y.; Zanini, G.D.S.; Borghi Silva, A.; Mendes, R.G.; et al. Cardiovascular, Respiratory, and Functional Effects of Home-Based Exercise Training after COVID-19 Hospitalization. Med. Sci. Sports Exerc. 2022, 54, 1795–1803. [Google Scholar] [CrossRef] [PubMed]
- del Corral, T.; Garrido, R.F.; Plaza-Manzano, G.; Fernández-de-las-Peñas, C.; Navarro-Santana, M.; López-de-Uralde-Villanueva, I. Home-Based Respiratory Muscle Training on Quality of Life and Exercise Tolerance in Long-Term Post-COVID-19: Randomized Controlled Trial. Ann. Phys. Rehabil. Med. 2022, 66, 101709. [Google Scholar] [CrossRef] [PubMed]
- Sharma, P.; Goswami, S.K. Pulmonary Tele-Rehabilitation in Patients (Post COVID-19) With Respiratory Complications: A Randomized Controlled Trial. Indian J. Physiother. Occup. Ther. 2022, 16, 182–189. [Google Scholar] [CrossRef]
- Li, J.; Xia, W.; Zhan, C.; Liu, S.; Yin, Z.; Wang, J.; Chong, Y.; Zheng, C.; Fang, X.; Cheng, W.; et al. Effectiveness of a Telerehabilitation Program for COVID-19 Survivors (TERECO) on Exercise Capacity, Pulmonary Function, Lower Limb Muscle Strength, and Quality of Life: A Randomized Controlled Trial. medRxiv 2021. [Google Scholar] [CrossRef]
- Day, S.J.; Altman, D.G. Statistics Notes: Blinding in Clinical Trials and Other Studies. BMJ Br. Med. J. 2000, 321, 504. [Google Scholar] [CrossRef]
- Escrig Sos, V.J.; Llueca Abella, J.A.; Granel Villach, L.; Bellver Oliver, M. Meta-Analysis: A Basic Way To Understand And Interpret Your Evidence. Rev. Senol. Y Patol. Mamar. 2021, 34, 44–51. [Google Scholar] [CrossRef]
- Vieira, A.G.D.S.; Pinto, A.C.P.N.; Garcia, B.M.S.P.; Eid, R.A.C.; Mól, C.G.; Nawa, R.K. Telerehabilitation Improves Physical Function and Reduces Dyspnoea in People with COVID-19 and Post-COVID-19 Conditions: A Systematic Review. J. Physiother. 2022, 68, 90–98. [Google Scholar] [CrossRef]
- Cashin, A.G.; McAuley, J.H. Clinimetrics: Physiotherapy Evidence Database (PEDro) Scale. J. Physiother. 2020, 66, 59. [Google Scholar] [CrossRef]
- Estebanez-Pérez, M.-J.; Pastora-Bernal, J.-M.; Martín-Valero, R. The Effectiveness of a Four-Week Digital Physiotherapy Intervention to Improve Functional Capacity and Adherence to Intervention in Patients with Long COVID-19. Int. J. Environ. Res. Public Health 2022, 19, 9566. [Google Scholar] [CrossRef]
- Carson, G.; Carson, G.; Sigfrid, L.; Olliaro, P.; Norton, A.; Paparella, G.; Matulevics, R.; Gillesen, A.; Horby, P.; Hastie, C.; et al. Research Priorities for Long Covid: Refined through an International Multi-Stakeholder Forum. BMC Med. 2021, 19, 84. [Google Scholar] [CrossRef]
- Crook, H.; Raza, S.; Nowell, J.; Young, M.; Edison, P. Long Covid—Mechanisms, Risk Factors, and Management. BMJ 2021, 374, n1648. [Google Scholar] [CrossRef]
- Day, H.L.S. Exploring Online Peer Support Groups for Adults Experiencing Long COVID in the United Kingdom: Qualitative Interview Study. J. Med. Internet Res. 2022, 24, e37674. [Google Scholar] [CrossRef]
- Alwan, N.A. The Road to Addressing Long Covid. Science 2021, 373, 491–493. [Google Scholar] [CrossRef]
- Hoaas, H.; Andreassen, H.K.; Lien, L.A.; Hjalmarsen, A.; Zanaboni, P. Adherence and Factors Affecting Satisfaction in Long-Term Telerehabilitation for Patients with Chronic Obstructive Pulmonary Disease: A Mixed Methods Study EHealth/ Telehealth/ Mobile Health Systems. BMC Med. Inform. Decis. Mak. 2016, 16, 26. [Google Scholar] [CrossRef]
- Peretti, A.; Amenta, F.; Tayebati, S.K.; Nittari, G.; Mahdi, S.S. Telerehabilitation: Review of the State-of-the-Art and Areas of Application. JMIR Rehabil. Assist. Technol. 2017, 4, e7. [Google Scholar] [CrossRef]
- Groenveld, T.; Achttien, R.; Smits, M.; de Vries, M.; van Heerde, R.; Staal, B.; van Goor, H.; Steemers, B.; Brink, L.; van den Rijk, T.; et al. Feasibility of Virtual Reality Exercises at Home for Post–COVID-19 Condition: Cohort Study. JMIR Rehabil. Assist. Technol. 2022, 9, e36836. [Google Scholar] [CrossRef]
- Pallavicini, F.; Pepe, A.; Mantovani, F. The Effects of Playing Video Games on Stress, Anxiety, Depression, Loneliness, and Gaming Disorder During the Early Stages of the COVID-19 Pandemic: PRISMA Systematic Review. Cyberpsychol. Behav. Soc. Netw. 2022, 25, 334–354. [Google Scholar] [CrossRef]
- Adamidi, E.S.; Mitsis, K.; Nikita, K.S. Artificial Intelligence in Clinical Care amidst COVID-19 Pandemic: A Systematic Review. Comput. Struct. Biotechnol. J. 2021, 19, 2833–2850. [Google Scholar] [CrossRef]
- Connor, J.; Madhavan, S.; Mokashi, M.; Amanuel, H.; Johnson, N.R.; Pace, L.E.; Bartz, D. Health Risks and Outcomes That Disproportionately Affect Women during the COVID-19 Pandemic: A Review. Soc. Sci. Med. 2020, 266, 113364. [Google Scholar] [CrossRef]
- Kumar, G.N.P.; Urs, A.N.R.; Undi, M.; Bakkannavar, S.M. Online Viva Voce as a Formative Assessment Method in Forensic Medicine during COVID-19 Pandemic. J. Educ. Health Promot. 2022, 11, 160. [Google Scholar] [CrossRef]
- Bernal-Utrera, C.; Montero-Almagro, G.; Anarte-Lazo, E.; Gonzalez-Gerez, J.J.; Rodriguez-Blanco, C.; Saavedra-Hernandez, M. Therapeutic Exercise Interventions through Telerehabilitation in Patients with Post COVID-19 Symptoms: A Systematic Review. J. Clin. Med. 2022, 11, 7521. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).