Digital Online Patient Informed Consent for Anesthesia before Elective Surgery—Recent Practice in Europe
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
4.1. Technical and Practical Implementation
4.2. Legal Basis of Informed Consent
4.3. Time Frame of Informed Consent
4.4. Strength and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ECDC | European Centre for Disease Prevention and Control |
| ESAIC | European Society of Anesthesia and Intensive Care |
| EU | European Union |
| GDPPC | Gross domestic product per capita |
| HCAI | Healthcare-associated infection |
| WHO | World Health Organisation |
References
- Tsai, H.-W.; Huang, S.-W.; Hung, Y.-L.; Hsu, Y.-S.; Huang, C.-C. Use of the Smart Lean Method to Conduct High-Quality Integrated Perioperative Management Prior to Hospitalization. Int. J. Environ. Res. Public Health 2021, 18, 13391. [Google Scholar] [CrossRef]
- Jia, H.; Li, L.; Li, W.; Hou, T.; Ma, H.; Yang, Y.; Wu, A.; Liu, Y.; Wen, J.; Yang, H.; et al. Impact of Healthcare-Associated Infections on Length of Stay: A Study in 68 Hospitals in China. BioMed Res. Int. 2019, 2019, 2590563. [Google Scholar] [CrossRef]
- World Health Organization. Report on the Burden of Endemic Health Care-Associated Infection Worldwide. 2011. Available online: https://www.who.int/publications/i/item/report-on-the-burden-of-endemic-health-care-associated-infection-worldwide (accessed on 14 May 2022).
- European Centre for Disease Prevention and Control. Annual Epidemiological Report on Communicable Diseases in Europe 2008; European Centre for Disease Prevention and Control: Stockholm, Sweden, 2008.
- Manoukian, S.; Stewart, S.; Dancer, S.; Graves, N.; Mason, H.; McFarland, A.; Robertson, C.; Reilly, J. Estimating excess length of stay due to healthcare-associated infections: A systematic review and meta-analysis of statistical methodology. J. Hosp. Infect. 2018, 100, 222–235. [Google Scholar] [CrossRef]
- Parzeller, M.; Wenk, M.; Zedler, B.; Rothschild, M. Patient Information and Informed Consent before and after Medical Intervention. Dtsch. Aerztebl. Int. 2007, 104, A-576. [Google Scholar]
- Bhaskar, S.; Bradley, S.; Chattu, V.K.; Adisesh, A.; Nurtazina, A.; Kyrykbayeva, S.; Sakhamuri, S.; Moguilner, S.; Pandya, S.; Schroeder, S.; et al. Telemedicine as the New Outpatient Clinic Gone Digital: Position Paper From the Pandemic Health System REsilience PROGRAM (REPROGRAM) International Consortium (Part 2). Front. Public Health 2020, 8, 410. [Google Scholar] [CrossRef]
- Neumann, C.; Schleifer, G.; Strassberger-Nerschbach, N.; Kamp, J.; Massoth, G.; Görtzen-Patin, A.; Cudian, D.; Velten, M.; Coburn, M.; Schindler, E.; et al. Digital Online Anaesthesia Patient Informed Consent before Elective Diagnostic Procedures or Surgery: Recent Practice in Children-An Exploratory ESAIC Survey (2021). J. Clin. Med. 2022, 11, 502. [Google Scholar] [CrossRef]
- Raposo, V.L. Telemedicine: The legal framework (or the lack of it) in Europe. GMS Health Technol. Assess. 2016, 12, Doc03. [Google Scholar] [PubMed]
- Greenhalgh, T.; Vijayaraghavan, S.; Wherton, J.; Shaw, S.; Byrne, E.; Campbell-Richards, D.; Bhattacharya, S.; Hanson, P.; Ramoutar, S.; Gutteridge, C.; et al. Virtual online consultations: Advantages and limitations (VOCAL) study. BMJ Open 2016, 6, e009388. [Google Scholar] [CrossRef] [PubMed]
- Rubin, R. Internet Access as a Social Determinant of Health. JAMA 2021, 326, 298. [Google Scholar] [CrossRef]
- Benda, N.C.; Veinot, T.C.; Sieck, C.J.; Ancker, J.S. Broadband Internet Access Is a Social Determinant of Health! Am. J. Public Health 2020, 110, 1123–1125. [Google Scholar] [CrossRef]
- Agboola, S.; Kvedar, J. Telemedicine and Patient Safety. 2016. Available online: https://psnet.ahrq.gov/perspective/telemedicine-and-patient-safety (accessed on 22 May 2022).
- Blandford, A.; Wesson, J.; Amalberti, R.; AlHazme, R.; Allwihan, R. Opportunities and challenges for telehealth within, and beyond, a pandemic. Lancet Glob. Health 2020, 8, e1364–e1365. [Google Scholar] [CrossRef] [PubMed]
- López Peláez, A.; Erro-Garcés, A.; Pinilla García, F.J.; Kiriakou, D. Working in the 21st Century. The Coronavirus Crisis: A Driver of Digitalisation, Teleworking, and Innovation, with Unintended Social Consequences. Information 2021, 12, 377. [Google Scholar] [CrossRef]
- Reidl, S.; Streicher, J.; Hock, M.; Hausner, B.; Waibel, G.; Gürtl, F. Digitale Ungleichheit—Wie Sie Entsteht, Was Sie Bewirkt und Was Dagegen Hilft Ögut und Joanneum Research, Österreichische Forschungsförderungsgesellschaft. Available online: https://www.joanneum.at/policies/publikationen/detail/digitale-ungleichheit-wie-sie-entsteht-was-sie-bewirkt-und-was-dagegen-hilft (accessed on 30 June 2022).
- Coventry, L.; Branley, D. Cybersecurity in healthcare: A narrative review of trends, threats and ways forward. Maturitas 2018, 113, 48–52. [Google Scholar] [CrossRef]
- Nittari, G.; Khuman, R.; Baldoni, S.; Pallotta, G.; Battineni, G.; Sirignano, A.; Amenta, F.; Ricci, G. Telemedicine Practice: Review of the Current Ethical and Legal Challenges. Telemed. J. E Health. 2020, 26, 1427–1437. [Google Scholar] [CrossRef]
- European Commission. Directorate-General for Health and Food Safety, Meine Gesundheit @ EU: Elektronische Grenzüberschreitende Gesundheitsdienste in der EU (Deutschland), Publications Office. 2020. Available online: https://op.europa.eu/en/publication-detail/-/publication/7344efd6-fed8-11ea-b44f-01aa75ed71a1/language-de (accessed on 22 June 2022). [CrossRef]
- Proposal for a Regulation of the European Parliament and of the Council on the European Health Data Space COM/2022/197 Final. Available online: https://eur-lex.europa.eu/legal-content/EN/TXT/?uri=celex%3A52022PC0197 (accessed on 22 June 2022).
- Biermann, E. Einwilligung nach Aufklärung—Ein juristisches Update. Anasthesiol. Intensivmed. Notfallmed Schmerzther. 2019, 54, 457–473. [Google Scholar] [CrossRef]
- Paterick, T.J.; Carson, G.V.; Allen, M.C.; Paterick, T.E. Medical informed consent: General considerations for physicians. Mayo Clin. Proc. 2008, 83, 313–319. [Google Scholar] [CrossRef]
- Adeleke, I.; Chae, C.; Okocha, O.; Sweitzer, B. Risk assessment and risk stratification for perioperative complications and mitigation: Where should the focus be? How are we doing? Best Pract. Res. Clin. Anaesthesiol. 2021, 35, 517–529. [Google Scholar] [CrossRef] [PubMed]
- Bashshur, R.L.; Shannon, G.W.; Krupinski, E.A.; Grigsby, J.; Kvedar, J.C.; Weinstein, R.S.; Sanders, J.H.; Rheuban, K.S.; Nesbitt, T.S.; Alverson, D.C.; et al. National telemedicine initiatives: Essential to healthcare reform. Telemed. e-Health 2009, 15, 600–610. [Google Scholar] [CrossRef] [PubMed]
- Strassberger-Nerschbach, N.; Magyaros, F.; Maria, W.; Ehrentraut, H.; Ghamari, S.; Schenk, A.; Neumann, C.; Schindler, E. Quality comparison of remote anesthetic consultation versus on-site consultation in children with sedation for a magnetic resonance imaging examination-A randomized controlled trial. Paediatr. Anaesth. 2023. Epub ahead of print. [Google Scholar] [CrossRef]
- Bobb, M.R.; Van Heukelom, P.G.; Faine, B.A.; Ahmed, A.; Messerly, J.T.; Bell, G.; Harland, K.K.; Simon, C.; Mohr, N.M. Telemedicine Provides Noninferior Research Informed Consent for Remote Study Enrollment: A Randomized Controlled Trial. Acad. Emerg. Med. 2016, 23, 759–765. [Google Scholar] [CrossRef]
- Wood, E.W.; Strauss, R.A.; Janus, C.; Carrico, C.K. Telemedicine Consultations in Oral and Maxillofacial Surgery: A Follow-Up Study. J. Oral Maxillofac. Surg. 2016, 74, 262–268. [Google Scholar] [CrossRef]
- Gioia, G.; Salducci, M. Medical and legal aspects of telemedicine in ophthalmology. Rom. J. Ophthalmol. 2019, 63, 197–207. [Google Scholar] [CrossRef] [PubMed]



| n (%) | Female | Male | Diverse | p |
|---|---|---|---|---|
| 406 (43.6) | 521 (56) | 3 (0.3) | ||
| Profession (%) | <0.001 | |||
| Medical doctor | 402 (99.0) | 516 (99.2) | 2 (66.7) | |
| Nurse | 0 (0.0) | 1 (0.2) | 1 (33.3) | |
| Physician assistant | 4 (1.0) | 2 (0.4) | 0 (0.0) | |
| Other | 0 (0.0) | 1 (0.2) | 0 (0.0) | |
| Your expert level (%) | 0.33 | |||
| Anaesthesia technician | 4 (1.0) | 6 (1.2) | 0 (0.0) | |
| Consultant | 303 (74.8) | 426 (81.8) | 2 (66.7) | |
| Resident | 75 (18.5) | 67 (12.9) | 1 (33.3) | |
| Special trained nurse | 0 (0.0) | 1 (0.2) | 0 (0.0) | |
| Other | 23 (5.7) | 21 (4.0) | 0 (0.0) |
| Country of Employment? n (%) | |||
|---|---|---|---|
| Albania | 3 (0.3) | Liechtenstein | 1 (0.1) |
| Austria | 32 (3.4) | Lithuania | 8 (0.9) |
| Belarus | 2 (0.2) | Luxembourg | 4 (0.4) |
| Belgium | 27 (2.9) | Malta | 6 (0.6) |
| Bosnia and Herzegovina | 5 (0.5) | Moldova | 3 (0.3) |
| Bulgaria | 8 (0.9) | Monaco | 1 (0.1) |
| Croatia | 26 (2.8) | Netherlands | 50 (5.4) |
| Cyprus | 4 (0.4) | Macedonia | 3 (0.3) |
| Czechia | 10 (1.1) | Norway | 8 (0.9) |
| Denmark | 11 (1.2) | Poland | 19 (2.0) |
| Estonia | 4 (0.4) | Portugal | 56 (6.0) |
| Finland | 12 (1.3) | Romania | 31 (3.3) |
| France | 24 (2.6) | Russia | 12 (1.3) |
| Georgia | 2 (0.2) | Serbia | 14 (1.5) |
| Germany | 132 (14.2) | Slovakia | 8 (0.9) |
| Greece | 45 (4.8) | Slovenia | 14 (1.5) |
| Hungary | 8 (0.9) | Spain | 73 (7.8) |
| Iceland | 1 (0.1) | Sweden | 43 (4.6) |
| Ireland | 18 (1.9) | Switzerland | 65 (7.0) |
| Israel | 6 (0.6) | Turkey | 23 (2.5) |
| Italy | 40 (4.3) | Ukraine | 7 (0.8) |
| Kazakhstan | 2 (0.2) | United Kingdom (UK) | 44 (4.7) |
| Kosovo | 3 (0.3) | Uzbekistan | 2 (0.2) |
| Latvia | 10 (1.1) |
| GDPPC | High | Middle | Low | |
|---|---|---|---|---|
| n | 454 | 144 | 329 | p |
| Preference n(%) | 0.039 | |||
| In person | 269 (75.1) | 102 (83.6) | 216 (79.1) | |
| Self assessment online | 39 (10.9) | 3 (2.5) | 14 (5.1) | |
| Video Conference online | 40 (11.2) | 13 (10.7) | 35 (12.8) | |
| Telephone | 10 (2.8) | 4 (3.3) | 8 (2.9) |
| Is it possible to obtain informed consent online via internet in your routine setting? | p = 0.101 | ||
| Yes | No | ||
| High GDPPCPC | 89 (75) [1.5] | 222 (235) [−0.85] | |
| Middle GDPPCPC | 49 (56) [−0.96] | 181 (174) [0.54] | |
| Low GDPPCPC | 19 (25) [−1.18] | 83 (77) [0.67] | |
| Is it possible to obtain informed consent online via telephone in your routine setting? | p = <0.001 | ||
| Yes | No | ||
| High GDPPCPC | 175 (124) [4.56] | 139 (190) [−3.69] | |
| Middle GDPPCPC | 56 (91) [−3.63] | 173 (138) [2.93] | |
| Low GDPPCPC | 24 (40) [−2.57] | 78 (61) [2.08] | |
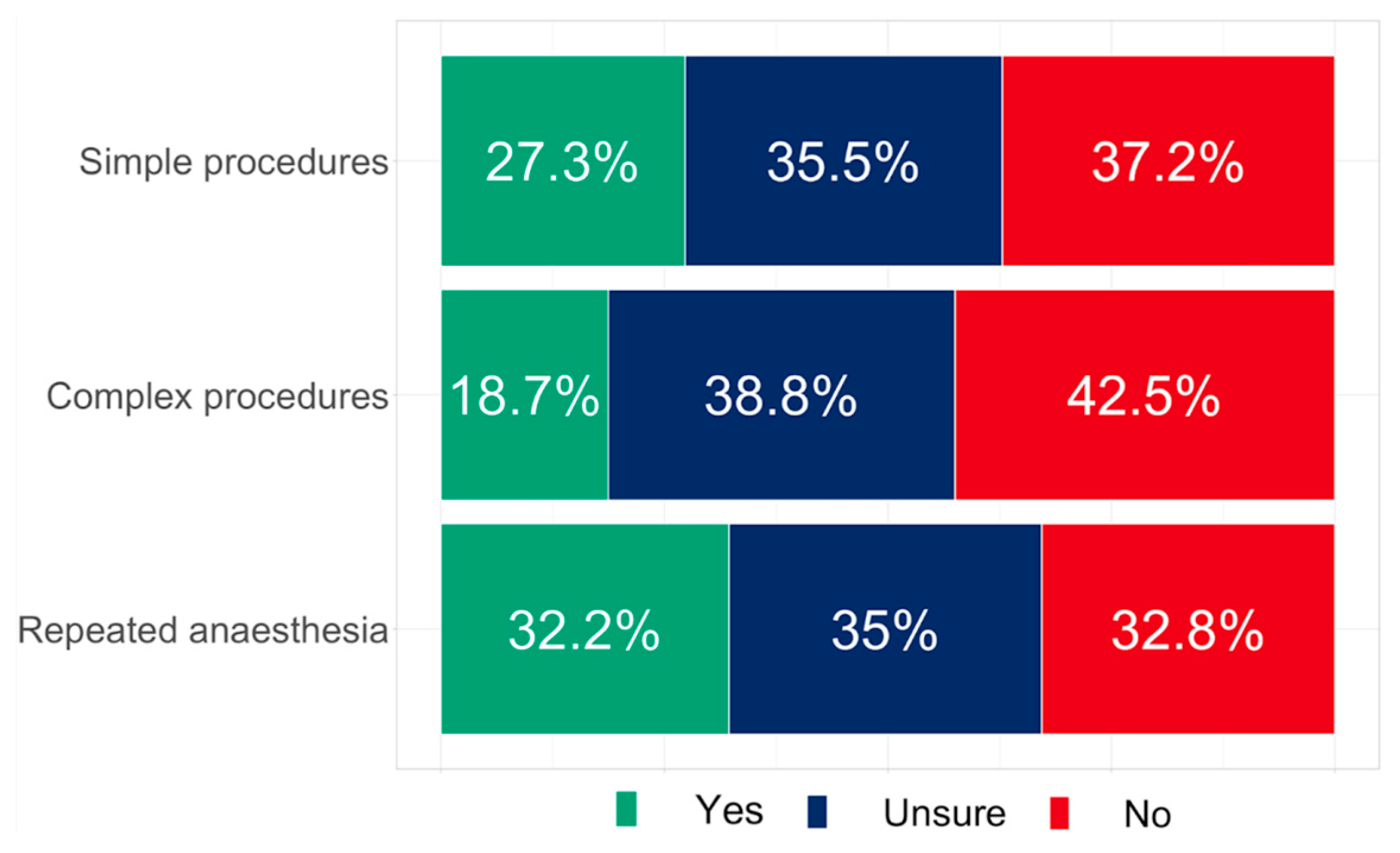
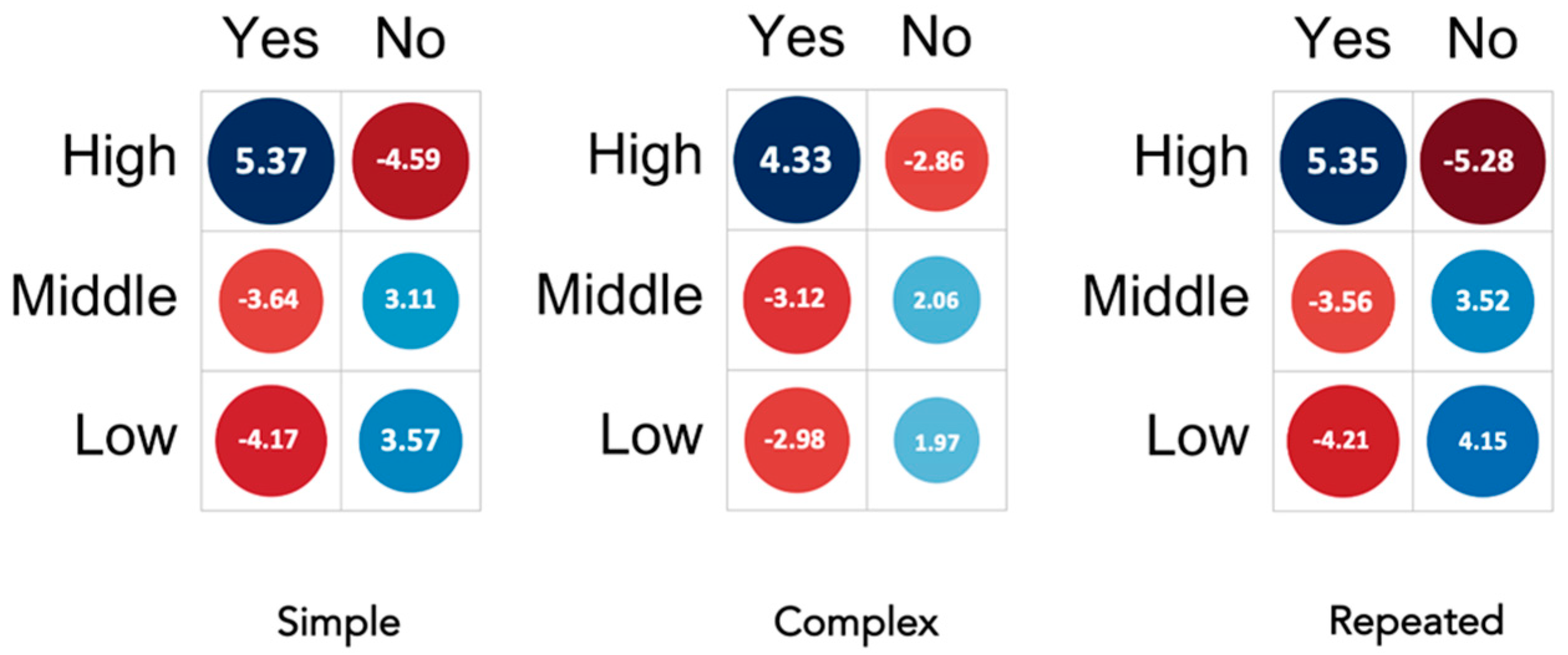
| Is an online telephone informed consent for elective surgery in accordance with the legal requirements in your country (simple) | p = <0.001 | ||
| Yes | No | ||
| High GDPPCPC | 164 (108) [5.37] | 92 (148) [−4.59] | |
| Middle GDPPCPC | 45 (77) [−3.64] | 137 (105) [3.11] | |
| Low GDPPCPC | 9 (32) [−4.17] | 69 (45) [3.57] | |
| Is an online telephone informed consent for elective surgery in accordance with the legal requirements in your country (complex) | p = <0.001 | ||
| Yes | No | ||
| High GDPPCPC | 110 (73) [4.33] | 130 (167) [−2.86] | |
| Middle GDPPCPC | 30 (53) [−3.12] | 143 (120) [2.06] | |
| Low GDPPCPC | 9 (23) [−2.98] | 68 (54) [1.97] | |
| Thinking of repeated anaesthesia, would an online telephone informed consent then be allowed for elective surgery due to legal requirements? | p = <0.001 | ||
| Yes | No | ||
| High GDPPCPC | 187 (127) [5.35] | 70 (130) [−5.28] | |
| Middle GDPPCPC | 54 (87) [−3.56] | 123 (90) [3.52] | |
| Low GDPPCPC | 14 (40) [−4.21] | 69 (42) [4.15] | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Neumann, C.; Straßberger-Nerschbach, N.; Delis, A.; Kamp, J.; Görtzen-Patin, A.; Cudian, D.; Fleischer, A.; Wietasch, G.; Coburn, M.; Schindler, E.; et al. Digital Online Patient Informed Consent for Anesthesia before Elective Surgery—Recent Practice in Europe. Healthcare 2023, 11, 1942. https://doi.org/10.3390/healthcare11131942
Neumann C, Straßberger-Nerschbach N, Delis A, Kamp J, Görtzen-Patin A, Cudian D, Fleischer A, Wietasch G, Coburn M, Schindler E, et al. Digital Online Patient Informed Consent for Anesthesia before Elective Surgery—Recent Practice in Europe. Healthcare. 2023; 11(13):1942. https://doi.org/10.3390/healthcare11131942
Chicago/Turabian StyleNeumann, Claudia, Nadine Straßberger-Nerschbach, Achilles Delis, Johannes Kamp, Alexandra Görtzen-Patin, Dishalen Cudian, Andreas Fleischer, Götz Wietasch, Mark Coburn, Ehrenfried Schindler, and et al. 2023. "Digital Online Patient Informed Consent for Anesthesia before Elective Surgery—Recent Practice in Europe" Healthcare 11, no. 13: 1942. https://doi.org/10.3390/healthcare11131942
APA StyleNeumann, C., Straßberger-Nerschbach, N., Delis, A., Kamp, J., Görtzen-Patin, A., Cudian, D., Fleischer, A., Wietasch, G., Coburn, M., Schindler, E., Schleifer, G., & Wittmann, M. (2023). Digital Online Patient Informed Consent for Anesthesia before Elective Surgery—Recent Practice in Europe. Healthcare, 11(13), 1942. https://doi.org/10.3390/healthcare11131942









