Breast Cancer Survivors’ Attitudes toward eMental Health: A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
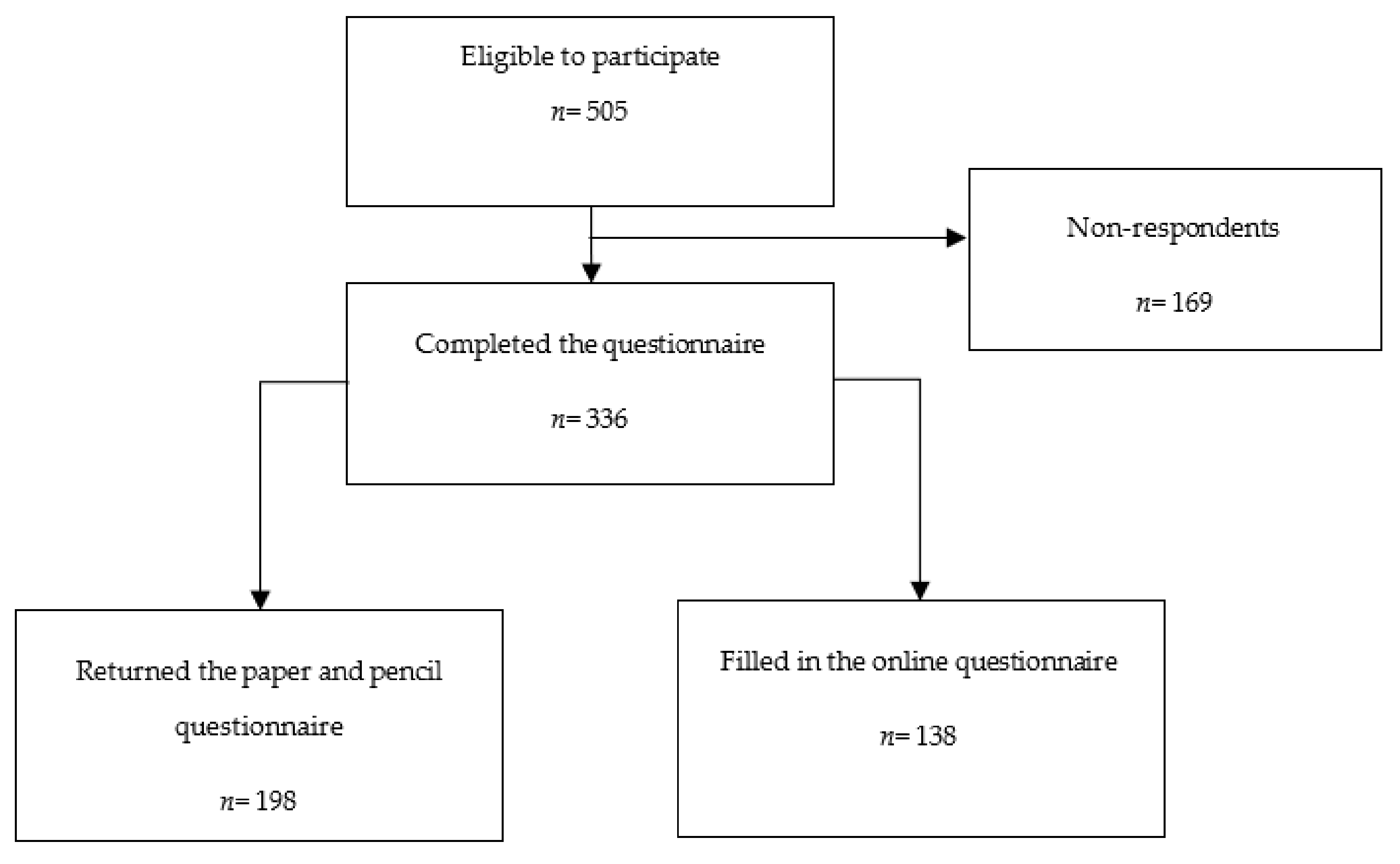
2.2. Procedures
2.3. Measures
2.3.1. Sociodemographic, Clinical, and Internet-Related Variables
2.3.2. Anxiety and Depression
2.3.3. HRQoL
2.3.4. Attitudes toward eMH
2.4. Analysis
3. Results
3.1. Participants’ Characteristics
3.2. Digital Technology Use and eMH Self-Reported Knowledge
3.3. BCS’ Attitudes toward eMH
3.4. Variables Associated with BCS’ Attitudes toward eMH
4. Discussion
4.1. Implications
4.2. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Global Cancer Observatory: Cancer Today. Lyon, France: International Agency for Research on Cancer. Available online: https://gco.iarc.fr/today/data/factsheets/populations/620-portugal-fact-sheets.pdf (accessed on 10 September 2021).
- Pilevarzadeh, M.; Amirshahi, M.; Afsargharehbagh, R.; Rafiemanesh, H.; Hashemi, S.-M.; Balouchi, A. Global prevalence of depression among breast cancer patients: A systematic review and meta-analysis. Breast Cancer Res. Treat. 2019, 176, 519–533. [Google Scholar] [CrossRef] [PubMed]
- Maass, S.W.M.C.; Roorda, C.; Berendsen, A.J.; Verhaak, P.F.M.; Bock, G.H. de The prevalence of long-term symptoms of depression and anxiety after breast cancer treatment: A systematic review. Maturitas 2015, 82, 100–108. [Google Scholar] [CrossRef] [PubMed]
- Mokhatri-Hesari, P.; Montazeri, A. Health-related quality of life in breast cancer patients: Review of reviews from 2008 to 2018. Health Qual. Life Outcomes 2020, 18, 338. [Google Scholar] [CrossRef] [PubMed]
- Guarino, A.; Polini, C.; Forte, G.; Favieri, F.; Boncompagni, I.; Casagrande, M. The Effectiveness of Psychological Treatments in Women with Breast Cancer: A Systematic Review and Meta-Analysis. J. Clin. Med. 2020, 9, 209. [Google Scholar] [CrossRef]
- Pham, Q.; Hearn, J.; Gao, B.; Brown, I.; Hamilton, R.J.; Berlin, A.; Cafazzo, J.A.; Feifer, A. Virtual care models for cancer survivorship. NPJ Digit. Med. 2020, 3, 113. [Google Scholar] [CrossRef]
- Riper, H.; Andersson, G.; Christensen, H.; Cuijpers, P.; Lange, A.; Eysenbach, G. Theme Issue on E-Mental Health: A Growing Field in Internet Research. J. Med. Internet Res. 2010, 12, e74. [Google Scholar] [CrossRef]
- Andersson, G.; Titov, N. Advantages and limitations of Internet-based interventions for common mental disorders. World Psychiatry 2014, 13, 4–11. [Google Scholar] [CrossRef]
- Sasseville, M.; LeBlanc, A.; Boucher, M.; Dugas, M.; Mbemba, G.; Tchuente, J.; Chouinard, M.-C.; Beaulieu, M.; Beaudet, N.; Skidmore, B.; et al. Digital health interventions for the management of mental health in people with chronic diseases: A rapid review. BMJ Open 2021, 11, e044437. [Google Scholar] [CrossRef]
- Donker, T.; Blankers, M.; Hedman, E.; Ljótsson, B.; Petrie, K.; Christensen, H. Economic evaluations of Internet interventions for mental health: A systematic review. Psychol. Med. 2015, 45, 3357–3376. [Google Scholar] [CrossRef]
- Van der Hout, A.; Jansen, F.; van Uden-Kraan, C.F.; Coupé, V.M.; Holtmaat, K.; Nieuwenhuijzen, G.A.; Hardillo, J.A.; de Jong, R.J.B.; Tiren-Verbeet, N.L.; Sommeijer, D.W.; et al. Cost-utility of an eHealth application “Oncokompas” that supports cancer survivors in self-management: Results of a randomised controlled trial. J. Cancer Surviv. 2021, 15, 77–86. [Google Scholar] [CrossRef]
- Post, K.E.; Flanagan, J. Web based survivorship interventions for women with breast cancer: An integrative review. Eur. J. Oncol. Nurs. 2016, 25, 90–99. [Google Scholar] [CrossRef]
- Chen, Y.-Y.; Guan, B.-S.; Li, Z.-K.; Li, X.-Y. Effect of telehealth intervention on breast cancer patients’ quality of life and psychological outcomes: A meta-analysis. J. Telemed. Telecare 2018, 24, 157–167. [Google Scholar] [CrossRef]
- Triberti, S.; Savioni, L.; Sebri, V.; Pravettoni, G. eHealth for improving quality of life in breast cancer patients: A systematic review. Cancer Treat. Rev. 2019, 74, 1–14. [Google Scholar] [CrossRef]
- Hauffman, A.; Alfonsson, S.; Bill-Axelson, A.; Bergkvist, L.; Forslund, M.; Mattsson, S.; Essen, L.; Nygren, P.; Igelström, H.; Johansson, B. Cocreated internet-based stepped care for individuals with cancer and concurrent symptoms of anxiety and depression: Results from the U-CARE AdultCan randomized controlled trial. Psycho-Oncology 2020, 29, 2012–2018. [Google Scholar] [CrossRef]
- Nissen, E.R.; O’Connor, M.; Kaldo, V.; Højris, I.; Borre, M.; Zachariae, R.; Mehlsen, M. Internet-delivered mindfulness-based cognitive therapy for anxiety and depression in cancer survivors: A randomized controlled trial. Psycho-Oncology 2020, 29, 68–75. [Google Scholar] [CrossRef]
- Lally, R.M.; Kupzyk, K.A.; Bellavia, G.; Hydeman, J.; Gallo, S.; Helgeson, V.S.; Erwin, D.; Mills, A.C.; Brown, J.K. CaringGuidanceTM after breast cancer diagnosis eHealth psychoeducational intervention to reduce early post-diagnosis distress. Support. Care Cancer 2020, 28, 2163–2174. [Google Scholar] [CrossRef]
- Wagner, L.I.; Tooze, J.A.; Hall, D.L.; Levine, B.J.; Beaumont, J.; Duffecy, J.; Victorson, D.; Gradishar, W.; Leach, J.; Saphner, T.; et al. Targeted eHealth Intervention to Reduce Breast Cancer Survivors’ Fear of Recurrence: Results From the FoRtitude Randomized Trial. J. Natl. Cancer Inst. 2021, 113, 1495–1505. [Google Scholar] [CrossRef]
- Zachariae, R.; Amidi, A.; Damholdt, M.F.; Clausen, C.D.R.; Dahlgaard, J.; Lord, H.; Thorndike, F.P.; Ritterband, L.M. Internet-Delivered Cognitive-Behavioral Therapy for Insomnia in Breast Cancer Survivors: A Randomized Controlled Trial. J. Natl. Cancer Inst. 2018, 110, 880–887. [Google Scholar] [CrossRef]
- Atema, V.; van Leeuwen, M.; Kieffer, J.M.; Oldenburg, H.S.A.; van Beurden, M.; Gerritsma, M.A.; Kuenen, M.A.; Plaisier, P.W.; Cardozo, A.M.F.L.; van Riet, Y.E.A.; et al. Efficacy of Internet-Based Cognitive Behavioral Therapy for Treatment-Induced Menopausal Symptoms in Breast Cancer Survivors: Results of a Randomized Controlled Trial. J. Clin. Oncol. 2019, 37, 809–822. [Google Scholar] [CrossRef]
- Hummel, S.B.; van Lankveld, J.J.D.M.; Oldenburg, H.S.A.; Hahn, D.E.E.; Kieffer, J.M.; Gerritsma, M.A.; Kuenen, M.A.; Bijker, N.; Borgstein, P.J.; Heuff, G.; et al. Internet-Based Cognitive Behavioral Therapy Realizes Long-Term Improvement in the Sexual Functioning and Body Image of Breast Cancer Survivors. J. Sex Marital Ther. 2018, 44, 485–496. [Google Scholar] [CrossRef] [PubMed]
- Børøsund, E.; Ehlers, S.L.; Varsi, C.; Clark, M.M.; Andrykowski, M.A.; Cvancarova, M.; Nes, L.S. Results from a randomized controlled trial testing StressProffen; an application-based stress-management intervention for cancer survivors. Cancer Med. 2020, 9, 3775–3785. [Google Scholar] [CrossRef] [PubMed]
- Holtdirk, F.; Mehnert, A.; Weiss, M.; Mayer, J.; Meyer, B.; Bröde, P.; Claus, M.; Watzl, C. Results of the Optimune trial: A randomized controlled trial evaluating a novel Internet intervention for breast cancer survivors. PLoS ONE 2021, 16, e0251276. [Google Scholar] [CrossRef] [PubMed]
- Bradbury, K.; Steele, M.; Corbett, T.; Geraghty, A.W.A.; Krusche, A.; Heber, E.; Easton, S.; Cheetham-Blake, T.; Slodkowska-Barabasz, J.; Müller, A.M.; et al. Developing a digital intervention for cancer survivors: An evidence-, theory- and person-based approach. NPJ Digit. Med. 2019, 2, 85. [Google Scholar] [CrossRef] [PubMed]
- Corbett, T.; Singh, K.; Payne, L.; Bradbury, K.; Foster, C.; Watson, E.; Richardson, A.; Little, P.; Yardley, L. Understanding acceptability of and engagement with Web-based interventions aiming to improve quality of life in cancer survivors: A synthesis of current research. Psycho-Oncology 2018, 27, 22–33. [Google Scholar] [CrossRef]
- Davies, F.; Shepherd, H.L.; Beatty, L.; Clark, B.; Butow, P.; Shaw, J. Implementing Web-Based Therapy in Routine Mental Health Care: Systematic Review of Health Professionals’ Perspectives. J. Med. Internet Res. 2020, 22, e17362. [Google Scholar] [CrossRef]
- Schuster, R.; Pokorny, R.; Berger, T.; Topooco, N.; Laireiter, A.-R. The Advantages and Disadvantages of Online and Blended Therapy: Survey Study Amongst Licensed Psychotherapists in Austria. J. Med. Internet Res. 2018, 20, e11007. [Google Scholar] [CrossRef]
- Durosini, I.; Triberti, S.; Pravettoni, G. Breast Cancer Survivors’ Attitudes Towards Internet-Based Psychotherapy. Annu. Rev. Cyberther. Telemed. 2020, 2020, 201. [Google Scholar]
- Im, E.-O.; Kim, S.; Jang, M.; Chee, W. Attitudes toward Technology-Based Cancer Support Programs Among Korean American Breast Cancer Survivors. West. J. Nurs. Res. 2020, 43, 732–741. [Google Scholar] [CrossRef]
- Yun, Y.H.; Lee, K.S.; Kim, Y.-W.; Park, S.Y.; Lee, E.S.; Noh, D.-Y.; Kim, S.; Oh, J.H.; Jung, S.Y.; Chung, K.-W.; et al. Web-based tailored education program for disease-free cancer survivors with cancer-related fatigue: A randomized controlled trial. J. Clin. Oncol. 2012, 30, 1296–1303. [Google Scholar] [CrossRef]
- Lee, M.K.; Yun, Y.H.; Park, H.-A.; Lee, E.S.; Jung, K.H.; Noh, D.-Y. A Web-based self-management exercise and diet intervention for breast cancer survivors: Pilot randomized controlled trial. Int. J. Nurs. Stud. 2014, 51, 1557–1567. [Google Scholar] [CrossRef]
- Bantum, E.O.; Albright, C.L.; White, K.K.; Berenberg, J.L.; Layi, G.; Ritter, P.L.; Laurent, D.; Plant, K.; Lorig, K. Surviving and Thriving With Cancer Using a Web-Based Health Behavior Change Intervention: Randomized Controlled Trial. J. Med. Internet Res. 2014, 16, e54. [Google Scholar] [CrossRef] [PubMed]
- Myall, M.; May, C.R.; Grimmett, C.; May, C.M.; Calman, L.; Richardson, A.; Foster, C.L. RESTORE: An exploratory trial of a web-based intervention to enhance self-management of cancer-related fatigue: Findings from a qualitative process evaluation. BMC Med. Inf. Decis. Mak. 2015, 15, 94. [Google Scholar] [CrossRef] [PubMed]
- Pauwels, E.; Van Hoof, E.; Charlier, C.; Lechner, L.; De Bourdeaudhuij, I. Design and process evaluation of an informative website tailored to breast cancer survivors’ and intimate partners’ post-treatment care needs. BMC Res. Notes 2012, 5, 548. [Google Scholar] [CrossRef]
- Song, L.; Rini, C.; Deal, A.M.; Nielsen, M.E.; Chang, H.; Kinneer, P.; Teal, R.; Johnson, D.C.; Dunn, M.W.; Mark, B.; et al. Improving couples’ quality of life through a Web-based prostate cancer education intervention. Oncol. Nurs. Forum 2015, 42, 183–192. [Google Scholar] [CrossRef]
- Wallin, E.E.K.; Mattsson, S.; Olsson, E.M.G. The Preference for Internet-Based Psychological Interventions by Individuals Without Past or Current Use of Mental Health Treatment Delivered Online: A Survey Study With Mixed-Methods Analysis. JMIR Ment. Health 2016, 3, e25. [Google Scholar] [CrossRef]
- Kanera, I.M.; Bolman, C.A.W.; Willems, R.A.; Mesters, I.; Lechner, L. Lifestyle-related effects of the web-based Kanker Nazorg Wijzer (Cancer Aftercare Guide) intervention for cancer survivors: A randomized controlled trial. J. Cancer Surviv. 2016, 10, 883–897. [Google Scholar] [CrossRef]
- Van der Hout, A.; van Uden-Kraan, C.; Holtmaat, K.; Jansen, F.; Lissenberg-Witte, B.; Nieuwenhuijzen, G.; Hardillo, J.; de Jong, R.B.; Tiren-Verbeet, N.; Sommeijer, D.; et al. Reasons for not reaching or using web-based self-management applications, and the use and evaluation of Oncokompas among cancer survivors, in the context of a randomised controlled trial. Internet Interv. 2021, 25, 100429. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P.; STROBE Initiative. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. BMJ 2007, 335, 806–808. [Google Scholar] [CrossRef]
- Vlaescu, G.; Alasjö, A.; Miloff, A.; Carlbring, P.; Andersson, G. Features and functionality of the Iterapi platform for internet-based psychological treatment. Internet Interv. 2016, 6, 107–114. [Google Scholar] [CrossRef]
- Sousa, T.V.; Viveiros, V.; Chai, M.V.; Vicente, F.L.; Jesus, G.; Carnot, M.J.; Gordo, A.C.; Ferreira, P.L. Reliability and validity of the Portuguese version of the Generalized Anxiety Disorder (GAD-7) scale. Health Qual. Life Outcomes 2015, 13, 50. [Google Scholar] [CrossRef]
- Torres, A.; Monteiro, S.; Pereira, A.; Albuquerque, E. Reliability and Validity of the PHQ-9 in Portuguese Women with Breast Cancer. Eur. Proc. Soc. Behav. Sci. 2016, 411–423. [Google Scholar] [CrossRef]
- Pais-Ribeiro, J.; Pinto, C.; Santos, C. Validation study of the portuguese version of the QLC-C30-V.3. Psicol. Saúde Doenças 2008, 9, 89–102. [Google Scholar]
- Sprangers, M.A.; Groenvold, M.; Arraras, J.I.; Franklin, J.; te Velde, A.; Muller, M.; Franzini, L.; Williams, A.; de Haes, H.C.; Hopwood, P.; et al. The European Organization for Research and Treatment of Cancer breast cancer-specific quality-of-life questionnaire module: First results from a three-country field study. J. Clin. Oncol. 1996, 14, 2756–2768. [Google Scholar] [CrossRef]
- Mendes-Santos, C.; Weiderpass, E.; Santana, R.; Andersson, G. Portuguese Psychologists’ Attitudes Toward Internet Interventions: Exploratory Cross-Sectional Study. JMIR Ment. Health 2020, 7, e16817. [Google Scholar] [CrossRef]
- Knauper, B. The Impact of Age and Education on Response Order Effects in Attitude Measurement. Public Opin. Q. 1999, 63, 347–370. [Google Scholar] [CrossRef]
- Apolinário-Hagen, J.; Harrer, M.; Kählke, F.; Fritsche, L.; Salewski, C.; Ebert, D.D. Public Attitudes Toward Guided Internet-Based Therapies: Web-Based Survey Study. JMIR Ment. Health 2018, 5, e10735. [Google Scholar] [CrossRef]
- Apolinário-Hagen, J.; Hennemann, S.; Fritsche, L.; Drüge, M.; Breil, B. Determinant Factors of Public Acceptance of Stress Management Apps: Survey Study. JMIR Ment. Health 2019, 6, e15373. [Google Scholar] [CrossRef]
- Yao, X.-Y.; Li, Z.; Arthur, D.; Hu, L.-L.; Cheng, G. The feasibility of an internet-based intervention for Chinese people with mental illness: A survey of willingness and attitude. Int. J. Nurs. Sci. 2014, 1, 28–33. [Google Scholar] [CrossRef][Green Version]
- Hennemann, S.; Beutel, M.E.; Zwerenz, R. Drivers and Barriers to Acceptance of Web-Based Aftercare of Patients in Inpatient Routine Care: A Cross-Sectional Survey. J. Med. Internet Res. 2016, 18, e337. [Google Scholar] [CrossRef]
- Lipschitz, J.; Miller, C.J.; Hogan, T.P.; Burdick, K.E.; Lippin-Foster, R.; Simon, S.R.; Burgess, J. Adoption of Mobile Apps for Depression and Anxiety: Cross-Sectional Survey Study on Patient Interest and Barriers to Engagement. JMIR Ment. Health 2019, 6, e11334. [Google Scholar] [CrossRef] [PubMed]
- Berry, N.; Lobban, F.; Emsley, R.; Bucci, S. Acceptability of Interventions Delivered Online and Through Mobile Phones for People Who Experience Severe Mental Health Problems: A Systematic Review. J. Med. Internet Res. 2016, 18, e121. [Google Scholar] [CrossRef] [PubMed]
- Schröder, J.; Berger, T.; Meyer, B.; Lutz, W.; Hautzinger, M.; Späth, C.; Eichenberg, C.; Klein, J.P.; Moritz, S. Attitudes Towards Internet Interventions Among Psychotherapists and Individuals with Mild to Moderate Depression Symptoms. Cogn. Ther. Res. 2017, 41, 745–756. [Google Scholar] [CrossRef]
- Drewes, C.; Kirkovits, T.; Schiltz, D.; Schinkoethe, T.; Haidinger, R.; Goldmann-Posch, U.; Harbeck, N.; Wuerstlein, R. EHealth Acceptance and New Media Preferences for Therapy Assistance Among Breast Cancer Patients. JMIR Cancer 2016, 2, e13. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Y.; West, B.T.; Barton, D.L.; Harris, M.R. Acceptance and Use of eHealth/mHealth Applications for Self-Management Among Cancer Survivors. Stud. Health Technol. Inf. 2017, 245, 131–135. [Google Scholar]
- Jansen, F.; van Uden-Kraan, C.F.; van Zwieten, V.; Witte, B.I.; Verdonck-de Leeuw, I.M. Cancer survivors’ perceived need for supportive care and their attitude towards self-management and eHealth. Support Care Cancer 2015, 23, 1679–1688. [Google Scholar] [CrossRef]
- Musiat, P.; Goldstone, P.; Tarrier, N. Understanding the acceptability of e-mental health—Attitudes and expectations towards computerised self-help treatments for mental health problems. BMC Psychiatry 2014, 14, 109. [Google Scholar] [CrossRef]
- Apolinário-Hagen, J.; Vehreschild, V.; Alkoudmani, R.M. Current Views and Perspectives on E-Mental Health: An Exploratory Survey Study for Understanding Public Attitudes Toward Internet-Based Psychotherapy in Germany. JMIR Ment. Health 2017, 4, e8. [Google Scholar] [CrossRef]
- Eichenberg, C.; Wolters, C.; Brähler, E. The Internet as a Mental Health Advisor in Germany—Results of a National Survey. PLoS ONE 2013, 8, e79206. [Google Scholar] [CrossRef]
- Watson, D.; Clark, L.A.; Carey, G. Positive and negative affectivity and their relation to anxiety and depressive disorders. J. Abnorm. Psychol. 1988, 97, 346–353. [Google Scholar] [CrossRef]
- Klein, B.; Cook, S. Preferences for e-mental health services amongst an online Australian sample. E J. Appl. Psychol. 2010, 6, 28–39. [Google Scholar] [CrossRef]
- Choi, I.; Sharpe, L.; Li, S.; Hunt, C. Acceptability of psychological treatment to Chinese- and Caucasian-Australians: Internet treatment reduces barriers but face-to-face care is preferred. Soc. Psychiatry Psychiatr. Epidemiol. 2015, 50, 77–87. [Google Scholar] [CrossRef]
- Gun, S.Y.; Titov, N.; Andrews, G. Acceptability of Internet treatment of anxiety and depression. Australas. Psychiatry 2011, 19, 259–264. [Google Scholar] [CrossRef]
- March, S.; Day, J.; Ritchie, G.; Rowe, A.; Gough, J.; Hall, T.; Yuen, C.Y.J.; Donovan, C.L.; Ireland, M. Attitudes Toward e-Mental Health Services in a Community Sample of Adults: Online Survey. J. Med. Internet Res. 2018, 20, e59. [Google Scholar] [CrossRef]
- Apolinário-Hagen, J.; Fritsche, L.; Bierhals, C.; Salewski, C. Improving attitudes toward e-mental health services in the general population via psychoeducational information material: A randomized controlled trial. Internet Interv. 2018, 12, 141–149. [Google Scholar] [CrossRef]
- Casey, L.M.; Joy, A.; Clough, B.A. The Impact of Information on Attitudes Toward E-Mental Health Services. Cyberpsychol. Behav. Soc. Netw. 2013, 16, 593–598. [Google Scholar] [CrossRef]
- Ebert, D.D.; Berking, M.; Cuijpers, P.; Lehr, D.; Pörtner, M.; Baumeister, H. Increasing the acceptance of internet-based mental health interventions in primary care patients with depressive symptoms. A randomized controlled trial. J. Affect. Disord. 2015, 176, 9–17. [Google Scholar] [CrossRef]
- Baumeister, H.; Nowoczin, L.; Lin, J.; Seifferth, H.; Seufert, J.; Laubner, K.; Ebert, D.D. Impact of an acceptance facilitating intervention on diabetes patients’ acceptance of Internet-based interventions for depression: A randomized controlled trial. Diabetes Res. Clin. Pract. 2014, 105, 30–39. [Google Scholar] [CrossRef]
- Hair, J.F.; Black, W.; Babin, B.; Anderson, R. Multivariate Data Analysis; Pearson Higher Education: Victoria, BC, Canada, 2014; ISBN 1-292-02190-X. [Google Scholar]
- Schröder, J.; Sautier, L.; Kriston, L.; Berger, T.; Meyer, B.; Späth, C.; Köther, U.; Nestoriuc, Y.; Klein, J.P.; Moritz, S. Development of a questionnaire measuring Attitudes towards Psychological Online Interventions-the APOI. J. Affect. Disord. 2015, 187, 136–141. [Google Scholar] [CrossRef]
- Ajzen, I. Nature and operation of attitudes. Annu Rev Psychol. 2001, 52, 27–58. [Google Scholar] [CrossRef]
- Barak, A.; Klein, B.; Proudfoot, J.G. Defining internet-supported therapeutic interventions. Ann Behav Med. 2009, 38, 4–17. [Google Scholar] [CrossRef] [PubMed]
- Pituch, K.; Stevens, J. Applied Multivariate Statistics for the Social Sciences: Analyses with SAS and IBM’s SPSS, Sixth Edition, Routledge. 2016. Available online: https://www.routledge.com/Applied-Multivariate-Statistics-for-the-Social-Sciences-Analyses-with-SAS/Pituch-Stevens/p/book/9780415836661 (accessed on 4 March 2021).
- SPSS for Windows Step by Step: A Simple Guide and Reference, 11.0 Update - Darren George, Paul Mallery-Google Livros, (n.d.). Available online: https://books.google.pt/books/about/SPSS_for_Windows_Step_by_Step.html?id=AghHAAAAMAAJ&redir_esc=y (accessed on 8 March 2021).
| Variables | ||
|---|---|---|
| Education, n (%) | ||
| No education | 2 (1) | |
| 4–6 school years | 109 (32) | |
| 9 school years | 66 (20) | |
| 12 school years | 78 (23) | |
| University degree | 81 (24) | |
| Marital status, n (%) | ||
| Single | 38 (11) | |
| Married/de facto relationship | 225 (67) | |
| Divorced/Separated | 43 (13) | |
| Widowed | 30 (9) | |
| Employment status, n (%) | ||
| Unemployed | 52 (16) | |
| Active | 107 (32) | |
| Sick leave | 94 (28.) | |
| Retired | 83 (25) | |
| Surgery, n (%) | ||
| Not performed | 68 (21) | |
| Lumpectomy | 156 (49) | |
| Mastectomy | 95 (29) | |
| Missing | 17 | |
| Chemo/Radiotherapy, n (%) | ||
| Not performed | 74 (23) | |
| Chemo and radiotherapy | 120 (38) | |
| Only chemotherapy | 87 (27) | |
| Only radiotherapy | 38 (12) | |
| Missing | 17 | |
| Hormone therapy, n (%) | ||
| Yes | 172 (54) | |
| No | 147 (46) | |
| Missing | 17 | |
| Immunotherapy, n (%) | ||
| Yes | 82 (25) | |
| No | 237 (74) | |
| Missing | 17 | |
| Disease staging, n (%) | ||
| 0 | 12 (4) | |
| I | 100 (32) | |
| II | 79 (25) | |
| III | 72 (23) | |
| IV | 34 (11) | |
| Under determination | 17 (5) | |
| Missing | 22 | |
| ECOG, n (%) | ||
| 0 | 198 (80) | |
| 1 | 42 (17) | |
| 2 | 8 (3) | |
| 3 | 1 (0) | |
| Missing | 87 | |
| PHQ-9, Median (IQR) 1,2 | 7.0 (8) | |
| GAD-7, Median (IQR) 1,3 | 6.0 (7) | |
| QLQ30, Median (IQR) 1,4 | ||
| Global Health Status | 50 (33) | |
| Functional scales | ||
| Physical Functioning | 73 (27) | |
| Role Functioning | 67 (50) | |
| Emotional Functioning | 67 (33) | |
| Cognitive Functioning | 83 (33) | |
| Social Functioning | 67 (33) | |
| Symptoms scales | ||
| Fatigue | 33 (33) | |
| Nausea and Vomiting | 0.0 (17) | |
| Pain | 33 (50) | |
| Single-item symptoms measures | ||
| Dyspnea | 0 (33) | |
| Insomnia | 33 (67) | |
| Appetite loss | 0.0 (33) | |
| Constipation | 0.0 (33) | |
| Diarrhea | 0.0 (33) | |
| Financial Difficulties | 33 (33) | |
| QLQBR23, Median (IQR) 1,5 | ||
| Functional scales | 83 (42) | |
| Body Image | 17 (33) | |
| Sexual Functioning | ||
| Symptoms scales | ||
| Systemic Therapy Side Effects | 19 (24) | |
| Breast Symptoms | 8 (25) | |
| Arm Symptoms | 22 (33) | |
| Single-items measures | ||
| Sexual Enjoyment | 0 (33) | |
| Future Perspective | 33 (67) | |
| Upset by Hair Loss | 0 (0) |
| ATIIS Score | Chi-Square Results | |||||
|---|---|---|---|---|---|---|
| Quartile 1 (≤37.49) | Quartile 2 (37.50–49.99) | Quartile 3 (50.00–60.93) | Quartile 4 (≥60.94) | p Value | Chi-Square | |
| Formal education | 0.000 | χ2 12 = 38.41 | ||||
| No degree | 1 (0.9) | 0 (−0.7) | 1 (0.6) | 0 (−0.9) | ||
| 1st/2nd cycles (4–6 school years) | 33 (1.9) | 26 (1.8) | 39 (1.3) | 11 (−4.8) | ||
| 3rd cycle (9 school years) | 13 (−0.9) | 11 (−0.4) | 26 (1.7) | 16 (−0.5) | ||
| Secondary (12 school years) | 20 (0.4) | 13 (−0.5) | 20 (−1.2) | 25 (1.2) | ||
| Tertiary (University degree) | 13 (−1.9) | 12 (−1.0) | 18 (−2.0) | 38 (4.7) | ||
| Psychiatric history | 0.023 | χ2 3 = 9.56 | ||||
| No | 41 (−1.1) | 44 (2.1) | 63 (1.3) | 44 (−2.2) | ||
| Yes | 34 (1.1) | 17 (−2.1) | 33 (−1.3) | 44 (2.2) | ||
| Internet access | 0.001 | χ2 3 = 15.74 | ||||
| No | 23 (1.7) | 13 (−0.2) | 30 (2.1) | 7 (−3.8) | ||
| Yes | 57 (−1.7) | 49 (0.2) | 74 (−2.1) | 83 (3.8) | ||
| Internet use frequency | 0.001 | χ2 12 = 33.11 | ||||
| Never | 25 (1.8) | 20 (1.7) | 29 (1.2) | 6 (−4.5) | ||
| Once a week or less | 6 (1.3) | 2 (−0.6) | 5 (0) | 3 (−0.7) | ||
| 2–3 times a week | 5 (−0.2) | 3 (−0.7) | 9 (0.9) | 6 (−0.1) | ||
| Daily, at least once a day | 24 (−0.6) | 22 (0.5) | 35 (0.2) | 29 (−0.1) | ||
| Daily, several times a day | 20 (−1.5) | 15 (−1.4) | 26 (−1.8) | 46 (4.6) | ||
| Social networks use | 0.000 | χ2 3 = 34.77 | ||||
| No | 39 (3.0) | 27 (1.6) | 42 (1.4) | 9 (−5.8) | ||
| Yes | 41 (−3.0) | 35 (−1.6) | 62 (−1.4) | 81 (5.8) | ||
| Online health information seeking 1 | 0.000 | χ2 3 = 29.93 | ||||
| No | 41 (3.5) | 27 (1.6) | 37 (0.2) | 12 (−5.0) | ||
| Yes | 39 (−3.5) | 35 (−1.6) | 67 (−0.2) | 78 (5.0) | ||
| Online mental healthcare seeking 2 | 0.000 | χ2 3 = 21.43 | ||||
| No | 77 (1.5) | 60 (1.5) | 100 (1.8) | 73 (−4.6) | ||
| Yes | 3 (−1.5) | 2 (−1.5) | 4 (−1.8) | 17 (4.6) | ||
| Remote healthcare use 3 | 0.011 | χ2 3 = 11.07 | ||||
| No | 70 (1.4) | 51 (0.0) | 91 (1.7) | 64 (−3.2) | ||
| Yes | 10 (−1.4) | 11 (0.0) | 13 (−1.7) | 26 (3.2) | ||
| eMH Self-reported knowledge 4 | 0.000 | χ2 12 = 80.53 | ||||
| Completely disagree | 36 (3.9) | 18 (0.2) | 20 (−2.4) | 20 (−1.4) | ||
| Moderately disagree | 6 (−0.3) | 5 (−0.1) | 9 (0.1) | 8 (0.2) | ||
| Neither agree nor disagree | 32 (0.5) | 29 (1.7) | 50 (2.7) | 15 (−4.8) | ||
| Moderately agree | 5 (−2.9) | 8 (−0.9) | 21 (1.2) | 22 (2.3) | ||
| Completely agree | 1 (−2.9) | 2 (−1.9) | 4 (−2.4) | 25 (6.9) | ||
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 | Model 7 | Model 8 | Model 9 | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | B | SE B | β | B | SE B | β | B | SE B | β | B | SE B | β | B | SE B | β | B | SE B | β | B | SE B | β | B | SE B | β | B | SE B | β |
| PHQ-9 | 0.38 | 0.19 | 0.11 * | ||||||||||||||||||||||||
| Emotional functioning | −0.10 | 0.04 | −0.13 * | ||||||||||||||||||||||||
| Cognitive functioning | −0.10 | 0.04 | −0.14 * | ||||||||||||||||||||||||
| Body image | −0.12 | 0.04 | −0.17 ** | ||||||||||||||||||||||||
| Social networks | 9.12 | 2.75 | 0.21 ** | ||||||||||||||||||||||||
| Online health information seeking 1 | 10.33 | 2.85 | 0.24 ** | ||||||||||||||||||||||||
| Online mental healthcare seeking 2 | 13.79 | 4.14 | 0.18 ** | ||||||||||||||||||||||||
| Previous use of remote healthcare 3 | 5.71 | 2.86 | 0.11 * | ||||||||||||||||||||||||
| 0 vs. eMH self-reported knowledge (Moderately Disagree) 4 | 5.61 | 3.99 | 0.08 | ||||||||||||||||||||||||
| 0 vs. eMH self-reported knowledge (Neither Agree nor Disagree) 4 | 1.34 | 2.50 | 0.03 | ||||||||||||||||||||||||
| 0 vs. eMH self-reported knowledge (Moderately Agree) 4 | 13.43 | 3.14 | 0.24 ** | ||||||||||||||||||||||||
| 0 vs. eMH self-reported knowledge (Totally Agree) 4 | 28.70 | 3.87 | 0.41 ** | ||||||||||||||||||||||||
| R2 | 0.08 | 0.09 | 0.09 | 0.10 | 0.10 | 0.11 | 0.10 | 0.08 | 0.24 | ||||||||||||||||||
| F for change in R2 | 5.02 (6329) ** | 5.39 (6324) ** | 5.49 (6324) ** | 6.11 (6317) ** | 6.24 (6329) ** | 6.63 (6329) ** | 6.26 (6329) ** | 4.98 (6329) ** | 11.48 (9326) ** | ||||||||||||||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mendes-Santos, C.; Campos, T.; Ferreira, D.; Weiderpass, E.; Santana, R.; Andersson, G. Breast Cancer Survivors’ Attitudes toward eMental Health: A Cross-Sectional Study. Healthcare 2023, 11, 1920. https://doi.org/10.3390/healthcare11131920
Mendes-Santos C, Campos T, Ferreira D, Weiderpass E, Santana R, Andersson G. Breast Cancer Survivors’ Attitudes toward eMental Health: A Cross-Sectional Study. Healthcare. 2023; 11(13):1920. https://doi.org/10.3390/healthcare11131920
Chicago/Turabian StyleMendes-Santos, Cristina, Teresa Campos, Diana Ferreira, Elisabete Weiderpass, Rui Santana, and Gerhard Andersson. 2023. "Breast Cancer Survivors’ Attitudes toward eMental Health: A Cross-Sectional Study" Healthcare 11, no. 13: 1920. https://doi.org/10.3390/healthcare11131920
APA StyleMendes-Santos, C., Campos, T., Ferreira, D., Weiderpass, E., Santana, R., & Andersson, G. (2023). Breast Cancer Survivors’ Attitudes toward eMental Health: A Cross-Sectional Study. Healthcare, 11(13), 1920. https://doi.org/10.3390/healthcare11131920






