Performance of the Malmgren Index for Assessing Root Resorption on 2D vs. 3D Radiographs: A Pilot Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Sample Selection
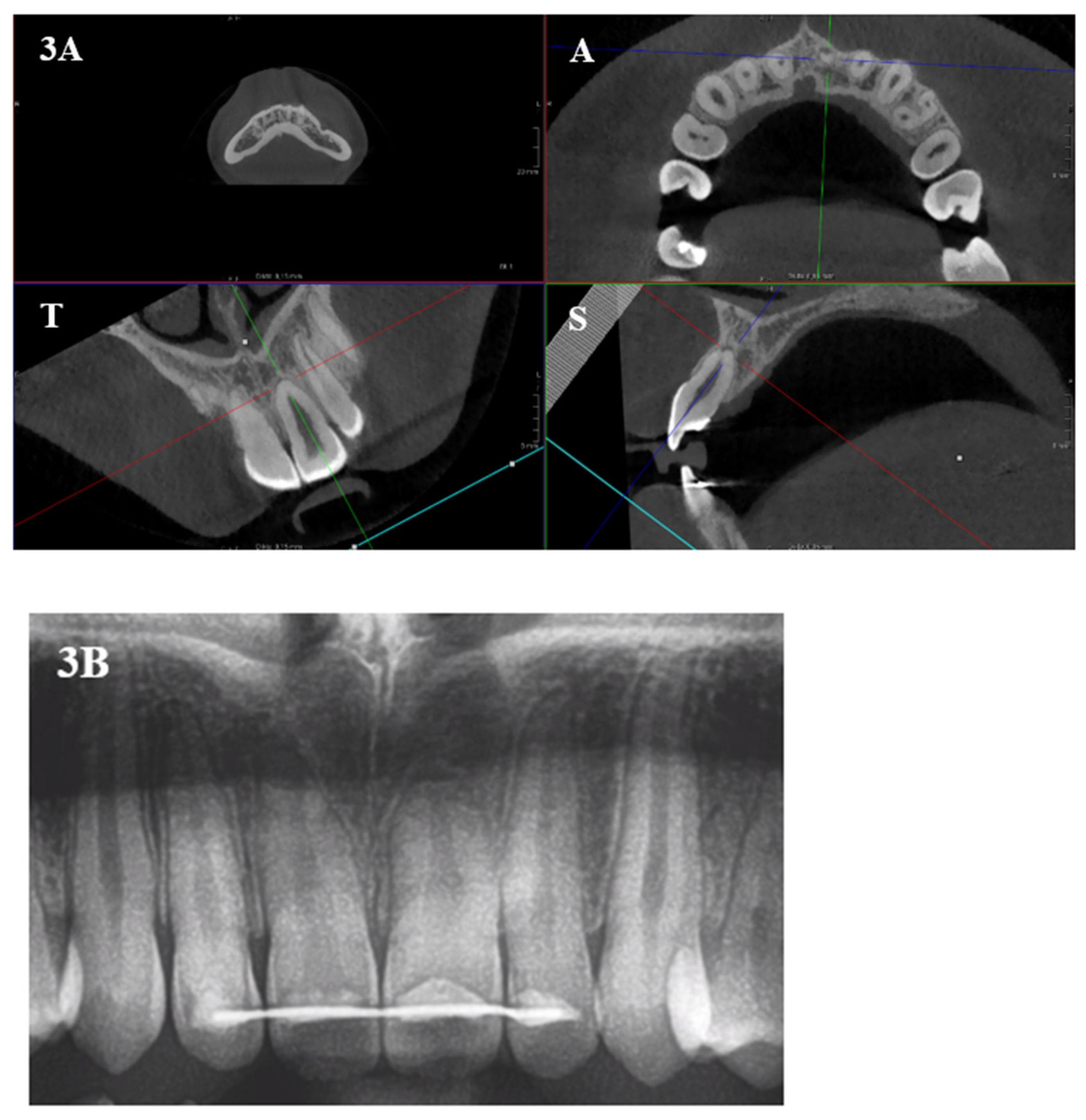
2.2. Methods
2.3. Statistical Analysis
3. Results
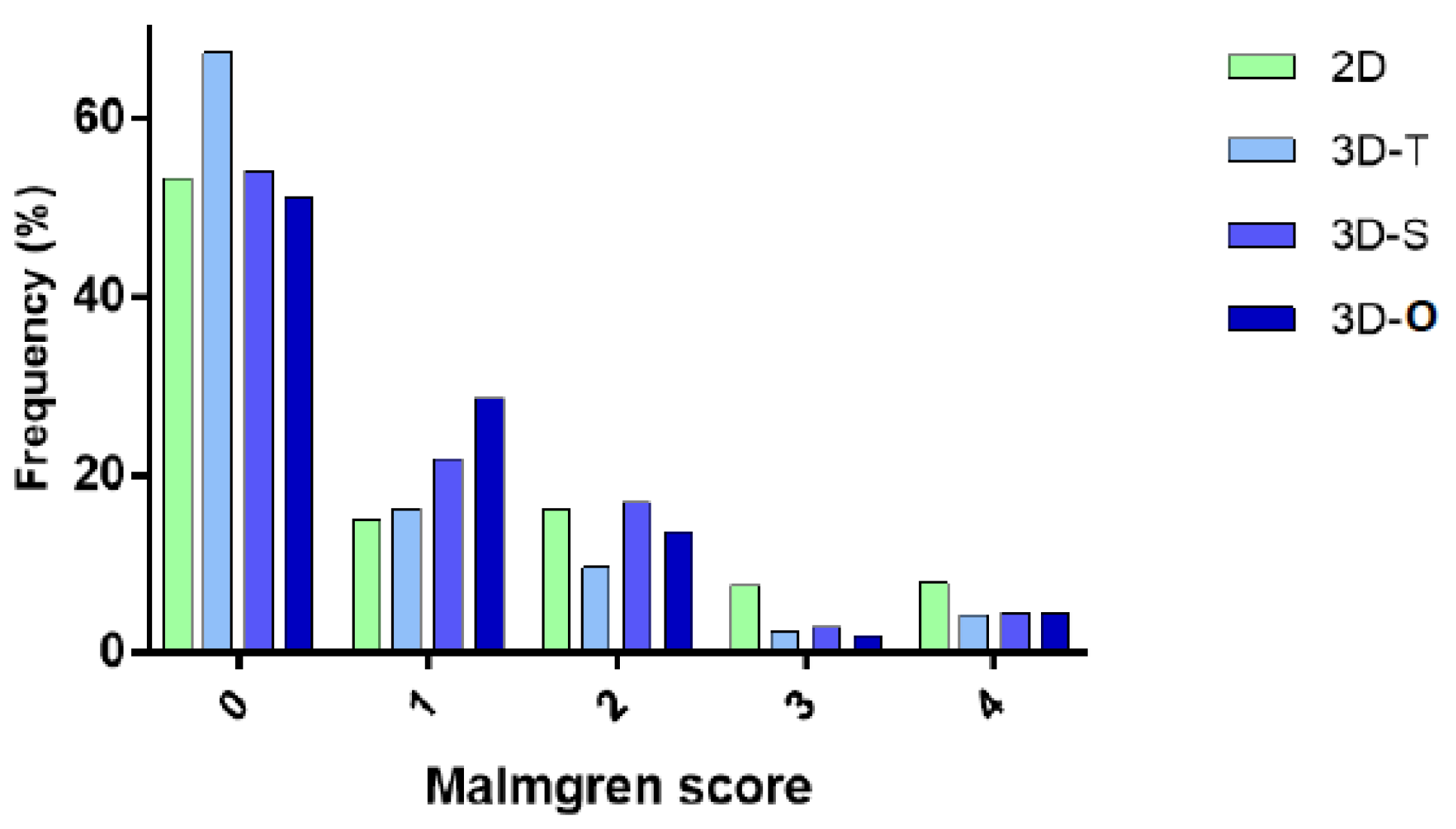
3.1. Malmgren Index in 3D vs. 2D
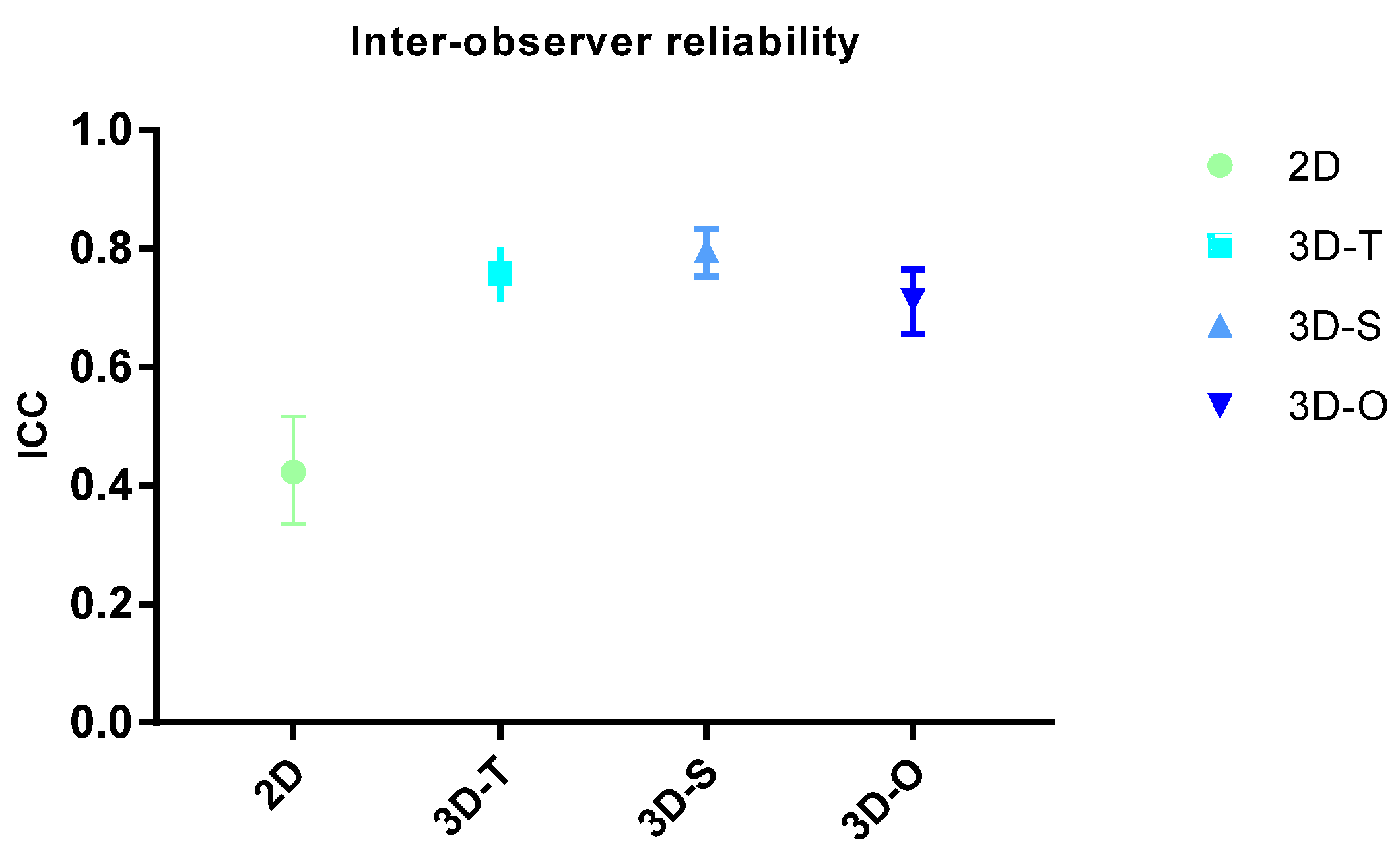
3.2. ICC
3.3. Analysis per Tooth
3.4. Sensitivity and Specificity
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Patel, S.; Saberi, N. The ins and outs of root resorption. Br. Dent. J. 2018, 224, 691–699. [Google Scholar] [CrossRef] [PubMed]
- Brezniak, N.; Wasserstein, A. Root resorption after orthodontic treatment: Part 1. Literature review. Am. J. Orthod. Dentofac. Orthop. 1993, 103, 62–66. [Google Scholar] [CrossRef] [PubMed]
- Sameshima, G.T.; Iglesias-Linares, A. Orthodontic root resorption. J. World Fed. Orthod. 2021, 10, 135–143. [Google Scholar] [CrossRef] [PubMed]
- Kaur, J.; Shetty, D.; Sharma, P.; Kumar, P.; Juneja, A. Evaluation of root resorption after orthodontic treatment: A clinical study of contributory factors. J. Dent. Spéc. 2020, 8, 3–8. [Google Scholar] [CrossRef]
- Alamadi, E.; Alhazmi, H.; Hansen, K.; Lundgren, T.; Naoumova, J. A comparative study of cone beam computed tomography and conventional radiography in diagnosing the extent of root resorptions. Prog. Orthod. 2017, 18, 37. [Google Scholar] [CrossRef] [PubMed]
- Heboyan, A.; Avetisyan, A.; Karobari, M.I.; Marya, A.; Khurshid, Z.; Rokaya, D.; Zafar, M.S.; Fernandes, G.V.D.O. Tooth root resorption: A review. Sci. Prog. 2022, 105, 368504221109217. [Google Scholar] [CrossRef]
- Levander, E.; Malmgren, O. Evaluation of the risk of root resorption during orthodontic treatment: A study of upper incisors. Eur. J. Orthod. 1988, 10, 30–38. [Google Scholar] [CrossRef]
- Bayir, F.; Gumus, E.B. External apical root resorption after orthodontic treatment: Incidence, severity and risk factors. J. Dent. Res. Dent. Clin. Dent. Prospect. 2021, 15, 100–105. [Google Scholar] [CrossRef]
- Topkara, A. External apical root resorption caused by orthodontic treatment: A review of the literature. Eur. J. Paediatr. Dent. 2011, 12, 163–166. [Google Scholar]
- Alqerban, A.; Jacobs, R.; Fieuws, S.; Willems, G. Comparison of two cone beam computed tomographic systems versus panoramic imaging for localization of impacted maxillary canines and detection of root resorption. Eur. J. Orthod. 2011, 33, 93–102. [Google Scholar] [CrossRef]
- Sameshima, G.T.; Asgarifar, K.O. Assessment of root resorption and root shape: Periapical vs panoramic films. Angle Orthod. 2001, 71, 185–189. [Google Scholar] [PubMed]
- Dudic, A.; Giannopoulou, C.; Martinez, M.; Montet, X.; Kiliaridis, S. Diagnostic accuracy of digitized periapical radiographs validated against micro-computed tomography scanning in evaluating orthodontically induced apical root resorption. Eur. J. Oral Sci. 2008, 116, 467–472. [Google Scholar] [CrossRef] [PubMed]
- Dudic, A.; Giannopoulou, C.; Leuzinger, M.; Kiliaridis, S. Detection of apical root resorption after orthodontic treatment by using panoramic radiography and cone-beam computed tomography of super-high resolution. Am. J. Orthod. Dentofac. Orthop. 2009, 135, 434–437. [Google Scholar] [CrossRef] [PubMed]
- Lund, H.; Gröndahl, K.; Gröndahl, H.G. Cone Beam Computed Tomography for Assessment of Root Length and Marginal Bone Level during Orthodontic Treatment. Angle Orthod. 2010, 80, 466–473. [Google Scholar] [CrossRef]
- Makedonas, D.; Lund, H.; Hansen, K. Root resorption diagnosed with cone beam computed tomography after 6 months and at the end of orthodontic treatment with fixed appliances. Angle Orthod. 2012, 83, 389–393. [Google Scholar] [CrossRef]
- Chandorikar, H.; Bhad, W.A. Impact of micro-osteoperforations on root resorption and alveolar bone in en-masse retraction in young adults: A CBCT randomized controlled clinical trial. Int. Orthod. 2023, 21, 100714. [Google Scholar] [CrossRef]
- Apajalahti, S.; Peltola, J.S. Apical root resorption after orthodontic treatment a retrospective study. Eur. J. Orthod. 2007, 29, 408–412. [Google Scholar] [CrossRef]
- Rohlin, M.; Kullendorff, B.; Ahlqwist, M.; Stenstrom, B. Observer performance in the assessment of periapical pathology: A comparison of panoramic with periapical radiography. Dentomaxillofacial Radiol. 1991, 20, 127–131. [Google Scholar] [CrossRef]
- Alqerban, A.; Willems, G.; Bernaerts, C.; Vangastel, J.; Politis, C.; Jacobs, R. Orthodontic treatment planning for impacted maxillary canines using conventional records versus 3D CBCT. Eur. J. Orthod. 2014, 36, 698–707. [Google Scholar] [CrossRef]
- Tang, Z.; Liu, X.; Chen, K. Comparison of digital panoramic radiography versus cone beam computerized tomography for measuring alveolar bone. Head Face Med. 2017, 13, 2. [Google Scholar] [CrossRef]
- Alqerban, A.; Jacobs, R.; Souza, P.C.; Willems, G. In-Vitro comparison of 2 cone-beam computed tomography systems and panoramic imaging for detecting simulated canine impaction-induced external root resorption in maxillary lateral incisors. Am. J. Orthod. Dentofac. Orthop. 2009, 136, 764.e1–764.e11; discussion 764–765. [Google Scholar] [CrossRef]
- Yassir, Y.A.; McIntyre, G.T.; Bearn, D.R. Orthodontic treatment and root resorption: An overview of systematic reviews. Eur. J. Orthod. 2020, 43, 442–456. [Google Scholar] [CrossRef] [PubMed]
- Weltman, B.; Vig, K.W.; Fields, H.W.; Shanker, S.; Kaizar, E.E. Root resorption associated with orthodontic tooth movement: A systematic review. Am. J. Orthod. Dentofac. Orthop. 2010, 137, 462–476. [Google Scholar] [CrossRef] [PubMed]
- Smeyers, F.; Fivez, S.; Van Gorp, G.; Willems, G.; Declerck, D.; Begnoni, G.; Verdonck, A.; Fieuws, S.; de Llano-Pérula, M.C. Evolution of root length throughout orthodontic treatment in maxillary incisors with previous history of dental trauma: A longitudinal controlled trial. Clin. Oral Investig. 2022, 26, 7179–7190. [Google Scholar] [CrossRef]
- Oenning, A.C.; Jacobs, R.; Pauwels, R.; Stratis, A.; Hedesiu, M.; Salmon, B.; DIMITRA Research Group. Cone-beam CT in paediatric dentistry: DIMITRA project position statement. Pediatr Radiol. 2018, 48, 308–316. [Google Scholar] [CrossRef]
- Campobasso, A.; Battista, G.; Muzio, E.L.; Muzio, L.L. The Virtual Patient in Daily Orthodontics: Matching Intraoral and Facial Scans without Cone Beam Computed Tomography. Appl. Sci. 2022, 12, 9870. [Google Scholar] [CrossRef]
- Yeung, A.W.K.; Harper, B.; Zhang, C.; Neelakantan, P.; Bornstein, M.M. Do different cone beam computed tomography exposure protocols influence subjective image quality prior to and after root canal treatment? Clin. Oral Investig. 2020, 25, 2119–2127. [Google Scholar] [CrossRef]
- Ruetters, M.; Gehrig, H.; Kronsteiner, D.; Doll, S.; Kim, T.-S.; Lux, C.J.; Sen, S. Low-dose CBCT imaging of alveolar buccal bone adjacent to mandibular anterior teeth—A pilot study. Clin. Oral Investig. 2022, 26, 4173–4182. [Google Scholar] [CrossRef]
| Comparison | Mean Difference (95% CI) | p-Value |
| 3D-T vs. 2D | −0.425 (−0.502; −0.348) | <0.0001 |
| 3D-S vs. 2D | −0.199 (−0.277; −0.120) | <0.0001 |
| 3D-O vs. 2D | −0.226 (−0.303; −0.149) | <0.0001 |
| Comparison | Odds Ratio (95% CI) | p-Value |
| 3D-A vs. 2D | 0.168 (0.113; 0.250) | <0.0001 |
| Mean Score Differences (p-Value) | ||||||
|---|---|---|---|---|---|---|
| Upper Jaw | Lower Jaw | |||||
| CI | LI | C | CI | LI | C | |
| 3D-T vs. 2D | −0.570 (<0.0001) * | −0.546 (<0.0001) * | −0.121 (0.0441) * | −0.593 (<0.0001) * | −0.396 (0.0001) * | −0.260 (0.0012) * |
| 3D-S vs. 2D | −0.648 (<0.0001) * | −0.204 (0.0307) * | 0.022 (0.7283) | 0.046 (0.7095) | −0.125 (0.2410) | −0.115 (0.1676) |
| 3D-O vs. 2D | −0.484 (<0.0001) * | −0.288 (0.0032) * | −0.013 (0.8424) | −0.172 (0.1361) | −0.187 (0.0715) | −0.102 (0.2165) |
| 3D-A vs. 2D | Odds Ratio (p-Value) | |||||
| Upper Jaw | Lower Jaw | |||||
| CI | LI | C | CI | LI | C | |
| 0.096 (<0.0001) * | 0.750 (0.0032) * | 0.9546 (0.8424) | 0.390 (0.0392) * | 0.112 (0.0004) * | 0.176 (0.0303) * | |
| Malmgren Scores | 3D-T | 3D-S | 3D-O | 3D-A | ||
|---|---|---|---|---|---|---|
| 0 vs. 1–4 | % Sensitivity (CI) | True positives | 72.0 (65.2; 78.1) | 66.4 (60.6; 71.9) | 65.8 (60.1; 71.1) | NA |
| False negatives | 28.0 (21.9; 34.8) | 33.6 (28.1; 39.4) | 34.2 (28.9; 39.9) | NA | ||
| % Specificity (CI) | True negatives | 65.2 (60.4; 69.8) | 69.7 (64.4; 74.6) | 70.8 (65.4; 75.8) | NA | |
| False positives | 34.8 (30.2; 39.4) | 30.3 (25.4; 35.6) | 29.2 (24.2; 34.6) | NA | ||
| 0–1 vs. 2–4 | % Sensitivity (CI) | True positives | 82.0 (73.1; 89.0) | 66.4 (58.3; 74.0) | 75.6 (67.0; 82.9) | 79.8 (69.9; 87.6) |
| False negatives | 18.0 (11.0; 26.9) | 33.6 (26.0; 41.7) | 24.4 (17.1; 33.0) | 20.2 (12.4; 30.1) | ||
| % Specificity (CI) | True negatives | 78.0 (74.2; 81.5) | 79.3 (75.3; 82.9) | 79.2 (75.3; 82.7) | 76.4 (72.5; 80.0) | |
| False positives | 22.0 (18.5; 25.8) | 20.7 (17.1; 24.7) | 20.8 (17.3; 24.7) | 23.6 (20.0; 27.5) | ||
| 0–2 vs. 3–4 | % Sensitivity (CI) | True positives | 90.2 (76.9; 97.3) | 82.6 (68.6; 92.2) | 92.5 (79.6; 98.4) | NA |
| False negatives | 9.8 (2.7; 23.1) | 17.4 (7.8; 31.4) | 7.5 (1.6; 20.4) | NA | ||
| % Specificity (CI) | True negatives | 89.7 (86.9; 92.1) | 89.8 (87.0; 92.1) | 89.7 (86.9; 92.1) | NA | |
| False positives | 10.3 (7.9; 13.8) | 10.2 (7.9; 13.0) | 10.3 (7.9; 13.1) | NA | ||
| 0–3 vs. 4 | % Sensitivity (CI) | True positives | 88.5 (69.8; 97.6) | 89.3 (71.8; 97.7) | 89.3 (71.8; 97.7) | NA |
| False negatives | 11.5 (2.4; 30.2) | 10.7 (2.3; 28.2) | 10.7 (2.3; 28.2) | NA | ||
| % Specificity (CI) | True negatives | 95.6 (93.6; 97.1) | 95.9 (94.0; 97.4) | 95.9 (94.0; 97.4) | NA | |
| False positives | 4.4 (2.9–6.4) | 4.1 (2.6; 6.0) | 4.1 (2.6; 6.0) | NA |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Michielsens, H.; Decreus, J.; Begnoni, G.; Verdonck, A.; Jacobs, R.; Willems, G.; Cadenas de Llano-Pérula, M. Performance of the Malmgren Index for Assessing Root Resorption on 2D vs. 3D Radiographs: A Pilot Study. Healthcare 2023, 11, 1860. https://doi.org/10.3390/healthcare11131860
Michielsens H, Decreus J, Begnoni G, Verdonck A, Jacobs R, Willems G, Cadenas de Llano-Pérula M. Performance of the Malmgren Index for Assessing Root Resorption on 2D vs. 3D Radiographs: A Pilot Study. Healthcare. 2023; 11(13):1860. https://doi.org/10.3390/healthcare11131860
Chicago/Turabian StyleMichielsens, Hanne, Julie Decreus, Giacomo Begnoni, Anna Verdonck, Reinhilde Jacobs, Guy Willems, and Maria Cadenas de Llano-Pérula. 2023. "Performance of the Malmgren Index for Assessing Root Resorption on 2D vs. 3D Radiographs: A Pilot Study" Healthcare 11, no. 13: 1860. https://doi.org/10.3390/healthcare11131860
APA StyleMichielsens, H., Decreus, J., Begnoni, G., Verdonck, A., Jacobs, R., Willems, G., & Cadenas de Llano-Pérula, M. (2023). Performance of the Malmgren Index for Assessing Root Resorption on 2D vs. 3D Radiographs: A Pilot Study. Healthcare, 11(13), 1860. https://doi.org/10.3390/healthcare11131860








