Benefits of Cultural Activities on People with Cognitive Impairment: A Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Eligibility
2.2. Search Strategy
2.3. Data Extraction and Variable Coding
2.4. Effect Size Index/s and Statistical Analysis
2.5. Quality Appraisal
3. Results
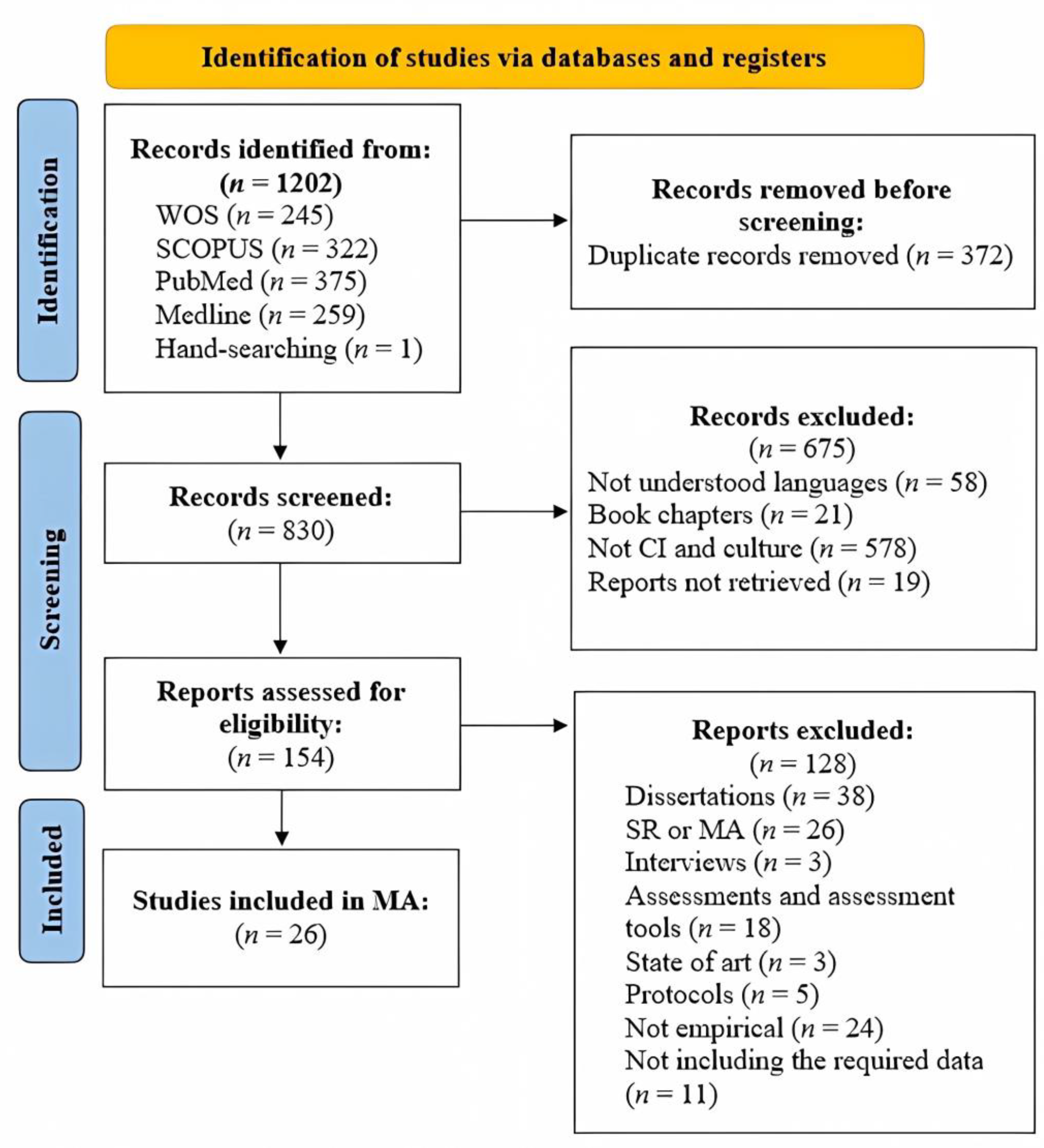
3.1. Search Outcome
3.2. Study Characteristics
3.3. Benefits Analysis
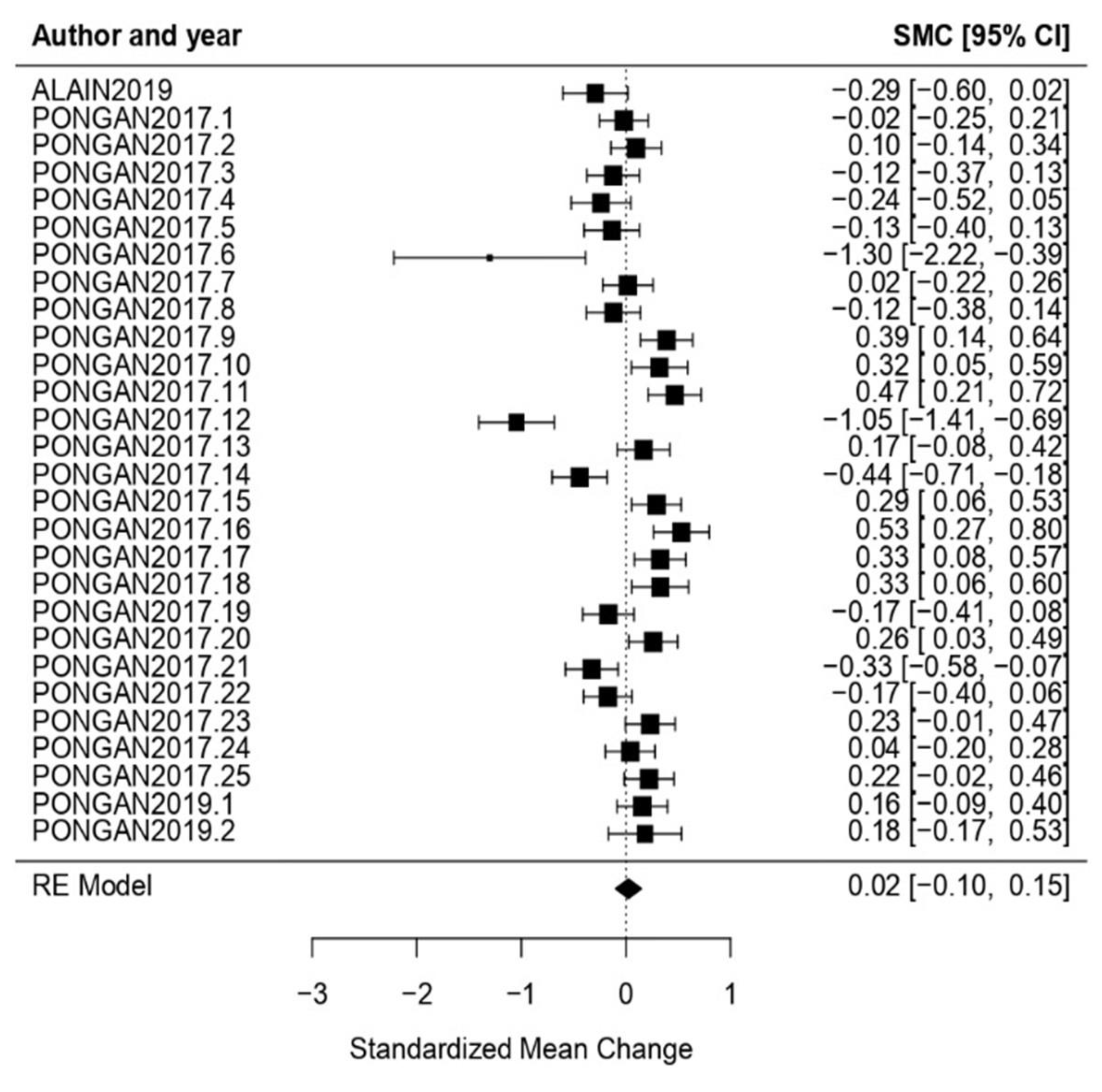
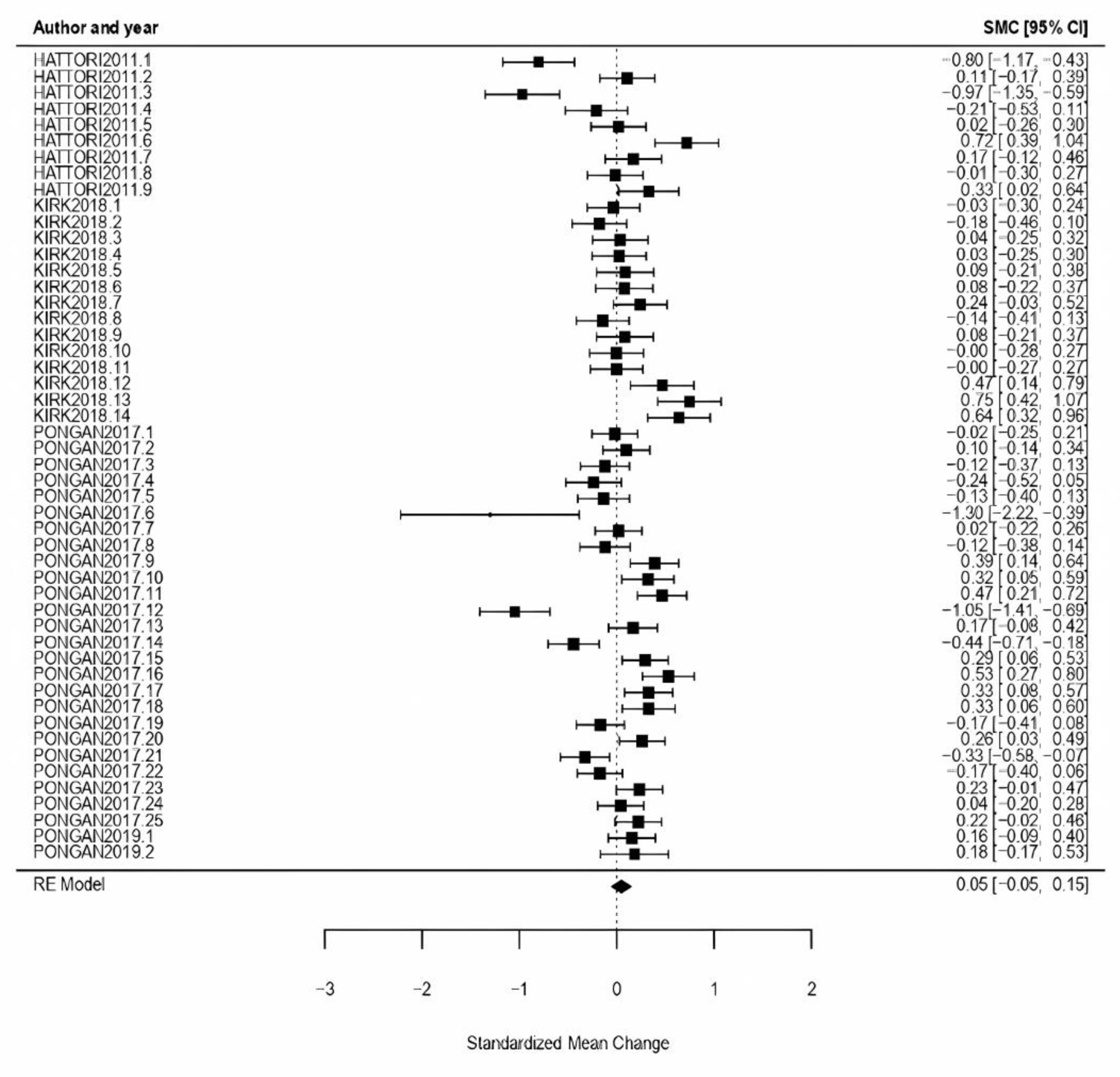
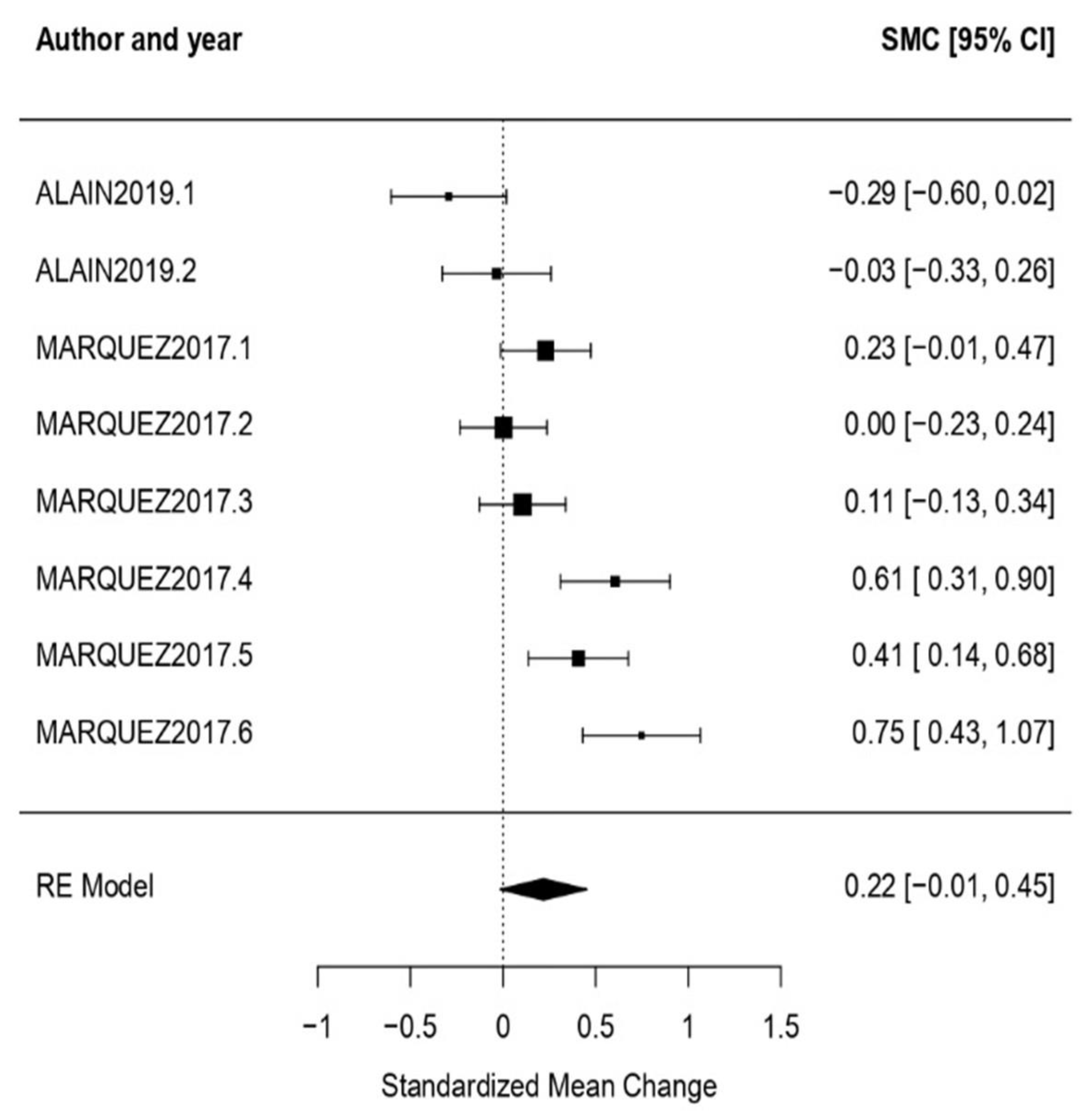
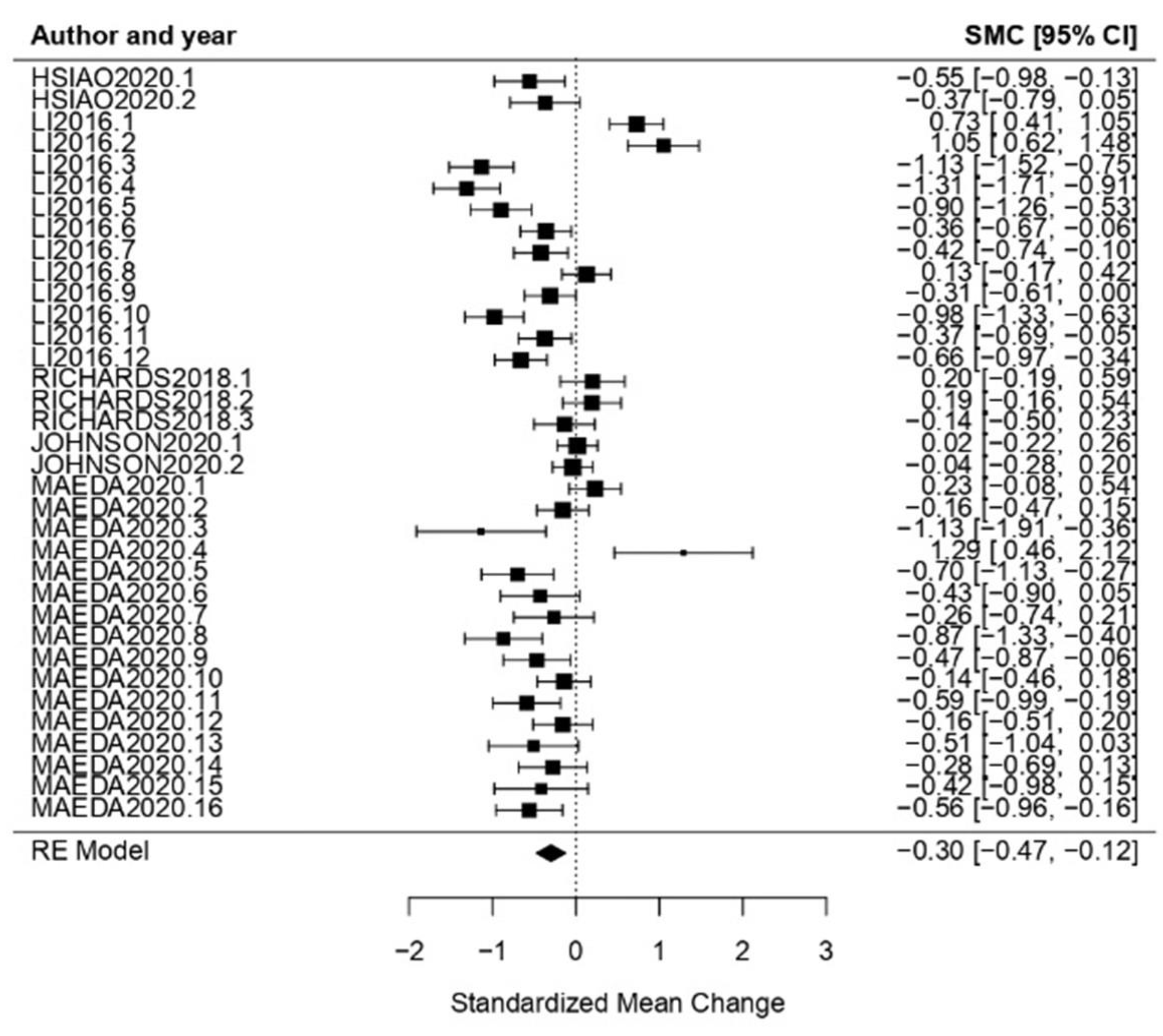
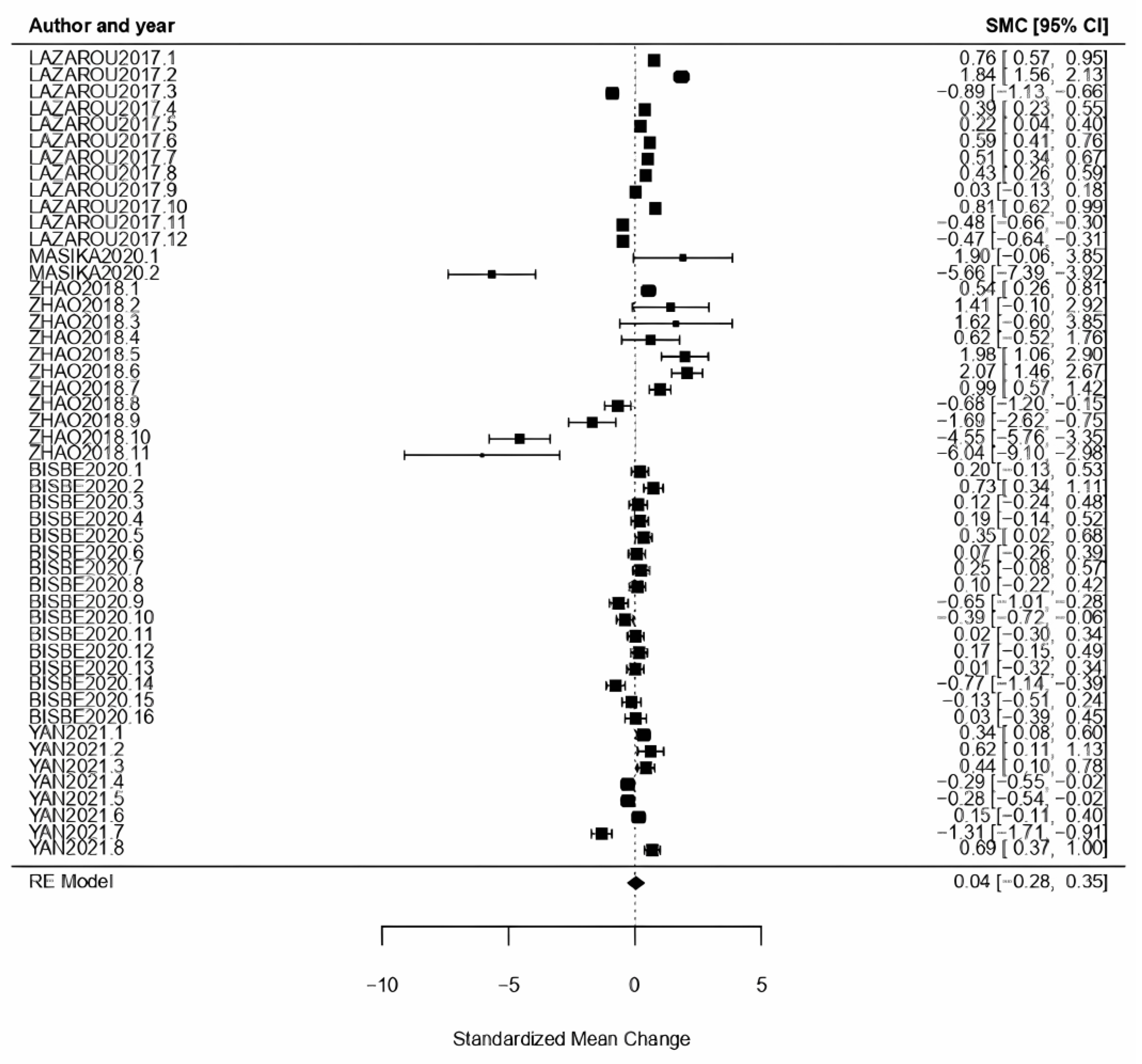
3.3.1. General Results
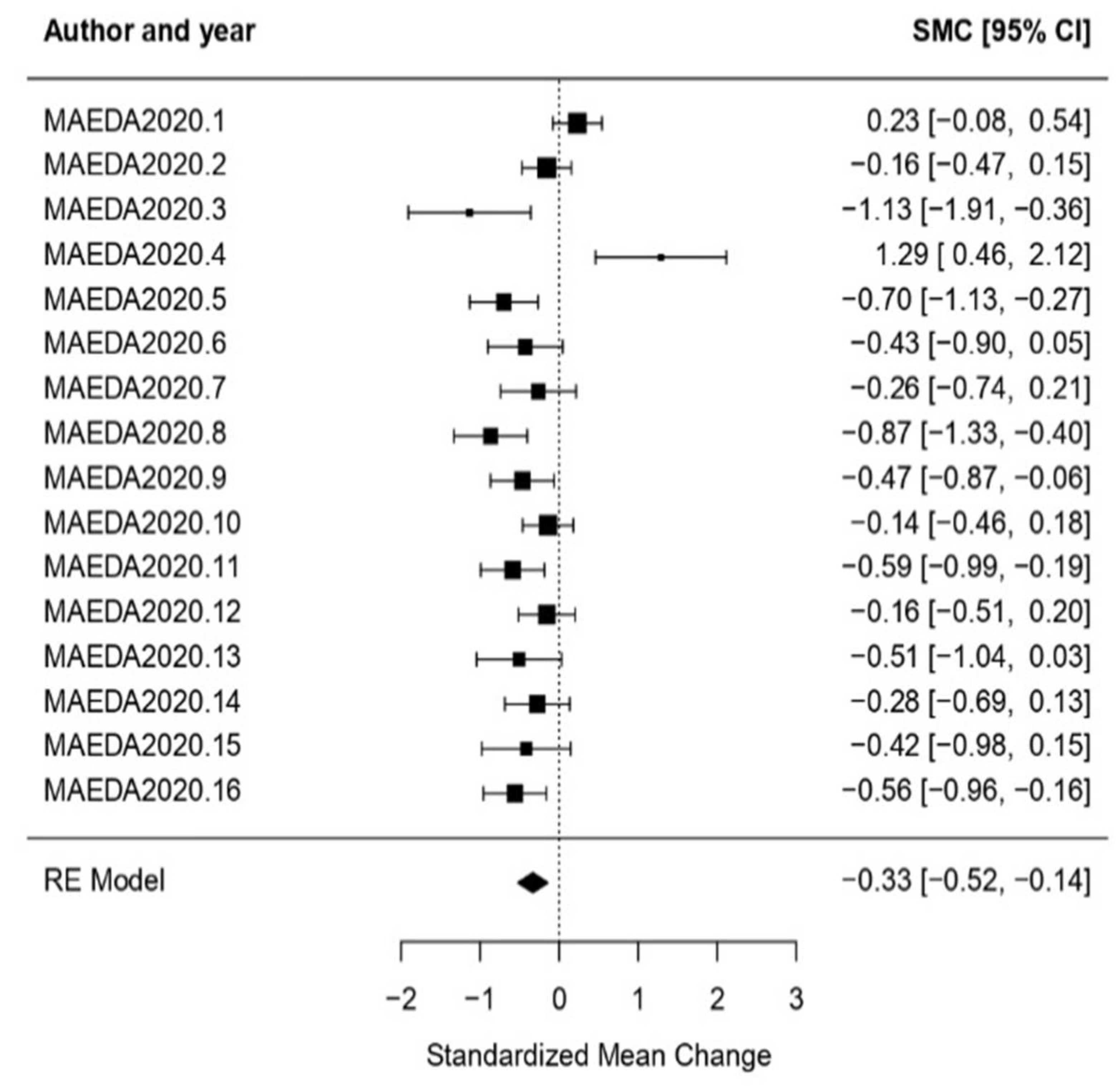
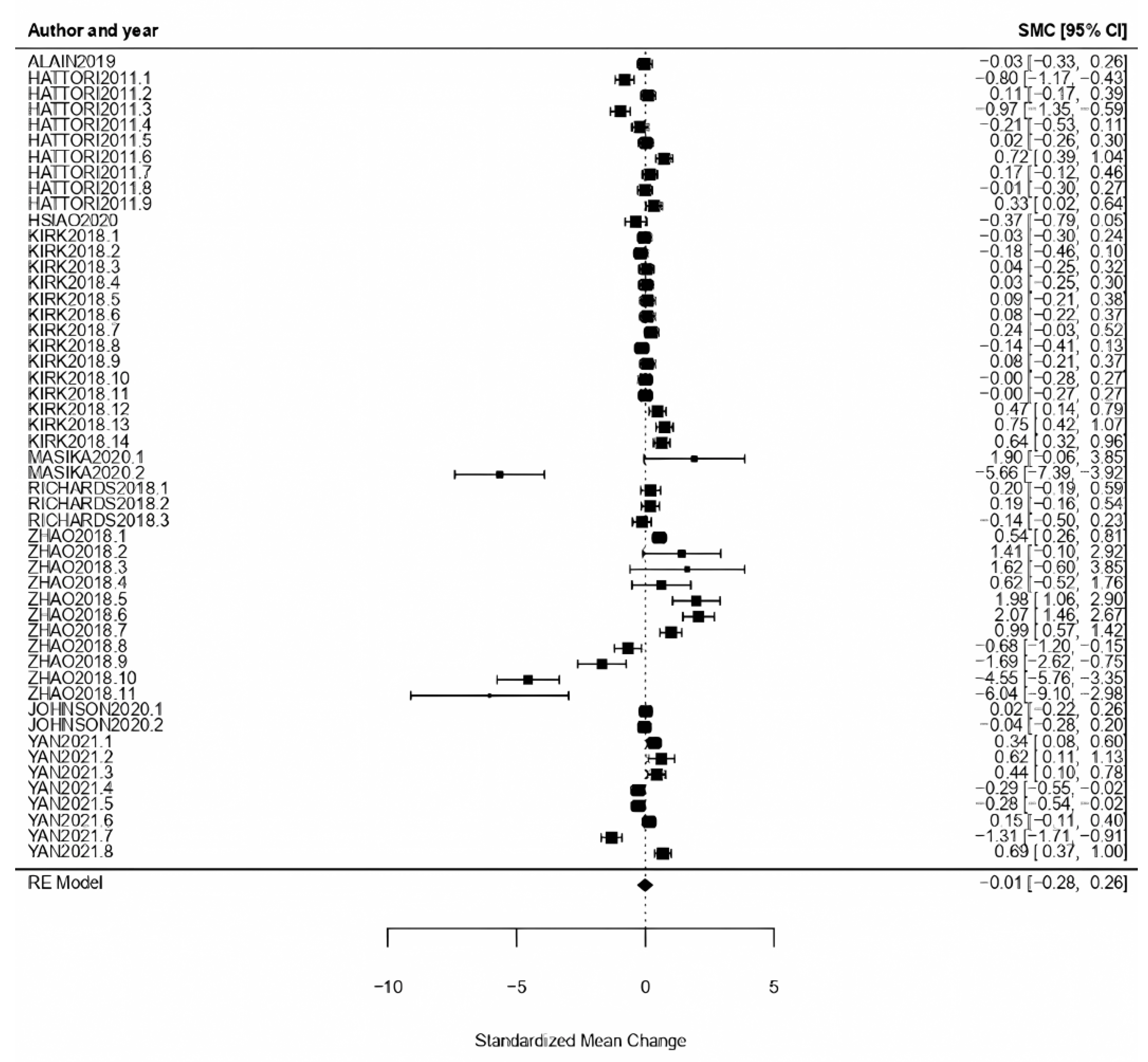
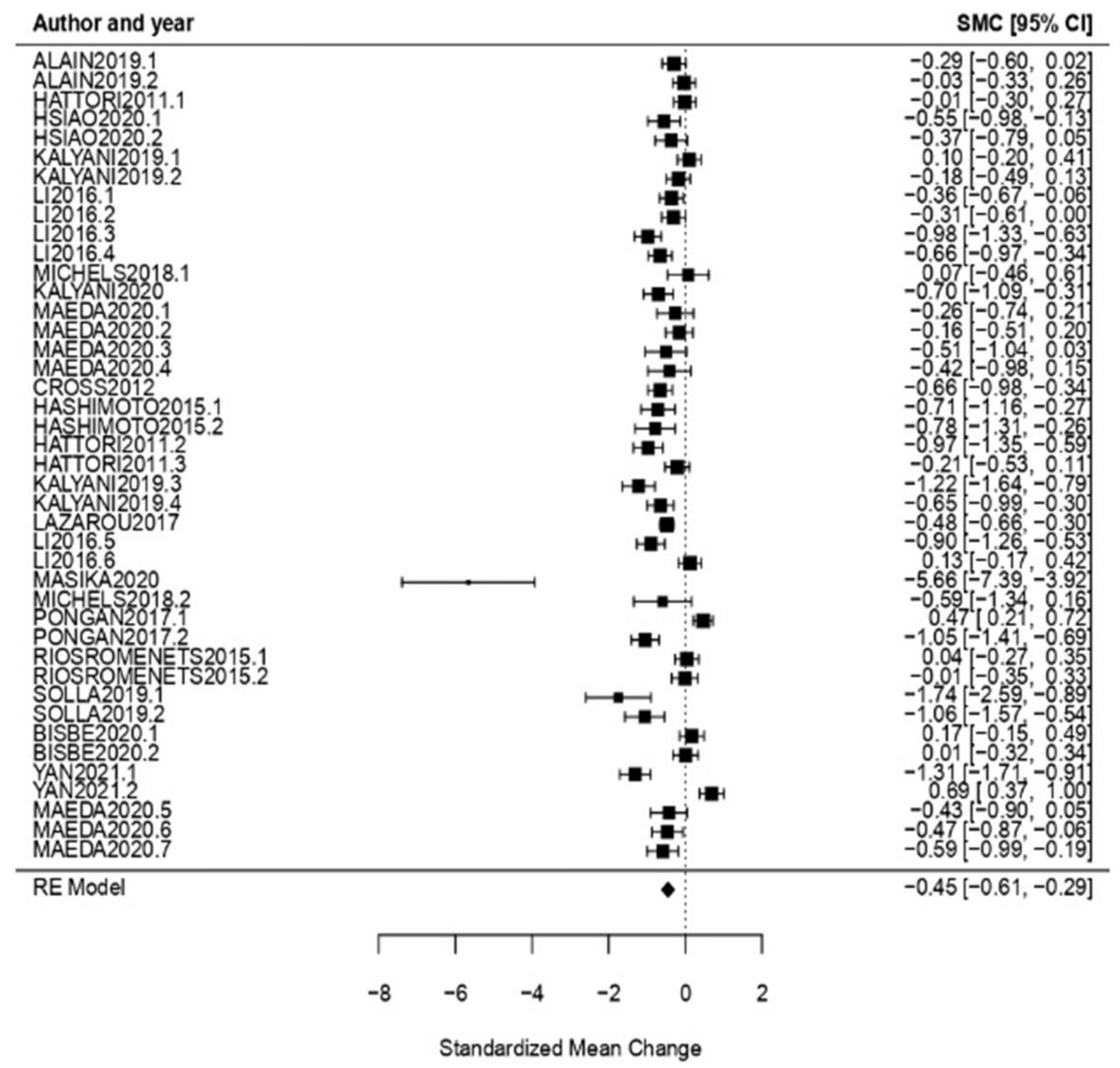
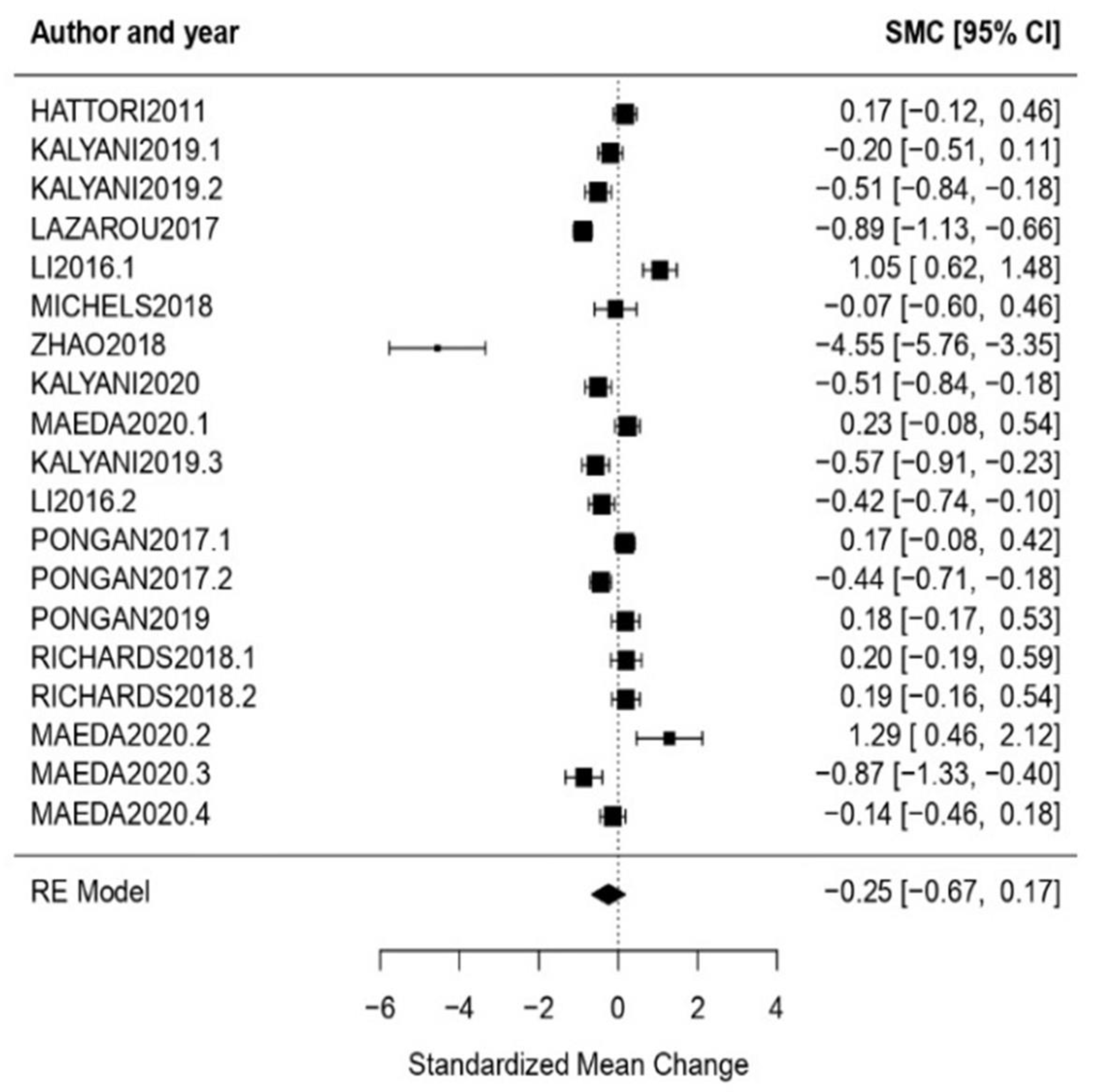
3.3.2. Analysis per Treatment
3.3.3. Analysis per Evaluation
3.3.4. Analysis per CI Typology
3.3.5. Moderator Variables Effects
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Critical Appraisal Checklists and Results
Appendix A.1. JBI Critical Appraisal Checklist for Randomized Controlled Trials
- Q1.
- Was true randomization used for the assignment of participants to treatment groups?
- Q2.
- Was allocation to treatment groups concealed?
- Q3.
- Were treatment groups similar at baseline?
- Q4.
- Were participants blind to treatment assignment?
- Q5.
- Were those delivering treatment blind to treatment assignment?
- Q6.
- Were outcomes assessors blind to treatment assignment?
- Q7.
- Were treatment groups treated identically other than the intervention of interest?
- Q8.
- Was follow-up complete, and if not, were differences between groups in terms of their follow-up adequately described and analyzed?
- Q9.
- Were participants analyzed in the groups to which they were randomized?
- Q10.
- Were outcomes measured in the same way for treatment groups?
- Q11.
- Were outcomes measured in a reliable way?
- Q12.
- Was appropriate statistical analysis used?
- Q13.
- Was the trial design appropriate, and were any deviations from the standard RCT design (individual randomization, parallel groups) accounted for in the conduct and analysis of the trial?
| Reference | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Q11 | Q12 | Q13 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| [45] | Y | Y | Y | N/A | N/A | Y | Y | Y | Y | Y | Y | Y | Y |
| [57] | Y | Y | Y | N | N/A | N/A | Y | Y | Y | Y | Y | Y | Y |
| [38] | Y | Y | Y | Y | N/A | N | U | Y | Y | Y | Y | Y | Y |
| [48] | Y | Y | Y | U | N/A | Y | Y | Y | Y | Y | Y | Y | Y |
| [7] | Y | Y | Y | N/A | N | Y | Y | Y | Y | Y | Y | Y | Y |
| [40] | Y | Y | Y | N/A | N/A | N/A | Y | Y | Y | Y | Y | Y | Y |
| [53] | Y | Y | Y | N | N/A | Y | Y | Y | Y | Y | Y | Y | Y |
| [10] | Y | N/A | Y | N | N/A | N/A | Y | Y | Y | Y | Y | Y | Y |
| [47] | U | N/A | Y | N/A | N/A | Y | Y | Y | Y | Y | Y | Y | Y |
| [50] | Y | N/A | Y | N/A | N/A | N/A | Y | Y | Y | Y | Y | Y | Y |
| [52] | Y | N/A | Y | N | N/A | N/A | Y | Y | Y | Y | Y | Y | Y |
| [43] | Y | N/A | Y | N | N/A | Y | Y | Y | Y | Y | Y | Y | Y |
| [46] | Y | Y | Y | N | N | Y | Y | Y | Y | Y | Y | Y | Y |
| [55] | Y | N/A | Y | U | N/A | N/A | Y | Y | Y | Y | Y | Y | Y |
| [42] | Y | N/A | Y | N/A | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| [56] | Y | N/A | Y | N/A | N/A | Y | Y | Y | Y | Y | Y | Y | Y |
| [44] | Y | N/A | Y | N/A | N/A | Y | Y | Y | Y | Y | Y | Y | Y |
| [37] | Y | Y | Y | N/A | N/A | Y | Y | Y | Y | Y | Y | Y | Y |
| [51] | Y | N/A | Y | N/A | N/A | Y | Y | Y | Y | Y | Y | Y | Y |
| % | 94.73 | 47.36 | 100.0 | 5.26 | 5.26 | 63.15 | 94.73 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 |
Appendix A.2. JBI Critical Appraisal Checklist for Quasi-Experimental Studies (Non-Randomized Experimental Studies)
- Q1.
- Is it clear in the study what is the ‘cause’ and what is the ‘effect’ (i.e., there is no confusion about which variable comes first)?
- Q2.
- Were the participants included in any comparisons similar?
- Q3.
- Were the participants included in any comparisons receiving similar treatment/care other than the exposure or intervention of interest?
- Q4.
- Was there a control group?
- Q5.
- Were there multiple measurements of the outcome both pre- and post-intervention or exposure?
- Q6.
- Was follow-up complete, and if not, were differences between groups in terms of their follow-up adequately described and analyzed?
- Q7.
- Were the outcomes of participants included in any comparisons measured in the same way?
- Q8.
- Were outcomes measured in a reliable way?
- Q9.
- Was appropriate statistical analysis used?
References
- Health Direct. Cognitive Impairment. Available online: https://www.healthdirect.gov.au/cognitive-impairment (accessed on 23 February 2022).
- World Health Organization. Dementia. Available online: https://www.who.int/es/news-room/fact-sheets/detail/dementia (accessed on 14 April 2022).
- O’Brien, J.T.; Erkinjuntti, T.; Reisberg, B.; Roman, G.; Sawada, T.; Pantoni, L.; Bowler, J.V.; Ballard, C.; DeCarli, C.; Gorelick, P.B.; et al. Vascular Cognitive Impairment. Lancet Neurol. 2003, 2, 89–98. [Google Scholar] [CrossRef] [PubMed]
- Macías Osuna, A.E. Alzheimer: La Enfermedad Del Siglo XXI. Avances 2005, 3, 7–14. [Google Scholar]
- Lucas, J.C.; Arambula, Z.; Arambula, A.M.; Yu, K.; Farrokhian, N.; D’Silva, L.; Staecker, H.; Villwock, J.A. Olfactory, Auditory, and Vestibular Performance: Multisensory Impairment Is Significantly Associated With Incident Cognitive Impairment. Front. Neurol. 2022, 13, 1471. [Google Scholar] [CrossRef]
- The Economist Intelligence Unit. Assessing the Socioeconomic Impact of Alzheimer’s Disease in Western Europe and Canada; Economist Intelligence Unit: London, UK, 2017; pp. 1–79. [Google Scholar]
- Volpe, D.; Signorini, M.; Marchetto, A.; Lynch, T.; Morris, M.E. A Comparison of Irish Set Dancing and Exercises for People with Parkinson’s Disease: A Phase II Feasibility Study. BMC Geriatr. 2013, 13, 54–56. [Google Scholar] [CrossRef] [PubMed]
- Ciccarelli, N.; Di Tella, S.; Lo Monaco, M.R.; Carfì, A.; Serafini, E.; Delle Donne, V.; Silveri, M.C. Emotional Valence May Influence Memory Performance for Visual Artworks in Parkinson’s Disease. Neurol. Sci. 2019, 40, 2175–2178. [Google Scholar] [CrossRef]
- Brown, C.J.; Chirino, A.F.C.; Cortez, C.M.; Gearhart, C.; Urizar, G.G. Conceptual Art for the Aging Brain: Piloting an Art-Based Cognitive Health Intervention. Act. Adapt. Aging 2020, 45, 39–69. [Google Scholar] [CrossRef]
- Cross, K.; Flores, R.; Butterfield, J.; Blackman, M.; Lee, S. The Efect of Passive Listening versus Active Observation of Music and Dance Performances on Memory Recognition and Mild to Moderate Depression in Cognitively Impaired Older Adults. Psychol. Rep. 2012, 111, 413–423. [Google Scholar] [CrossRef] [PubMed]
- Fancourt, D.; Finn, S. What Is the Evidence on the Role of the Arts in Improving Health Scoping Review; World Health Organization. Regional Office for Europe: Copenhagen, Denmark, 2019. [Google Scholar]
- Letrondo, P.A.; Ashley, S.A.; Flinn, A.; Burton, A.; Kador, T.; Mukadam, N. Systematic Review of Arts and Culture-Based Interventions for People Living with Dementia and Their Caregivers. Ageing Res. Rev. 2023, 83, 101793. [Google Scholar] [CrossRef]
- UNESCO. Sobre Definiciones: ¿Qué Se Entiende por Industrias Culturales y Creativas? Available online: http://www.unesco.org/new/es/culture/themes/cultural-diversity/diversity-of-%09cultural-expressions/tools/policy-guide/como-usar-esta-guia/sobre-definiciones-%09que-se-entiende-por-industrias-culturales-y-creativas/ (accessed on 28 April 2022).
- Throsby, D. The Concentric Circles Model of the Cultural Industries. Cult. Trends 2008, 17, 147–164. [Google Scholar] [CrossRef]
- Camic, P.M.; Chatterjee, H.J. Museums and Art Galleries as Partners for Public Health Interventions. Perspect. Public Health 2013, 133, 66–71. [Google Scholar] [CrossRef]
- Desmarais, S.; Bedford, L.; Chatterjee, H.J. Museums as Spaces for Wellbeing: A Second Report from the National Alliance for Museums, Health and Wellbeing; National Alliance for Museums, Health & Wellbeing: London, UK, 2018. [Google Scholar]
- Jung, Y. The Art Museum Ecosystem: A New Alternative Model. Mus. Manag. Curatorship 2011, 26, 321–338. [Google Scholar] [CrossRef]
- Chatterjee, H.J.; Camic, P.M. The Health and Well-Being Potential of Museums and Art Galleries. Arts Health 2015, 7, 183–186. [Google Scholar] [CrossRef]
- Cuypers, K.; Krokstad, S.; Holmen, T.L.; Knudtsen, M.S.; Bygren, L.O.; Holmen, J. Patterns of Receptive and Creative Cultural Activities and Their Association with Perceived Health, Anxiety, Depression and Satisfaction with Life among Adults: The HUNT Study, Norway. J. Epidemiol. Community Health 2012, 66, 698–703. [Google Scholar] [CrossRef]
- O’Neill, M. Cultural Attendance and Public Mental Health—from Research to Practice. J. Public Ment. Health 2010, 9, 22–29. [Google Scholar] [CrossRef]
- Thomson, L.J.; Ander, E.E.; Menon, U.; Lanceley, A.; Chatterjee, H.J. Evaluating the Therapeutic Effects of Museum Object Handling with Hospital Patients: A Review and Initial Trial of Well-Being Measures. J. Appl. Arts Health 2011, 2, 37–56. [Google Scholar] [CrossRef] [PubMed]
- Delfa-Lobato, L.; Guàrdia-Olmos, J.; Feliu-Torruella, M. Benefits of Cultural Activities on People With Cognitive Impairment: A Systematic Review. Front. Psychol. 2021, 12, 5332. [Google Scholar] [CrossRef]
- Hutton, B.; Catalá-López, F.; Moher, D. La Extensión de La Declaración PRISMA Para Revisiones Sistemáticas Que Incorporan Metaanálisis En Red: PRISMA-NMA. Med. Clin. 2016, 147, 262–266. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Altman, D.; Antes, G.; Atkins, D.; Barbour, V.; Barrowman, N.; Berlin, J.A.; et al. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- UNESCO. MUNDIACULT. Declaración de México Sobre Las Políticas Culturales (1982). Available online: http://www.culturalrights.net/descargas/drets_culturals400.pdf (accessed on 25 March 2022).
- de los Ángeles Fernández-Altuna, M.; del Prado, A.M.; Arriarán Rodríguez, E.; Gutiérrez Rayón, D.; Toriz Castillo, H.A.; Lifshitz Guinzberg, A. Uso de Los MeSH: Una Guía Práctica. Investig. Educ. Médica 2016, 5, 220–229. [Google Scholar] [CrossRef]
- Ruiz Martín, J.-F. Los Factores Definitorios de Los Grandes Grupos de Edad de La Población: Tipos, Subgrupos y Umbrales. Scr. Nova. Rev. Electrónica Geogr. Cienc. Soc. 2005, 9, 181–204. [Google Scholar]
- Dyussenbayev, A. Age Periods of Human Life. Adv. Soc. Sci. Res. J. 2017, 4, 260–262. [Google Scholar] [CrossRef]
- Frías Navarro, M.D.; Pascual Llobell, J.; García Pérez, J.F. Tamaño Del Efecto Del Tratamiento y Significación Estadística. Psicothema 2000, 12 (Suppl. S2), 236–240. [Google Scholar]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; New York University, Ed.; Lawrence Erlbaum Associates: New York, NY, USA, 1988. [Google Scholar]
- Marín Martínez, F.; Sánchez Meca, J.; López López, J.A. El Metaanálisis En El Ámbito de Las Ciencias de La Salud: Una Metodología Imprescindible Para La Eficiente Acumulación Del Conocimiento. Fisioterapia 2009, 31, 107–114. [Google Scholar] [CrossRef]
- Gordon, H.R.D. Meta-Analysis Research: A Potential Choice for CTE Researchers and Consumers; Marshall University: Huntington, WV, USA, 2007. [Google Scholar]
- Giménez, A. ¿Qué Es Un Meta-Análisis? Y ¿cómo Leerlo? Biomedicina 2012, 7, 16–27. [Google Scholar]
- Kalyani, H.H.N.; Sullivan, K.A.; Moyle, G.; Brauer, S.; Jeffrey, E.R.; Kerr, G.K. Impacts of Dance on Cognition, Psychological Symptoms and Quality of Life in Parkinson’s Disease. NeuroRehabilitation 2019, 45, 273–283. [Google Scholar] [CrossRef]
- Kalyani, H.H.N.; Sullivan, K.A.; Moyle, G.; Brauer, S.; Jeffrey, E.R.; Kerr, G.K. Dance Improves Symptoms, Functional Mobility and Fine Manual Dexterity in People with Parkinson Disease: A Quasi-Experimental Controlled Efficacy Study. Eur. J. Phys. Rehabil. Med. 2020, 56, 563–574. [Google Scholar] [CrossRef]
- Dos Santos, M.; Monteiro, E.P.; Donida, R.G.; Wolffenbuttel, M.; Peyré-Tartaruga, L.A.; Haas, A.N. Can Samba and Forró Brazilian Rhythmic Dance Be More Effective than Walking in Improving Functional Mobility and Spatiotemporal Gait Parameters in Patients with Parkinson’s Disease? BMC Neurol. 2020, 20, 305. [Google Scholar] [CrossRef]
- Johnson, K.G.; D’Souza, A.A.; Wiseheart, M. Art Training in Dementia: A Randomized Controlled Trial. Front. Psychol. 2020, 11, 585508. [Google Scholar] [CrossRef] [PubMed]
- Rios Romenets, S.; Anang, J.; Fereshtehnejad, S.M.; Pelletier, A.; Postuma, R. Tango for Treatment of Motor and Non-Motor Manifestations in Parkinson’s Disease: A Randomized Control Study. Complement. Ther. Med. 2015, 23, 175–184. [Google Scholar] [CrossRef]
- Li, D.M.; Li, X.X. The Effect of Folk Recreation Program in Improving Symptoms: A Study of Chinese Elder Dementia Patients. Int. J. Geriatr. Psychiatry 2016, 32, 901–908. [Google Scholar] [CrossRef]
- Zhao, J.; Li, H.; Lin, R.; Wei, Y.; Yang, A. Effects of Creative Expression Therapy for Older Adults with Mild Cognitive Impairment at Risk of Alzheimer’s Disease: A Randomized Controlled Clinical Trial. Clin. Interv. Aging 2018, 13, 1313–1320. [Google Scholar] [CrossRef]
- Yan, Y.J.; Lin, R.; Zhou, Y.; Luo, Y.T.; Cai, Z.Z.; Zhu, K.Y.; Li, H. Effects of Expressive Arts Therapy in Older Adults with Mild Cognitive Impairment: A Pilot Study. Geriatr. Nurs. 2021, 42, 129–136. [Google Scholar] [CrossRef] [PubMed]
- Masika, G.M.; Yu, D.S.F.; Li, P.W.C. Can Visual Art Therapy Be Implemented With Illiterate Older Adults With Mild Cognitive Impairment? A Pilot Mixed-Method Randomized Controlled Trial. J. Geriatr. Psychiatry Neurol. 2020, 34, 76–86. [Google Scholar] [CrossRef] [PubMed]
- Kirk, M.; Rasmussen, K.W.; Overgaard, S.B.; Berntsen, D. Five Weeks of Immersive Reminiscence Therapy Improves Autobiographical Memory in Alzheimer’s Disease. Memory 2018, 27, 441–454. [Google Scholar] [CrossRef]
- Pongan, E.; Tillmann, B.; Leveque, Y.; Trombert, B.; Getenet, J.C.; Auguste, N.; Dauphinot, V.; El Haouari, H.; Navez, M.; Dorey, J.M.; et al. Can Musical or Painting Interventions Improve Chronic Pain, Mood, Quality of Life, and Cognition in Patients with Mild Alzheimer’s Disease? Evidence from a Randomized Controlled Trial. J. Alzheimer’s Dis. 2017, 60, 663–677. [Google Scholar] [CrossRef]
- Pongan, E.; Delphin-Combe, F.; Krolak-Salmon, P.; Leveque, Y.; Tillmann, B.; Bachelet, R.; Getenet, J.C.; Auguste, N.; Trombert, B.; Dorey, J.M.; et al. Immediate Benefit of Art on Pain and Well-Being in Community-Dwelling Patients with Mild Alzheimer’s. Am. J. Alzheimer’s Dis. Other Dement. 2019, 35, 1533317519859202. [Google Scholar] [CrossRef]
- Lazarou, I.; Parastatidis, T.; Tsolaki, A.; Gkioka, M.; Karakostas, A.; Douka, S.; Tsolaki, M. International Ballroom Dancing Against Neurodegeneration: A Randomized Controlled Trial in Greek Community-Dwelling Elders With Mild Cognitive Impairment. Am. J. Alzheimer’s Dis. Dement. 2017, 32, 489–499. [Google Scholar] [CrossRef]
- De Natale, E.R.; Paulus, K.S.; Aiello, E.; Sanna, B.; Manca, A.; Sotgiu, G.; Leali, P.T.; Deriu, F. Dance Therapy Improves Motor and Cognitive Functions in Patients with Parkinson’s Disease. NeuroRehabilitation 2016, 40, 141–144. [Google Scholar] [CrossRef]
- Solla, P.; Cugusi, L.; Bertoli, M.; Cereatti, A.; Della Croce, U.; Pani, D.; Fadda, L.; Cannas, A.; Marrosu, F.; Defazio, G.; et al. Sardinian Folk Dance for Individuals with Parkinson’s Disease: A Randomized Controlled Pilot Trial. J. Altern. Complement. Med. 2019, 25, 305–316. [Google Scholar] [CrossRef]
- Hashimoto, H.; Takabatake, S.; Miyaguchi, H.; Nakanishi, H.; Naitou, Y. Effects of Dance on Motor Functions, Cognitive Functions, and Mental Symptoms of Parkinson’s Disease: A Quasi-Randomized Pilot Trial. Complement. Ther. Med. 2015, 23, 210–219. [Google Scholar] [CrossRef]
- Hattori, H.; Hattori, C.; Hokao, C.; Mizushima, K.; Mase, T. Controlled Study on the Cognitive and Psychological Effect of Coloring and Drawing in Mild Alzheimer’s Disease Patients. Geriatr. Gerontol. Int. 2011, 11, 431–437. [Google Scholar] [CrossRef] [PubMed]
- Maeda, Y.; Fukushima, K.; Kyoutani, S.; Butler, J.P.; Fujii, M.; Sasaki, H. Dramatic Performance by a Professional Actor for the Treatment of Patients with Behavioral and Psychological Symptoms of Dementia. Tohoku J. Exp. Med. 2020, 252, 263–267. [Google Scholar] [CrossRef] [PubMed]
- Hsiao, C.Y.; Chen, S.L.; Hsiao, Y.S.; Huang, H.Y.; Yeh, S.H. Effects of Art and Reminiscence Therapy on Agitated Behaviors among Older Adults with Dementia. J. Nurs. Res. 2020, 28, e100. [Google Scholar] [CrossRef] [PubMed]
- Bisbe, M.; Fuente-Vidal, A.; López, E.; Moreno, M.; Naya, M.; De Benetti, C.; Milà, R.; Bruna, O.; Boada, M.; Alegret, M. Comparative Cognitive Effects of Choreographed Exercise and Multimodal Physical Therapy in Older Adults with Amnestic Mild Cognitive Impairment: Randomized Clinical Trial. J. Alzheimer’s Dis. 2020, 73, 769–783. [Google Scholar] [CrossRef]
- Alain, C.; Moussard, A.; Singer, J.; Lee, Y.; Bidelman, G.M.; Moreno, S. Music and Visual Art Training Modulate Brain Activity in Older Adults. Front. Neurosci. 2019, 13, 182. [Google Scholar] [CrossRef] [PubMed]
- Marquez, D.X.; Wilson, R.; Aguiñaga, S.; Vásquez, P.; Fogg, L.; Yang, Z.; Wilbur, J.; Hughes, S.; Spanbauer, C. Regular Latin Dancing and Health Education May Improve Cognition of Late Middle-Aged and Older Latinos. J. Aging Phys. Act. 2017, 25, 482–489. [Google Scholar] [CrossRef] [PubMed]
- Michels, K.; Dubaz, O.; Hornthal, E.; Bega, D. “Dance Therapy” as a Psychotherapeutic Movement Intervention in Parkinson’s Disease. Complement. Ther. Med. 2018, 40, 248–252. [Google Scholar] [CrossRef]
- Richards, A.G.; Tietyen, A.C.; Jicha, G.A.; Bardach, S.H.; Schmitt, F.A.; Fardo, D.W.; Kryscio, R.J.; Abner, E.L. Visual Arts Education Improves Self-Esteem for Persons with Dementia and Reduces Caregiver Burden: A Randomized Controlled Trial. Dementia 2018, 18, 3130–3142. [Google Scholar] [CrossRef]
- Fancourt, D.; Warran, K.; Aughterson, H.; DCMS. Evidence Summary for Policy: The Role of Arts in Improving Health and Wellbeing: Report to the Department for Digital, Culture, Media & Sport; University College London: London, UK, 2020; pp. 1–27. [Google Scholar]
- Fields, N.; Xu, L.; Greer, J.; Murphy, E. Shall I Compare Thee…to a Robot? An Exploratory Pilot Study Using Participatory Arts and Social Robotics to Improve Psychological Well-Being in Later Life. Aging Ment. Health 2019, 25, 575–584. [Google Scholar] [CrossRef]
- Kontos, P.; Miller, K.L.; Mitchell, G.J.; Stirling-Twist, J. Presence Redefined: The Reciprocal Nature of Engagement between Elder-Clowns and Persons with Dementia. Dementia 2017, 16, 46–66. [Google Scholar] [CrossRef]
- Dassa, A.; Harel, D. People with Dementia as ‘Spect-Actors’ in a Musical Theatre Group with Performing Arts Students from the Community. Arts Psychother. 2019, 65, 101592. [Google Scholar] [CrossRef]
- Loewy, J.; Torossian, A.; Appelbaum, M.; Fleming, A.; Tomaino, C. Lincoln Center Moments: Integrating Accessibility and Enhancement through Expanding Performing Arts Experiences. Arts Health 2020, 12, 182–193. [Google Scholar] [CrossRef] [PubMed]
- Uttley, L.; Scope, A.; Stevenson, M.; Rawdin, A.; Taylor Buck, E.; Sutton, A.; Stevens, J.; Kaltenthaler, E.; Dent-Brown, K.; Wood, C. Systematic Review and Economic Modelling of the Clinical Effectiveness and Cost-Effectiveness of Art Therapy among People with Non-Psychotic Mental Health Disorders. Health Technol. Assess. 2015, 19, 1–120. [Google Scholar] [CrossRef]
- Stuckey, H.L.; Nobel, J. The Connection between Art, Healing, and Public Health: A Review of Current Literature. Am. J. Public Health 2010, 100, 254–263. [Google Scholar] [CrossRef] [PubMed]
- Deygout, F. Art Therapy for Elderly Women Diagnosed with Alzheimers: A Positive Person-Centred Approach Increases Ease in the Care Process. Biomed. J. Sci. Tech. Res. 2019, 22, 16535–16547. [Google Scholar] [CrossRef]
- Mees, P. State of Mind Assessments. J. Child Psychother. 2017, 43, 380–394. [Google Scholar] [CrossRef]
- Prothmann, A.; Bienert, M.; Ettrich, C. Dogs in Child Psychotherapy: Effects on State of Mind. Anthrozoos 2006, 19, 265–277. [Google Scholar] [CrossRef]
- Thomson, L.J.; Lockyer, B.; Camic, P.M.; Chatterjee, H.J. Effects of a Museum-Based Social Prescription Intervention on Quantitative Measures of Psychological Wellbeing in Older Adults. Perspect. Public Health 2018, 138, 28–38. [Google Scholar] [CrossRef] [PubMed]
- Collins. Therapy. In Collins Dictionary. Available online: https://www.collinsdictionary.com/dictionary/english/therapy (accessed on 20 May 2022).
- Chancellor, B.; Duncan, A.; Chatterjee, A. Art Therapy for Alzheimer’s Disease and Other Dementias. J. Alzheimer’s Dis. 2014, 39, 1–11. [Google Scholar] [CrossRef]


| Reference | Year | Country | CI Typology | Nº CI Participants | Nº Groups | Mean Age Treatment | Mean Age Control | Treatment Type | Treatment Design | Study Design |
|---|---|---|---|---|---|---|---|---|---|---|
| [54] | 2019 | United States | Older adults | 53 | 3 | 67.70 | 68.50 | Group-Music | Cultural treatment vs. Cultural treatment vs. Control | Quasi-randomized |
| [53] | 2020 | Spain | Mild cognitive impairment | 31 | 2 | 72.88 | 77.29 | Group-Dance | Cultural treatment vs. Treatment | Randomized |
| [10] | 2012 | United States | Cognitive impaired | 100 | 2 | 75.58 | 77.30 | Group-Music and dance | Cultural treatment vs. Cultural treatment | Randomized |
| [47] | 2016 | Italy | Parkinson | 16 | 2 | 66.00 | 70.00 | Group-Dance | Cultural treatment vs. Treatment | Randomized |
| [36] | 2020 | Brazil | Parkinson | 18 | 2 | 68.60 | 64.20 | Group-Dance | Cultural treatment vs. Treatment | Not randomized |
| [49] | 2015 | Japan | Parkinson | 46 | 3 | 67.90 | 69.70 | Group-Dance | Cultural treatment vs. Treatment | Quasi-randomized |
| [50] | 2011 | Japan | Alzheimer | 39 | 2 | 75.30 | 73.30 | Group-Visual art | Cultural treatment vs. Treatment | Randomized |
| [52] | 2020 | Republic of China | Dementia | 54 | 3 | / | / | Group-Reminiscence | Cultural treatment vs. Treatment vs. Comparison | Randomized |
| [37] | 2020 | Canada | Dementia | 53 | 2 | 79.70 | 82.30 | Group-Visual art | Cultural treatment vs. Control | Randomized |
| [34] | 2019 | Australia | Parkinson | 33 | 2 | 65.24 | 66.50 | Group-Dance | Cultural treatment vs. Control | Not randomized |
| [35] | 2020 | Australia | Parkinson | 33 | 2 | 65.24 | 66.50 | Group-Dance | Cultural treatment vs. Control | Quasi-randomized |
| [43] | 2018 | Denmark | Alzheimer | 43 | 2 | 80.18 | 79.86 | Group-Visual art | Cultural treatment vs. Control | Randomized |
| [46] | 2017 | Greece | Mild cognitive impairment | 129 | 2 | 65.89 | 67.92 | Group-Dance | Cultural treatment vs. Control | Randomized |
| [39] | 2016 | China | Dementia | 48 | 2 | 83.10 | 81.80 | Group-Mixed | Cultural treatment vs. Control | Quasi-randomized |
| [51] | 2020 | Japan | Dementia | 34 | 2 | 84.00 | 82.00 | Group-Scenic arts | Cultural treatment vs. Control | Randomized |
| [55] | 2017 | United States | Older adults | 57 | 2 | 64.80 | 66.40 | Group-Dance | Cultural treatment vs. Control | Randomized |
| [42] | 2020 | China | Mild cognitive impairment | 39 | 2 | 73.40 | 72.00 | Group-Visual art | Cultural treatment vs. Treatment | Randomized |
| [56] | 2018 | United States | Parkinson | 13 | 2 | 66.44 | 75.50 | Group-Dance | Cultural treatment vs. Control | Randomized |
| [44] | 2017 | France | Alzheimer | 59 | 2 | 78.80 | 80.20 | Group-Music | Cultural treatment vs. Cultural treatment | Randomized |
| [45] | 2019 | France | Alzheimer | 59 | 2 | 78.80 | 80.20 | Group-Music | Cultural treatment vs. Cultural treatment | Randomized |
| [57] | 2018 | United States | Dementia | 26 | 4 | 74.80 | 74.00 | Group-Visual art | Cultural treatment vs. Control | Randomized |
| [38] | 2015 | Canada | Parkinson | 33 | 2 | 63.20 | 64.30 | Group-Dance | Cultural treatment vs. Treatment | Randomized |
| [48] | 2019 | Italy | Parkinson | 20 | 2 | 67.80 | 67.10 | Group-Dance | Cultural treatment vs. Control | Randomized |
| [7] | 2013 | Italy | Parkinson | 24 | 2 | 61.60 | 65.00 | Group-Dance | Cultural treatment vs. Treatment | Randomized |
| [41] | 2021 | China | Mild cognitive impairment | 48 | 2 | 69.00 | 66.00 | Group-Visual art | Cultural treatment vs. Control | Randomized |
| [40] | 2018 | China | Mild cognitive impairment | 93 | 2 | 70.60 | 69.50 | Group-Visual art | Cultural treatment vs. Control | Randomized |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Delfa-Lobato, L.; Feliu-Torruella, M.; Cañete-Massé, C.; Ruiz-Torras, S.; Guàrdia-Olmos, J. Benefits of Cultural Activities on People with Cognitive Impairment: A Meta-Analysis. Healthcare 2023, 11, 1854. https://doi.org/10.3390/healthcare11131854
Delfa-Lobato L, Feliu-Torruella M, Cañete-Massé C, Ruiz-Torras S, Guàrdia-Olmos J. Benefits of Cultural Activities on People with Cognitive Impairment: A Meta-Analysis. Healthcare. 2023; 11(13):1854. https://doi.org/10.3390/healthcare11131854
Chicago/Turabian StyleDelfa-Lobato, Laia, Maria Feliu-Torruella, Cristina Cañete-Massé, Silvia Ruiz-Torras, and Joan Guàrdia-Olmos. 2023. "Benefits of Cultural Activities on People with Cognitive Impairment: A Meta-Analysis" Healthcare 11, no. 13: 1854. https://doi.org/10.3390/healthcare11131854
APA StyleDelfa-Lobato, L., Feliu-Torruella, M., Cañete-Massé, C., Ruiz-Torras, S., & Guàrdia-Olmos, J. (2023). Benefits of Cultural Activities on People with Cognitive Impairment: A Meta-Analysis. Healthcare, 11(13), 1854. https://doi.org/10.3390/healthcare11131854