The Effect of Cardiorespiratory Exercise in the Prevention and Treatment of Hypertension among HIV-Infected Individuals on Antiretroviral Therapy in Mthatha, South Africa
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Enrolment Criteria
2.3. Ethical Approval
2.4. Sample Size
2.5. Sampling Procedure
2.6. Intervention
2.7. Data Collection
2.8. Definition of Variables
2.8.1. Hypertension Measure
2.8.2. Overweight and Obesity Measure
2.8.3. Social, Economic, and Demographic Measure
2.9. Data Analysis
2.10. Validity and Reliability
3. Results
3.1. Sociodemographic Characteristics of Study Participants
3.2. Physical Characteristics of the Study Participants before and after the Exercise Intervention
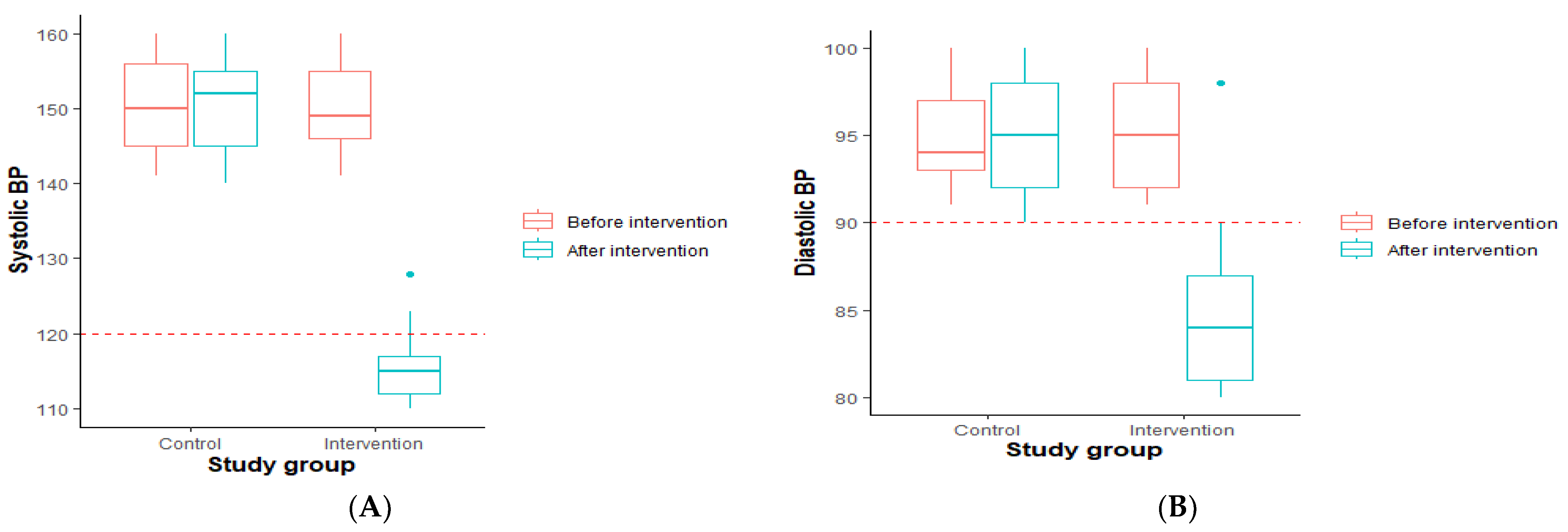
3.2.1. Comparison of Blood Pressure among the Control and Intervention Groups before and after Exercise
3.2.2. Comparison of Blood Pressure among the Control and Intervention Groups before and after Exercise, Categorized by the Participants’ Smoking and Drinking Status
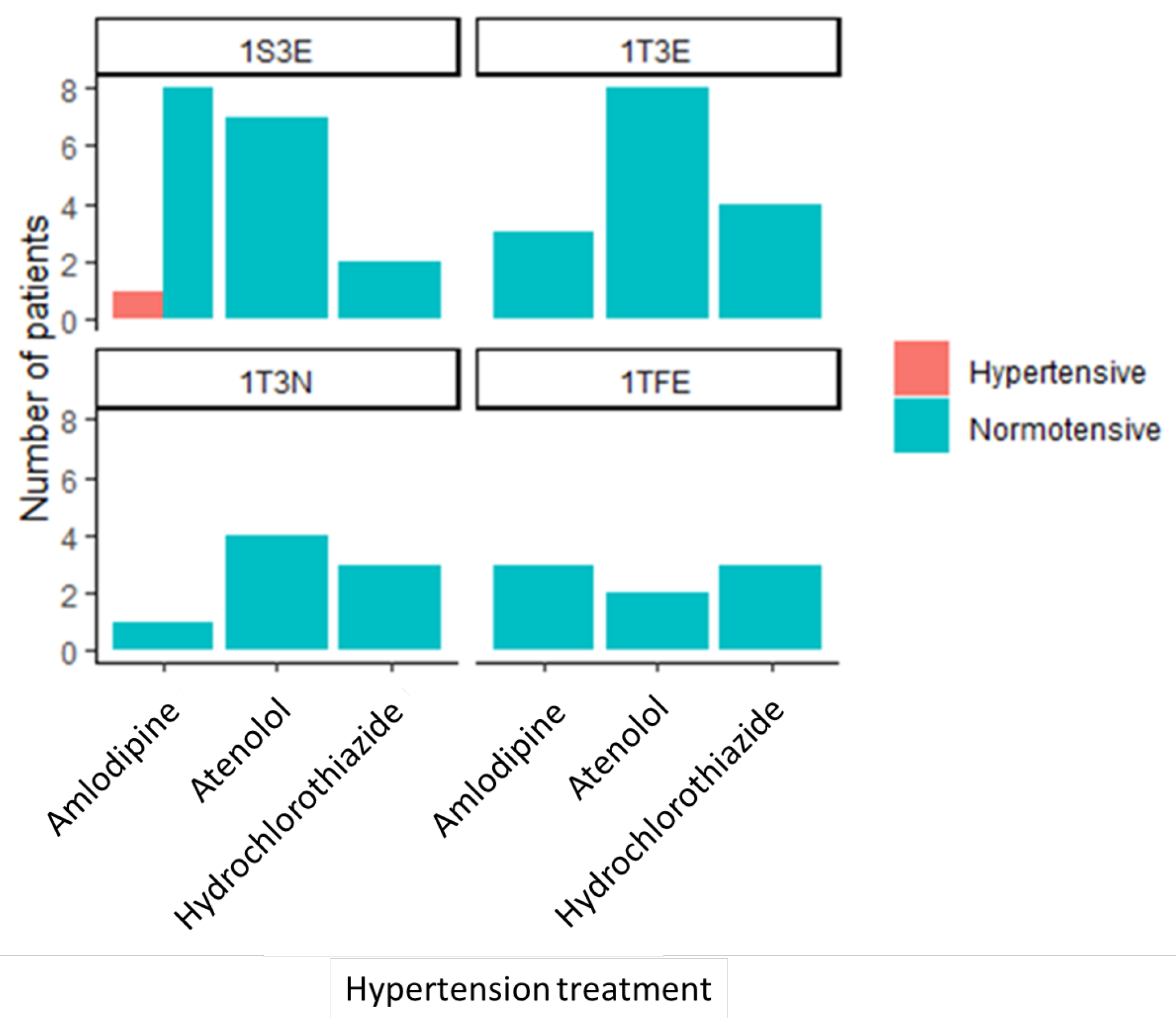
3.3. Drug-to-Drug Interaction among the Intervention Group
3.4. Variable Selection
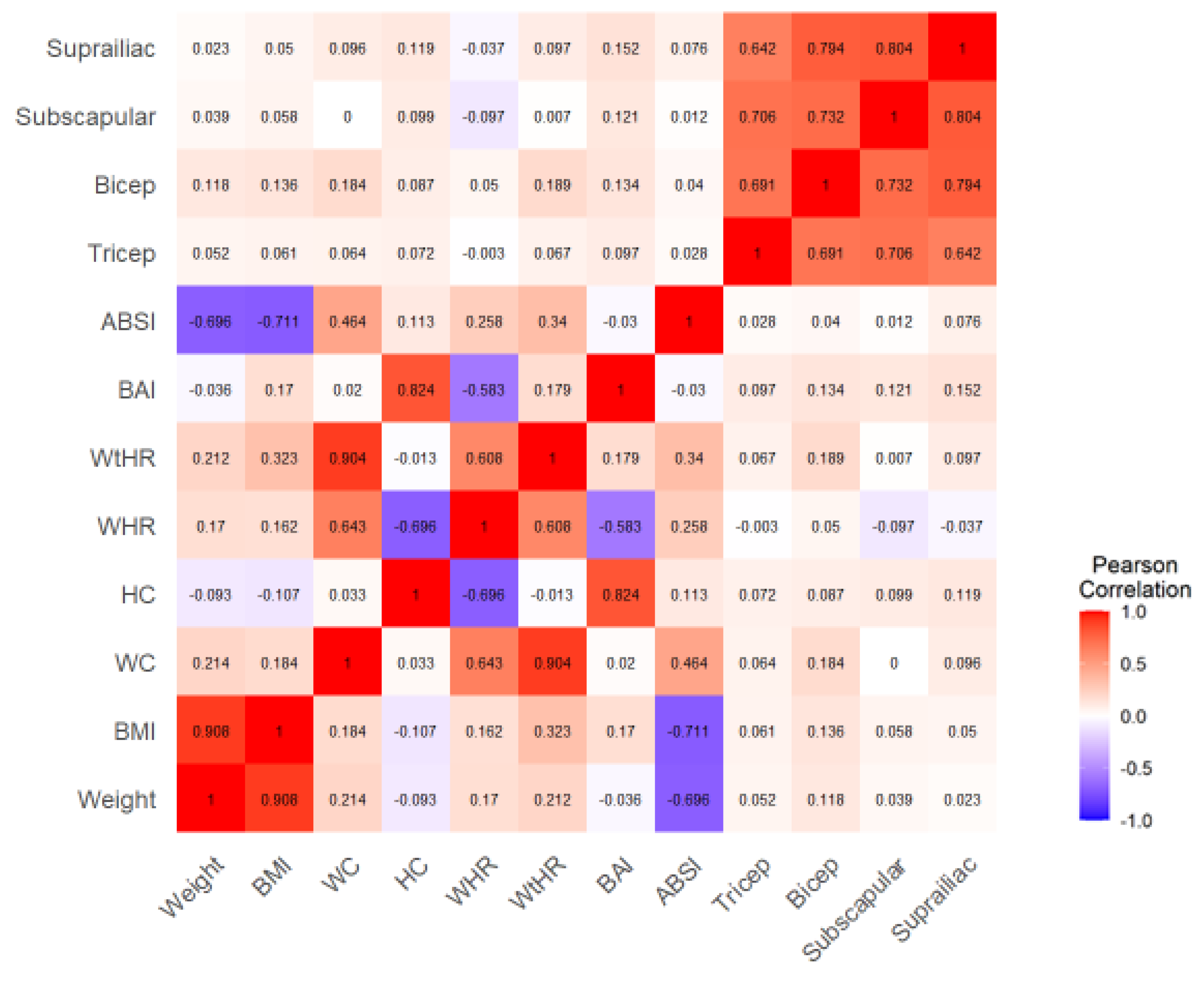
3.5. Anthropometric Factors Associated with Hypertension among PLHIV
4. Discussion
4.1. Strength
4.2. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zhao, Y.; Wu, Z.; McGoogan, J.; Shi, C.; Li, A.; Dou, Z.; Ma, Y.; Qin, Q.; Brookmeyer, R.; Detels, R.; et al. Immediate Antiretroviral Therapy Decreases Mortality among Patients with High Cd4 Counts in China: A Nationwide, Retrospective Cohort Study. Clin. Infect. Dis. 2018, 66, 727–734. [Google Scholar] [CrossRef]
- Masenga, S.K.; Elijovich, F.; Koethe, J.R.; Hamooya, B.M.; Heimburger, D.C.; Munsaka, S.M.; Laffer, C.L.; Kirabo, A. Hypertension and Metabolic Syndrome in Persons with HIV. Curr. Hypertens. Rep. 2020, 22, 78. [Google Scholar] [CrossRef]
- Pangmekeh, P.J.; Awolu, M.M.; Gustave, S.; Gladys, T.; Cumber, S.N. Association between highly active antiretroviral therapy (HAART) and hypertension in persons living with HIV/AIDS at the Bamenda regional hospital, Cameroon. Pan Afr. Med. J. 2019, 33, 87. [Google Scholar] [CrossRef] [PubMed]
- Masenga, S.K.; Hamooya, B.M.; Nzala, S.; Kwenda, G.; Heimburger, D.C.; Mutale, W.; Munsaka, S.M.; Koethe, J.R.; Kirabo, A. Patho-immune Mechanisms of Hypertension in HIV: A Systematic and Thematic Review. Curr. Hypertens. Rep. 2019, 21, 56. [Google Scholar] [CrossRef]
- Davis, K.; Perez-Guzman, P.; Hoyer, A.; Brinks, R.; Gregg, E.; Althoff, K.; Justice, A.; Reiss, P.; Gregson, S.; Smit, M. Association between Hiv Infection and Hypertension: A Global Systematic Review and Meta-Analysis of Cross-Sectional Studies. BMC Med. 2021, 19, 105. [Google Scholar]
- Stanaway, J.D.; Afshin, A.; Gakidou, E.; Lim, S.S.; Abate, D.; Abate, K.H.; Abbafati, C.; Abbasi, N.; Abbastabar, H.; Abd-Allah, F.; et al. Global, Regional, and National Comparative Risk Assessment of 84 Behavioural, Environmental and Occupational, and Metabolic Risks or Clusters of Risks for 195 Countries and Territories, 1990–2017: A Systematic Analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1923–1994. [Google Scholar]
- Roth, G.A.; Abate, D.; Abate, K.H.; Abay, S.M.; Abbafati, C.; Abbasi, N.; Abbastabar, H.; Abd-Allah, F.; Abdela, J.; Abdelalim, A.; et al. Global, Regional, and National Age-Sex-Specific Mortality for 282 Causes of Death in 195 Countries and Territories, 1980–2017: A Systematic Analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1736–1788. [Google Scholar] [CrossRef]
- Mills, K.T.; Bundy, J.D.; Kelly, T.N.; Reed, J.; Kearney, P.M.; Reynolds, K.; Chen, J.; He, J. Abstract 16828: Global Disparities of Hypertension Prevalence and Control: A Systematic Analysis of Population-based Studies From 90 Countries. Circulation 2016, 134, 441–450. [Google Scholar] [CrossRef]
- Wrottesley, S.; Micklesfield, L.; Hamill, M.M.; Goldberg, G.R.; Prentice, A.; Pettifor, J.; Norris, S.; Feeley, A.B. Dietary intake and body composition in HIV-positive and -negative South African women. Public Health Nutr. 2014, 17, 1603–1613. [Google Scholar] [CrossRef]
- Bailin, S.S.; Gabriel, C.L.; Wanjalla, C.N.; Koethe, J.R. Obesity and Weight Gain in Persons with HIV. Curr. HIV/AIDS Rep. 2020, 17, 138–150. [Google Scholar] [CrossRef]
- Strumpf, E. The Obesity Epidemic in the United States: Causes and Extent, Risks and Solutions. Issue Brief (Commonw Fund) 2004, 713, 1–6. [Google Scholar]
- Bloomgarden, Z.T. Third Annual World Congress on the Insulin Resistance Syndrome: Associated Conditions. Diabetes Care 2006, 29, 2165–2174. [Google Scholar] [CrossRef] [PubMed]
- Cheah, W.L.; Hazmi, H.; Chia, H.Q.; Tindin, E.; Zafri, N.A.A.; Shah, S.H.M. Hypertension and its association with anthropometric indexes among pre-university students. Int. J. Adolesc. Med. Health 2016, 28, 373–379. [Google Scholar] [CrossRef]
- Tadesse, T.; Alemu, H. Hypertension and Associated Factors among University Students in Gondar, Ethiopia: A Cross-Sectional Study. BMC Public Health 2014, 14, 937. [Google Scholar] [CrossRef] [PubMed]
- Silva, D.A.S.; Petroski, E.L.; Peres, M.A. Is high body fat estimated by body mass index and waist circumference a predictor of hypertension in adults? A population-based study. Nutr. J. 2012, 11, 112. [Google Scholar] [CrossRef]
- Bouchi, R.; Asakawa, M.; Ohara, N.; Nakano, Y.; Takeuchi, T.; Murakami, M.; Sasahara, Y.; Numasawa, M.; Minami, I.; Izumiyama, H.; et al. Indirect measure of visceral adiposity ‘A Body Shape Index’ (ABSI) is associated with arterial stiffness in patients with type 2 diabetes. BMJ Open Diabetes Res. Care 2016, 4, e000188. [Google Scholar] [CrossRef] [PubMed]
- Blus, E.; Wojciechowska-Kulik, A.; Majewska, E.; Baj, Z. Usefulness of New Indicators of Obesity (BAI and VAI) in Estimation of Weight Reduction. J. Am. Coll. Nutr. 2020, 39, 171–177. [Google Scholar] [CrossRef] [PubMed]
- Jiménez, E.G. Body composition: Assessment and clinical value. Endocrinol. Nutr. 2013, 60, 69–75. [Google Scholar] [CrossRef]
- Ying-Xiu, Z.; Zhao-Xia, W.; Ling, Y.; Chun-Bo, G.; Yu-Lin, G. Association between body mass index, skinfold thickness and blood pressure in 12-year-old children. Eur. J. Pediatr. 2013, 172, 1167–1171. [Google Scholar] [CrossRef]
- Ramos-Arellano, L.E.; Benito-Damián, F.; Salgado-Goytia, L.; Muñoz-Valle, J.F.; Guzmán-Guzmán, I.P.; Vences-Velázquez, A.; Castro-Alarcón, N.; Parra-Rojas, I. Body Fat Distribution and Its Association with Hypertension in a Sample of Mexican Children. J. Investig. Med. 2011, 59, 1116–1120. [Google Scholar] [CrossRef]
- Schutte, A.E.; Venkateshmurthy, N.S.; Mohan, S.; Prabhakaran, D. Hypertension in Low- and Middle-Income Countries. Circ. Res. 2021, 128, 808–826. [Google Scholar] [CrossRef] [PubMed]
- Hajjar, I.; Kotchen, J.; Kotchen, T.A. Hypertension: Trends in Prevalence, Incidence, and Control. Annu. Rev. Public Health 2006, 27, 465–490. [Google Scholar] [CrossRef] [PubMed]
- Hossain, A.; Ahmed, N.; Rahman, M.; Islam; Sadhya, G.; Fatema, K. Analysis of Sociodemographic and Clinical Factors Associated with Hospitalized Stroke Patients of Bangladesh. Faridpur Med. Coll. J. 2011, 6, 19–23. [Google Scholar] [CrossRef]
- Ibekwe, R. Modifiable Risk Factors of Hypertension and Socio-Demographic Profile in Oghara, Delta State; Prevalence and Correlates. Ann. Med. Health Sci. Res. 2015, 5, 71–77. [Google Scholar] [CrossRef]
- Ewald, D.R.; Haldeman, L.A. Risk Factors in Adolescent Hypertension. Glob Pediatr. Health 2016, 3, 1–26. [Google Scholar] [CrossRef]
- Boden-Albala, B.; Sacco, R.L. Lifestyle Factors and Stroke Risk: Exercise, Alcohol, Diet, Obesity, Smoking, Drug Use, and Stress. Curr. Atheroscler. Rep. 2000, 2, 160–166. [Google Scholar] [CrossRef]
- Pujari, S.N.; Dravid, A.; Naik, E.; Bhagat, S.; Tash, K.; Nadler, J.P.; Sinnott, J.T. Lipodystrophy and dyslipidemia among patients taking first-line, World Health Organization-recommended highly active antiretroviral therapy regimens in Western India. Am. J. Ther. 2005, 39, 199–202. [Google Scholar]
- Mutimura, E.; Stewart, A.; Crowther, N.J. The Prevalence and Metabolic Consequences of Antiretroviral-Associated Lipodystrophy in a Population of HIV-Infected African Subjects. Antiviral Therapy. 2006. Available online: https://www.researchgate.net/publication/295738077_The_prevalence_and_metabolic_consequences_of_antiretroviral-associated_lipodystrophy_in_a_population_of_HIV-infected_African_subjects (accessed on 22 June 2023).
- Egger, M.; May, M.; Chêne, G.; Phillips, A.N.; Ledergerber, B.; Dabis, F.; Costagliola, D.; Monforte, A.D.; de Wolf, F.; Reiss, P.; et al. Prognosis of HIV-1-infected patients starting highly active antiretroviral therapy: A collaborative analysis of prospective studies. Lancet 2002, 360, 119–129. [Google Scholar] [CrossRef]
- Gayle, H.D. Expanding access to HIV prevention. AIDS Res. Ther. 2006, 3, 2. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.; Hernán, A.M.; Ledergerber, B.; Tilling, K.; Weber, R.; Sendi, P.; Rickenbach, M.; Robins, J.M.; Egger, M. Long-term effectiveness of potent antiretroviral therapy in preventing AIDS and death: A prospective cohort study. Lancet 2005, 366, 378–384. [Google Scholar] [CrossRef]
- Pescatello, L.S.; Franklin, B.; Fagard, R.; Farquhar, W.; Kelley, G.; Ray, C.A. American College of Sports Medicine Position Stand. Exercise and Hypertension. Med. Sci. Sports Exerc. 2004, 36, 533–553. [Google Scholar] [CrossRef]
- Cornelissen, V.A.; Smart, N.A. Exercise training for blood pressure: A systematic review and meta-analysis. J. Am. Heart Assoc. 2013, 2, e004473. [Google Scholar] [CrossRef] [PubMed]
- Watts, K.; Beye, P.; Siafarikas, A.; Davis, E.A.; Jones, T.W.; O’Driscoll, G.; Green, D.J. Exercise training normalizes vascular dysfunction and improves central adiposity in obese adolescents. J. Am. Coll. Cardiol. 2004, 43, 1823–1827. [Google Scholar] [CrossRef] [PubMed]
- Fitch, K.V.; Anderson, E.J.; Hubbard, J.L.; Carpenter, S.J.; Waddell, W.R.; Caliendo, A.M.; Grinspoon, S.K. Effects of a lifestyle modification program in HIV-infected patients with the metabolic syndrome. Aids 2006, 20, 1843–1850. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, K.; Nixon, S.; Tynan, A.-M.; Glazier, R. Aerobic exercise interventions for adults living with HIV/AIDS. Cochrane Database Syst. Rev. 2010, 2010, CD001796. [Google Scholar] [CrossRef] [PubMed]
- Barros, J.P.; de Paula, T.; Mediano, M.; Rangel, M.; Monteiro, W.; da Cunha, F.; Farinatti, P.; Borges, J.P. The Effects of Acute Aerobic Exercise on Blood Pressure, Arterial Function, and Heart Rate Variability in Men Living with HIV. Front. Physiol. 2021, 12, 685306. [Google Scholar] [CrossRef]
- Statistics South Africa. Census 2022; Statistics South Africa: Pretoria, South Africa, 2022. [Google Scholar]
- Hansoti, B.; Mwinnyaa, G.; Hahn, E.; Rao, A.; Black, J.; Chen, V.; Clark, K.; Clarke, W.; Eisenberg, A.L.; Fernandez, R.; et al. Targeting the HIV Epidemic in South Africa: The Need for Testing and Linkage to Care in Emergency Departments. Eclinicalmedicine 2019, 15, 14–22. [Google Scholar] [CrossRef]
- Zuma, K.; Simbayi, L.; Zungu, N.; Moyo, S.; Marinda, E.; Jooste, S.; North, A.; Nadol, P.; Aynalem, G.; Igumbor, E.; et al. The HIV Epidemic in South Africa: Key Findings from 2017 National Population-Based Survey. Int. J. Environ. Res. Public Health 2022, 19, 8125. [Google Scholar] [CrossRef] [PubMed]
- The World Medical Association. World Medical Association Declaration of Helsinki. Recommendations Guiding Physicians in Biomedical Research Involving Human Subjects. JAMA 1997, 277, 925–926. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.-G. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef]
- Ingle, A.S.; Kashyap, N.K.; Trivedi, S.; Chaudhary, R.; Suryavanshi, G.; Thangaraju, P.; Bagale, K.R. Assessment of Body Fat Percentage Using B-Mode Ultrasound Technique versus Skinfold Caliper in Obese Healthy Volunteers. Cureus 2022, 14, e22993. [Google Scholar] [CrossRef]
- Cakit, M.O.; Çakit, B.; Genç, H.; Vural, S.P.; Erdem, H.; Saraçoğlu, M.; Karagöz, A. The Association of Skinfold Anthropometric Measures, Body Composition and Disease Severity in Obese and Non-Obese Fibromyalgia Patients: A Cross-Sectional Study. Arch. Rheumatol. 2018, 33, 59–65. [Google Scholar]
- James, P.A.; Oparil, S.; Carter, B.; Cushman, W.; Dennison-Himmelfarb, C.; Handler, J.; Lackland, D.; LeFevre, M.; MacKenzie, T.; Ogedegbe, O.; et al. 2014 Evidence-Based Guideline for the Management of High Blood Pressure in Adults: Report from the Panel Members Appointed to the Eighth Joint National Committee (Jnc 8). JAMA 2014, 311, 507–520. [Google Scholar] [CrossRef] [PubMed]
- WHO. Obesity: Preventing and Managing the Global Epidemic: Report of a WHO Consultation; WHO Technical Report Series; WHO: Geneva, Switzerland, 2000; 252p. [Google Scholar]
- Krakauer, N.Y.; Krakauer, J.C. A New Body Shape Index Predicts Mortality Hazard Independently of Body Mass Index. PLoS ONE 2012, 7, e39504. [Google Scholar] [CrossRef] [PubMed]
- Freedman, D.; SThornton, J.; Pi-Sunyer, F.; Heymsfield, S.; Wang, J.; Pierson, R., Jr.; Blanck, H.; Gallagher, D. The Body Adiposity Index (Hip Circumference ÷ Height(1.5)) Is Not a More Accurate Measure of Adiposity Than Is Bmi, Waist Circumference, or Hip Circumference. Obesity 2012, 20, 2438–2444. [Google Scholar] [CrossRef] [PubMed]
- Harimenshi, D.; Niyongabo, T.; Preux, P.-M.; Aboyans, V.; Desormais, I. Hypertension and associated factors in HIV-infected patients receiving antiretroviral treatment in Burundi: A cross-sectional study. Sci. Rep. 2022, 12, 20509. [Google Scholar] [CrossRef]
- Hsue, P.Y.; Deeks, S.G.; Hunt, P.W. Immunologic Basis of Cardiovascular Disease in HIV-Infected Adults. J. Infect. Dis. 2012, 205, S375–S382. [Google Scholar] [CrossRef]
- McMurray, R.G.; Harrell, J.S.; Bangdiwala, I.S.; Bradley, C.B.; Deng, S.; Levine, A. A school-based intervention can reduce body fat and blood pressure in young adolescents. J. Adolesc. Health 2002, 31, 125–132. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, A.; Rodriguez, K.J.; Sabag, A.; Mavros, Y.; Parker, H.M.; Keating, S.E.; Johnson, N.A. Effect of aerobic exercise on waist circumference in adults with overweight or obesity: A systematic review and meta-analysis. Obes. Rev. 2022, 23, e13446. [Google Scholar] [CrossRef]
- Alpsoy, Ş. Exercise and Hypertension. Adv. Exp. Med. Biol. 2020, 1228, 153–167. [Google Scholar]
- Wang, M.; Li, W.; Zhou, R.; Wang, S.; Zheng, H.; Jiang, J.; Wang, S.; Yu, C.; Gao, W.; Lv, J.; et al. The Paradox Association between Smoking and Blood Pressure among Half Million Chinese People. Int. J. Environ. Res. Public Health 2020, 17, 2824. [Google Scholar] [CrossRef] [PubMed]
- Peyriere, H.; Eiden, C.; Macia, J.-C.; Reynes, J. Antihypertensive Drugs in Patients Treated with Antiretroviral. Ann. Pharmacother. 2012, 46, 703–709. [Google Scholar] [CrossRef] [PubMed]
- Leblanc, E.S.; O’Connor, E.; Whitlock, E.; Patnode, C.; Kapka, T. Effectiveness of Primary Care-Relevant Treatments for Obesity in Adults: A Systematic Evidence Review for the U.S. Preventive Services Task Force. Ann. Intern. Med. 2011, 155, 434–447. [Google Scholar] [CrossRef] [PubMed]
- Cox, C.E. Role of Physical Activity for Weight Loss and Weight Maintenance. Diabetes Spectr. 2017, 30, 157–160. [Google Scholar] [CrossRef]
- Park, S.-H.; Kim, C.-G. Effects of aerobic exercise on waist circumference, VO2 max, blood glucose, insulin, and lipid index in middle-aged women: A meta-analysis of randomized controlled trials. Health Care Women Int. 2021, 43, 1158–1180. [Google Scholar] [CrossRef] [PubMed]

| Variable | N | Overall, N = 98 1 | Control, N = 49 1 | Intervention, N = 49 1 | p-Value 2 |
|---|---|---|---|---|---|
| Age category | 98 | >0.9 | |||
| 15–30 years | 18 (18%) | 9 (18%) | 9 (18%) | ||
| 31–40 years | 24 (24%) | 12 (24%) | 12 (24%) | ||
| >40 years | 56 (57%) | 28 (57%) | 28 (57%) | ||
| Gender, n (%) | 98 | >0.9 | |||
| Female | 60 (61%) | 30 (61%) | 30 (61%) | ||
| Male | 38 (39%) | 19 (39%) | 19 (39%) | ||
| Marital status, n (%) | 98 | 0.8 | |||
| Single | 45 (46%) | 22 (45%) | 23 (47%) | ||
| Cohabiting | 2 (2.0%) | 2 (4.1%) | 0 (0%) | ||
| Married | 31 (32%) | 14 (29%) | 17 (35%) | ||
| Divorced | 8 (8.2%) | 4 (8.2%) | 4 (8.2%) | ||
| Widowed | 12 (12%) | 7 (14%) | 5 (10%) | ||
| Education, n (%) | 98 | 0.055 | |||
| None | 6 (6.1%) | 5 (10%) | 1 (2.0%) | ||
| Primary | 18 (18%) | 6 (12%) | 12 (24%) | ||
| Matric | 68 (69%) | 37 (76%) | 31 (63%) | ||
| Tertiary | 6 (6.1%) | 1 (2.0%) | 5 (10%) | ||
| Employment status, n (%) | 98 | 0.4 | |||
| Employed | 34 (35%) | 19 (39%) | 15 (31%) | ||
| Unemployed | 64 (65%) | 30 (61%) | 34 (69%) | ||
| Smoking status, n (%) | 98 | 0.5 | |||
| Non-smokers | 86 (88%) | 42 (86%) | 44 (90%) | ||
| Smokers | 12 (12%) | 7 (14%) | 5 (10%) | ||
| Alcohol consumption, n (%) | 98 | 0.3 | |||
| Non-drinker | 78 (80%) | 37 (76%) | 41 (84%) | ||
| Drinker | 20 (20%) | 12 (24%) | 8 (16%) |
| Before | After | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Variable | N | Overall, N = 98 1 | Control, N = 49 1 | Intervention, N = 49 1 | p-Value 2 | N | Overall, N = 98 1 | Control, N = 49 1 | Intervention, N = 49 1 | p-Value 2 |
| Tricep (mm) | 98 | 13 (4) | 14 (4) | 13 (4) | 0.9 | 98 | 13 (4) | 15 (4) | 11 (3) | <0.001 |
| Bicep (mm) | 98 | 7.79 (2.45) | 7.90 (2.49) | 7.67 (2.42) | 0.9 | 98 | 6.7 (3.1) | 8.6 (1.8) | 4.7 (2.9) | <0.001 |
| Subscapular (mm) | 98 | 19 (4) | 19 (4) | 19 (3) | >0.9 | 98 | 17 (3) | 18 (2) | 16 (3) | <0.001 |
| Suprailiac (mm) | 98 | 19 (4) | 20 (4) | 19 (3) | 0.5 | 98 | 18 (3) | 19 (3) | 16 (4) | <0.001 |
| Weight (kg) | 98 | 98 (19) | 97 (18) | 98 (19) | 0.7 | 98 | 93 (21) | 101 (20) | 86 (19) | 0.001 |
| BMI (kg/m2) | 98 | 40 (9) | 39 (8) | 40 (10) | 0.6 | 98 | 38 (10) | 41 (9) | 35 (10) | 0.005 |
| BMI category | 98 | >0.9 | 98 | 0.001 | ||||||
| <25 kg/m2 | 4 (4.1%) | 2 (4.1%) | 2 (4.1%) | 13 (13%) | 1 (2.0%) | 12 (24%) | ||||
| ≥25 kg/m2 | 94 (96%) | 47 (96%) | 47 (96%) | 85 (87%) | 48 (98%) | 37 (76%) | ||||
| WC (cm) | 98 | 101 (9) | 100 (9) | 102 (9) | 0.10 | 98 | 92 (12) | 100 (10) | 83 (9) | <0.001 |
| HC (cm) | 98 | 101 (12) | 101 (12) | 101 (12) | >0.9 | 98 | 99 (12) | 101 (12) | 97 (11) | 0.045 |
| WHR | 98 | 0.98 (0.16) | 1.00 (0.15) | 0.96 (0.16) | 0.2 | 98 | 0.94 (0.17) | 1.00 (0.16) | 0.88 (0.16) | <0.001 |
| WtHR | 98 | 0.64 (0.07) | 0.63 (0.07) | 0.65 (0.07) | 0.076 | 98 | 0.58 (0.08) | 0.63 (0.06) | 0.53 (0.06) | <0.001 |
| BAI | 98 | 33 (7) | 33 (6) | 34 (7) | 0.7 | 98 | 32 (7) | 33 (6) | 31 (7) | 0.2 |
| ABSI | 98 | 0.72 (0.13) | 0.70 (0.11) | 0.74 (0.16) | 0.3 | 98 | 0.67 (0.14) | 0.69 (0.13) | 0.65 (0.15) | 0.10 |
| SBP (mmHg) | 98 | 150 (6) | 150 (6) | 150 (6) | 0.6 | 98 | 133 (19) | 151 (6) | 115 (4) | <0.001 |
| DBP (mmHg) | 98 | 95 (3) | 95 (3) | 95 (3) | 0.5 | 98 | 90 (6) | 95 (3) | 84 (4) | <0.001 |
| HTN status, n (%) | 98 | >0.9 | 98 | <0.001 | ||||||
| Hypertensive | 98(100%) | 49(100%) | 49(100%) | 50 (51%) | 49 (100%) | 1 (2.0%) | ||||
| Normotensive | 0(0%) | 0(0%) | 0(0%) | 48 (49%) | 0 (0%) | 48 (98%) | ||||
| Variable | OR 1 | 95% CI | p-Value |
|---|---|---|---|
| Bicep (mm) | 1.08 | 0.99, 1.19 | 0.090 |
| Subscapular (mm) | 1.42 | 0.95, 2.31 | 0.11 |
| Suprailiac (mm) | 0.86 | 0.60, 1.21 | 0.4 |
| Body Mass Index (kg/m2) | 1.71 | 1.20, 2.63 | 0.006 |
| Waist Circumference (mm) | 1.33 | 1.17, 1.61 | <0.001 |
| Body Adiposity Index | 1.00 | 0.88, 1.12 | >0.9 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tsuro, U.; Oladimeji, K.E.; Pulido-Estrada, G.-A.; Apalata, T.R. The Effect of Cardiorespiratory Exercise in the Prevention and Treatment of Hypertension among HIV-Infected Individuals on Antiretroviral Therapy in Mthatha, South Africa. Healthcare 2023, 11, 1836. https://doi.org/10.3390/healthcare11131836
Tsuro U, Oladimeji KE, Pulido-Estrada G-A, Apalata TR. The Effect of Cardiorespiratory Exercise in the Prevention and Treatment of Hypertension among HIV-Infected Individuals on Antiretroviral Therapy in Mthatha, South Africa. Healthcare. 2023; 11(13):1836. https://doi.org/10.3390/healthcare11131836
Chicago/Turabian StyleTsuro, Urgent, Kelechi Elizabeth Oladimeji, Guillermo-Alfredo Pulido-Estrada, and Teke Ruffin Apalata. 2023. "The Effect of Cardiorespiratory Exercise in the Prevention and Treatment of Hypertension among HIV-Infected Individuals on Antiretroviral Therapy in Mthatha, South Africa" Healthcare 11, no. 13: 1836. https://doi.org/10.3390/healthcare11131836
APA StyleTsuro, U., Oladimeji, K. E., Pulido-Estrada, G.-A., & Apalata, T. R. (2023). The Effect of Cardiorespiratory Exercise in the Prevention and Treatment of Hypertension among HIV-Infected Individuals on Antiretroviral Therapy in Mthatha, South Africa. Healthcare, 11(13), 1836. https://doi.org/10.3390/healthcare11131836






