Exploring Older Adults’ Perceived Affordability and Accessibility of the Healthcare System: Empirical Evidence from the Chinese Social Survey 2021
Abstract
1. Introduction
2. Literature Review
2.1. Healthcare System Reform in China
2.2. Public Perceptions of the Healthcare System
2.3. Patient Experience and Public Perception
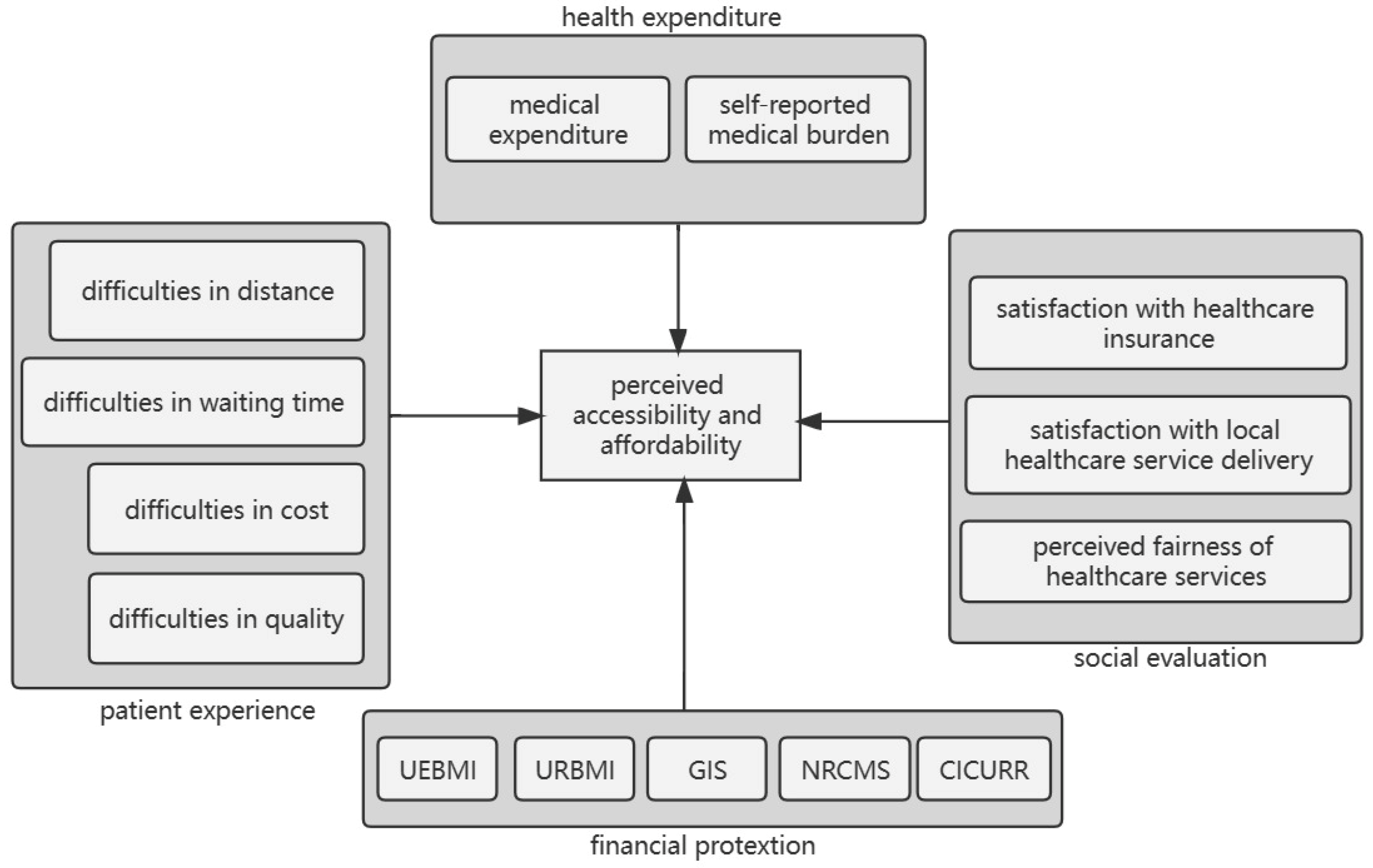
2.4. Conceptual Framework
3. Method
3.1. Data and Sampling
3.2. Variables
3.2.1. Dependent Measure
3.2.2. Independent Measures
3.2.3. Statistical Analysis
4. Findings
4.1. Descriptive Characteristics of the Sample
4.2. Logistic Regression Model of Perceived Affordability and Accessibility
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Tao, W.J.; Zeng, Z.; Dang, H.X.; Lu, B.Q.; Chuong, L.; Yue, D.H.; Wen, J.; Zhao, R.; Li, W.M.; Kominski, G.F. Towards universal health coverage: Lessons from 10 years of healthcare reform in China. BMJ Glob. Health 2020, 5, e002086. [Google Scholar] [CrossRef] [PubMed]
- Ta, Y.Q.; Zhu, Y.S.; Fu, H.Q. Trends in access to health services, financial protection and satisfaction between 2010 and 2016: Has China achieved the goals of its health system reform? Soc. Sci. Med. 2020, 245, 112715. [Google Scholar] [CrossRef] [PubMed]
- Yip, W.; Fu, H.Q.; Chen, A.T.; Zhai, T.M.; Jian, W.Y.; Xu, R.; Pan, J.; Hu, M.; Zhou, Z.L.; Chen, Q.L.; et al. 10 years of health-care reform in China: Progress and gaps in universal health coverage. Lancet 2019, 394, 1192–1204. [Google Scholar] [CrossRef] [PubMed]
- National Bureau of Statistics. Report of the Seventh National Population Census. Available online: http://www.gov.cn/guoqing/2021-05/13/content_5606149.htm (accessed on 11 May 2023).
- Bao, J.B.; Zhou, L.; Liu, G.H.; Tang, J.; Lu, X.; Cheng, C.; Jin, Y.Y.; Bai, J.J. Current state of care for the elderly in China in the context of an aging population. Biosci. Trends 2022, 16, 107–118. [Google Scholar] [CrossRef] [PubMed]
- Han, Y.Y.; He, Y.; Lyu, J.; Yu, C.Q.; Bian, M.Z.; Lee, L. Aging in China: Perspectives on public health. Glob. Health J. 2020, 4, 11–17. [Google Scholar] [CrossRef]
- Yip, W.; Hsiao, W.C. What drove the cycles of Chinese health system reforms? Health Syst. Reform 2015, 1, 52–61. [Google Scholar] [CrossRef]
- Hsiao, W.; Li, M.Q.; Zhang, S.F. Universal Health Coverage: The Case of China; UNRISD Working Paper, No. 2014–2015; United Nations Research Institute for Social Development: Geneva, Switzerland, 2015. [Google Scholar]
- Liu, G.G.; Vortherms, S.A.; Hong, X.Z. China’s health reform update. Annu. Rev. Public Health 2017, 38, 431–448. [Google Scholar] [CrossRef]
- Li, Z.; Li, J. Lessons and prospects of universal health coverage in China: The importance of equity, quality, and affordability. Asian Bioeth. Rev. 2019, 11, 21–40. [Google Scholar] [CrossRef]
- Zhao, C.R.; Wang, C.; Shen, C.W.; Wang, Q. China’s achievements and challenges in improving health insurance coverage. Drug Discov. Ther. 2018, 12, 1–6. [Google Scholar] [CrossRef]
- Zhang, X.P.; Xiong, Y.Q.; Ye, J.; Deng, Z.H.; Zhang, X.P. Analysis of government investment in primary healthcare institutions to promote equity during the three-year health reform program in China. BMC Health Serv. Res. 2013, 13, 114. [Google Scholar] [CrossRef]
- Wang, H.H.X.; Wang, J.J.; Wong, S.Y.S.; Wong, M.C.S.; Mercer, S.W.; Griffiths, S.M. The development of urban community health centres for strengthening primary care in China: A systematic literature review. Br. Med. Bull. 2015, 116, 139–153. [Google Scholar] [CrossRef] [PubMed]
- Meng, Q.Y.; Yin, D.X.; Mills, A.; Abbasi, K. China’s encouraging commitment to health. BMJ 2019, 365, l4178. [Google Scholar] [CrossRef] [PubMed]
- Li, H.Z.; Liu, K.; Gu, J.J.; Zhang, Y.M.; Qiao, Y.; Sun, X.M. The development and impact of primary health care in China from 1949 to 2015: A focused review. Int. J. Health Plann. Manag. 2017, 32, 339–350. [Google Scholar] [CrossRef] [PubMed]
- Wu, D.; Lam, T.P. Underuse of primary care in China: The scale, causes, and solutions. J. Am. Board Fam. Med. 2016, 29, 240–247. [Google Scholar] [CrossRef]
- Fu, L.P.; Fang, Y.N.; Yang, S.; Xu, Y.Q. How to make primary healthcare more popular: Evidence from the middle-aged and elderly in China. Healthcare 2022, 10, 1783. [Google Scholar] [CrossRef]
- Fang, G.X.; Yang, D.L.; Wang, L.; Wang, Z.H.; Liang, Y.Y.; Yang, J.X. Experiences and challenges of implementing universal health coverage with China’s national basic public health service program: Literature review, regression analysis, and insider interviews. JMIR Public Health Surveill. 2022, 8, e31289. [Google Scholar] [CrossRef]
- Wang, N.S.; Gao, W.; Ma, M.Y.; Shan, L.H.; Fu, X.L.; Sun, T.; Xia, Q.; Tian, W.X.; Liu, L.M.; Yang, H.Y.; et al. The medical insurance system’s weakness to provide economic protection for vulnerable citizens in China: A five-year longitudinal study. Arch. Gerontol. Geriatr. 2021, 92, 104227. [Google Scholar] [CrossRef]
- Wang, X.Q.; Chen, P.J. Population ageing challenges health care in China. Lancet 2014, 383, 870. [Google Scholar] [CrossRef]
- Teng, H.Y.; Cao, Z.Z.; Liu, J.L.; Liu, P.; Hua, W.; Yang, Y.; Xiong, L.P. Health status and burden of health care costs among urban elderly in China. Asia Pac. J. Public Health 2015, 27, 61S–68S. [Google Scholar] [CrossRef]
- Eggleston, K. Kan bing nan, kan bing gui: Challenges for China’s healthcare system thirty years into reform. In Growing Pains: Tensions and Opportunities in China’s Transformation; Oi, J.C., Rozelle, S., Zhou, X.G., Eds.; Brookings Institution Press: Baltimore, MD, USA, 2010; pp. 229–272. [Google Scholar]
- Zhang, J.H.; Peng, X.X.; Liu, C.K.; Chen, Y.J.; Zhang, H.M.; Iwaloye, O.O. Public satisfaction with the healthcare system in China during 2013–2015: A cross-sectional survey of the associated factors. BMJ Open 2020, 10, e034414. [Google Scholar] [CrossRef]
- Lee, S.Y.; Suh, N.K.; Song, J.K. Determinants of public satisfaction with the National Health Insurance in South Korea. Int. J. Health Plan. Manag. 2009, 24, 131–146. [Google Scholar] [CrossRef] [PubMed]
- Yuan, Y.Q. Public satisfaction with health care system in 30 countries: The effects of individual characteristics and social contexts. Health Policy 2021, 125, 1359–1366. [Google Scholar] [CrossRef] [PubMed]
- Ruelens, A. Analyzing user-generated content using natural language processing: A case study of public satisfaction with healthcare systems. J. Comput. Soc. Sci. 2022, 5, 731–749. [Google Scholar] [CrossRef] [PubMed]
- Papanicolas, I.; Cylus, J.; Smith, P.C. An analysis of survey data from eleven countries finds that ‘satisfaction’ with health system performance means many things. Health Aff. 2013, 32, 734–742. [Google Scholar] [CrossRef]
- Munro, N.; Duckett, J. Explaining public satisfaction with health-care systems: Findings from a nationwide survey in China. Health Expect. 2016, 19, 654–666. [Google Scholar] [CrossRef]
- Nie, J.B.; Cheng, Y.; Zou, X.; Gong, N.; Tucker, J.D.; Wong, B.; Kleinman, A. The vicious circle of patient–physician mistrust in China: Health professionals’ perspectives, institutional conflict of interest, and building trust through medical professionalism. Dev. World Bioeth. 2018, 18, 26–36. [Google Scholar] [CrossRef]
- Wang, M.S.; Raynard, M.; Greenwood, R. From grace to violence: Stigmatizing the medical profession in China. Acad. Manag. J. 2021, 64, 1842–1872. [Google Scholar] [CrossRef]
- Sun, J.; Liu, S.Y.; Liu, Q.N.; Wang, Z.J.; Wang, J.; Hu, C.J.; Stuntz, M.; Ma, J.; Liu, Y.L. Impact of adverse media reporting on public perceptions of the doctor–patient relationship in China: An analysis with propensity score matching method. BMJ Open 2018, 8, e022455. [Google Scholar] [CrossRef]
- Bleich, S.N.; Özaltin, E.; Murray, C.J.L. How does satisfaction with the health-care system relate to patient experience? Bull. World Health Organ. 2009, 87, 271–278. [Google Scholar] [CrossRef]
- Ahmed, F.; Burt, J.; Roland, M. Measuring patient experience: Concepts and methods. Patient 2014, 7, 235–241. [Google Scholar] [CrossRef]
- Kumah, E. Patient experience and satisfaction with a healthcare system: Connecting the dots. Int. J. Healthcare Man. 2019, 12, 173–179. [Google Scholar] [CrossRef]
- Hougaard, J.L.; Østerdal, L.P.; Yu, Y. The Chinese healthcare system: Structure, problems and challenges. Appl. Health Econ. Health Policy 2011, 9, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Zou, X.; Cheng, Y.; Nie, J.B. The social practice of medical guanxi (personal connections) and patient-physician trust in China: An anthropological and ethical study. Dev. World Bioeth. 2018, 18, 45–55. [Google Scholar] [CrossRef] [PubMed]
- Tucker, J.D.; Cheng, Y.; Wong, B.; Gong, N.; Nie, J.B.; Zhu, W.; McLaughlin, M.M.; Xie, R.S.; Deng, Y.H.; Huang, M.J.; et al. Patient–physician mistrust and violence against physicians in Guangdong Province, China: A qualitative study. BMJ Open 2015, 5, e008221. [Google Scholar] [CrossRef] [PubMed]
- Hu, H.; Xu, J.G.; Zhang, X. The role of housing wealth, financial wealth, and social welfare in elderly households’ consumption behaviors in China. Cities 2020, 96, 102437. [Google Scholar] [CrossRef]
- Peng, X.X.; Zhang, J.H. Socioeconomic inequality in public satisfaction with the healthcare system in China: A quantile regression analysis. Arch. Public Health 2022, 80, 165. [Google Scholar] [CrossRef]
- Chen, J.E.; Lou, V.W.; Jian, H.; Zhou, Z.; Yan, M.Q.; Zhu, J.F.; Li, G.H.; He, Y.Q. Objective and subjective financial burden and its associations with health-related quality of life among lung cancer patients. Support Care Cancer 2018, 26, 1265–1272. [Google Scholar] [CrossRef]
- Qian, H.; Li, G.B.; Chen, H.X.; Zhang, D.L. An exploratory research of patient perceived value in China. J. Med. Mark. 2011, 11, 277–283. [Google Scholar] [CrossRef]
- Zhu, Y.S.; Li, Y.Y.; Wu, M.; Fu, H.Q. How do Chinese people perceive their healthcare system? Trends and determinants of public satisfaction and perceived fairness, 2006–2019. BMC Health Serv. Res. 2022, 22, 22. [Google Scholar] [CrossRef]
- Zhou, Q.; He, Q.; Eggleston, K.; Liu, G.G. Urban-rural health insurance integration in China: Impact on health care utilization, financial risk protection, and health status. Appl. Econ. 2022, 54, 2491–2509. [Google Scholar] [CrossRef]
- Shan, L.H.; Zhao, M.H.; Ning, N.; Hao, Y.H.; Li, Y.; Liang, L.B.; Kang, Z.; Sun, H.; Ding, D.; Liu, B.H.; et al. Dissatisfaction with current integration reforms of health insurance schemes in China: Are they a success and what matters? Health Policy Plan. 2018, 33, 345–354. [Google Scholar] [CrossRef] [PubMed]
- Meng, Q.Y.; Fang, H.; Liu, X.Y.; Yuan, B.B.; Xu, J. Consolidating the social health insurance schemes in China: Towards an equitable and efficient health system. Lancet 2015, 386, 1484–1492. [Google Scholar] [CrossRef] [PubMed]
- Xi, Y.M.; Ding, Y.; Cheng, Y.N.; Zhao, J.J.; Zhou, M.Q.; Qin, S.R. Evaluation of the medical resource allocation: Evidence from China. Healthcare 2023, 11, 829. [Google Scholar] [CrossRef]
- Chen, D.J.; Lang, Y.X. The cream-skimming effect in China’s health care services: A mixed methods study. Int. J. Health Plan. Manag. 2021, 36, 113–133. [Google Scholar] [CrossRef] [PubMed]
- Brixi, H.; Mu, Y.; Targa, B.; Hipgrave, D. Engaging sub-national governments in addressing health equities: Challenges and opportunities in China’s health system reform. Health Policy Plan. 2013, 28, 809–824. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.F.; Liu, N. Health reform and out-of-pocket payments: Lessons from China. Health Policy Plan. 2014, 29, 217–226. [Google Scholar] [CrossRef]
- Huang, J.W. Income inequality, distributive justice beliefs, and happiness in China: Evidence from a nationwide survey. Soc. Indic. Res. 2019, 142, 83–105. [Google Scholar] [CrossRef]
- Liu, Q.Y.; Lucas, K.; Marsden, G.; Liu, Y. Egalitarianism and public perception of social inequities: A case study of Beijing congestion charge. Transp. Policy 2019, 74, 47–62. [Google Scholar] [CrossRef]
- Cooke, F.L. Public-sector pay in China: 1949–2001. In Human Resource Management in China Revisited; Malcolm, W., Ed.; Routledge: London, UK, 2005; pp. 279–300. [Google Scholar]
- Wu, D.; Lam, T.P.; Lam, K.F.; Zhou, X.D.; Sun, K.S. Challenges to healthcare reform in China: Profit-oriented medical practices, patients’ choice of care and guanxi culture in Zhejiang province. Health Policy Plan. 2017, 32, 1241–1247. [Google Scholar] [CrossRef]
- Zhang, T.; Xu, Y.J.; Ren, J.P.; Sun, L.Q.; Liu, C.J. Inequality in the distribution of health resources and health services in China: Hospitals versus primary care institutions. Int. J. Equity Health 2017, 16, 42. [Google Scholar] [CrossRef]
- Li, C.F.; Dou, L.; Wang, H.P.; Jing, S.S.; Yin, A.T. Horizontal inequity in health care utilization among the middle-aged and elderly in China. Int. J. Environ. Res. Public Health 2017, 14, 842. [Google Scholar] [CrossRef] [PubMed]
- Tan, S.Y.; Wu, X.; Yang, W. Impacts of the Type of Social Health Insurance on Health Service Utilisation and Expenditures: Implications for a Unified System in China. Health Econ. Policy Law 2019, 14, 468–486. [Google Scholar] [CrossRef] [PubMed]
- Fu, X.Z.; Sun, N.; Xu, F.; Li, J.; Tang, Q.X.; He, J.J.; Wang, D.D.; Sun, C.Q. Influencing factors of inequity in health services utilization among the elderly in China. Int. J. Equity Health 2018, 17, 144. [Google Scholar] [CrossRef] [PubMed]
- State Council. Proposal of the State Council on Integrating the Basic Medical Insurance System for Urban and Rural Residents. Available online: https://www.gov.cn/zhengce/content/2016-01/12/content_10582.htm (accessed on 11 May 2023).
| Variable | Variable Type | Percentage | Mean (SD) | N | |
|---|---|---|---|---|---|
| Dependent variable | |||||
| Affordability and Accessibility | No = 0 | 45.5% | - | 2169 | |
| Yes = 1 | 54.5% | ||||
| Demographic characteristics | 2169 | ||||
| Gender | Male (1) | 48.0% | |||
| Female (2) | 52.0% | ||||
| Age | - | 64.92 (2.75) | |||
| Education level | Primary education or below (1) | 50.3% | |||
| Secondary school (2) | 26.9% | ||||
| College or above (3) | 17.8% | ||||
| Annual income | - | - | 18,569.12 (23,629.29) | ||
| Residency | Urban (1) | 48.1% | |||
| Rural (2) | 51.9% | ||||
| Independent variables | |||||
| Healthcare expenditure | |||||
| Medical expenditure | Continuous | - | 10,271.27 (33,948.3) | 1986 | |
| Medical burden | No = 0 | 58.6% | - | 2169 | |
| Yes = 1 | 41.4% | ||||
| Patient experience | |||||
| Difficulties in distance | Continuous | - | 3.17 (0.987) | 1636 | |
| Difficulties in waiting time | Continuous | - | 3.14 (0.994) | 1637 | |
| Difficulties in cost | Continuous | - | 2.37 (1.101) | 1582 | |
| Difficulties in quality | Continuous | - | 3.18 (0.944) | 1515 | |
| Social evaluation | |||||
| Satisfaction with healthcare insurance | Continuous | - | 6.23 (3.351) | 2021 | |
| Satisfaction with local healthcare service delivery | Continuous | - | 2.80 (1.267) | 2013 | |
| Perceived fairness of healthcare services | Continuous | - | 2.55 (1.420) | 1957 | |
| Financial protection | |||||
| Insurance coverage | No = 0 | 34.8% | - | 2130 | |
| Yes = 1 | 64.2% | ||||
| Own UEBMI | No = 0 | 74.4% | 1388 | ||
| Yes = 1 | 25.6% | ||||
| Own URBMI | No = 0 | 88.0% | 1388 | ||
| Yes = 1 | 12.0% | ||||
| Own GIS | No = 0 | 92.4% | 1388 | ||
| Yes = 1 | 7.6% | ||||
| Own NRCMS | No = 0 | 40.0% | 1388 | ||
| Yes = 1 | 60.0% | ||||
| Own CICURR | No = 0 | 93.2% | 1388 | ||
| Yes = 1 | 6.8% | ||||
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B (OR) | SE | 95%CI | B (OR) | SE | 95%CI | B (OR) | SE | 95%CI | B (OR) | SE | 95%CI | B (OR) | SE | 95%CI | |
| Demographic characteristics | |||||||||||||||
| Gender | 0.15 (1.16) | 0.09 | 0.97–1.40 | 0.07 (1.08) | 0.10 | 0.89–1.31 | 0.14 (1.15) | 0.13 | 0.90–1.48 | 0.25 (1.29) | 0.16 | 0.94–1.77 | 0.23 (1.26) | 0.18 | 0.89–1.77 |
| Age | −0.03 (0.97) | 0.02 | 0.94–1.00 | −0.03 (0.97) | 0.02 | 0.94–1.00 | −0.02 (0.98) | 0.02 | 0.94–1.03 | −0.03 (0.97) | 0.03 | 0.92–1.03 | −0.02 (0.98) | 0.03 | 0.92–1.04 |
| Education level | |||||||||||||||
| Secondary school | 0.26 * (1.30) | 0.11 | 1.05–1.61 | 0.29 * (1.34) | 0.12 | 1.06–1.69 | 0.23 (1.25) | 0.15 | 0.94–1.68 | 0.36 (1.44) | 0.19 | 0.99–2.11 | 0.17 (1.19) | 0.21 | 0.78–1.79 |
| College or above | 0.39 ** (1.48) | 0.13 | 1.14–1.91 | 0.40 ** (1.50) | 0.14 | 1.14–1.97 | 0.31 (1.36) | 0.18 | 0.96–1.93 | 0.40 (1.50) | 0.24 | 0.95–2.37 | 0.26 (1.30) | 0.25 | 0.80–2.12 |
| Annual income | <0.01 (1.00) | <0.01 | 1.00–1.00 | <0.01 (1.00) | <0.01 | 1.00–1.00 | <0.01 (1.00) | <.01 | 1.00–1.00 | <0.01 (1.00) | <0.01 | 1.00–1.00 | <0.01 (1.00) | <0.01 | 1.00–1.00 |
| Region | 0.01 (1.01) | 0.10 | 0.84–1.22 | −0.04 (0.97) | 0.10 | 0.79–1.18 | 0.07 (1.07) | 0.13 | 0.83–1.39 | −0.11 (0.89) | 0.19 | 0.62–1.29 | −0.04 (0.96) | 0.20 | 0.65–1.43 |
| Healthcare expenditure | |||||||||||||||
| Medical expenditure | <0.01 (1.00) | <0.01 | 1.00–1.00 | <0.01 * (1.00) | <.01 | 1.00–1.00 | <0.01 (1.00) | <0.01 | 1.00–1.00 | <0.01 (1.00) | <0.01 | 1.00–1.00 | |||
| Medical burden | 0.82 *** (2.28) | 0.10 | 1.87–2.77 | 0.48 *** (1.61) | 0.13 | 1.26–2.07 | 0.38 * (1.46) | 0.16 | 1.06–2.02 | 0.24 * (1.27) | 0.18 | 0.89–1.80 | |||
| Patient experience | |||||||||||||||
| Distance | −0.01 (0.99) | 0.07 | 0.86–1.14 | −0.04 (0.96) | 0.09 | 0.81–1.15 | −0.06 (0.95) | 0.10 | 0.78–1.15 | ||||||
| Waiting time | −0.05 (0.95) | 0.08 | 0.82–1.11 | 0.09 (1.09) | 0.09 | 0.91–1.30 | 0.13 (1.14) | 0.10 | 0.93–1.39 | ||||||
| Cost | −0.52 *** (0.60) | 0.07 | 0.52–0.68 | −0.64 *** (0.53) | 0.09 | 0.45–0.63 | −0.60 *** (0.55) | 0.10 | 0.46–0.67 | ||||||
| Quality | 0.02 (1.02) | 0.07 | 0.89–1.17 | 0.08(1.09) | 0.09 | 0.91–1.30 | 0.13 (1.14) | 0.10 | 0.93–1.39 | ||||||
| Financial protection | |||||||||||||||
| Own UEBMI | 0.09 (1.10) | 0.32 | 0.59–2.04 | 0.38 (1.46) | 0.35 | 0.74–2.88 | |||||||||
| Own URBMI | −0.09 (0.92) | 0.30 | 0.51–1.66 | 0.15 (1.16) | 0.33 | 0.61–2.22 | |||||||||
| Own GIS | −0.19 (0.83) | 0.36 | 0.41–1.68 | −0.05 (0.95) | 0.40 | 0.43–2.07 | |||||||||
| Own NRCMS | 0.21 (1.24) | 0.32 | 0.66–2.31 | 0.48 (1.61) | 0.35 | 0.81–3.17 | |||||||||
| Own CICURR | −0.18 (0.84) | 0.29 | 0.48–1.46 | −0.11 (0.90) | 0.31 | 0.49–1.65 | |||||||||
| Social evaluation | |||||||||||||||
| Satisfaction with healthcare insurance | −0.04 (0.96) | 0.04 | 0.90–1.03 | ||||||||||||
| Satisfaction with local healthcare delivery | −0.11 (0.89) | 0.13 | 0.69–1.16 | ||||||||||||
| Fairness of healthcare services | −0.37 ** (0.69) | 0.12 | 0.54–0.88 | ||||||||||||
| N | 2060 | 1882 | 1283 | 817 | 727 | ||||||||||
| Nagelkerke R2 | 0.01 | 0.06 | 0.15 | 0.17 | 0.22 | ||||||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, L.; Cheng, M. Exploring Older Adults’ Perceived Affordability and Accessibility of the Healthcare System: Empirical Evidence from the Chinese Social Survey 2021. Healthcare 2023, 11, 1818. https://doi.org/10.3390/healthcare11131818
Chen L, Cheng M. Exploring Older Adults’ Perceived Affordability and Accessibility of the Healthcare System: Empirical Evidence from the Chinese Social Survey 2021. Healthcare. 2023; 11(13):1818. https://doi.org/10.3390/healthcare11131818
Chicago/Turabian StyleChen, Lu, and Miaoting Cheng. 2023. "Exploring Older Adults’ Perceived Affordability and Accessibility of the Healthcare System: Empirical Evidence from the Chinese Social Survey 2021" Healthcare 11, no. 13: 1818. https://doi.org/10.3390/healthcare11131818
APA StyleChen, L., & Cheng, M. (2023). Exploring Older Adults’ Perceived Affordability and Accessibility of the Healthcare System: Empirical Evidence from the Chinese Social Survey 2021. Healthcare, 11(13), 1818. https://doi.org/10.3390/healthcare11131818





