Effectiveness of Health Promotion Interventions in Primary Schools—A Mixed Methods Literature Review
Abstract
1. Introduction
1.1. Promoting Health in Schools
1.2. Components of the School-Based HPIs Related to the Effectiveness
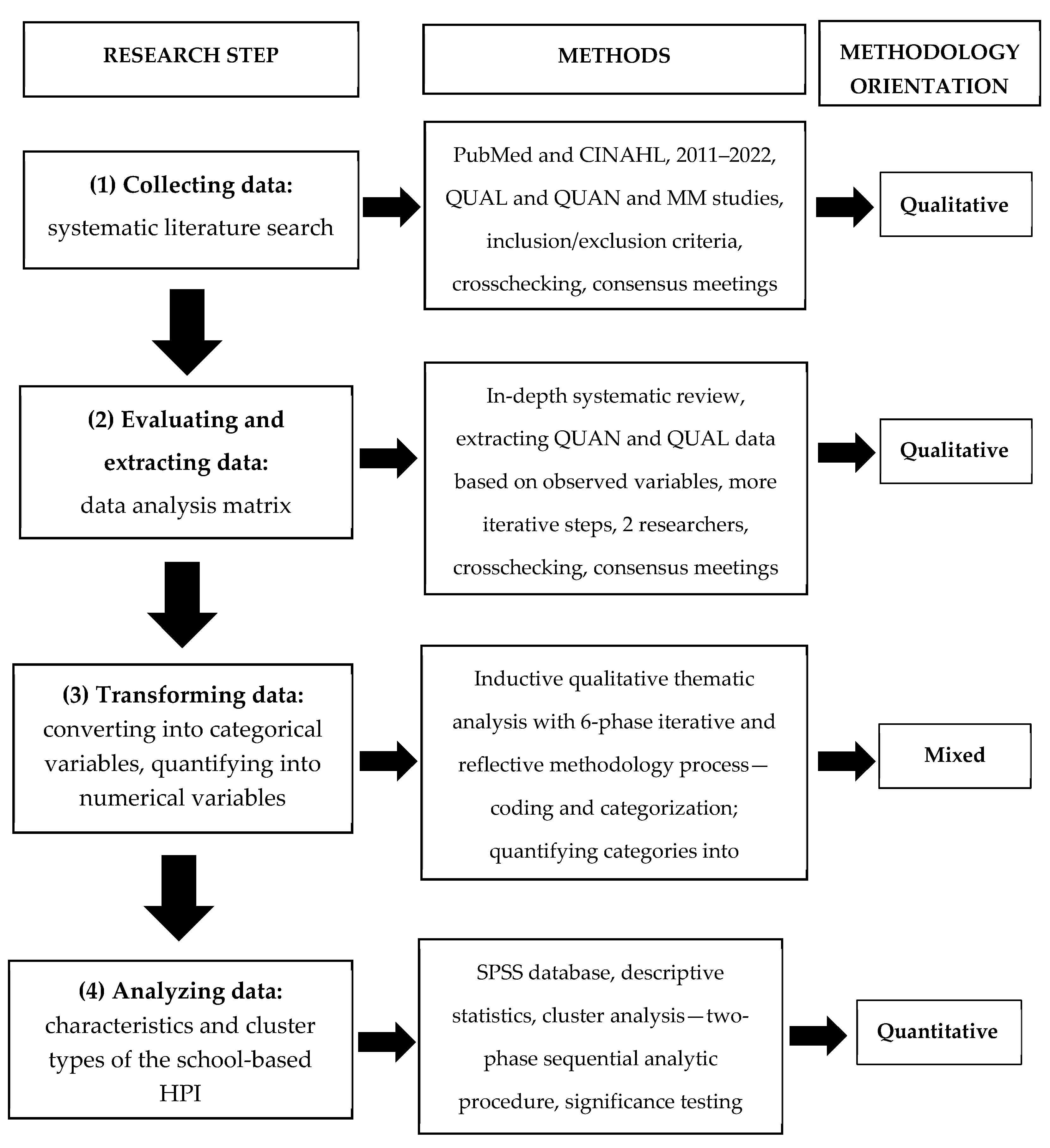
2. Methods
2.1. Conducting the Mixed Methods Literature Review
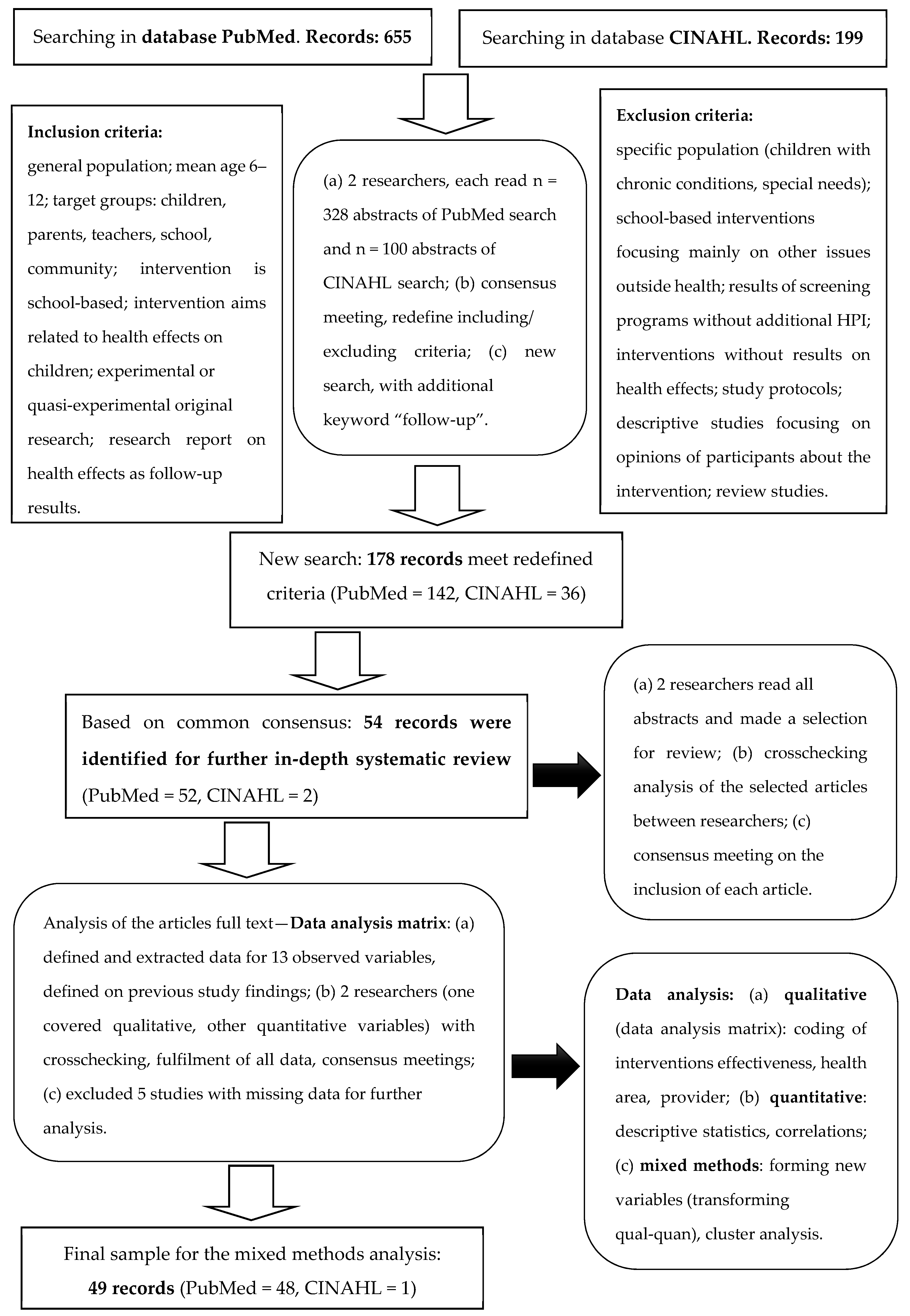
2.2. Procedure of the Literature Search and Literature Selection
2.3. Data Extraction and Categorization
2.4. Quantitative Data Analysis
3. Results
3.1. Characteristics of the School-Based HPIs
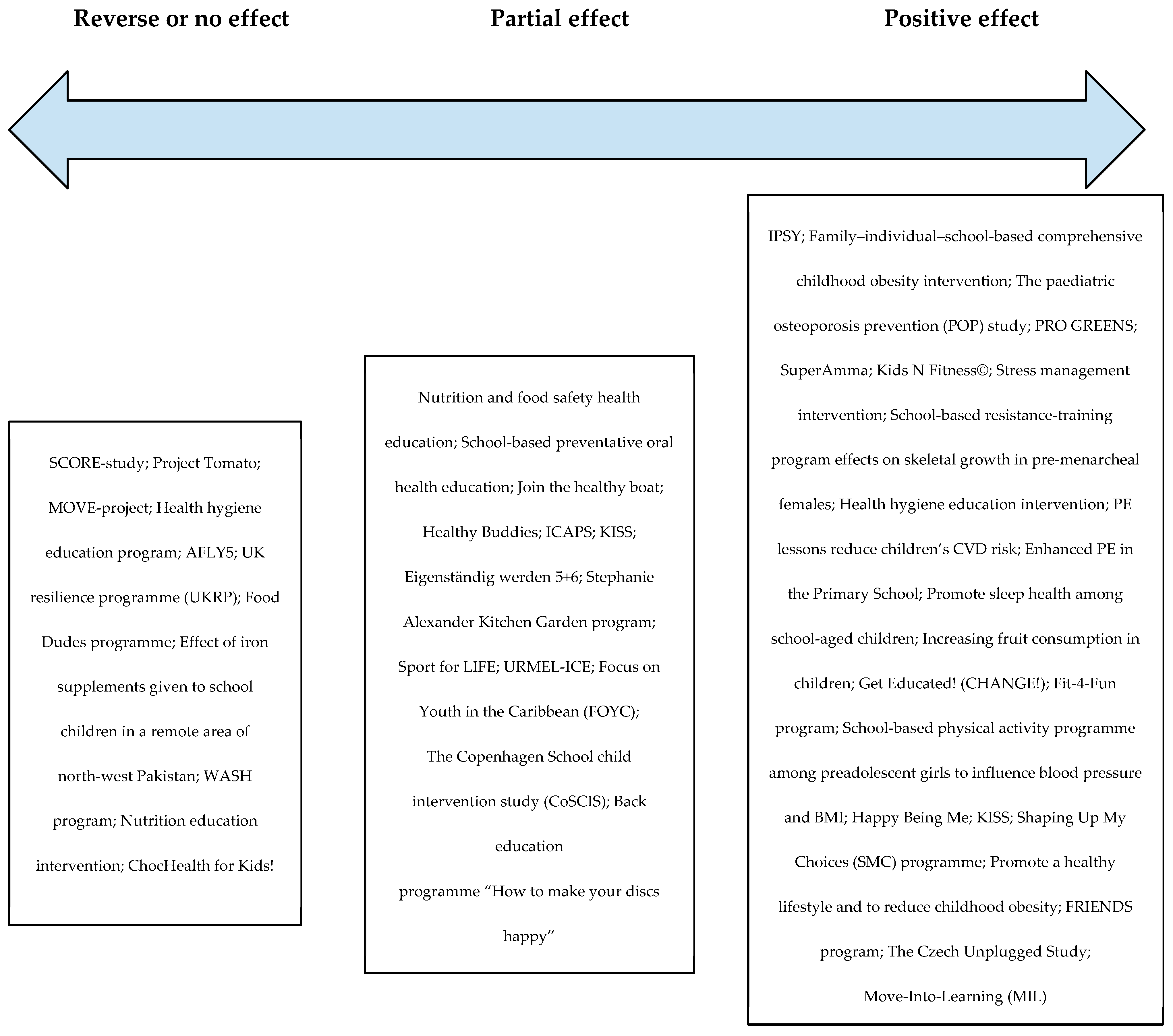
3.2. Effectiveness of the Interventions
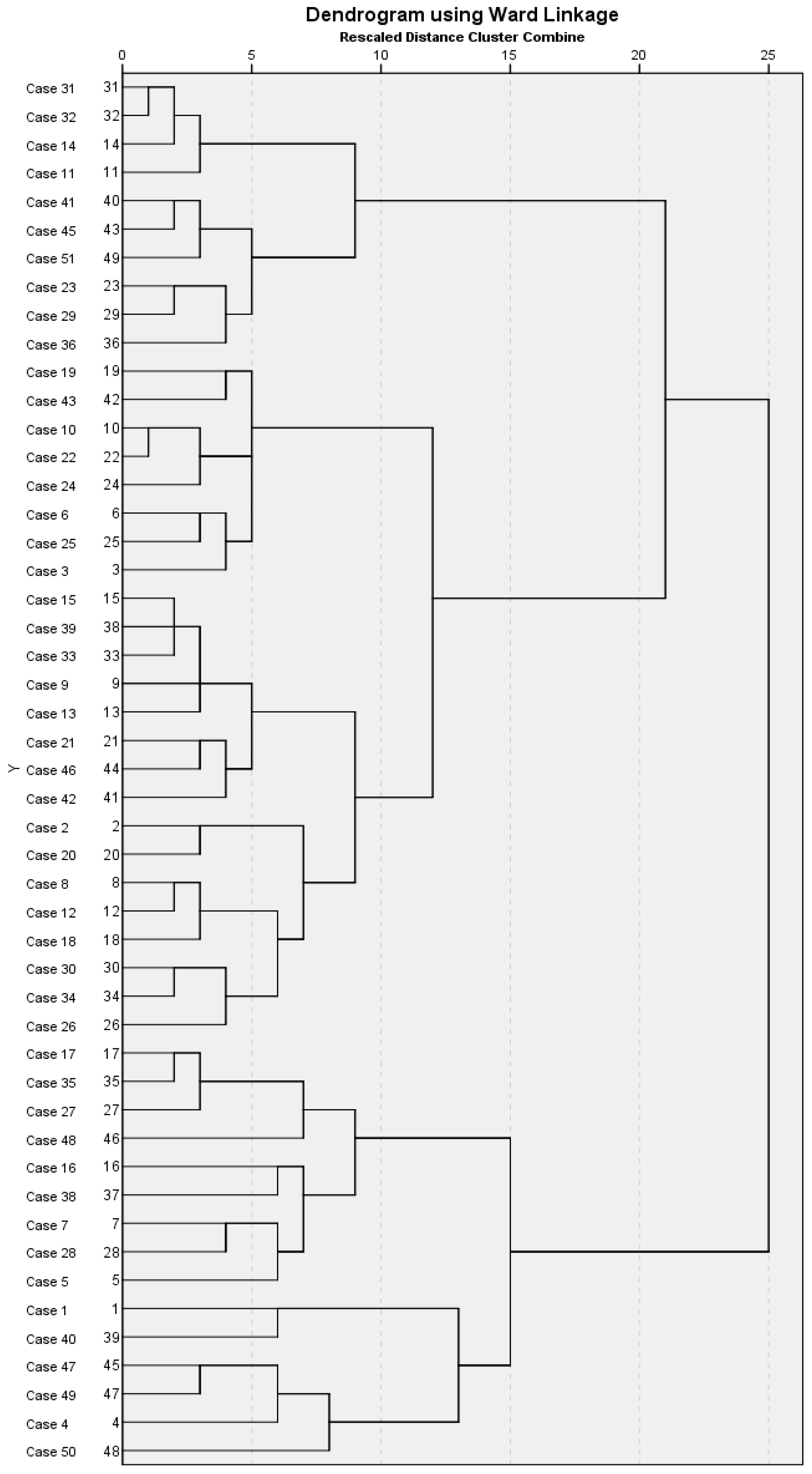
3.3. Cluster Types of the School-Based HPIs
3.3.1. Cluster 1: “Extensive and Long-Term HPI”
3.3.2. Cluster 2: “School Policy-Changing HPI”
3.3.3. Cluster 3: “Highly Effective HPI”
3.4. The Relationships between Structures of HPIs and Their Effectiveness on the Mental and Physical Well-Being of Primary School Children
4. Discussion
4.1. Cluster Types of the School-Based HPIs
4.2. Key Structural Elements of the Effective School-Based HPIs
4.3. Implications for Educational Research and School Practice
4.4. Limitations of the Present Review and Directions for Future Studies
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Joung, K.H.; Chung, S.S. Factors related to depressive symptoms among multicultural adolescents in Korea. J. Sch. Nurs. 2022, 38, 138–147. [Google Scholar] [CrossRef]
- Laaksonen, C.; Aromaa, M.E.; Asanti, R.E.; Heinonen, O.J.; Koivusilta, L.K.; Koski, P.; Suominen, S.B.; Vahlberg, T.J.; Salanterä, S. The change in child self-assessed and parent proxy–assessed Health Related Quality of Life (HRQL) in early adolescence (age 10–12). Scand. J. Public Health 2010, 38, 9–16. [Google Scholar] [CrossRef]
- Moore, G.F.; Littlecott, H.J.; Turley, R.; Waters, E.; Murphy, S. Socioeconomic gradients in the effects of universal school-based health behaviour interventions: A systematic review of intervention studies. BMC Public Health 2015, 15, 907. [Google Scholar] [CrossRef]
- Lima-Serrano, M.; Lima-Rodríguez, J.S. Impact of school-based health promotion interventions aimed at different behavioral domains: A systematic review. Gac. Sanit. 2014, 28, 411–417. [Google Scholar] [CrossRef][Green Version]
- Salerno, J.P. Effectiveness of universal school-based mental health awareness programs among youth in the United States: A systematic review. J. Sch. Health 2016, 86, 922–931. [Google Scholar] [CrossRef]
- Stentiford, L.; Koutsouris, G.; Allan, A. Girls, mental health and academic achievement: A qualitative systematic review. Educ. Rev. 2021. [Google Scholar] [CrossRef]
- Zurc, J.; Planinšec, J. Associations between physical activity and academic competence: A cross-sectional study among Slovenian primary school students. Int. J. Environ. Res. Public Health 2022, 19, 623. [Google Scholar] [CrossRef] [PubMed]
- Snyder, K.E.; Fong, C.J.; Painter, J.K.; Pittard, C.M.; Barr, S.M.; Patall, E.A. Interventions for academically underachieving students: A systematic review and meta-analysis. Educ. Res. Rev. 2019, 28, 100294. [Google Scholar] [CrossRef]
- Delnoij, L.E.C.; Dirkx, K.J.H.; Janssen, J.P.W.; Martens, R.L. Predicting and resolving non-completion in higher (online) education: A literature review. Educ. Res. Rev. 2020, 29, 100313. [Google Scholar] [CrossRef]
- Jourdan, D.; Christensen, J.H.; Darlington, E.; Bonde, A.H.; Bloch, P.; Jensen, B.B.; Bentsen, P. The involvement of young people in school- and community-based noncommunicable disease prevention interventions: A scoping review of designs and outcomes. BMC Public Health 2016, 16, e1123. [Google Scholar] [CrossRef] [PubMed]
- Dowling, K.; Barry, M.M. Evaluating the implementation quality of a Social and Emotional Learning Program: A mixed methods approach. Int. J. Environ. Res. Public Health 2020, 17, 3249. [Google Scholar] [CrossRef] [PubMed]
- Hillier-Brown, F.C.; Bambra, C.L.; Cairn, J.M.; Kasim, A.; Moore, H.; Summerbell, C.D. A systematic review of the effectiveness of individual, community and societal level interventions at reducing socioeconomic inequalities in obesity amongst children. BMC Public Health 2014, 14, 834. [Google Scholar] [CrossRef] [PubMed]
- Love, R.E.; Adams, J.; van Sluijs, E.M.F. Equity effects of children’s physical activity interventions: A systematic scoping review. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 134. [Google Scholar] [CrossRef] [PubMed]
- Racey, M.; O’Brien, C.; Douglas, S.; Marquez, O.; Hendrie, G.; Newton, G. Systematic review of school-based interventions to modify dietary behavior: Does intervention intensity impact effectiveness? J. Sch. Health 2016, 86, 452–463. [Google Scholar] [CrossRef] [PubMed]
- Dugan, J.E. Teaching the body: A systematic review of posture interventions in primary schools. Educ. Rev. 2018, 70, 643–661. [Google Scholar] [CrossRef]
- Health Promoting Schools; World Health Organization: Copenhagen, Denmark, 2017; Available online: http://apps.who.int/iris/bitstream/handle/10665/255625/WHO-NMH-PND-17.3-eng.pdf;jsessionid=2B8953A151196ABBDACC07F4BBB55593?sequence=1 (accessed on 2 March 2023).
- UNICEF Data: Monitoring the Situation of Children and Women; UNICEF: New York, NY, USA, 2018; Available online: https://data.unicef.org/topic/education/primary-education/ (accessed on 2 March 2023).
- Petosa, R.L.; Smith, L. Effective recruitment of schools for randomized clinical trials: Role of school nurses. J. Sch. Nurs. 2017, 34, 430–434. [Google Scholar] [CrossRef]
- Singh, A.; Bassi, S.; Nazar, G.P.; Saluja, K.; Park, M.H.; Kinra, S.; Arora, M. Impact of school policies on noncommunicable disease risk factors: A systematic review. BMC Public Health 2017, 17, 292. [Google Scholar] [CrossRef]
- Carney, T.; Myers, B.J.; Louw, J.; Okwundu, C.I. Brief school-based interventions and behavioural outcomes for substance-using adolescents. Cochrane Database Syst. Rev. 2016, 1, CD008969. [Google Scholar] [CrossRef]
- Thomas, R.E.; McLellan, J.; Perera, R. School-based programmes for preventing smoking. Cochrane Database Syst. Rev. 2013, 4, CD001293. [Google Scholar] [CrossRef]
- Limone, P.; Toto, G.A. Psychological strategies and protocols for promoting school well-being: A systematic review. Front. Psychol. 2022, 13, 914063. [Google Scholar] [CrossRef]
- Chen, C.; Yang, C.; Nie, Q. Social–emotional learning competencies and problematic internet use among Chinese adolescents: A structural equation modelling analysis. Int. J. Environ. Res. Public Health 2021, 18, 3091. [Google Scholar] [CrossRef] [PubMed]
- Santamaría-Villar, M.B.; Gilar-Corbi, R.; Pozo-Rico, T.; Castejón, J.L. Teaching socio-emotional competencies among primary school students: Improving conflict resolution and promoting democratic co-existence in schools. Front. Psychol. 2021, 12, 659348. [Google Scholar] [CrossRef] [PubMed]
- La Grutta, S.; Epifanio, M.S.; Piombo, M.A.; Alfano, P.; Maltese, A.; Marcantonio, S.; Ingoglia, S.; Alesi, M.; Lo Baido, R.; Mancini, G.; et al. Emotional competence in primary school children: Examining the effect of a psycho-educational group intervention: A pilot prospective study. Int. J. Environ. Res. Public Health 2022, 19, 7628. [Google Scholar] [CrossRef] [PubMed]
- Moore, G.F.; Littlecott, H.J. School- and family-level socioeconomic status and health behaviors: Multilevel analysis of a national survey in Wales, United Kingdom. J. Sch. Health 2015, 85, 267–275. [Google Scholar] [CrossRef]
- Peters, L.W.; Kok, G.; TenDam, G.T.; Buijis, G.J.; Paulussen, T.G. Effective elements of school health promotion across behavioral domains: A systematic review of reviews. BMC Public Health 2009, 9, 182. [Google Scholar] [CrossRef]
- Shackleton, N.; Jamal, F.; Viner, R.M.; Dickson, K.; Patton, G.; Bonell, C. School-based interventions going beyond health education to promote adolescent health: Systematic review of reviews. J. Adolesc. Health 2016, 58, 382–396. [Google Scholar] [CrossRef]
- Hung, T.T.M.; Chiang, V.C.L.; Dawson, A.; Lee, R.L.T. Understanding of factors that enable health promoters in implementing health-promoting schools: A systematic review and narrative synthesis of qualitative evidence. PLoS ONE 2014, 9, e108284. [Google Scholar] [CrossRef]
- Langford, R.; Bonnell, C.P.; Johen, H.E.; Pouliou, T.; Murphy, S.M.; Waters, E.; Komro, K.A.; Gibbs, L.F.; Magnus, D.; Campbell, R. The WHO Health Promoting School framework for improving the health and well-being of students and their academic achievement. Cochrane Database Syst. Rev. 2014, 16, CD008958. [Google Scholar] [CrossRef]
- Grant, M.J.; Booth, A. A typology of reviews: An analysis of 14 review types and associated methodologies. Health Inf. Libr. J. 2009, 26, 91–108. [Google Scholar] [CrossRef]
- Harden, A. Mixed methods systematic reviews: Integrating quantitative and qualitative findings. FOCUS Tech. Brief. 2010, 25, 1–8. Available online: http://ktdrr.org/ktlibrary/articles_pubs/ncddrwork/focus/focus25/ (accessed on 2 March 2023).
- Pluye, P.; Hong, Q.N. Combining the power of stories and the power of numbers: Mixed methods research and mixed studies reviews. Annu. Rev. Public Health 2014, 35, 29–45. [Google Scholar] [CrossRef]
- Zurc, J. Validity Assessment Criteria for the Mixed Methods Research. Ph.D. Dissertation, Faculty of Social Sciences, University of Ljubljana, Ljubljana, Slovenia, 10 October 2017. Available online: http://dk.fdv.uni-lj.si/doktorska_dela/pdfs/dr_zurc-joca.pdf (accessed on 2 March 2023).
- Creswell, J.W.; Clark, V.L.P. Designing and Conducting Mixed Methods Research, 3rd ed.; Sage Publications, Inc.: Thousand Oaks, CA, USA, 2017. [Google Scholar]
- Nowell, L.S.; Norris, J.M.; White, D.E.; Moules, N.J. Thematic analysis: Striving to meet the trustworthiness criteria. Int. J. Qual. Methods 2017, 16, 1609406917733847. [Google Scholar] [CrossRef]
- Andermann, A.; Pang, T.; Newton, J.N.; Davis, A.; Panisset, U. Evidence for health I: Producing evidence for improving health and reducing inequities. Health Res. Policy Syst. 2016, 14, 18. [Google Scholar] [CrossRef] [PubMed]
- Schneider, S.; Huy, C.; Schuessler, M.; Diehl, K.; Schwarz, S. Optimising lifestyle interventions: Identification of health behaviour patterns by cluster analysis in a German 50+ survey. Eur. J. Public Health 2009, 19, 271–277. [Google Scholar] [CrossRef] [PubMed]
- Doron, J.; Trouillet, R.; Maneveau, A.; Neveu, D.; Ninot, G. Coping profiles, perceived stress and health-related behaviors: A cluster analysis approach. Health Promot. Int. 2014, 30, 88–100. [Google Scholar] [CrossRef] [PubMed]
- Ferligoj, A. Razvrščanje v Skupine: Teorija in Uporaba v Družboslovju [Cluster Analysis: Theory and Application in Social Sciences]; Faculty of Social Sciences, University of Ljubljana: Ljubljana, Slovenia, 1989; Available online: http://dk.fdv.uni-lj.si/metodoloskizvezki/Pdfs/Mz_4Ferligoj.pdf (accessed on 2 March 2023).
- Wright, K.; Giger, J.N.; Norris, K.; Suro, Z. Impact of a nurse-directed, coordinated school health program to enhance physical activity behaviors and reduce body mass index among minority children: A parallel-group, randomized control trial. Int. J. Nurs. Stud. 2013, 50, 727–737. [Google Scholar] [CrossRef]
- Wright, K.; Suro, Z. Using community-academic partnerships and a comprehensive school-based program to decrease health disparities in activity in school-aged children. J. Prev. Interv. Community 2014, 42, 125–139. [Google Scholar] [CrossRef]
- Eather, N.; Morgan, P.J.; Lubans, D.R. Social support from teachers mediates physical activity behavior change in children participating in the Fit-4-Fun intervention. Int. J. Behav. Nutr. Phys. Act. 2013, 10, 68. [Google Scholar] [CrossRef]
- Eather, N.; Morgan, P.J.; Lubans, D.R. Improving the fitness and physical activity levels of primary school children: Results of the Fit-4-Fun group randomized controlled trial. Prev. Med. 2013, 56, 12–19. [Google Scholar] [CrossRef]
- Meyer, U.; Ernst, D.; Zahner, L.; Schindler, C.; Puder, J.J.; Kraenzlin, M.; Rizzoli, R.; Kriemler, S. 3-Year follow-up results of bone mineral content and density after a school-based physical activity randomized intervention trial. Bone 2013, 55, 16–22. [Google Scholar] [CrossRef]
- Meyer, U.; Schindler, C.; Zahner, L.; Ernst, D.; Hebestreit, H.; van Mechelen, W.; Brunner-La Rocca, H.P.; Probst-Hensch, N.; Puder, J.J.; Kriemler, S. Long-term effect of a school-based physical activity program (KISS) on fitness and adiposity in children: A cluster-randomized controlled trial. PLoS ONE 2014, 9, e87929. [Google Scholar] [CrossRef] [PubMed]
- Assaré, R.K.; Tian-Bi, Y.N.; Yao, P.K.; N’Guessan, N.A.; Ouattara, M.; Yapi, A.; Coulibaly, J.T.; Meïté, A.; Hürlimann, E.; Knopp, S.; et al. Sustaining control of Schistosomiasis mansoni in western Côte d’Ivoire: Results from a SCORE Study, one year after initial praziquantel administration. PLoS Negl. Trop. Dis. 2016, 10, e0004329. [Google Scholar] [CrossRef] [PubMed]
- Evans, C.E.; Ransley, J.K.; Christian, M.S.; Greenwood, D.C.; Thomas, J.D.; Cade, J.E. A cluster-randomised controlled trial of a school-based fruit and vegetable intervention: Project Tomato. Public Health Nutr. 2013, 16, 1073–1081. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Tymms, P.B.; Curtis, S.E.; Routen, A.C.; Thomson, K.H.; Bolden, D.S.; Bock, S.; Dunn, C.E.; Cooper, A.R.; Elliott, J.G.; Moore, H.J.; et al. Clustered randomised controlled trial of two education interventions designed to increase physical activity and well-being of secondary school students: The MOVE Project. BMJ Open 2016, 6, e009318. [Google Scholar] [CrossRef]
- Thériault, F.L.; Maheu-Giroux, M.; Blouin, B.; Casapía, M.; Gyorkos, T.W. Effects of a post-deworming health hygiene education intervention on absenteeism in school-age children of the Peruvian Amazon. PLoS Negl. Trop. Dis. 2014, 8, e3007. [Google Scholar] [CrossRef]
- Kipping, R.R.; Howe, L.D.; Jago, R.; Campbell, R.; Wells, S.; Chittleborough, C.R.; Mytton, J.; Noble, S.M.; Peters, T.J.; Lawlor, D.A. Effect of intervention aimed at increasing physical activity, reducing sedentary behaviour, and increasing fruit and vegetable consumption in children: Active for Life Year 5 (AFLY5) school based cluster randomised controlled trial. BMJ 2014, 348, g3256. [Google Scholar] [CrossRef]
- Challen, A.R.; Machin, S.J.; Gillham, J.E. The UK Resilience Programme: A school-based universal nonrandomized pragmatic controlled trial. J. Consult. Clin. Psychol. 2014, 82, 75–89. [Google Scholar] [CrossRef]
- Taylor, C.; Darby, H.; Upton, P.; Upton, D. Can a school-based intervention increase children’s fruit and vegetable consumption in the home setting? J. Consult. Clin. Psychol. 2013, 133, 330–336. [Google Scholar] [CrossRef]
- Rousham, E.K.; Uzaman, B.; Abbott, D.; Lee, S.F.; Mithani, S.; Roschnik, N.; Hall, A. The effect of a school-based iron intervention on the haemoglobin concentration of school children in north-west Pakistan. Eur. J. Clin. Nutr. 2013, 67, 1188–1192. [Google Scholar] [CrossRef]
- Freeman, M.C.; Clasen, T.; Brooker, S.J.; Akoko, D.O.; Rheingans, R. The impact of a school-based hygiene, water quality and sanitation intervention on soil-transmitted helminth reinfection: A cluster-randomized trial. Am. J. Trop. Med. Hyg. 2013, 89, 875–883. [Google Scholar] [CrossRef]
- Rappaport, E.B.; Daskalakis, C.; Sendecki, J.A. Using routinely collected growth data to assess a school-based obesity prevention strategy. Int. J. Obes. 2013, 37, 79–85. [Google Scholar] [CrossRef]
- Chan, E.K.; Quach, J.; Mensah, F.K.; Sung, V.; Cheung, M.; Wake, M. Dark chocolate for children’s blood pressure: Randomised trial. Arch. Dis. Child. 2012, 97, 637–640. [Google Scholar] [CrossRef] [PubMed]
- Shen, M.; Hu, M.; Sun, Z. Assessment of school-based quasi-experimental nutrition and food safety health education for primary school students in two poverty-stricken counties of west China. PLoS ONE 2015, 10, e0145090. [Google Scholar] [CrossRef] [PubMed]
- Blake, H.; Dawett, B.; Leighton, P.; Rose-Brady, L.; Deery, C. School-based educational intervention to improve children’s oral health-related knowledge. Health Promot. Pract. 2015, 16, 571–582. [Google Scholar] [CrossRef] [PubMed]
- Kobel, S.; Wirt, T.; Schreiber, A.; Kesztyüs, D.; Kettner, S.; Erkelenz, N.; Wartha, O.; Steinacker, J.M. Intervention effects of a school-based health promotion programme on obesity related behavioural outcomes. J. Obes. 2014, 2014, 476230. [Google Scholar] [CrossRef] [PubMed]
- Santos, R.G.; Durksen, A.; Rabbanni, R.; Chanoine, J.P.; Lamboo Miln, A.; Mayer, T.; McGavock, J.M. Effectiveness of peer-based healthy living lesson plans on anthropometric measures and physical activity in elementary school students: A cluster randomized trial. JAMA Pediatr. 2014, 168, 330–337. [Google Scholar] [CrossRef] [PubMed]
- Simon, C.; Kellou, N.; Dugas, J.; Platat, C.; Copin, N.; Schweitzer, B.; Hausser, F.; Bergouignan, A.; Lefai, E.; Blanc, S. A socio-ecological approach promoting physical activity and limiting sedentary behavior in adolescence showed weight benefits maintained 2.5 years after intervention cessation. Int. J. Obes. 2014, 38, 936–943. [Google Scholar] [CrossRef] [PubMed]
- Isensee, B.; Hansen, J.; Maruska, K.; Hanewinkel, R. Effects of a school-based prevention programme on smoking in early adolescence: A 6-month follow-up of the “Eigenstandig warden” cluster randomised trial. BMJ Open 2014, 4, e004422. [Google Scholar] [CrossRef]
- Gibbs, L.; Staiger, P.K.; Johnson, B.; Block, K.; Macfarlane, S.; Gold, L.; Kulas, J.; Townsend, M.; Long, C.; Ukoumunne, O. Expanding children’s food experiences: The impact of a school-based kitchen garden program. J. Nutr. Educ. Behav. 2013, 45, 137–146. [Google Scholar] [CrossRef]
- Breslin, G.; Brennan, D.; Rafferty, R.; Gallagher, A.M.; Hanna, D. The effect of a healthy lifestyle programme on 8–9 year olds from social disadvantage. Arch. Dis. Child. 2012, 97, 618–624. [Google Scholar] [CrossRef]
- Brandstetter, S.; Klenk, J.; Berg, S.; Galm, C.; Fritz, M.; Peter, R.; Prokopchuk, D.; Steiner, R.P.; Wartha, O.; Steinacker, J.; et al. Overweight prevention implemented by primary school teachers: A randomized controlled trial. Obes. Facts. 2012, 5, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Wang, B.; Stanton, B.; Chen, X.; Li, X.; Dinaj-Koci, V.; Brathwaite, N.; Deveaux, L.; Lunn, S. Predictors of responsiveness among early adolescents to a school-based risk reduction intervention over 3 years. AIDS Behav. 2013, 17, 1096–1104. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Bugge, A.; El-Naaman, B.; Dencker, M.; Froberg, K.; Holme, I.M.; McMurray, R.G.; Andersen, L.B. Effects of a three-year intervention: The Copenhagen School Child Intervention Study. Med. Sci. Sports Exerc. 2012, 44, 1310–1317. [Google Scholar] [CrossRef] [PubMed]
- Dolphens, M.; Cagnie, B.; Danneels, L.; De Clercq, D.; De Bourdeaudhuij, I.; Cardon, G. Long-term effectiveness of a back education programme in elementary schoolchildren: An 8-year follow-up study. Eur. Spine J. 2011, 20, 2134–2142. [Google Scholar] [CrossRef][Green Version]
- Weichold, K.; Blumenthal, A. Long-term effects of the Life Skills Program IPSY on substance use: Results of a 4.5-year longitudinal study. Prev. Sci. 2016, 17, 13–23. [Google Scholar] [CrossRef]
- Cao, Z.J.; Wang, S.M.; Chen, Y. A randomized trial of multiple interventions for childhood obesity in China. Am. J. Prev. Med. 2015, 48, 552–560. [Google Scholar] [CrossRef]
- Detter, F.; Nilsson, J.Å.; Karlsson, C.; Dencker, M.; Rosengren, B.E.; Karlsson, M.K. A 3-year school-based exercise intervention improves muscle strength: A prospective controlled population-based study in 223 children. BMC Musculoskelet. Disord. 2014, 15, 353. [Google Scholar] [CrossRef]
- Lehto, R.; Määttä, S.; Lehto, E.; Ray, C.; Te Velde, S.; Lien, N.; Thorsdottir, I.; Yngve, A.; Roos, E. The PRO GREENS intervention in Finnish schoolchildren: The degree of implementation affects both mediators and the intake of fruits and vegetables. Br. J. Nutr. 2014, 112, 1185–1194. [Google Scholar] [CrossRef]
- Biran, A.; Schmidt, W.P.; Varadharajan, K.S.; Rajaraman, D.; Kumar, R.; Greenland, K.; Gopalan, B.; Aunger, R.; Curtis, V. Effect of a behaviour-change intervention on handwashing with soap in India (SuperAmma): A cluster-randomised trial. Lancet Glob. Health 2014, 2, e145–e154. [Google Scholar] [CrossRef]
- Bothe, D.A.; Grignon, J.B.; Olness, K.N. The effects of a stress management intervention in elementary school children. J. Dev. Behav. Pediatr. 2014, 35, 62–67. [Google Scholar] [CrossRef]
- Bernardoni, B.; Thein-Nissenbaum, J.; Fast, J.; Day, M.; Li, Q.; Wang, S.; Scerpella, T. A school-based resistance intervention improves skeletal growth in adolescent females. Osteoporos. Int. 2014, 25, 1025–1032. [Google Scholar] [CrossRef] [PubMed]
- Gyorkos, T.W.; Maheu-Giroux, M.; Blouin, B.; Casapia, M. Impact of health education on soil-transmitted helminth infections in schoolchildren of the Peruvian Amazon: A cluster-randomized controlled trial. PLoS Negl. Trop. Dis. 2013, 7, e2397. [Google Scholar] [CrossRef]
- Klakk, H.; Andersen, L.B.; Heidemann, M.; Møller, N.C.; Wedderkopp, N. Six physical education lessons a week can reduce cardiovascular risk in school children aged 6–13 years: A longitudinal study. Scand. J. Public Health 2014, 42, 128–136. [Google Scholar] [CrossRef] [PubMed]
- Sacchetti, R.; Ceciliani, A.; Garulli, A.; Dallolio, L.; Beltrami, P.; Leoni, E. Effects of a 2-year school-based intervention of enhanced physical education in the primary school. J. Sch. Health 2013, 83, 639–646. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Arguelles, L.; Jiang, F.; Chen, W.; Jin, X.; Yan, C.; Tian, Y.; Hong, X.; Qian, C.; Zhang, J.; et al. Sleep, school performance, and a school-based intervention among school-aged children: A sleep series study in China. PLoS ONE 2013, 8, e67928. [Google Scholar] [CrossRef] [PubMed]
- Perikkou, A.; Gavrieli, A.; Kougioufa, M.M.; Tzirkali, M.; Yannakoulia, M. A novel approach for increasing fruit consumption in children. J. Acad. Nutr. Diet. 2013, 113, 1188–1193. [Google Scholar] [CrossRef]
- Fairclough, S.J.; Hackett, A.F.; Davies, I.G.; Gobbi, R.; Mackintosh, K.A.; Warburton, G.L.; Stratton, G.; van Sluijs, E.M.; Boddy, L.M. Promoting healthy weight in primary school children through physical activity and nutrition education: A pragmatic evaluation of the CHANGE! Randomized intervention study. BMC Public Health 2013, 13, 626. [Google Scholar] [CrossRef]
- Almas, A.; Islam, M.; Jafar, T.H. School-based physical activity programme in preadolescent girls (9–11 years): A feasibility trial in Karachi, Pakistan. Arch. Dis. Child. 2013, 98, 515–519. [Google Scholar] [CrossRef]
- Bird, E.L.; Halliwell, E.; Diedrichs, P.C.; Harcourt, D. Happy Being Me in the UK: A controlled evaluation of a school-based body image intervention with pre-adolescent children. Body Image 2013, 10, 326–334. [Google Scholar] [CrossRef]
- Dunton, G.F.; Liao, Y.; Grana, R.; Lagloire, R.; Riggs, N.; Chou, C.P.; Robertson, T. State-wide dissemination of a school-based nutrition education programme: A RE-AIM (Reach, Efficacy, Adoption, Implementation, Maintenance) analysis. Public Health Nutr. 2014, 17, 422–430. [Google Scholar] [CrossRef]
- Centis, E.; Marzocchi, R.; Di Luzio, R.; Moscatiello, S.; Salardi, S.; Villanova, N.; Marchesini, G.; the “G. C. Croce” School of Health Promotion. A controlled, class-based multicomponent intervention to promote healthy lifestyle and to reduce the burden of childhood obesity. Pediatr. Obes. 2012, 7, 436–445. [Google Scholar] [CrossRef] [PubMed]
- Essau, C.A.; Conradt, J.; Sasagawa, S.; Ollendick, T.H. Prevention of anxiety symptoms in children: Results from a universal school-based trial. Behav. Ther. 2012, 43, 450–464. [Google Scholar] [CrossRef] [PubMed]
- Gabrhelik, R.; Duncan, A.; Miovsky, M.; Furr-Holden, C.D.; Stastna, L.; Jurystova, L. “Unplugged”: A school-based randomized control trial to prevent and reduce adolescent substance use in the Czech Republic. Drug Alcohol. Depend. 2012, 124, 79–87. [Google Scholar] [CrossRef]
- Klatt, M.; Harpster, K.; Browne, E.; White, S.; Case-Smith, J. Feasibility and preliminary outcomes for Move-Into-Learning: An arts-based mindfulness classroom intervention. J. Posit. Psychol. 2013, 8, 233–241. [Google Scholar] [CrossRef]
- Kong, K.; Liu, J.; Tao, Y. Limitations of studies on school-based nutrition education interventions for obesity in China: A systematic review and meta-analysis. Asia Pac. J. Clin. Nutr. 2016, 25, 589–601. [Google Scholar] [CrossRef] [PubMed]
- Orton, E.; Whitehead, J.; Mhizha-Murira, J.; Clarkson, M.; Watson, M.C.; Mulvaney, C.A.; Staniforth, J.U.; Bhuchar, M.; Kendrick, D. School-based education programmes for the prevention of unintentional injuries in children and young people. Cochrane Database Syst. Rev. 2016, 27, CD010246. [Google Scholar] [CrossRef]
- Cicutto, L.; Gleason, M.; Haas-Howard, C.; White, M.; Hollenbach, J.P.; Williams, S.; McGinn, M.; Villarreal, M.; Mitchell, H.; Cloutier, M.M.; et al. Building Bridges for Asthma Care Program: A school-centered program connecting schools, families, and community health-care providers. J. Sch. Nurs. 2018, 33, 277–284. [Google Scholar] [CrossRef] [PubMed]
- Fàbregues, S.; Sáinz, M.; Romano, M.J.; Escalante-Barrios, E.L.; Younas, A.; López-Pérez, B.S. Use of mixed methods research in intervention studies to increase young people's interest in STEM: A systematic methodological review. Front. Psychol. 2023, 13, 956300. [Google Scholar] [CrossRef]
| Structural Elements of HPI | Codes | Categories | Type of New Variable | Analysis |
|---|---|---|---|---|
| Health area of intervention | Infection control, physical activity, physical fitness, nutrition, substance abuse, obesity prevention, sleep health, oral health, prevention of anemia, blood pressure, cardiovascular disease prevention, skeletal growth, osteoporosis prevention, spine care, prevention of falls and injuries, healthy lifestyle; Stress management, depression, anxiety, hyperactivity, mindfulness, body image. | Physical health Mental health | Categorical | Thematic analysis |
| Research design | RCT, stratified randomized trial; Nonrandomized controlled trial, cluster randomized quasi-experiment, nonrandomized pretest–post-test study, prospective controlled study, longitudinal study, prospective longitudinal study, cohort study, prospective cohort study, cross-sectional survey, participatory research approach. | RCT Other designs (quasi-experimental, pretest–post-test, controlled interventions) | Categorical | Thematic analysis |
| Region of study | Switzerland, Belgium, the United Kingdom, Germany, Sweden, Finland, France, Denmark, the Netherlands, Czech Republic, Italy, Cyprus; Canada, the USA; China, India, Pakistan; Australia; Peru, Bahamas; Kenya. | Europe North America Asia Australia South America Africa | Categorical | Thematic analysis |
| Target group | Children; Children + one additional group: family, school, teacher, community, peers. | Children Multiple target groups | Categorical | Thematic analysis |
| Intervention provider | School policy/regulation/curriculum change or improvement; Experts—trained teachers for HPI implementation, trained students, external experts (physiotherapist, registered nurse, school nurse, physician, researcher, dietitian, kinesiologist, psychologist); Multiple providers (≥2 from above). | School policy/curriculum change Experts Multiple providers | Categorical | Thematic analysis |
| Intervention effectiveness | 1—Reverse effect; 2—No effect; 3—Partial/moderate effect; 4—Positive effect; 5—Strong positive effect. | Reverse or no effect Partial effect Positive effect | Numerical, interval | Quantification |
| Characteristics | Category | Total Interventions | % of Total |
|---|---|---|---|
| Intervention characteristics | |||
| Area of intervention | Physical health | 40 | 81.6 |
| Mental health | 9 | 18.4 | |
| Target groups | Children target group | 34 | 69.4 |
| Multiple target groups | 15 | 30.6 | |
| Intervention provider | School policy/curriculum change | 23 | 46.9 |
| Experts—trained teachers | 13 | 26.5 | |
| External experts | 4 | 8.2 | |
| Multiple providers | 9 | 18.4 | |
| Intervention duration (months) | ≤2 months | 13 | 26.5 |
| 2.1–12 months | 23 | 47.0 | |
| >12 months | 13 | 26.5 | |
| Number of follow-ups | One follow-up | 28 | 57.2 |
| Two follow-ups | 13 | 26.5 | |
| >2 follow-ups | 8 | 16.3 | |
| The first follow-up (months after intervention) | ≤3 months | 28 | 57.1 |
| 3.1–6 months | 6 | 12.3 | |
| >6 months | 15 | 30.6 | |
| The last follow-up (months after intervention) | ≤6 months | 20 | 40.8 |
| 6.1 months–1 year | 14 | 28.6 | |
| >1 year | 15 | 30.6 | |
| Sample characteristics | |||
| Sample size at the baseline | ≤200 | 9 | 18.4 |
| 201–600 | 13 | 26.5 | |
| 601–1199 | 13 | 26.5 | |
| ≥1200 | 14 | 28.6 | |
| Age of participants at the intervention baseline | ≤8 years | 15 | 30.6 |
| 9–10 years | 22 | 44.9 | |
| ≥11 years | 12 | 24.5 | |
| Study characteristics | |||
| Research design | RCT | 30 | 61.2 |
| Other designs | 19 | 38.8 | |
| Regions | Europe | 27 | 55.1 |
| North America | 8 | 16.3 | |
| Asia | 6 | 12.3 | |
| Australia | 5 | 10.2 | |
| South America | 2 | 4.1 | |
| Africa | 1 | 2.0 |
| Characteristics | Group 1 Extensive and Long-Term HPI (n = 15) | Group 2 School Policy-Changing HPI (n = 24) | Group 3 Highly Effective HPI (n = 10) | F (p)/ χ2 (p) + | |||
|---|---|---|---|---|---|---|---|
| n (%) | M (SD) | n (%) | M (SD) | n (%) | M (SD) | ||
| Research design—RCT | 11 (73.3) | 13 (54.2) | 6 (60.0) | 11 (73.3) | 1.036 (0.363) + | ||
| Sample size at baseline | 1801.93 (2446.24) | 901.67 (916.19) | 634.70 (692.92) | 2.243 (0.118) | |||
| Age of participants at baseline | 9.30 (1.87) | 9.82 (1.47) | 9.99 (0.76) | 0.798 (0.456) | |||
| Intervention duration (months) | 25.37 (16.87) | 7.53 (7.06) | 4.54 (3.53) | 16.276 (0.000) | |||
| Number of follow-ups | 2.40 (1.72) | 1.38 (0.58) | 1.60 (0.70) | 4.257 (0.020) | |||
| The first follow-up (months after intervention completion) | 18.28 (15.20) | 1.83 (2.64) | 5.15 (4.26) | 16.605 (0.000) | |||
| The last follow-up (months after intervention completion) | 38.00 (20.09) | 4.75 (6.28) | 8.20 (4.57) | 37.174 (0.000) | |||
| Area of intervention—physical health | 12 (80.0) | 20 (83.3) | 8 (80.0) | 0.091 (0.956) + | |||
| Changing school policy, curriculum | 9 (39.1) | 13 (56.5) | 1 (4.4) | 7.009 (0.030) + | |||
| Experts and multiple providers 1 | 6 (40.0) | 11 (45.8) | 9 (90.0) | 7.009 (0.030) + | |||
| Multiple target groups | 5 (33.3) | 0 (0.0) | 10 (100) | 33.307 (0.000) + | |||
| Effectiveness—positive and strong positive effects, average effect 2 (Total sample: M = 3.39, SD = 1.08). | 7 (46.6) | 3.27 (1.22) | 9 (37.5) | 3.08 (0.93) | 9 (90.0) | 4.30 (0.68) | 5.519 (0.007) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zurc, J.; Laaksonen, C. Effectiveness of Health Promotion Interventions in Primary Schools—A Mixed Methods Literature Review. Healthcare 2023, 11, 1817. https://doi.org/10.3390/healthcare11131817
Zurc J, Laaksonen C. Effectiveness of Health Promotion Interventions in Primary Schools—A Mixed Methods Literature Review. Healthcare. 2023; 11(13):1817. https://doi.org/10.3390/healthcare11131817
Chicago/Turabian StyleZurc, Joca, and Camilla Laaksonen. 2023. "Effectiveness of Health Promotion Interventions in Primary Schools—A Mixed Methods Literature Review" Healthcare 11, no. 13: 1817. https://doi.org/10.3390/healthcare11131817
APA StyleZurc, J., & Laaksonen, C. (2023). Effectiveness of Health Promotion Interventions in Primary Schools—A Mixed Methods Literature Review. Healthcare, 11(13), 1817. https://doi.org/10.3390/healthcare11131817







