Work–Family Conflict and Mental Health among Chinese Female Healthcare Workers during the COVID-19 Pandemic: The Moderating Effects of Resilience
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Collection
2.2. Measures
2.2.1. Mental Health
2.2.2. Work–Family Conflict
2.2.3. Resilience
2.3. Statistical Analysis
3. Results
3.1. Description of the Sample Characteristics and Differences in Study Variables
3.2. Mental Health Status of Female Healthcare Workers during the COVID-19 Pandemic Compared with the National Norm
3.3. Relationship between Mental Health, Work–family Conflict, and Resilience
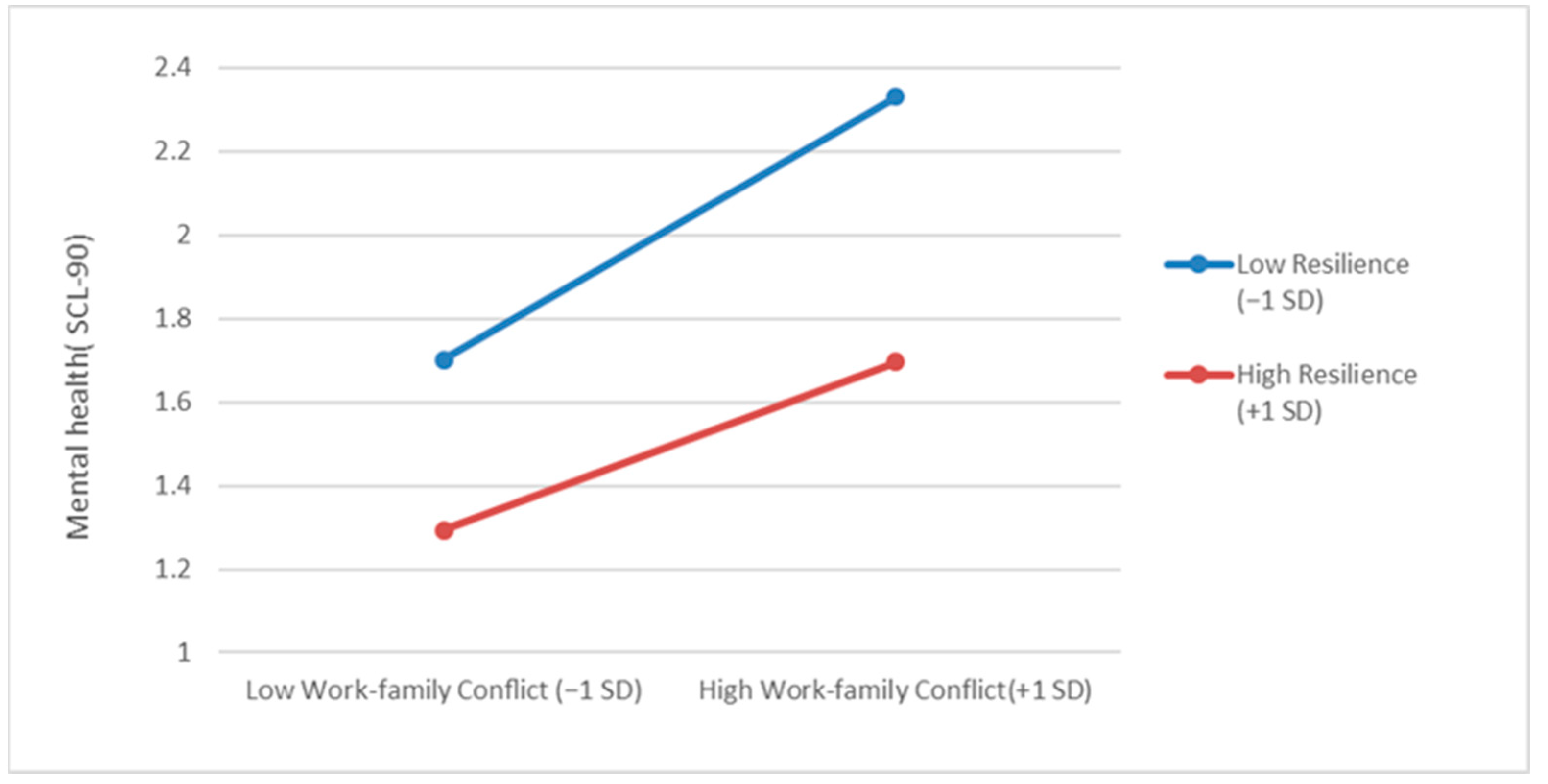
3.4. Moderating Effects of Resilience
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- He, G.; Chen, Y.; Wang, D.; Wang, H. Influencing factors of work stress of medical workers in clinical laboratory during COVID-19 pandemic: Working hours, compensatory leave, job satisfaction. Front. Public Health 2023, 11, 1078540. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.Y.; Yang, Y.Z.; Zhang, X.M.; Xu, X.Y.; Dou, Q.L.; Zhang, W.W.; Cheng, A.S. The Prevalence and Influencing Factors in Anxiety in Medical Workers Fighting COVID-19 in China: A Cross-Sectional Survey. Epidemiol. Infect. 2020, 148, e98. [Google Scholar] [CrossRef]
- Greenberg, N.; Docherty, M.; Gnanapragasam, S.; Wessely, S. Managing mental health challenges faced by healthcare workers during COVID-19 pandemic. BMJ 2020, 368, m1211. [Google Scholar] [CrossRef]
- Spoorthy, M.S.; Pratapa, S.K.; Mahant, S. Mental health problems faced by healthcare workers due to the COVID-19 pandemic–A review. Asian J. Psychiatr. 2020, 51, 102119. [Google Scholar] [CrossRef]
- Thatrimontrichai, A.; Weber, D.J.; Apisarnthanarak, A. Mental health among healthcare personnel during COVID-19 in Asia: A systematic review. J. Formos. Med. Assoc. 2021, 120, 1296–1304. [Google Scholar] [CrossRef]
- Chatzittofis, A.; Karanikola, M.; Michailidou, K.; Constantinidou, A. Impact of the COVID-19 Pandemic on the Mental Health of Healthcare Workers. Int. J. Environ. Res. Public Health 2021, 18, 1435. [Google Scholar] [CrossRef] [PubMed]
- Carmassi, C.; Dell’Oste, V.; Bui, E.; Foghi, C.; Bertelloni, C.A.; Atti, A.R.; Buselli, R.; Di Paolo, M.; Goracci, A.; Malacarne, P.; et al. The interplay between acute post-traumatic stress, depressive and anxiety symptoms on healthcare workers functioning during the COVID-19 emergency: A multicenter study comparing regions with increasing pandemic incidence. J. Affect. Disord. 2022, 298, 209–216. [Google Scholar] [CrossRef]
- National Health and Wellness Commission. China’s Health and Health Care Development Statistics Bulletin. Available online: http://www.gov.cn/xinwen/2022-07/12/content_5700670.htm (accessed on 12 July 2022). (In Chinese)
- World Health Organization. World Health Statistics 2020: Monitoring Health for The Sdgs, Sustainable Development Goals. World Health Organization. Available online: https://apps.who.int/iris/handle/10665/332070 (accessed on 11 May 2023).
- Hu, D.; Kong, Y.; Li, W.; Han, Q.; Zhang, X.; Zhu, L.X.; Wan, S.W.; Liu, Z.; Shen, Q.; Yang, J.; et al. Frontline nurses’ burnout, anxiety, depression, and fear statuses and their associated factors during the COVID-19 outbreak in Wuhan, China: A large-scale cross-sectional study. E Clin. Med. 2020, 24, 100424. [Google Scholar] [CrossRef]
- Zhou, Y.; Wang, W.; Sun, Y.; Qian, W.; Liu, Z.; Wang, R.; Qi, L.; Yang, J.; Song, X.; Zhou, X.; et al. The prevalence and risk factors of psychological disturbances of frontline medical staff in china under the COVID-19 epidemic: Workload should be concerned. J. Affect. Disord. 2020, 277, 510–514. [Google Scholar] [CrossRef] [PubMed]
- Lai, J.B.; Ma, S.; Wang, Y.; Cai, Z.; Hu, J.; Wei, N.; Wu, J.; Du, H.; Chen, T.; Li, R.; et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw. Open 2020, 3, e203976. [Google Scholar] [CrossRef] [PubMed]
- Pappa, S.; Ntella, V.; Giannakas, T.; Giannakoulis, V.G.; Papoutsi, E.; Katsaounou, P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav. Immun. 2020, 88, 901–907. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.Z.; Han, M.F.; Luo, T.D.; Zhou, X.P. Mental health survey of medical staff in a tertiary infectious disease hospital for COVID-19. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi 2020, 38, 192–195. Available online: https://pubmed.ncbi.nlm.nih.gov/32131151/ (accessed on 11 May 2023). (In Chinese). [PubMed]
- Buselli, R.; Corsi, M.; Baldanzi, S.; Chiumiento, M.; Del Lupo, E.; Dell’Oste, V.; Bertelloni, C.A.; Massimetti, G.; Dell’Osso, L.; Cristaudo, A.; et al. Professional Quality of Life and Mental Health Outcomes among Health Care Workers Exposed to SARS-CoV-2 (COVID-19). Int. J. Environ. Res. Public Health 2020, 17, 6180. [Google Scholar] [CrossRef] [PubMed]
- Zerbini, G.; Ebigbo, A.; Reicherts, P.; Kunz, M.; Messman, H. Psychosocial burden of healthcare professionals in times of COVID-19—A survey conducted at the University Hospital Augsburg. Ger. Med. Sci. 2020, 18, doc05. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.Y.; Yang, Y.Y. Mental Health Status and Its Influencing Factors: The Case of Nurses Working in COVID-19 Hospitals in South Korea. Int. J. Environ. Res. Public Health 2021, 18, 6531. [Google Scholar] [CrossRef]
- Swift, A.; Banks, L.; Baleswaran, A.; Cooke, N.; Little, C.; McGrath, L.; Meechan-Rogers, R.; Neve, A.; Rees, H.; Tomlinson, A.; et al. COVID-19 and student nurses: A view from England. J. Clin. Nurs. 2020, 29, 3111. [Google Scholar] [CrossRef]
- Casafont, C.; Fabrellas, N.; Rivera, P.; Olivé-Ferrer, M.C.; Querol, E.; Venturas, M.; Prats, J.; Cuzco, C.; Frías, C.E.; Pérez-Ortega, S.; et al. Experiences of nursing students as healthcare aid during the COVID-19 pandemic in Spain: A phemonenological research study. Nurse Educ. Today 2021, 97, 104711. [Google Scholar] [CrossRef]
- Takeuchi, T.; Yamazaki, Y. Relationship between work-family conflict and a sense of coherence among Japanese registered nurses. Jpn. J. Nurs. Sci. 2010, 7, 158–168. [Google Scholar] [CrossRef]
- Simon, M.; Kümmerling, A.; Hasselhorn, H.M. Work-home conflict in the European nursing profession. Int. J. Occup. Environ. Health 2004, 10, 384–391. [Google Scholar] [CrossRef]
- Liu, Q.; Luo, D.; Haase, J.E.; Guo, Q.; Wang, X.Q.; Liu, S.; Xia, L.; Liu, Z.; Yang, J.; Yang, B.X. The experiences of health-care providers during the COVID-19 crisis in China: A qualitative study. Lancet Glob. Health 2020, 8, e790–e798. [Google Scholar] [CrossRef]
- Zhang, X.; Wang, J.; Hao, Y.; Wu, K.; Jiao, M.; Liang, L.; Gao, L.; Ning, N.; Kang, Z.; Shan, L.; et al. Prevalence and Factors Associated with Burnout of Frontline Healthcare Workers in Fighting Against the COVID-19 Pandemic: Evidence from China. Front. Psychol. 2021, 16, 680614. [Google Scholar] [CrossRef]
- Hwang, E.H.; Yu, Y.B. Effect of sleep quality and depression on married female nurses’ work-family conflict. Int. J. Environ. Res. Public Health 2021, 18, 7838. [Google Scholar] [CrossRef]
- Vargas-Jiménez, E.; Castro-Castañeda, R.; Agulló, T.E.; Medina, C.R. Job Insecurity, Family Functionality and Mental Health: A Comparative Study between Male and Female Hospitality Workers. Behav. Sci. 2020, 10, 146. [Google Scholar] [CrossRef]
- Zuo, J.; Bian, Y. Gendered resources, division of housework, and perceived fairness—A case in urban China. J. Marriage Fam. 2001, 63, 1122–1133. [Google Scholar] [CrossRef]
- Wang, Y.; Peng, J. Work-Family Conflict and Depression in Chinese Professional Women: The Mediating Roles of Job Satisfaction and Life Satisfaction. Int. J. Ment. Health Addict. 2017, 15, 394–406. [Google Scholar] [CrossRef]
- Zhou, S.Y.; Da, S.; Guo, H.; Zhang, X. Work-Family Conflict and Mental Health Among Female Employees: A Sequential Mediation Model via Negative Affect and Perceived Stress. Front. Psychol. 2018, 9, 544. [Google Scholar] [CrossRef] [PubMed]
- Chu, L.C. The influence of perceived stress on work-family conflict and mental health: The moderating effect of person-environment fit. J. Nurs. Manag. 2014, 22, 613–620. [Google Scholar] [CrossRef]
- Zhang, H.; Ye, Z.; Tang, L.; Zou, P.; Du, C.; Shao, J.; Wang, X.; Chen, D.; Qiao, G.; Mu, S.Y. Anxiety symptoms and burnout among Chinese medical staff of intensive care unit: The moderating effect of social support. BMC Psychiatry 2020, 20, 197. [Google Scholar] [CrossRef]
- Lu, F.; Xu, Y.; Yu, Y.; Peng, L.; Wu, T.; Wang, T.; Liu, B.; Xie, J.; Xu, S.; Li, M. Moderating effect of mindfulness on the relationships between perceived stress and mental health outcomes among Chinese intensive care nurses. Front. Psychiatry 2019, 10, 260. [Google Scholar] [CrossRef]
- Chu, L.C. Impact of providing compassion on job performance and mental health: The moderating effect of interpersonal relationship quality. J. Nurs. Scholarsh. 2017, 49, 456–465. [Google Scholar] [CrossRef]
- Tugade, M.M.; Fredrickson, B.L. Resilient individuals use positive emotions to bounce back from negative emotional experiences. J. Pers. Soc. Psychol. 2004, 86, 320–333. [Google Scholar] [CrossRef] [PubMed]
- Masten, A.S. Global perspectives on resilience in children and youth. Child Dev. 2014, 85, 6–20. [Google Scholar] [CrossRef]
- Liu, J.J.W.; Reed, M.; Girard, T.A. Advancing resilience: An integrative, multi-system model of resilience. Personal. Individ. Differ. 2017, 111, 111–118. [Google Scholar] [CrossRef]
- Hu, T.; Zhang, D.; Wang, J. A meta-analysis of the trait resilience and mental health. Personal. Individ. Differ. 2015, 76, 18–27. [Google Scholar] [CrossRef]
- Fino, E.; Mema, D.; Russo, P.M. War trauma exposed refugees and posttraumatic stress disorder: The moderating role of trait resilience. J. Psychosom. Res. 2020, 129, 109905. [Google Scholar] [CrossRef]
- Julian, M.; Le, H.N.; Coussons-Read, M.; Hobel, C.J.; Schetter, D.C. The moderating role of resilience resources in the association between stressful life events and symptoms of postpartum depression. J. Affect. Disord. 2021, 293, 261–267. [Google Scholar] [CrossRef] [PubMed]
- Thurston, I.B.; Hardin, R.; Kamody, R.C.; Herbozo, S.; Kaufman, C. The moderating role of resilience on the relationship between perceived stress and binge eating symptoms among young adult women. Eat. Behav. 2018, 29, 114–119. [Google Scholar] [CrossRef]
- Pérez-Gómez, H.R.; González-Díaz, E.; Herrero, M.; de Santos-Ávila, F.; Vázquez-Castellanos, J.L.; Juárez-Rodríguez, P.; Moreno-Jiménez, B.; Meda-Lara, R.M. The moderating effect of resilience on mental health deterioration among COVID-19 survivors in a Mexican sample. Healthcare 2022, 10, 305. [Google Scholar] [CrossRef]
- Gonçalves, L.; Sala, R.; Navarro, J.B. Resilience and occupational health of health care workers: A moderator analysis of organizational resilience and sociodemographic attributes. Int. Arch. Occup. Environ. Health 2022, 95, 223–232. [Google Scholar] [CrossRef]
- Derogatis, L.R.; Lipman, R.S.; Covi, L. SCL-90: An outpatient psychiatric rating scale—Preliminary report. Psychopharmacol. Bull. 1973, 9, 13–28. [Google Scholar] [PubMed]
- Lei, X.S.; Liu, C.J.; Jiang, H. Mental health of college students and associated factors in Hubei of China. PLoS ONE 2021, 16, e0254183. [Google Scholar] [CrossRef] [PubMed]
- Carlson, D.S.; Kacmar, K.M.; Williams, L.J. Construction and initial validation of a multidimensional measure of work–family conflict. J. Vocat. Behav. 2000, 56, 249–276. [Google Scholar] [CrossRef]
- Wu, S.; Cao, K. Abusive Supervision and Work-Family Conflict: The Mediating Role of Emotional Exhaustion. J. Hum. Resour. Sustain. Stud. 2015, 3, 171–178. [Google Scholar] [CrossRef]
- Wang, S.H.; Wang, T.J.; Hsu, S.T.; Wang, M.-H. Reliability and Validity of the Chinese Version of the Connor-Davidson Resilience Scale. Rehabil. Couns. 2017, 8, 47–71. Available online: https://www.airitilibrary.com/Publication/alDetailedMesh?DocID=a0000536-201703-201803270009-201803270009-47-71 (accessed on 11 May 2023). (In Chinese).
- Jin, H.; Wu, W.Y.; Zhang, M.Y. Zhong Guo Zheng Chang Ren SCL-90 Ping Ding Jie Guo De Chu Bu Fen Xi [Preliminary analysis of the SCL-90 assessment results in the Chinese general population]. Chin. J. Nerv. Ment. Dis. 1986, 5, 260–263. (In Chinese) [Google Scholar]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach, 2nd ed.; Guilford Press: New York, NY, USA, 2017; ISBN 978-14-6253-465-4. [Google Scholar]
- Aiken, L.S.; West, S.G. Multiple Regression: Testing and Interpreting Interactions; Sage Publications: New Delhi, IL, USA, 1991; ISBN 0-7619-0712-2. [Google Scholar]
- Wang, J.; Cheng, Y.Q.; Zhou, Z.; Jiang, A.; Guo, J.; Chen, Z.; Wan, Q. Psychological status of Wuhan medical staff in fighting against COVID-19. Med. J. Wuhan Univ. 2020, 41, 547–550. Available online: https://search.bvsalud.org/global-literature-on-novel-coronavirus-2019-ncov/resource/en/covidwho-616546 (accessed on 11 May 2023). (In Chinese).
- Teng, Y.Y.; Sun, Y.J.; Wang, T.; Chen, W.; Wu, Y.; Chen, M.; Huang, X. Results of symptom checklist-90 for medical personnel in Zhuhai. Occup. Health Damage 2022, 37, 29–34. Available online: http://qikan.cqvip.com/Qikan/Article/Detail?id=7106547370&from=Qikan_Search_Index (accessed on 11 May 2023). (In Chinese).
- Caplan, G. Loss, stress, and mental health. Community Ment. Health J. 1990, 26, 27–48. [Google Scholar] [CrossRef]
- Lim, S.L.; Lim, B.K. Po Xi Wen Ti: The “mother-in-law problem” navigating tradition and modernity in transforming familial relationships in the Chinese family. J. Fam. Psychother. 2012, 23, 202–216. [Google Scholar] [CrossRef]
- Baruth, K.E.; Caroll, J.J. A formal assessment of resilience: The Baruth Protective Factors Inventory. J. Individ. Psychol. 2002, 58, 235–244. [Google Scholar]
- Kumphfer, K.L. Factors and processes contributing to resilience: The resilience framework. In Resilience and Development: Positive Life Adaptations; Glantz, M.D., Johnson, J.L., Eds.; Kluwer Academic Publishers: New York, NY, USA, 1999; pp. 179–224. ISBN 978-0-3064-6123-1. [Google Scholar]
- Chen, F.; Liu, G.; Mair, C.A. Intergenerational ties in context: Grandparents caring for grandchildren in China. Soc. Forces 2011, 90, 571–594. [Google Scholar] [CrossRef]
- Ning, X.; Yu, F.; Huang, Q.; Li, X.; Luo, Y.; Huang, Q.; Chen, C. The mental health of neurological doctors and nurses in Hunan Province, China during the initial stages of the COVID-19 outbreak. BMC Psychiatry 2020, 20, 436. [Google Scholar] [CrossRef]
- Fang, X.H.; Wu, L.; Lu, L.S.; Kan, X.H.; Wang, H.; Xiong, Y.J.; Ma, D.C.; Wu, G.C. Mental health problems and social supports in the COVID-19 healthcare workers: A Chinese explanatory study. BMC Psychiatry 2021, 21, 34. [Google Scholar] [CrossRef] [PubMed]
- Cooklin, A.R.; Dinh, H.; Strazdins, L.; Westrupp, E.; Leach, L.S.; Nicholson, J.M. Change and stability in work-family conflict and mothers’ and fathers’ mental health: Longitudinal evidence from an Australian cohort. Soc. Sci. Med. 2016, 155, 24–34. [Google Scholar] [CrossRef] [PubMed]
- Gao, T.; Ding, X.; Chai, J.; Zhang, Z.; Zhang, H.; Kong, Y.; Mei, S. The influence of resilience on mental health: The role of general well-being. Int. J. Nurs. Pract. 2017, 23, e12535. [Google Scholar] [CrossRef]
- Wu, Y.; Sang, Z.; Zhang, X.C.; Margraf, J. The Relationship Between Resilience and Mental Health in Chinese College Students: A Longitudinal Cross-Lagged Analysis. Front. Psychol. 2020, 11, 108. [Google Scholar] [CrossRef]
- Verdolini, N.; Amoretti, S.; Montejo, L.; García-Rizo, C.; Hogg, B.; Mezquida, G.; Rabelo-da-Ponte, F.D.; Vallespir, C.; Radua, J.; Martinez-Aran, A.; et al. Resilience and mental health during the COVID-19 pandemic. J. Affect. Disord. 2021, 283, 156–164. [Google Scholar] [CrossRef] [PubMed]
- Gerino, E.; Rollè, L.; Sechi, C.; Brustia, P. Loneliness, resilience, mental health, and quality of life in old age: A structural equation model. Front. Psychol. 2017, 8, 2003. [Google Scholar] [CrossRef] [PubMed]
- Masten, A.S. Ordinary Magic: Resilience in Development; Guildford Press: New York, NY, USA, 2014; pp. 286–291. ISBN 978-1-4625-1716-9. [Google Scholar]
- Gitterman, A.; Knight, C. Promoting resilience through social work practice with groups: Implications for the practice and field curricula. J. Soc. Work. Educ. 2016, 52, 448–461. [Google Scholar] [CrossRef]
- Carolyn, K. Group Work with Homeless Mothers: Promoting Resilience Through Mutual Aid. Soc. Work 2017, 62, 235–242. [Google Scholar] [CrossRef]
- Cassidy, S. Resilience Building in Students: The Role of Academic Self-Efficacy. Front. Psychol. 2015, 6, 1781. [Google Scholar] [CrossRef] [PubMed]
- Rosenberg, A.R.; Yi-Frazier, J.P.; Eaton, L.; Wharton, C.; Cochrane, K.; Pihoker, C.; Baker, K.S.; McCauley, E. Promoting Resilience in Stress Management: A Pilot Study of a Novel Resilience-Promoting Intervention for Adolescents and Young Adults with Serious Illness. J. Pediatr. Psychol. 2015, 40, 992–999. [Google Scholar] [CrossRef] [PubMed]
- Mehta, D.H.; Perez, G.K.; Traeger, L.; Park, E.R.; Goldman, R.E.; Haime, V.; Chittenden, E.H.; Denninger, J.W.; Jackson, V.A. Building resiliency in a palliative care team: A pilot study. J. Pain Symptom Manag. 2016, 51, 604–608. [Google Scholar] [CrossRef] [PubMed]
- Sun, J.Y.; Li, J. Women in Leadership in China: Past, Present, and Future. In Current Perspectives on Asian Women in Leadership: A Cross-Cultural Analysis; Cho, Y., Ghosh, R., Sun, J., McLean, G., Eds.; Palgrave Macmillan: London, UK, 2017; pp. 19–36. ISBN 978-3-319-54995-8. [Google Scholar] [CrossRef]
| Variables | Categories | n (%) | Mental Health (SCL-90) | Work–family Conflict | Resilience | |||
|---|---|---|---|---|---|---|---|---|
| M ± SD | F | M ± SD | F | M ± SD | F | |||
| Age(year) | 20–29 (a) | 132 (30.6) | 2.03 ± 0.75 | 1.48 | 2.77 ± 0.73 | 4.58 *** a = b > c | 3.30 ± 0.64 | 11.96 *** a = b < c |
| 30–39 (b) | 180 (41.8) | 2.05 ± 0.75 | 2.84 ± 0.64 | 3.37 ± 0.64 | ||||
| ≥40 (c) | 119 (27.6) | 1.91 ± 0.64 | 2.61 ± 0.59 | 3.66 ± 0.63 | ||||
| Educational level | High school | 13 (3) | 2.00 ± 0.64 | 0.49 | 2.50 ± 0.60 | 2.27 | 3.63 ± 0.56 | 0.81 |
| Junior college | 222 (51.5) | 1.97 ± 0.73 | 2.72 ± 0.63 | 3.44 ± 0.65 | ||||
| Bachelor | 196 (45.5) | 2.04 ± 0.72 | 2.82 ± 0.70 | 3.40 ± 0.67 | ||||
| Position | Doctor (a) | 83 (19.3) | 1.87 ± 0.65 | 3.06 * a = e < b e < d | 2.66 ± 0.72 | 4.38 ** e < a = c < b | 3.44 ± 0.67 | 1.84 |
| Nurse (b) | 241 (55.9) | 2.09 ± 0.75 | 2.87 ± 0.63 | 3.35 ± 0.63 | ||||
| Medical technicians (c) | 47 (10.9) | 1.87 ± 0.71 | 2.57 ± 0.67 | 3.57 ± 0.73 | ||||
| Administrative staff (d) | 27 (6.3) | 2.17 ± 0.61 | 2.69 ± 0.62 | 3.57 ± 0.68 | ||||
| Other positions (e) | 21 (4.9) | 1.64 ± 0.56 | 2.35 ± 0.45 | 3.61 ± 0.63 | ||||
| Logistics staff (f) | 12 (2.8) | 2.10 ± 0.77 | 2.77 ± 0.75 | 3.60 ± 0.53 | ||||
| Marital status | Married | 318 (73.8) | 1.98 ± 0.70 | 2.07 | 2.73 ± 0.64 | 1.26 | 3.45 ± 0.66 | 2.12 |
| Single | 113 (26.2) | 2.09 ± 0.78 | 2.82 ± 0.73 | 3.35 ± 0.63 | ||||
| Whether or not the participant has children | Yes | 308 (71.5) | 1.99 ± 0.70 | 0.51 | 2.74 ± 0.64 | 0.51 | 3.48 ± 0.65 | 6.69 * |
| No | 123 (28.5) | 2.04 ± 0.76 | 2.79 ± 0.71 | 3.30 ± 0.64 | ||||
| Dimension | This Study (n = 431) | National Norm (n = 1388) | t |
|---|---|---|---|
| Total score | 2.01 ± 0.72 | 1.44 ± 0.43 | 16.31 *** |
| Anxiety | 1.94 ± 0.77 | 1.39 ± 0.43 | 14.75 *** |
| Depression | 2.13 ± 0.81 | 1.50 ± 0.59 | 16.23 *** |
| Somatization | 2.01 ± 0.75 | 1.37 ± 0.48 | 17.67 *** |
| Obsessive | 2.37 ± 0.78 | 1.62 ± 0.58 | 20.07 *** |
| Interpersonal sensitivity | 2.02 ± 0.78 | 1.65 ± 0.51 | 9.86 *** |
| Hostility | 2.00 ± 0.80 | 1.48 ± 0.56 | 13.36 *** |
| Phobia anxiety | 1.73 ± 0.73 | 1.23 ± 0.41 | 14.15 *** |
| Paranoid ideation | 1.80 ± 0.73 | 1.43 ± 0.57 | 10.36 *** |
| Psychoticism | 1.82 ± 0.74 | 1.29 ± 0.42 | 14.75 *** |
| Variable | 1 | 2 | 3 |
|---|---|---|---|
| 1. Mental health (SCL-90) | 1 | ||
| 2. Work–family conflict | 0.46 ** | 1 | |
| 3. Resilience | −0.45 ** | −0.32 ** | 1 |
| The Regression Equation | Overall Fitting Index | Significance of Regression Coefficient | |||
|---|---|---|---|---|---|
| Outcome variable | Prognosis variate | R2 | F | β | t |
| Mental health (SCL-90) | Work–family conflict | 0.33 | 25.96 *** | 0.39 | 8.42 *** |
| Resilience | −0.40 | −8.44 *** | |||
| Work–family conflict * Resilience | −0.13 | −2.36 * | |||
| Age | 0.05 | 1.09 | |||
| Education level | 0.00 | 0.01 | |||
| Position | 0.02 | 0.83 | |||
| Marital status | 0.13 | 1.32 | |||
| Whether or not participant has children | −0.06 | −0.61 | |||
| Level of Moderator Variable | B | SE | t | LLCI | ULCI |
|---|---|---|---|---|---|
| Low resilience | −0.65 | 0.06 | 7.78 *** | 0.36 | 0.60 |
| High resilience | 0.65 | 0.06 | 5.35 *** | 0.19 | 0.41 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, Z.; Hong, L. Work–Family Conflict and Mental Health among Chinese Female Healthcare Workers during the COVID-19 Pandemic: The Moderating Effects of Resilience. Healthcare 2023, 11, 1696. https://doi.org/10.3390/healthcare11121696
Liu Z, Hong L. Work–Family Conflict and Mental Health among Chinese Female Healthcare Workers during the COVID-19 Pandemic: The Moderating Effects of Resilience. Healthcare. 2023; 11(12):1696. https://doi.org/10.3390/healthcare11121696
Chicago/Turabian StyleLiu, Zixiao, and Liu Hong. 2023. "Work–Family Conflict and Mental Health among Chinese Female Healthcare Workers during the COVID-19 Pandemic: The Moderating Effects of Resilience" Healthcare 11, no. 12: 1696. https://doi.org/10.3390/healthcare11121696
APA StyleLiu, Z., & Hong, L. (2023). Work–Family Conflict and Mental Health among Chinese Female Healthcare Workers during the COVID-19 Pandemic: The Moderating Effects of Resilience. Healthcare, 11(12), 1696. https://doi.org/10.3390/healthcare11121696






