German Physicians and Medical Students Do Not Represent the Population They Serve
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design, Participants, and Data Collection
2.2. Instruments
2.3. Data Analysis
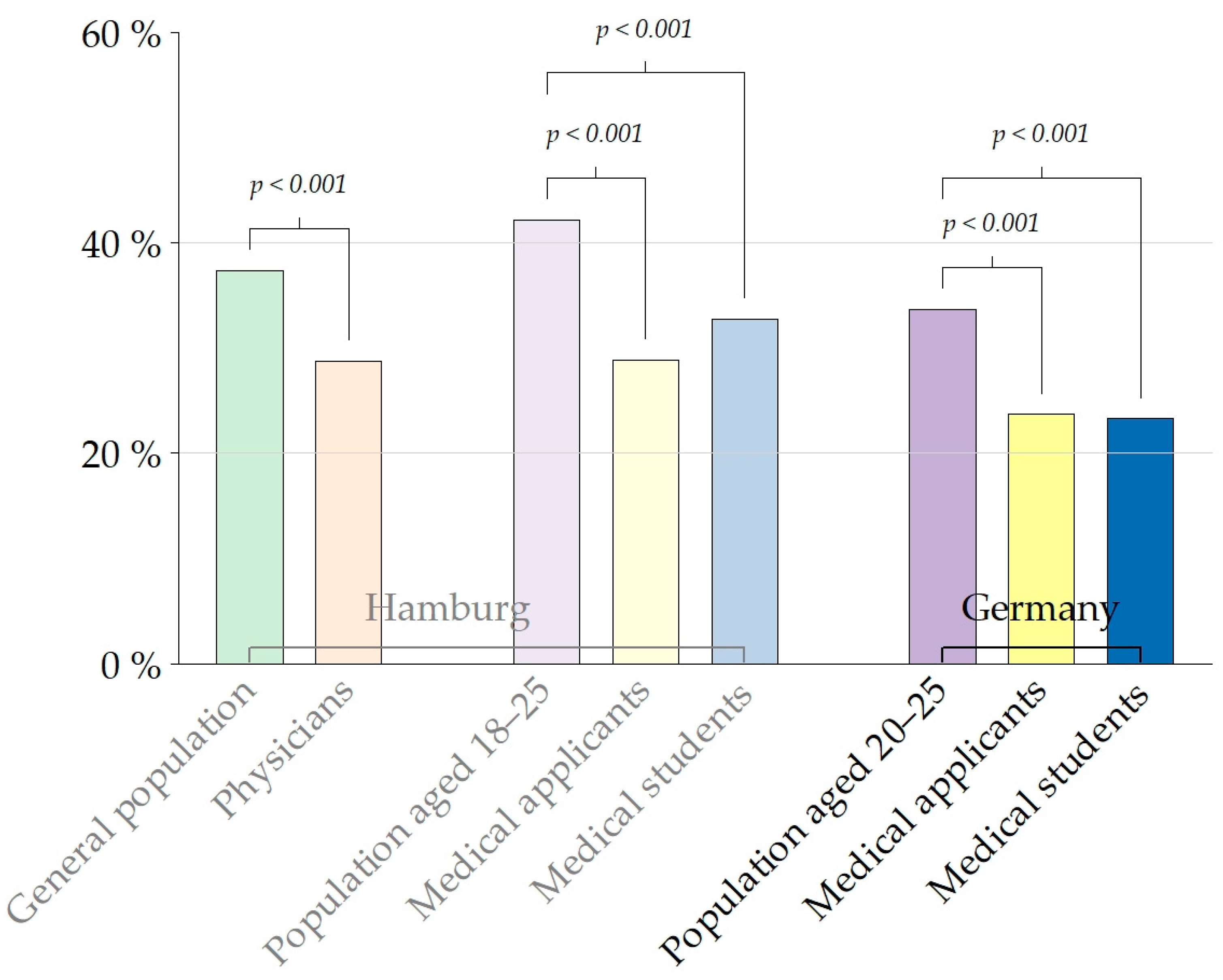
3. Results
4. Discussion
4.1. Socio-Economic Diversity
4.2. Cultural Diversity
4.3. Practical and Political Implications
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cooper, L.A.; Roter, D.L.; Johnson, R.L.; Ford, D.E.; Steinwachs, D.M.; Powe, N.R. Patient-centered communication, ratings of care, and concordance of patient and physician race. Ann. Intern. Med. 2003, 139, 907–915. [Google Scholar] [CrossRef]
- Marcelin, J.R.; Siraj, D.S.; Victor, R.; Kotadia, S.; Maldonado, Y.A. The Impact of Unconscious Bias in Healthcare: How to Recognize and Mitigate It. J. Infect. Dis. 2019, 220, 62–73. [Google Scholar] [CrossRef]
- Burgess, D.; van Ryn, M.; Dovidio, J.; Saha, S. Reducing racial bias among health care providers: Lessons from social-cognitive psychology. J. Gen. Intern. Med. 2007, 22, 882–887. [Google Scholar] [CrossRef] [PubMed]
- van Ryn, M.; Burke, J. The effect of patient race and socio-economic status on physicians’ perceptions of patients. Soc. Sci. Med. 2000, 50, 813–828. [Google Scholar] [CrossRef]
- Ha, J.F.; Longnecker, N. Doctor-patient communication: A review. Ochsner J. 2010, 10, 38–43. [Google Scholar] [PubMed]
- Golubinski, V.; Wild, E.M.; Winter, V.; Schreyögg, J. Once is rarely enough: Can social prescribing facilitate adherence to non-clinical community and voluntary sector health services? Empirical evidence from Germany. BMC Public Health 2020, 20, 1827. [Google Scholar] [CrossRef]
- Saizan, A.L.; Douglas, A.; Elbuluk, N.; Taylor, S. A diverse nation calls for a diverse healthcare force. EClinicalMedicine 2021, 34, 100846. [Google Scholar] [CrossRef] [PubMed]
- Komaromy, M.; Grumbach, K.; Drake, M.; Vranizan, K.; Lurie, N.; Keane, D.; Bindman, A.B. The role of black and Hispanic physicians in providing health care for underserved populations. N. Engl. J. Med. 1996, 334, 1305–1310. [Google Scholar] [CrossRef]
- Walker, K.O.; Moreno, G.; Grumbach, K. The association among specialty, race, ethnicity, and practice location among California physicians in diverse specialties. J. Natl. Med. Assoc. 2012, 104, 46–52. [Google Scholar] [CrossRef]
- Younger, K.; Gascoine, L.; Menzies, V.; Torgerson, C. A systematic review of evidence on the effectiveness of interventions and strategies for widening participation in higher education. J. Furth. High. Educ. 2019, 43, 742–773. [Google Scholar] [CrossRef]
- Lokko, H.N.; Chen, J.A.; Parekh, R.I.; Stern, T.A. Racial and Ethnic Diversity in the US Psychiatric Workforce: A Perspective and Recommendations. Acad. Psychiatry 2016, 40, 898–904. [Google Scholar] [CrossRef] [PubMed]
- Santhosh, L.; Babik, J.M. Diversity in the Pulmonary and Critical Care Medicine Pipeline. Trends in Gender, Race, and Ethnicity among Applicants and Fellows. ATS Sch. 2020, 1, 152–160. [Google Scholar] [CrossRef]
- Wang, N.C. Diversity, Inclusion, and Equity: Evolution of Race and Ethnicity Considerations for the Cardiology Workforce in the United States of America from 1969 to 2019. J. Am. Heart Assoc. 2020, 9, e015959. [Google Scholar] [CrossRef] [PubMed]
- White, M.J.; Wyse, R.J.; Ware, A.D.; Deville, C. Current and Historical Trends in Diversity by Race, Ethnicity, and Sex Within the US Pathology Physician Workforce. Am. J. Clin. Pathol. 2020, 154, 450–458. [Google Scholar] [CrossRef]
- Wyse, R.; Hwang, W.T.; Ahmed, A.A.; Richards, E.; Deville, C., Jr. Diversity by Race, Ethnicity, and Sex within the US Psychiatry Physician Workforce. Acad. Psychiatry 2020, 44, 523–530. [Google Scholar] [CrossRef]
- Morris, D.B.; Gruppuso, P.A.; McGee, H.A.; Murillo, A.L.; Grover, A.; Adashi, E.Y. Diversity of the National Medical Student Body—Four Decades of Inequities. N. Engl. J. Med. 2021, 384, 1661–1668. [Google Scholar] [CrossRef]
- Shahriar, A.A.; Puram, V.V.; Miller, J.M.; Sagi, V.; Castañón-Gonzalez, L.A.; Prasad, S.; Crichlow, R. Socioeconomic Diversity of the Matriculating US Medical Student Body by Race, Ethnicity, and Sex, 2017–2019. JAMA Netw. Open 2022, 5, e222621. [Google Scholar] [CrossRef] [PubMed]
- Medical Schools Council: Selecting for Excellence Final Report. Available online: https://www.medschools.ac.uk/media/1203/selecting-for-excellence-final-report.pdf (accessed on 22 March 2023).
- Steven, K.; Dowell, J.; Jackson, C.; Guthrie, B. Fair access to medicine? Retrospective analysis of UK medical schools application data 2009–2012 using three measures of socioeconomic status. BMC Med. Educ. 2016, 16, 11. [Google Scholar] [CrossRef]
- Hochschul-Bildungs-Report 2020, Abschlussbericht. Hochschulbildung in der Transformation; Stifterverband: Essen, Germany, 2022; p. 13. [Google Scholar]
- Middendorff, E.; Poskowsky, J.; Kandulla, M.; Netz, N. Die wirtschaftliche und Soziale Lage der Studierenden in Deutschland 2012. Sozialerhebung des Deutschen Studentenwerks Durchgeführt Durch das HIS Institut für Hochschulforschung. Available online: https://www.studentenwerke.de/sites/default/files/01_20-SE-Hauptbericht.pdf (accessed on 22 March 2023).
- Schwarzer, A.; Fabian, G. Medizinerreport 2012—Berufsstart und Berufsverlauf von Humanmedizinerinnen und Humanmedizinern. Available online: http://www.mft-online.de/files/medizinerreport_2012.pdf (accessed on 22 March 2023).
- Statistisches Bundesamt, Bevölkerung mit Migrationshintergrund, Ergebnisse des Mikrozensus 2021. Available online: https://www.destatis.de/DE/Themen/Gesellschaft-Umwelt/Bevoelkerung/Migration-Integration/Publikationen/_publikationen-innen-migrationshintergrund.html (accessed on 23 March 2023).
- Fikrat-Wevers, S.; De Leng, W.E.; Van Den Broek, W.W.; Woltman, A.M.; Stegers-Jager, K.M. The added value of free preparatory activities for widening access to medical education: A multi-cohort study. BMC Med. Educ. 2023, 23, 196. [Google Scholar] [CrossRef]
- Lampert, T.; Hoebel, J.; Kuntz, B.; Müters, S.; Kroll, L.E. Socioeconomic status and subjective social status measurement in KiGGS Wave 2. J. Health Monit. 2018, 3, 108–125. [Google Scholar]
- Holm, S. A Simple Sequentially Rejective Multiple Test Procedure. Scand. J. Stat. 1979, 6, 65–70. [Google Scholar]
- van Buuren, S. Predictive Mean Matching. In Flexible Imputation of Missing Data, 2nd ed.; Van Buuren, S., Ed.; Chapman and Hall/CRC: Boca Raton, FL, USA, 2018; Available online: https://stefvanbuuren.name/fimd/sec-pmm.html (accessed on 23 March 2023).
- Meyer, H.; Zimmermann, S.; Hissbach, J.; Klusmann, D.; Hampe, W. Selection and academic success of medical students in Hamburg, Germany. BMC Med. Educ. 2019, 19, 23. [Google Scholar] [CrossRef] [PubMed]
- R Core Team: R: A Language and Environment for Statistical Computing. Available online: https://www.R-project.org/ (accessed on 23 March 2023).
- Buuren, S.; Groothuis-Oudshoorn, C. MICE: Multivariate Imputation by Chained Equations in R. J. Stat. Softw. 2011, 45, 1–67. [Google Scholar] [CrossRef]
- Youngclaus, J.R.L. An Updated Look at the Economic Diversity of U.S. Medical Students. AAMC 2018, 18, 1–5. [Google Scholar]
- Polyakova, M.; Persson, P.; Hofmann, K.; Jena, A.B. Does medicine run in the family—Evidence from three generations of physicians in Sweden: Retrospective observational study. BMJ 2020, 371, m4453. [Google Scholar] [CrossRef]
- Mendoza-Sanchez, I.; deGruyter, J.N.; Savage, N.T.; Polymenis, M. Undergraduate GPA Predicts Biochemistry PhD Completion and Is Associated with Time to Degree. CBE Life Sci. Educ. 2022, 21, ar19. [Google Scholar] [CrossRef]
- Watrin L, Geiger M, Levacher J, Spinath B, Wilhelm O: Development and Initial Validation of an Admission Test for Bachelor Psychology Studies. Front. Educ. 2022, 7, 1–12.
- OECD. Results from PISA 2015. Available online: https://www.oecd.org/pisa/pisa-2015-results-in-focus.pdf (accessed on 23 March 2023).
- Autorengruppe Bildungsberichterstattung: Bildung in Deutschland. 2018. Available online: https://www.bildungsbericht.de/de/bildungsberichte-seit-2006/bildungsbericht-2018/pdf-bildungsbericht-2018/bildungsbericht-2018.pdf (accessed on 22 March 2023).
- Düvell, F. Shifts in the global migration order and migration transitions in Europe: The cases of Turkey and Russia. Comp. Migr. Stud. 2020, 8, 45. [Google Scholar] [CrossRef] [PubMed]
- Bafekr, S.; Leman, J. Highly-qualified Iranian immigrants in Germany: The role of ethnicity and culture. J. Ethn. Migr. Stud. 1999, 25, 95–112. [Google Scholar] [CrossRef]
- Baines, L.; Gooch, D.; Ng-Knight, T. Do widening participation interventions change university attitudes in UK school children? A systematic review of the efficacy of UK programmes, and quality of evaluation evidence. Educ. Rev. 2022, 1–20. [Google Scholar] [CrossRef]
- Girotti, J.A.; Park, Y.S.; Tekian, A. Ensuring a fair and equitable selection of students to serve society’s health care needs. Med. Educ. 2015, 49, 84–92. [Google Scholar] [CrossRef]
- Joy, T.R. Strategies For Enhancing Equity, Diversity, and Inclusion in Medical School Admissions-A Canadian Medical School’s Journey. Front. Public Health 2022, 10, 879173. [Google Scholar] [CrossRef]
- Leduc, J.M.; Kpadé, V.; Bizimungu, S.; Bourget, M.; Gauthier, I.; Bourdy, C.; Chétrit, E.; Razack, S. Black students applying and admitted to medicine in the province of Quebec, Canada: What do we know so far? Can. Med. Educ. J. 2021, 12, 78–81. [Google Scholar] [CrossRef]
- Ten Cate, O. Rationales for a Lottery among the Qualified to Select Medical Trainees: Decades of Dutch Experience. J. Grad. Med. Educ. 2021, 13, 612–615. [Google Scholar] [CrossRef] [PubMed]
- Lakhan, S.E. Diversification of U.S. medical schools via affirmative action implementation. BMC Med. Educ. 2003, 3, 6. [Google Scholar] [CrossRef] [PubMed]
- Thomas, B.R.; Dockter, N. Affirmative Action and Holistic Review in Medical School Admissions: Where We Have Been and Where We Are Going. Acad. Med. 2019, 94, 473–476. [Google Scholar] [CrossRef] [PubMed]
- Medical School Council: Entry Requirements for UK Medical Schools: 2022 Entry. Available online: https://www.medschools.ac.uk/media/2877/entry-requirements-document-2022-digital.pdf (accessed on 22 March 2023).
- Sachverständigenrat für Integration und Migration: Systemrelevant: Migration als Stütze und Herausforderung für die Gesundheitsversorgung in Deutschland. Available online: https://www.svr-migration.de/publikationen/jahresgutachten/jahresgutachten-2022/ (accessed on 22 March 2023).
- Cometto, G.; Tulenko, K.; Muula, A.S.; Krech, R. Health workforce brain drain: From denouncing the challenge to solving the problem. PLoS Med. 2013, 10, e1001514. [Google Scholar] [CrossRef]
- Saluja, S.; Rudolfson, N.; Massenburg, B.B.; Meara, J.G.; Shrime, M.G. The impact of physician migration on mortality in low and middle-income countries: An economic modelling study. BMJ Glob Health. 2020, 5, e001535. [Google Scholar] [CrossRef]
- Ammi, M.; Fooken, J.; Klein, J.; Scott, A. Does doctors’ personality differ from those of patients, the highly educated and other caring professions? An observational study using two nationally representative Australian surveys. BMJ Open 2023, 13, e069850. [Google Scholar] [CrossRef]
- Galizzi, M.M.; Miraldo, M.; Stavropoulou, C.; van der Pol, M. Doctor–patient differences in risk and time preferences: A field experiment. J. Health Econ. 2016, 50, 171–182. [Google Scholar] [CrossRef]


| Characteristic | SEKHHA Survey | Stav Survey | |||
|---|---|---|---|---|---|
| Hamburg Physicians (N = 1457) | Hamburg Medical Applicants (N = 717) | Hamburg Medical Students (N = 195) | Medical Applicants in Germany (N = 2013) | Medical Students in Germany (N = 1256) | |
| Female Gender (N) | 58.5% (853) | 72.1% (517) | 66.7% (130) | 74.6% (1502) | 73.3% (921) |
| Mean Age (SD) | 48.6 (14.6) | 22.9 (2.9) | 24.1 (4.5) | 22.5 (3.2) | 22.4 (3.3) |
| German citizenship (N) | 95.2% (1387) | 95.8% (687) | 97.4% (190) | 96.9% (1950) | 97.6% (1226) |
| German native language (N) | 88.4% (1288) | 90.4% (648) | 88.7% (173) | 93.2% (1877) | 93.8% (1178) |
| Highschool GPA * Mean (SD) | 1.9 (0.6) | 1.7 (0.4) | 1.5 (0.5) | 1.7 (0.5) | 1.6 (0.5) |
| Parent physician Mean (SD) | 21.4 (312) | 20.1 (144) | 17.4 (34) | 18.9 (381) | 19.2 (241) |
| Study financed by parents (N) | 69.3% (1010) | 78.0% (559) | 77.9% (152) | 77.0% (1551) | 80.4% (1010) |
| Objective SEB ** Mean (SD) | 16.6 (3.4) | 17.6 (2.8) | 18.0 (2.3) | 17.6 (2.7) | 17.8 (2.6) |
| Subjective SEB *** Mean (SD) | 6.4 (2.0) | 6.6 (1.8) | 6.7 (1.8) | 6.6 (1.8) | 6.8 (1.7) |
| For Each Cultural Subgroup: N (% of General Population)% of Population with Migratory Background | |||||||
|---|---|---|---|---|---|---|---|
| German | Turkish | Polish | Russian | Afghan | Kasach | Syrian | |
| Germany | |||||||
| German census– general population * | 59,564,000 (72.7%) | 2,747,000 (3.4%) 12.3% | 2,176,000 (2.7%) 9.8% | 1,303,000 (1.6%) 5.8% | 337,000 (0.4%) 1.5% | 1,252,000 (1.5%) 5.6% | 1,052,000 (1.3%) 4.7% |
| German census– population aged 20–25 * | 2,963,000 (66.3%) | 226,000 (5.1%) 15% | 97,000 (2.2%) 6.4% | 61,000 (1.4%) 4.0% | 53,000 (1.2%) 3.5% | 56,000 (1.3%) 3.7% | 105,000 (2.3%) 7% |
| Medical applicants in Germany (stav) | 1536 (76.3%) | 47 (2.3%) 9.9% | 31 (1.5%) 6.5% | 25 (1.2%) 5.2% | 19 (0.9%) 4.0% | 24 (1.2%) 5.0% | 13 (0.6%) 2.7% |
| Medical students in Germany (stav) | 963 (76.7%) | 23 (1.8%) 7.8% | 20 (1.6%) 6.8% | 14 (1.1%) 4.8% | 11 (0.9%) 3.8% | 15 (1.2%) 5.1% | 5 (0.4%) 1.7% |
| Hamburg | |||||||
| Hamburg census– general population ** | 1,189,365 (62.6%) | 95,007 (5.0%) 13.4% | 73,444 (3.9%) 10.3% | 36,883 (1.9%) 5.2% | 51,006 (2.7%) 7.2% | 20,676 (1.1%) 2.9% | 20,584 (1.1%) 2.9% |
| Hamburg physicians (SEKHHA) | 1037 (71.2%) | 33 (2.3%) 7.9% | 34 (2.3%) 8.1% | 17 (1.2%) 4.0% | 16 (1.1%) 3.8% | 6 (0.4%) 1.4% | 11 (0.8%) 2.6% |
| Medical applicants in Hamburg (stav) | 510 (71.1%) | 21 (2.9%) 10.1% | 9 (1.3%) 4.3% | 10 (1.4%) 4.8% | 19 (2.6%) 9.2% | 6 (0.8%) 2.9% | 8 (1.1%) 3.9% |
| Medical students in Hamburg (stav) | 131 (67.2%) | 7 (3.6%) 10.9% | 2 (1.0%) 3.1% | 3 (1.5%) 4.7% | 5 (2.6%) 7.8% | 3 (1.5%) 4.7% | 1 (0.5%) 1.6% |
| p-Value | OR | 95% CI | |
|---|---|---|---|
| SEB | <0.001 | 1.070 | 1.028–1.103 |
| High school GPA | <0.001 | 0.370 | 0.305–0.449 |
| Migratory background | 0.217 | 1.154 | 0.919–1.450 |
| Gender | 0.014 | 1.320 | 1.057–1.648 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Groene, O.R.; Huelmann, T.; Hampe, W.; Emami, P. German Physicians and Medical Students Do Not Represent the Population They Serve. Healthcare 2023, 11, 1662. https://doi.org/10.3390/healthcare11121662
Groene OR, Huelmann T, Hampe W, Emami P. German Physicians and Medical Students Do Not Represent the Population They Serve. Healthcare. 2023; 11(12):1662. https://doi.org/10.3390/healthcare11121662
Chicago/Turabian StyleGroene, Oana R., Thorben Huelmann, Wolfgang Hampe, and Pedram Emami. 2023. "German Physicians and Medical Students Do Not Represent the Population They Serve" Healthcare 11, no. 12: 1662. https://doi.org/10.3390/healthcare11121662
APA StyleGroene, O. R., Huelmann, T., Hampe, W., & Emami, P. (2023). German Physicians and Medical Students Do Not Represent the Population They Serve. Healthcare, 11(12), 1662. https://doi.org/10.3390/healthcare11121662





