EASY-NET Program: Methods and Preliminary Results of an Audit and Feedback Intervention in the Emergency Care for Acute Myocardial Infarction in the Lazio Region, Italy
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. A&F Intervention
- -
- Sending periodic reports (feedback) with the results of a set of process and outcome indicators evaluating the in-hospital emergency care for AMI patients, in a defined reference period;
- -
- Inviting the recipients to organize audit meetings in which they should discuss the reported results, identify critical issues and define improvement actions;
- -
- Inviting the recipients to return a form collecting information about the audit meetings characteristics to the research team.
2.3. Indicators and Population
- -
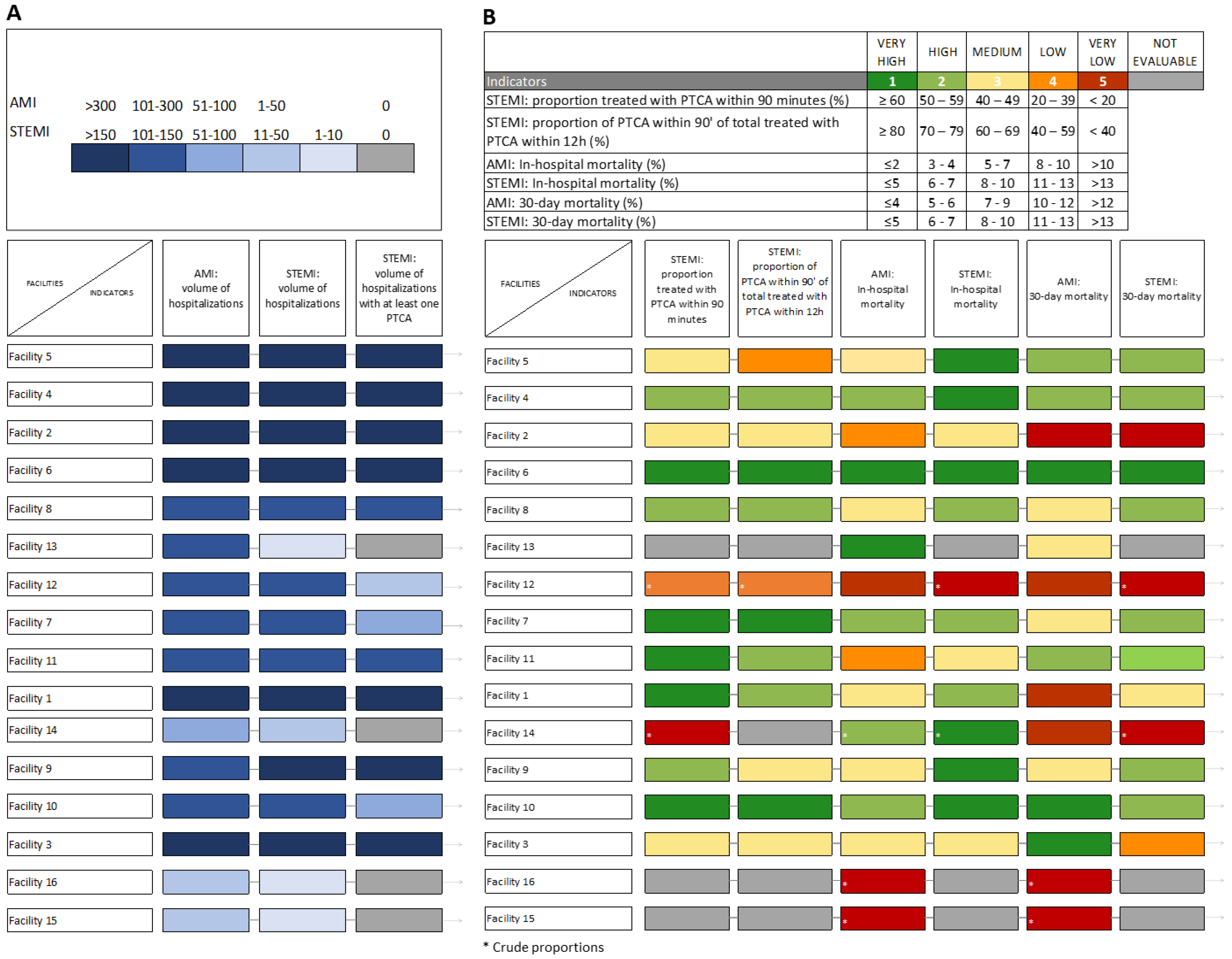
- Three volume indicators to provide a description of the amount of activity in each participating facility, which are useful for the interpretation of process and outcome indicators.
- -
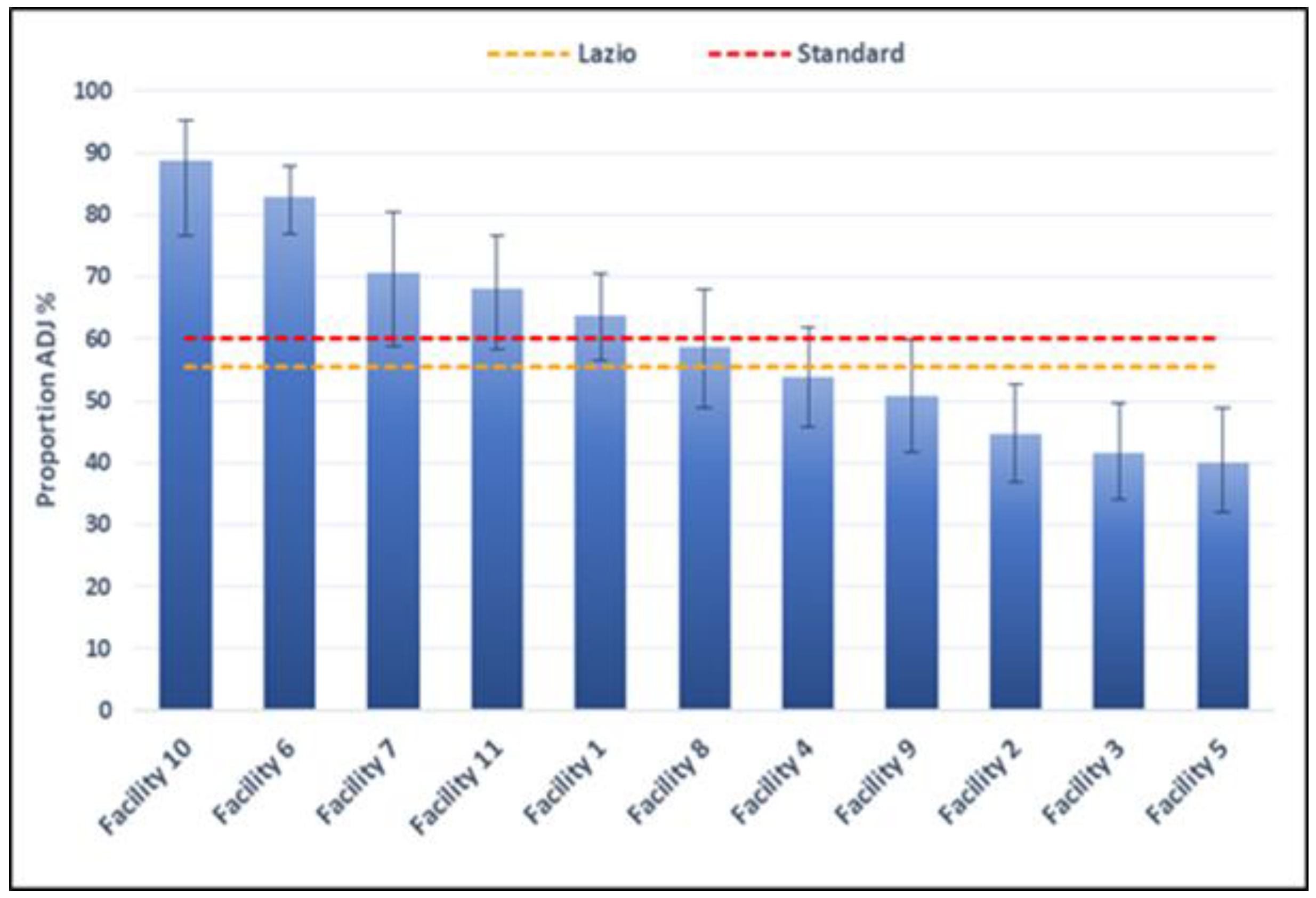
- Two process indicators, evaluating PTCA in ST-segment-elevation myocardial infarction (STEMI) patients. In Italy, the DM 70/2015 indicates as a target value a minimum proportion of patients treated with PTCA within 90 min of 60%. The second indicator is a modified version of the first one calculated with the intention of excluding those patients for whom PTCA is no longer appropriate due to the large timeframe (longer than 12 h) passed since the access in the ER. In these patients, we can consider that PTCA was appropriately not performed.
- -
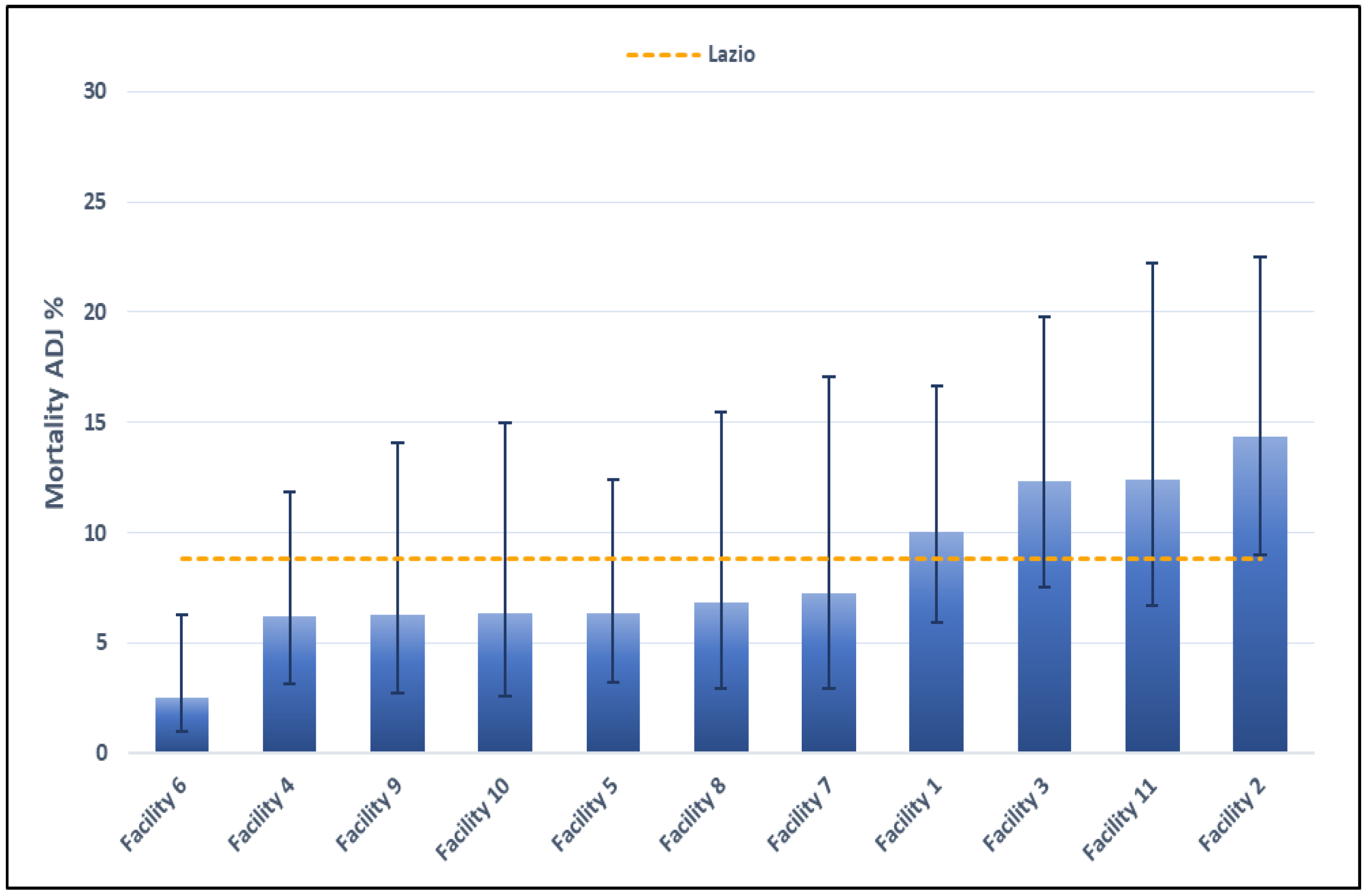
- Four outcome indicators, evaluating 30-day mortality and in-hospital mortality for AMI and STEMI inpatients. As no standard values are available for these indicators, the regional mean was used as reference value.
2.4. Data Sources
2.5. Data Management and Statistical Analysis
3. Results
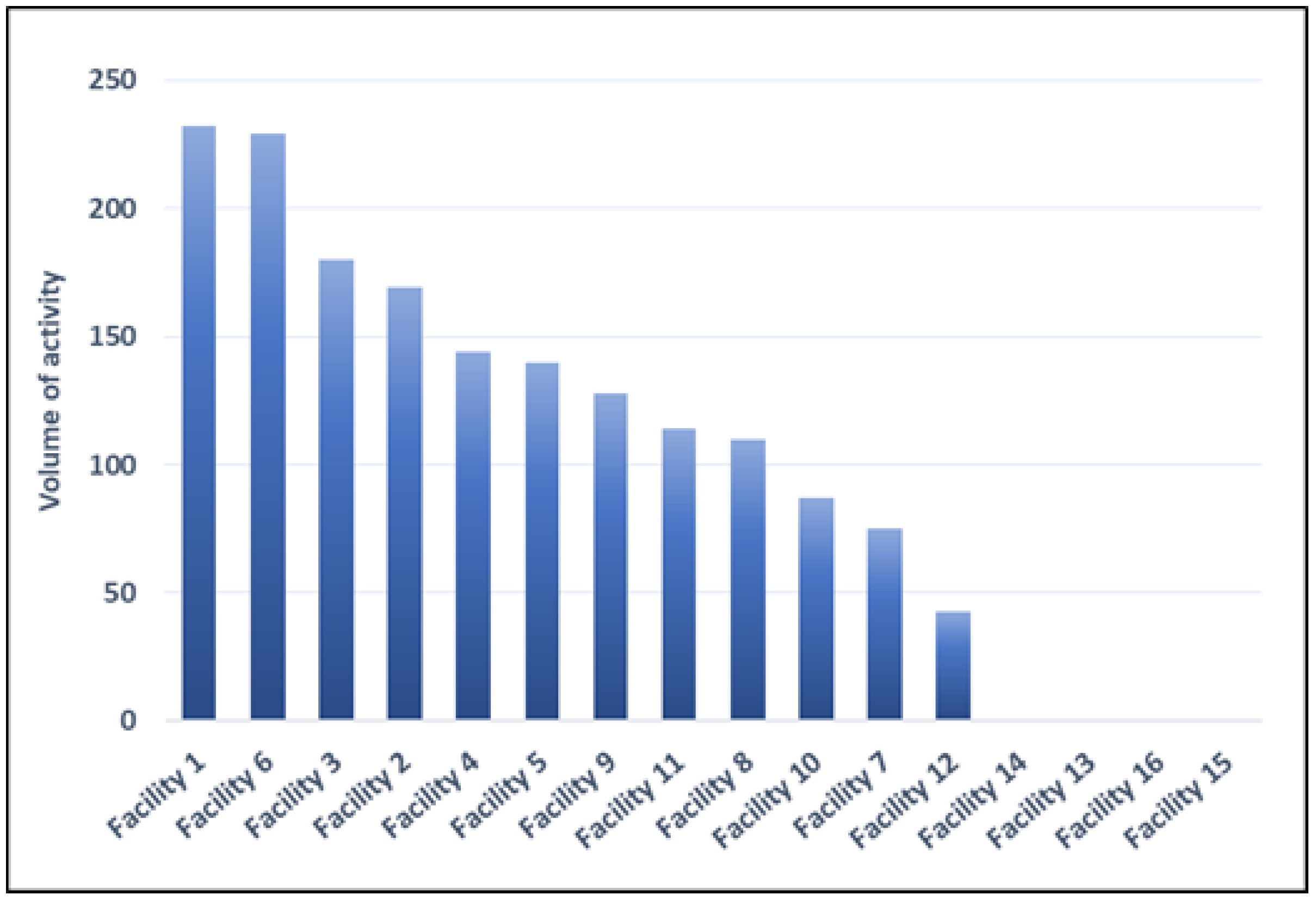
3.1. Volume Indicators
3.2. Process Indicators
3.3. Outcome Indicators
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Agenzia Nazionale per i Servizi Sanitari Regionali (AGENAS). Programma Nazionale Esiti. 2021. Available online: https://pne.agenas.it/ (accessed on 10 May 2022).
- Flottorp, S.A.; Jamtvedt, G.; Gibis, B.; Mckee, M. Using audit and feedback to health professionals to improve the quality and safety of health care. In Proceedings of the Belgian EU Presidency Conference on Investing in Europe’s Health Workforce of Tomorrow: Scope for Innovation and Collaboration, La Hulpe, Belgium, 9–10 September 2010; Available online: https://apps.who.int/iris/handle/10665/332014?show=full (accessed on 15 September 2022).
- Davis, D.A.; Mazmanian, P.E.; Fordis, M.; Van Harrison, R.; Thorpe, K.E.; Perrier, L. Accuracy of physician self-assessment compared with observed measures of competence: A systematic review. JAMA 2006, 296, 1094–1102. [Google Scholar] [CrossRef] [PubMed]
- Hysong, S.J.; Kell, H.J.; Petersen, L.A.; Campbell, B.A.; Trautner, B.V. Theory-based and evidence-based design of audit and feedback programmes: Examples from two clinical interventions studies. BMJ Qual. Saf. 2017, 26, 323–334. [Google Scholar] [CrossRef] [PubMed]
- Ivers, N.; Jamtvedt, G.; Flottorp, S.; Young, J.M.; Odgaard-Jensen, J.; French, S.D.; O’Brien, M.A.; Johansen, M.; Grimshaw, J.; Oxman, A.D. Audit and feedback: Effects on professional practice and healthcare outcomes. Cochrane Database Syst. Rev. 2012, 6, 1465–1858. [Google Scholar] [CrossRef]
- Ivers, N.M.; Grimshaw, J.M.; Jamtvedt, G.; Flottorp, S.; O’Brien, M.A.; French, S.D.; Young, J.; Odgaard-Jensen, J. Growing literature, stagnant Science? Systematic review, meta-regression and cumulative analysis of audit and feedback interventions in health care. J. Gen. Intern. Med. 2014, 29, 1534–1541. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vecchi, S.; Agabiti, N.; Mitrova, S.; Cacciani, L.; Amato, L.; Davoli, M.; Bargagli, A.M. Audit and feedback, and continuous quality improvement strategies to improve the quality of care for type 2 diabetes: A systematic review of literature. Epidemiol. Prev. 2016, 40, 215–223. [Google Scholar] [CrossRef] [PubMed]
- Foy, R.; Eccles, M.P.; Jamtvedt, G.; Young, J.; Grimshaw, J.M.; Baker, R. What do we know about how to do audit and feedback? Pitfalls in applying evidence from a systematic review. BMC Health Serv. Res. 2005, 5, 50. [Google Scholar] [CrossRef] [Green Version]
- Brehaut, J.C.; Colquhoun, H.L.; Eva, K.W.; Carroll, K.; Sales, A.; Michie, S.; Ivers, N.; Grimshaw, J.M. Practice feedback interventions: 15 suggestions for optimizing effectiveness. Ann. Intern. Med. 2016, 164, 435–441. [Google Scholar] [CrossRef]
- Johnson, M.J.; May, C.R. Promoting professional behaviour change in healthcare: What interventions work, and why? A theory-led overview of systematic reviews. BMJ Open 2015, 5, e008592. [Google Scholar] [CrossRef] [Green Version]
- EASY-NET Project Web Site. Available online: https://easy-net.info/ (accessed on 15 July 2022).
- EASY-NET Work Package 1 Lazio Web Site. Available online: https://easy-net.info/progetti/wp1-lazio/ (accessed on 15 July 2022).
- P.Re.Val.E Edition 2021 Web Sites. Available online: https://www.dep.lazio.it/prevale2021/index.php (accessed on 15 September 2022).
- Colquhoun, H.L.; Carroll, K.; Eva, K.W.; Grimshaw, G.M.; Ivers, N.; Michie, S.; Sales, A.; Brehaut, J.C. Advancing the literature on designing audit and feedback interventions: Identifying theory-informed hypotheses. Implement. Sci. 2017, 12, 117. [Google Scholar] [CrossRef]
- Bourrée, F.; Michel, P.; Salmi, L.R. Méthodes de consensus: Revue des méthodes originales et de leurs grandes variantes utilisées en santé publique [Consensus methods: Review of original methods and their main alternatives used in public health]. Rev. Epidemiol. Sante Publique 2008, 56, 415–423. [Google Scholar] [CrossRef]
- Angioletti, C.; Pinnarelli, L.; Colais, P.; Angelici, L.; de Mattia, E.; Davoli, M.; de Belvis, A.G.; Agabiti, N.; Acampora, A. Audit and Feedback in the Hospitals of the Emergency Networks in the Lazio Region, Italy: A Cross-Sectional Evaluation of the State of Implementation. Healthcare 2022, 11, 24. [Google Scholar] [CrossRef] [PubMed]
- Yousuf, M.I. Using experts’ opinions through Delphi technique. Pract. Assess. Res. Eval. 2007, 12, 1–8. [Google Scholar] [CrossRef]
- Ministerial Decree 2 April 2015 n. 70. (G.U. 4 2015, n. 127). Available online: https://www.camera.it/temiap/2016/09/23/OCD177-2353.pdf (accessed on 20 September 2022).
- World Health Organization Working Group. The International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM); National Center for Health Statistics: Hyattsville, MD, USA, 2007.
- Renzi, C.; Sorge, C.; Fusco, D.; Agabiti, N.; Davoli, M.; Perucci, C.A. Reporting of quality indicators and improvement in hospital performance: The P.Re.Val.E. regional outcome evaluation program. Health Serv. Res. 2012, 47, 1880–1901. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Colais, P.; Pinnarelli, L.; Mataloni, F.; Giordani, B.; Duranti, G.; D’Errigo, P.; Rosato, S.; Seccareccia, F.; Baglio, G.; Davoli, M.; et al. The national outcomes evaluation programme in Italy: The impact of publication of health indicators. Int. J. Environ. Res. Public Health 2022, 19, 11685. [Google Scholar] [CrossRef]
- Jenks, G.F. The data model concept in statistical mapping. Int. Yearb. Cartogr. 1967, 7, 186–190. [Google Scholar]
- P.Re.Val.E Edition 2022 Web Site. Volume of Hospitalization for AMI from 2012 to 2021. Available online: https://www.dep.lazio.it/prevale2022/risultati/tipo5/home_tipo5.php?ind=122&tipo=5&area=1 (accessed on 15 September 2022).
- Amato, L.; Fusco, D.; Acampora, A.; Bontempi, K.; Rosa, A.C.; Colais, P.; Cruciani, F.; D’Ovidio, M.; Mataloni, F.; Minozzi, S.; et al. Volume and health outcomes: Evidence from systematic reviews and from evaluation of Italian hospital data. Epidemiol. Prev. 2017, 41 (Suppl. S2), 1–128. [Google Scholar] [CrossRef]
- Park, J.; Choi, K.H.; Lee, J.M.; Kim, H.K.; Hwang, D.; Rhee, T.M.; Kim, J.; Park, T.K.; Yang, J.H.; Song, Y.B.; et al. KAMIR-NIH (Korea Acute Myocardial Infarction Registry–National Institutes of Health) investigators. Prognostic implications of door-to-balloon time and onset-to-door time on mortality in patients with ST-segment-elevation myocardial infarction treated with primary percutaneous coronary intervention. J. Am. Heart Assoc. 2019, 8, e012188. [Google Scholar] [CrossRef] [Green Version]
- Laforgia, P.L.; Auguadro, C.; Bronzato, S.; Durante, A. The reduction of mortality in acute myocardial infarction: From bed rest to future directions. Int. J. Prev. Med. 2022, 13, 56. [Google Scholar]
- Fusco, D.; Barone, A.P.; Sorge, C.; D’Ovidio, M.; Stafoggia, M.; Lallo, A.; Davoli, M.; Perucci, C.A. P.Re.Val.E.: Outcome research program for the evaluation of health care quality in Lazio, Italy. BMC Health Serv. Res. 2012, 12, 25. [Google Scholar] [CrossRef] [Green Version]
- Aylin, P.; Bottle, A.; Majeed, A. Use of administrative data or clinical databases as predictors of risk of death in hospital: Comparison of models. BMJ 2007, 334, 1044. [Google Scholar] [CrossRef] [Green Version]
- Di Martino, M.; Fusco, D.; Colais, P.; Pinnarelli, L.; Davoli, M.; Perucci, C.A. Differential misclassification of confounders in comparative evaluation of hospital care quality: Caesarean sections in Italy. BMC Public Health 2014, 14, 1049. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lezzoni, L.I. Assessing quality using administrative data. Ann. Intern. Med. 1997, 127, 666–674. [Google Scholar] [CrossRef]

| Indicators | Calculation | Reference Value |
|---|---|---|
| AMI: volume of hospitalizations | Number of hospitalizations of patients diagnosed with AMI | 100/y (DM 70/2015) |
| STEMI: volume of hospitalizations | Number of hospitalizations of patients diagnosed with STEMI | NA |
| STEMI: volume of hospitalizations with at least one PTCA | Number of hospitalizations of patients diagnosed with STEMI who received at least one PTCA | NA |
| STEMI: proportion treated with PTCA within 90 min | Number of hospitalized patients diagnosed with STEMI who received PTCA within 90 min from access to the ER/number of hospitalization of patients diagnosed with STEMI | ≥60% (DM 70/2015) |
| STEMI: proportion of PTCA within 90 min of those treated with PTCA within 12 h | Number of hospitalized patients diagnosed with STEMI who received PTCA within 90 min from access to the ER/number of hospitalization of patients diagnosed with STEMI who received PTCA within 12 h | NA Compared to regional mean |
| AMI: in-hospital mortality | Number of hospitalized patients diagnosed with AMI who died during the hospital stay/number of hospitalized patients diagnosed with AMI | NA Compared to regional mean |
| STEMI: in-hospital mortality | Number of hospitalized patients diagnosed with STEMI who died during the hospital stay/number of hospitalized patients diagnosed with STEMI | NA Compared to regional mean |
| AMI: 30-day mortality | Number of hospitalized patients diagnosed with STEMI who died during the 30 days after hospital discharge/number of hospitalized patients diagnosed with AMI | NA Compared to regional mean |
| STEMI: 30-day mortality | Number hospitalized patients diagnosed with STEMI who died during the 30 days after hospital discharge/number of hospitalized patients diagnosed with STEMI | NA Compared to regional mean |
| Facility | Volume of Activity | ||
|---|---|---|---|
| 2019 | 2020 | 2021 | |
| Lazio | 9794 | 8061 | 7766 |
| Facility 1 | 710 | 584 | 514 |
| Facility 2 | 506 | 413 | 442 |
| Facility 3 | 696 | 420 | 418 |
| Facility 4 | 470 | 363 | 416 |
| Facility 5 | 491 | 427 | 378 |
| Facility 6 | 426 | 378 | 354 |
| Facility 7 | 399 | 306 | 295 |
| Facility 8 | 289 | 266 | 292 |
| Facility 9 | 389 | 306 | 266 |
| Facility 10 | 396 | 323 | 231 |
| Facility 11 | 253 | 230 | 218 |
| Facility 12 | 305 | 237 | 143 |
| Facility 13 | 97 | 75 | 91 |
| Facility 14 | 106 | 72 | 56 |
| Facility 15 | 51 | 27 | 20 |
| Facility 16 | 9 | 10 | 7 |
| Facility | Volume of Activity | ||
|---|---|---|---|
| 2019 | 2020 | 2021 | |
| Lazio | 2870 | 2625 | 2719 |
| Facility 1 | 369 | 274 | 232 |
| Facility 6 | 215 | 188 | 229 |
| Facility 3 | 217 | 178 | 180 |
| Facility 2 | 172 | 140 | 169 |
| Facility 4 | 162 | 139 | 144 |
| Facility 5 | 156 | 146 | 140 |
| Facility 9 | 172 | 118 | 128 |
| Facility 11 | 121 | 121 | 114 |
| Facility 8 | 114 | 113 | 110 |
| Facility 10 | 112 | 99 | 87 |
| Facility 7 | 87 | 80 | 75 |
| Facility 12 | 105 | 72 | 43 |
| Facility 14 | 0 | 0 | 0 |
| Facility 13 | 0 | 1 | 0 |
| Facility 16 | 1 | 0 | 0 |
| Facility 15 | 0 | 0 | 0 |
| Facility | N | Crude % | 95% CI | Adj % | 95% CI | ||
|---|---|---|---|---|---|---|---|
| Lazio | 2601 | 55.48 | 53.56 | 57.38 | _ | _ | _ |
| Facility 10 | 55 | 89.09 | 78.17 | 94.90 | 88.80 | 76.56 | 95.25 |
| Facility 6 | 206 | 82.04 | 76.23 | 86.68 | 82.98 | 76.89 | 87.77 |
| Facility 7 | 71 | 67.61 | 56.06 | 77.34 | 70.66 | 58.68 | 80.39 |
| Facility 11 | 109 | 67.89 | 58.64 | 75.92 | 68.15 | 58.37 | 76.60 |
| Facility 1 | 201 | 66.67 | 59.89 | 72.82 | 63.85 | 56.60 | 70.53 |
| Facility 8 | 110 | 61.82 | 52.49 | 70.35 | 58.73 | 48.91 | 67.93 |
| Facility 4 | 164 | 51.83 | 44.23 | 59.35 | 53.93 | 45.84 | 61.84 |
| Facility 9 | 122 | 54.10 | 45.27 | 62.68 | 50.76 | 41.70 | 59.79 |
| Facility 2 | 161 | 45.96 | 38.45 | 53.67 | 44.68 | 36.97 | 52.67 |
| Facility 3 | 168 | 40.48 | 33.35 | 48.03 | 41.62 | 34.09 | 49.56 |
| Facility 5 | 136 | 40.44 | 32.57 | 48.84 | 40.14 | 32.00 | 48.88 |
| Facility 12 | 39 | 38.46 | 24.89 | 54.10 | _ | _ | _ |
| Facility 14 | 6 | 0.00 | 0.00 | _ | _ | _ | _ |
| Facility 15 | 3 | 0.00 | 0.00 | _ | _ | _ | _ |
| Facility 13 | 2 | 0.00 | 0.00 | _ | _ | _ | _ |
| Facility 16 | 1 | 0.00 | 0.00 | _ | _ | _ | _ |
| Facility | N | Crude % | 95% CI | Adj % | 95% CI | ||
|---|---|---|---|---|---|---|---|
| Lazio | 2623 | 8.84 | 7.82 | 9.99 | _ | _ | _ |
| Facility 6 | 206 | 2.43 | 1.04 | 5.56 | 2.54 | 1.01 | 6.31 |
| Facility 4 | 164 | 7.32 | 4.23 | 12.35 | 6.18 | 3.17 | 11.86 |
| Facility 9 | 122 | 4.92 | 2.27 | 10.32 | 6.31 | 2.75 | 14.09 |
| Facility 10 | 77 | 7.79 | 3.62 | 15.98 | 6.36 | 2.61 | 14.98 |
| Facility 5 | 136 | 8.09 | 4.58 | 13.90 | 6.38 | 3.22 | 12.40 |
| Facility 8 | 110 | 5.45 | 2.52 | 11.39 | 6.82 | 2.92 | 15.45 |
| Facility 7 | 71 | 8.45 | 3.93 | 17.24 | 7.24 | 2.96 | 17.08 |
| Facility 1 | 201 | 8.46 | 5.35 | 13.13 | 10.01 | 5.90 | 16.68 |
| Facility 3 | 168 | 11.90 | 7.84 | 17.67 | 12.32 | 7.53 | 19.79 |
| Facility 11 | 109 | 11.93 | 7.10 | 19.34 | 12.42 | 6.73 | 22.23 |
| Facility 2 | 161 | 13.66 | 9.20 | 19.82 | 14.38 | 8.99 | 22.53 |
| Facility 12 | 39 | 25.64 | 14.57 | 41.08 | _ | _ | _ |
| Facility 15 | 3 | 33.33 | 6.15 | 79.23 | _ | _ | _ |
| Facility 14 | 6 | 33.33 | 9.68 | 70.00 | _ | _ | _ |
| Facility 13 | 2 | 0.00 | _ | _ | _ | _ | _ |
| Facility 16 | 1 | 0.00 | _ | _ | _ | _ | _ |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Angelici, L.; Angioletti, C.; Pinnarelli, L.; Colais, P.; de Mattia, E.; Agabiti, N.; Davoli, M.; Acampora, A. EASY-NET Program: Methods and Preliminary Results of an Audit and Feedback Intervention in the Emergency Care for Acute Myocardial Infarction in the Lazio Region, Italy. Healthcare 2023, 11, 1651. https://doi.org/10.3390/healthcare11111651
Angelici L, Angioletti C, Pinnarelli L, Colais P, de Mattia E, Agabiti N, Davoli M, Acampora A. EASY-NET Program: Methods and Preliminary Results of an Audit and Feedback Intervention in the Emergency Care for Acute Myocardial Infarction in the Lazio Region, Italy. Healthcare. 2023; 11(11):1651. https://doi.org/10.3390/healthcare11111651
Chicago/Turabian StyleAngelici, Laura, Carmen Angioletti, Luigi Pinnarelli, Paola Colais, Egidio de Mattia, Nera Agabiti, Marina Davoli, and Anna Acampora. 2023. "EASY-NET Program: Methods and Preliminary Results of an Audit and Feedback Intervention in the Emergency Care for Acute Myocardial Infarction in the Lazio Region, Italy" Healthcare 11, no. 11: 1651. https://doi.org/10.3390/healthcare11111651
APA StyleAngelici, L., Angioletti, C., Pinnarelli, L., Colais, P., de Mattia, E., Agabiti, N., Davoli, M., & Acampora, A. (2023). EASY-NET Program: Methods and Preliminary Results of an Audit and Feedback Intervention in the Emergency Care for Acute Myocardial Infarction in the Lazio Region, Italy. Healthcare, 11(11), 1651. https://doi.org/10.3390/healthcare11111651