Embedding the Patient-Citizen Perspective into an Operational Framework for the Development and the Introduction of New Technologies in Rehabilitation Care: The Smart&Touch-ID Model
Abstract
:1. Introduction
1.1. Technological Innovation to Meet the Need for Rehabilitation for People with Non-Communicable Diseases
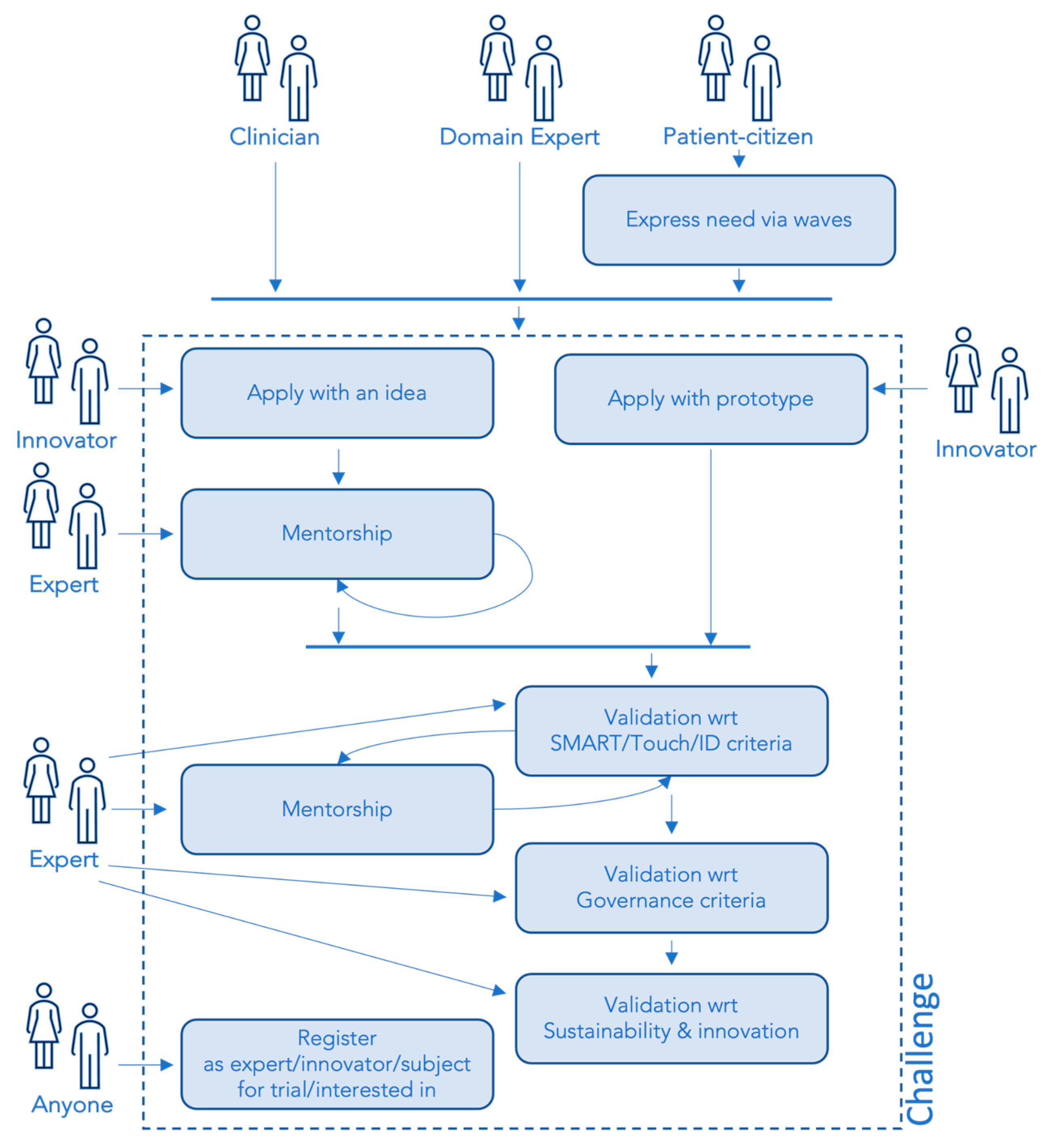
1.2. Embedding Patients’ Perspective into an Operational Framework for Technological Innovation in Rehabilitation Care: The Smart&Touch-ID Approach
2. Materials and Methods
2.1. Participants and Procedure
2.2. Measures
2.2.1. Frequency and Perceived Expertise in the Use of Technologies
2.2.2. Health-Related Quality of Life and Perceived Health of Participants with Chronic Disabilities
2.2.3. Rehabilitation Experiences of Participants with Chronic Disabilities
2.2.4. Basic Attitudes and Beliefs towards Rehabilitation
2.3. Data Analysis
3. Results
3.1. Study Participants
3.2. Frequency and Perceived Proficiency in the Use of Technologies
3.3. Participants with Chronic Disabilities: Clinical Conditions and Perceived Quality of Life
3.4. Participants with Chronic Disabilities: The Rehabilitation Experience
3.5. Basic Attitudes and Beliefs towards Rehabilitation
4. Discussion
5. Limitations and Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Isernia, S.; Pagliari, C.; Morici, N.; Toccafondi, A.; Banfi, P.I.; Rossetto, F.; Borgnis, F.; Tavanelli, M.; Brambilla, L.; Baglio, F.; et al. Telerehabilitation Approaches for People with Chronic Heart Failure: A Systematic Review and Meta-Analysis. J. Clin. Med. 2022, 12, 64. [Google Scholar] [CrossRef] [PubMed]
- Wale, J.L.; Thomas, S.; Hamerlijnck, D.; Hollander, R. Patients and Public Are Important Stakeholders in Health Technology Assessment but the Level of Involvement Is Low—A Call to Action. Res. Involv. Engagem. 2021, 7, 1. [Google Scholar] [CrossRef] [PubMed]
- Vos, T.; Lim, S.S.; Abbafati, C.; Abbas, K.M.; Abbasi, M.; Abbasifard, M.; Abbasi-Kangevari, M.; Abbastabar, H.; Abd-Allah, F.; Abdelalim, A.; et al. Global Burden of 369 Diseases and Injuries in 204 Countries and Territories, 1990–2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef] [PubMed]
- Cieza, A.; Causey, K.; Kamenov, K.; Hanson, S.W.; Chatterji, S.; Vos, T. Global Estimates of the Need for Rehabilitation Based on the Global Burden of Disease Study 2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 2006–2017. [Google Scholar] [CrossRef] [PubMed]
- Topol, E.J. The Topol Review—NHS Health Education England. Available online: https://topol.hee.nhs.uk/ (accessed on 21 February 2023).
- Ellis, T.D.; Colón-Semenza, C.; DeAngelis, T.R.; Thomas, C.A.; Hilaire, M.-H.S.; Earhart, G.M.; Dibble, L.E. Evidence for Early and Regular Physical Therapy and Exercise in Parkinson’s Disease. Semin. Neurol. 2021, 41, 189–205. [Google Scholar] [CrossRef]
- Jelcic, N.; Agostini, M.; Meneghello, F.; Bussè, C.; Parise, S.; Galano, A.; Tonin, P.; Dam, M.; Cagnin, A. Feasibility and Efficacy of Cognitive Telerehabilitation in Early Alzheimer’s Disease: A Pilot Study. Clin. Interv. Aging 2014, 9, 1605–1611. [Google Scholar] [CrossRef]
- Ryrsø, C.K.; Godtfredsen, N.S.; Kofod, L.M.; Lavesen, M.; Mogensen, L.; Tobberup, R.; Farver-Vestergaard, I.; Callesen, H.E.; Tendal, B.; Lange, P.; et al. Lower Mortality after Early Supervised Pulmonary Rehabilitation Following COPD-Exacerbations: A Systematic Review and Meta-Analysis. BMC Pulm. Med. 2018, 18, 154. [Google Scholar] [CrossRef]
- Topol, E.J. A Decade of Digital Medicine Innovation. Sci. Transl. Med. 2019, 11, eaaw7610. [Google Scholar] [CrossRef]
- Dorsey, E.R.; Topol, E.J. State of Telehealth. N. Engl. J. Med. 2016, 375, 154–161. [Google Scholar] [CrossRef]
- Di Tella, S.; Pagliari, C.; Blasi, V.; Mendozzi, L.; Rovaris, M.; Baglio, F. Integrated Telerehabilitation Approach in Multiple Sclerosis: A Systematic Review and Meta-Analysis. J. Telemed. Telecare 2020, 26, 385–399. [Google Scholar] [CrossRef]
- Isernia, S.; Di Tella, S.; Pagliari, C.; Jonsdottir, J.; Castiglioni, C.; Gindri, P.; Salza, M.; Gramigna, C.; Palumbo, G.; Molteni, F.; et al. Effects of an Innovative Telerehabilitation Intervention for People With Parkinson’s Disease on Quality of Life, Motor, and Non-Motor Abilities. Front. Neurol. 2020, 11, 846. [Google Scholar] [CrossRef]
- Isernia, S.; Pagliari, C.; Jonsdottir, J.; Castiglioni, C.; Gindri, P.; Gramigna, C.; Palumbo, G.; Salza, M.; Molteni, F.; Baglio, F.; et al. Efficiency and Patient-Reported Outcome Measures From Clinic to Home: The Human Empowerment Aging and Disability Program for Digital-Health Rehabilitation. Front. Neurol. 2019, 10, 1206. [Google Scholar] [CrossRef]
- de Wit, M.; Guillemin, F.; Grimm, S.; Boonen, A.; Fautrel, B.; Joore, M. Patient Engagement in Health Technology Assessment (HTA) and the Regulatory Process: What about Rheumatology? RMD Open. 2020, 6, e001286. [Google Scholar] [CrossRef]
- Directorate-General for Research and Innovation (European Commission). Options for Strengthening Responsible Research and Innovation: Report of the Expert Group on the State of Art in Europe on Responsible Research and Innovation; Publications Office of the European Union: Luxembourg, 2013; ISBN 978-92-79-28233-1. [Google Scholar]
- PROCS—SCAI Group. Available online: https://www.grupposcai.it/en/procs/ (accessed on 20 May 2023).
- Facey, K.; Boivin, A.; Gracia, J.; Hansen, H.P.; Lo Scalzo, A.; Mossman, J.; Single, A. Patients’ Perspectives in Health Technology Assessment: A Route to Robust Evidence and Fair Deliberation. Int. J. Technol. Assess. Health Care 2010, 26, 334–340. [Google Scholar] [CrossRef]
- Drummond, M.; Torbica, A.; Tarricone, R. Should Health Technology Assessment Be More Patient Centric? If so, How? Eur. J. Health Econ. 2020, 21, 1117–1120. [Google Scholar] [CrossRef]
- Milevska-Kostova, N.; Duddi, S.R.D.; Cooper, R.J. Role of Patients’ Organizations in Health Technology Assessment: A Habermasian System and Lifeworld Perspective. Int. J. Technol. Assess. Health Care 2020, 37, e6. [Google Scholar] [CrossRef]
- Condizioni di Salute e Ricorso ai Servizi Sanitari. Available online: https://www.istat.it/it/archivio/5471 (accessed on 20 May 2023).
- Ustün, T.B.; Chatterji, S.; Kostanjsek, N.; Rehm, J.; Kennedy, C.; Epping-Jordan, J.; Saxena, S.; von Korff, M.; Pull, C. WHO/NIH Joint Project Developing the World Health Organization Disability Assessment Schedule 2.0. Bull. World Health Organ. 2010, 88, 815–823. [Google Scholar] [CrossRef]
- West, S.G.; Finch, J.F.; Curran, P.J. Structural Equation Models with Nonnormal Variables: Problems and Remedies. In Structural Equation Modeling: Concepts, Issues, and Applications; Sage Publications, Inc: Thousand Oaks, CA, USA, 1995; pp. 56–75. ISBN 978-0-8039-5317-8. [Google Scholar]
- Worthington, R.L.; Whittaker, T.A. Scale Development Research: A Content Analysis and Recommendations for Best Practices. Couns. Psychol. 2006, 34, 806–838. [Google Scholar] [CrossRef]
- Comrey, A.L.; Lee, H.B. Interpretation and Application of Factor Analytic Results. In A First Course in Factor Analysis; Psychology Press: New York, NY, USA, 1992; ISBN 978-1-315-82750-6. [Google Scholar]
- Nunnally, J.C.; Bernstein, I.H. Psychometric Theory. In McGraw-Hill Series in Psychology, 3rd ed.; McGraw-Hill: New York, NY, USA, 1994; ISBN 978-0-07-047849-7. [Google Scholar]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Lawrence Erlbaum: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Cotelli, M.; Calabria, M.; Zanetti, O. Cognitive Rehabilitation in Alzheimer’s Disease. Aging Clin. Exp. Res. 2006, 18, 141–143. [Google Scholar] [CrossRef]
- Hong, Y. A Dynamic Constructivist Approach to Culture: Moving from Describing Culture to Explaining Culture. In Understanding Culture: Theory, Research, and Application; Psychology Press: New York, NY, USA, 2009; pp. 3–23. ISBN 978-1-84872-808-0. [Google Scholar]
- Palacholla, R.S.; Fischer, N.; Coleman, A.; Agboola, S.; Kirley, K.; Felsted, J.; Katz, C.; Lloyd, S.; Jethwani, K. Provider- and Patient-Related Barriers to and Facilitators of Digital Health Technology Adoption for Hypertension Management: Scoping Review. JMIR Cardio 2019, 3, e11951. [Google Scholar] [CrossRef]
- Davis, F.D. Perceived Usefulness, Perceived Ease of Use, and User Acceptance of Information Technology. MIS Q. 1989, 13, 319–340. [Google Scholar] [CrossRef]
- Tsertsidis, A.; Kolkowska, E.; Hedström, K. Factors Influencing Seniors’ Acceptance of Technology for Ageing in Place in the Post-Implementation Stage: A Literature Review. Int. J. Med. Inform. 2019, 129, 324–333. [Google Scholar] [CrossRef] [PubMed]
- Savazzi, F.; Isernia, S.; Jonsdottir, J.; Di Tella, S.; Pazzi, S.; Baglio, F. Design and Implementation of a Serious Game on Neurorehabilitation: Data on Modifications of Functionalities along Implementation Releases. Data Brief. 2018, 20, 864–869. [Google Scholar] [CrossRef] [PubMed]
- Triberti, S.; Riva, G. Engaging Users to Design Positive Technologies for Patient Engagement: The Perfect Interaction Model. In Engaging Users to Design Positive Technologies for Patient Engagement: The Perfect Interaction Model; De Gruyter Open: Warsaw, Poland, 2015; pp. 56–65. ISBN 978-3-11-045244-0. [Google Scholar]
- Lowenhaupt Tsing, A. The Mushroom at the End of the World, 2015th ed.; Princeton University Press: Princeton, NJ, USA, 2021; ISBN 978-0-691-22055-0. [Google Scholar]
- Lupton, D. Medicine as Culture: Illness, Disease and the Body, 3rd ed.; SAGE Publications Ltd: London, UK, 2012. [Google Scholar]
- Riva, G.; Baños, R.M.; Botella, C.; Wiederhold, B.K.; Gaggioli, A. Positive Technology: Using Interactive Technologies to Promote Positive Functioning. Cyberpsychol. Behav. Soc. Netw. 2012, 15, 69–77. [Google Scholar] [CrossRef]
| Frequency | Percentage | ||
|---|---|---|---|
| Age | 24 or less | 4 | 4.2 |
| 25–34 | 9 | 9.5 | |
| 35–44 | 11 | 11.6 | |
| 45–54 | 10 | 10.5 | |
| 55–64 | 16 | 16.8 | |
| 65–74 | 23 | 24.2 | |
| 75–84 | 16 | 16.8 | |
| 85 or more | 6 | 6.3 | |
| Gender | Man | 36 | 37.9 |
| Woman | 57 | 60.0 | |
| Other/Prefer not to state | 2 | 2.1 | |
| Living condition (more than one answer possible) | Alone | 22 | 23.2 |
| Partner | 60 | 63.2 | |
| Children | 24 | 25.3 | |
| Caregiver | 1 | 1.1 | |
| A family member (other than a partner and children) | 6 | 6.3 | |
| Someone else | 1 | 1.1 | |
| Education | Primary school diploma | 12 | 12.6 |
| Middle School diploma | 22 | 23.2 | |
| High school diploma | 25 | 26.3 | |
| Degree | 23 | 24.2 | |
| Postgraduate training | 13 | 13.7 | |
| Working status | Paid worker | 38 | 40.0 |
| Retired | 52 | 54.7 | |
| No paid work | 5 | 5.3 | |
| Prevalent chronic disability | Neurological | 22 | 24.2 |
| Cardiovascular | 3 | 8.4 | |
| Pulmonary | 6 | 9.5 | |
| Osteoarticular | 22 | 24.2 | |
| No disability | 42 | 44.2 | |
| Items of the “Use Frequency of Technologies” Scale | Factor Loadings |
|---|---|
| 0.931 | |
| Internet | 0.878 |
| Computer | 0.842 |
| Social network | 0.785 |
| Online reading | 0.745 |
| Smartphone | 0.730 |
| Digital Music | 0.685 |
| Tablet | 0.528 |
| E-gaming | 0.468 |
| Monitoring health with a device | 0.390 |
| Smartwatch | 0.363 |
| Voice home assistant | 0.329 |
| A mobile phone without touch technology | 0.208 |
| Use of … | Age | Never | Once a Month or More Rarely | Sometimes a Month | A Few Times a Week | Everyday |
|---|---|---|---|---|---|---|
| Smartphone | All sample | 16 (16.8%) | 2 (2.1%) | 1 (1.1%) | 3 (3.2%) | 73 (76.8%) |
| Under 65 | 4 (8.0%) | \ | \ | 1 (2.0%) | 45 (90.0%) | |
| Over 65 | 12 (26.7%) | 2 (4.4%) | 1 (2.2%) | 2 (4.4%) | 28 (62.2%) | |
| A mobile phone without touch technology | All sample | 65 (68.4%) | 9 (9.5%) | 1 (1.1%) | 2 (2.1%) | 18 (18.9%) |
| Under 65 | 40 (80.0%) | 2 (4.0%) | 1 (2.0%) | \ | 7 (14.0%) | |
| Over 65 | 25 (55.6%) | 7 (15.6%) | \ | 2 (4.4%) | 11 (24.4%) | |
| Tablet | All sample | 50 (52.6%) | 10 (10.5%) | 13 (13.7%) | 11 (11.6%) | 11 (11.6%) |
| Under 65 | 17 (34.0%) | 8 (16.0%) | 9 (18.0%) | 7 (14.0%) | 9 (18.0%) | |
| Over 65 | 33 (73.3%) | 2 (4.4%) | 4 (8.9%) | 4 (8.9%) | 2 (4.4%) | |
| Computer | All sample | 31 (32.6%) | 7 (7.4%) | 5 (5.3%) | 9 (9.5%) | 43 (45.3%) |
| Under 65 | 6 (12.0%) | 4 (8.0%) | 1 (2.0%) | 6 (12.0%) | 33 (66.0%) | |
| Over 65 | 25 (55.6%) | 3 (6.7%) | 4 (8.9%) | 3 (6.7%) | 10 (22.2%) | |
| Smartwatch | All sample | 72 (75.8%) | 3 (3.2%) | 1 (1.1%) | 5 (5.3%) | 14 (14.7%) |
| Under 65 | 32 (64.0%) | 3 (6.0%) | 1 (2.0%) | 5 (10.0%) | 9 (18.0%) | |
| Over 65 | 40 (89.0%) | \ | \ | \ | 5 (11.1%) | |
| Voice home assistant | All sample | 73 (76.8%) | 5 (5.3%) | 2 (2.1%) | 3 (3.2%) | 12 (12.6%) |
| Under 65 | 33 (66.0%) | 5 (10.0%) | \ | 2 (4.0%) | 10 (20.0%) | |
| Over 65 | 40 (88.9%) | \ | 2 (4.4%) | 1 (2.2%) | 2 (4.4%) | |
| Internet | All sample | 21 (22.1%) | 4 (4.2%) | 3 (3.2%) | 5 (5.3%) | 62 (65.3%) |
| Under 65 | 2 (4.0%) | 2 (4.0%) | 2 (4.0%) | 1 (2.0%) | 43 (86.0%) | |
| Over 65 | 19 (42.2%) | 2 (4.4%) | 1 (2.2%) | 4 (8.9%) | 19 (42.2%) | |
| Social network | All sample | 41 (43.2%) | 2 (2.1%) | 1 (1.1%) | 7 (7.4%) | 44 (46.3%) |
| Under 65 | 11 (22.0%) | 1 (2.0%) | 1 (2.0%) | 5 (10.0%) | 32 (64.0%) | |
| Over 65 | 30 (66.7%) | 1 (2.2%) | \ | 2 (4.4%) | 12 (26.7%) | |
| E-gaming | All sample | 63 (66.3%) | 4 (4.2%) | 8 (8.4%) | 8 (8.4%) | 12 (12.6%) |
| Under 65 | 24 (48.0%) | 3 (6.0%) | 7 (14.0%) | 7 (14.0%) | 9 (18.0%) | |
| Over 65 | 39 (86.7%) | 1 (2.2%) | 1 (2.2%) | 1 (2.2%) | 3 (6.7%) | |
| Online reading | All sample | 30 (31.6%) | 6 (6.3%) | 11 (11.6%) | 21 (22.1%) | 27 (28.4%) |
| Under 65 | 5 (10.0%) | 5 (10.0%) | 9 (18.0%) | 12 (24.0%) | 19 (38.0%) | |
| Over 65 | 25 (55.6%) | 1 (2.2%) | 2 (4.4%) | 9 (20.0%) | 8 (17.8%) | |
| All sample | 30 (31.6%) | 3 (3.2%) | 2 (2.1%) | 8 (8.4%) | 52 (54.7%) | |
| Under 65 | 4 (8.0%) | 3 (6.0%) | \ | 6 (12.0%) | 37 (74.0%) | |
| Over 65 | 26 (57.8%) | \ | 2 (4.4%) | 2 (4.4%) | 15 (33.3%) | |
| Digital Music | All sample | 31 (32.6%) | 10 (10.5%) | 7 (7.4%) | 23 (24.2%) | 24 (25.3%) |
| Under 65 | 7 (14.0%) | 6 (12.0%) | 3 (6.0%) | 14 (28.0%) | 20 (40.0%) | |
| Over 65 | 24 (53.3%) | 4 (8.9%) | 4 (8.9%) | 9 (20.0%) | 4 (8.9%) | |
| Monitoring health with a device | All sample | 51 (53.7%) | 8 (8.4%) | 10 (10.5%) | 12 (12.6%) | 14 (14.7%) |
| Under 65 | 23 (46.0%) | 3 (6.0%) | 8 (16.0%) | 9 (18.0%) | 7 (14.0%) | |
| Over 65 | 28 (62.2%) | 5 (11.1%) | 2 (4.4%) | 3 (6.7%) | 7 (15.6%) |
| Items of the “Proficiency in the Technologies Use” Scale | Factor Loadings |
|---|---|
| Internet | 0.923 |
| Online reading | 0.909 |
| Computer | 0.908 |
| Smartphone | 0.899 |
| Tablet | 0.892 |
| 0.887 | |
| Social network | 0.852 |
| Digital Music | 0.844 |
| E-gaming | 0.757 |
| Monitoring health with a device | 0.740 |
| Smartwatch | 0.722 |
| Voice home assistant | 0.659 |
| A mobile phone without touch technology | 0.430 |
| Use of … | Age | Not at All | A Little | Neither a Little nor Enough | Enough | Very |
|---|---|---|---|---|---|---|
| Smartphone | All sample | 12 (12.6%) | 11 (11.6%) | 12 (12.6%) | 31 (32.6%) | 29 (30.5%) |
| Under 65 | 1 (2.0%) | 3 (6.0%) | 3 (6.0%) | 20 (40.0%) | 23 (46.0%) | |
| Over 65 | 11 (24.4%) | 8 (17.8%) | 9 (20.0%) | 11 (24.4%) | 6 (13.3%) | |
| A mobile phone without touch technology | All sample | 4 (4.2%) | 11 (11.6%) | 14 (14.7%) | 35 (36.8%) | 31 (32.6%) |
| Under 65 | 3 (6.0%) | 4 (8.0%) | 5 (10.0%) | 17 (34.0%) | 21 (42.0%) | |
| Over 65 | 1 (2.2%) | 7 (15.6%) | 9 (20.0%) | 18 (40%) | 10 (22.2%) | |
| Tablet | All sample | 31 (32.6%) | 6 (6.3%) | 13 (13.7%) | 23 (24.2%) | 22 (23.2%) |
| Under 65 | 5 (10.0%) | 1 (2.0%) | 10 (20.0%) | 16 (32.0%) | 18 (36.0%) | |
| Over 65 | 26 (57.8%) | 5 (11.1%) | 3 (6.7%) | 7 (15.6%) | 4 (8.9%) | |
| Computer | All sample | 25 (26.3%) | 8 (8.4%) | 8 (8.4%) | 26 (27.4%) | 28 (29.5%) |
| Under 65 | 3 (6.0%) | 4 (8.0%) | 5 (10.0%) | 16 (32.0%) | 22 (44.0%) | |
| Over 65 | 22 (48.9%) | 4 (8.9%) | 3 (6.7%) | 10 (22.2%) | 6 (13.3%) | |
| Smartwatch | All sample | 38 (40%) | 13 (13.7%) | 10 (10.5%) | 20 (21.1%) | 14 (14.7%) |
| Under 65 | 8 (16.0%) | 8 (16.0%) | 8 (16.0%) | 16 (32.0%) | 10 (20.0%) | |
| Over 65 | 30 (66.7%) | 5 (11.1%) | 2 (4.4%) | 4 (8.9%) | 4 (8.9%) | |
| Voice home assistant | All sample | 48 (50.5%) | 12 (12.6%) | 9 (9.5%) | 13 (13.7%) | 13 (13.7%) |
| Under 65 | 17 (34.0%) | 7 (14.0%) | 5 (10.0%) | 8 (16.0%) | 13 (26.0%) | |
| Over 65 | 31 (68.9%) | 5 (11.1%) | 4 (8.9%) | 5 (11.1%) | \ | |
| Internet | All sample | 16 (16.8%) | 10 (10.5%) | 6 (6.3%) | 21 (22.1%) | 42 (44.2%) |
| Under 65 | 1 (2.0%) | 1 (2.0%) | 3 (6.0%) | 14 (28.0%) | 31 (62.0%) | |
| Over 65 | 15 (33.3%) | 9 (20%) | 3 (6.7%) | 7 (15.6%) | 11 (24.4%) | |
| Social network | All sample | 30 (31.6%) | 10 (10.5%) | 11 (11.6%) | 20 (21.1%) | 24 (25.3%) |
| Under 65 | 6 (12.0%) | 5 (10.0%) | 5 (10.0%) | 16 (32.0%) | 18 (36.0%) | |
| Over 65 | 24 (53.3%) | 5 (11.1%) | 6 (13.3%) | 4 (8.9%) | 6 (13.3%) | |
| E-gaming | All sample | 40 (42.1%) | 9 (9.5%) | 14 (14.7%) | 15 (15.8%) | 17 (17.9%) |
| Under 65 | 7 (14.0%) | 6 (12.0%) | 9 (18.0%) | 13 (26.0%) | 15 (30.0%) | |
| Over 65 | 33 (73.3%) | 3 (6.7%) | 5 (11.1%) | 2 (4.4%) | 2 (4.4%) | |
| Online reading | All sample | 21 (22.1%) | 6 (6.3%) | 9 (9.5%) | 26 (27.4%) | 33 (34.7%) |
| Under 65 | 1 (2.0%) | 2 (4.0%) | 5 (10.0%) | 16 (32.0%) | 26 (52.0%) | |
| Over 65 | 20 (44.4%) | 4 (8.9%) | 4 (8.9%) | 10 (22.2%) | 7 (15.6%) | |
| All sample | 28 (29.5%) | 4 (4.2%) | 2 (2.1%) | 19 (20.0%) | 42 (44.2%) | |
| Under 65 | 3 (6.0%) | 2 (4.0%) | 1 (2.0%) | 11 (22.0%) | 33 (66.0%) | |
| Over 65 | 25 (55.6%) | 2 (4.4%) | 1 (2.2%) | 8 (17.8%) | 9 (20.0%) | |
| Digital Music | All sample | 27 (28.4%) | 8 (8.4%) | 6 (6.3%) | 21 (22.1%) | 33 (34.7%) |
| Under 65 | 3 (6.0%) | 5 (10.0%) | 4 (8.0%) | 9 (18.0%) | 29 (58.0%) | |
| Over 65 | 24 (53.3%) | 3 (6.7%) | 2 (4.4%) | 12 (26.7%) | 4 (8.9%) | |
| Monitoring health with a device | All sample | 32 (33.7%) | 11 (11.6%) | 14 (14.7%) | 20 (21.1%) | 18 (18.9%) |
| Under 65 | 8 (16.0%) | 7 (14.0%) | 7 (14.0%) | 13 (26.0%) | 15 (30.0%) | |
| Over 65 | 24 (53.3%) | 4 (8.9%) | 7 (15.6%) | 7 (15.6%) | 3 (6.7%) |
| Rehabilitation … | Mean | SD | Asym. | Kurt. | Statistic | df | p |
|---|---|---|---|---|---|---|---|
| is useful | 4.58 | 0.88 | −2.67 | 7.49 | (M) 1.65 | / | 0.102 |
| is an engaging activity | 3.98 | 1.02 | −0.88 | 0.23 | (S) −0.97 | 51 | 0.338 |
| helps to manage the activities of daily life better | 4.18 | 1.00 | −1.35 | 1.66 | (W) −2.00 | 37 | 0.053 |
| is necessary for health | 4.58 | 0.77 | −2.59 | 8.68 | (M) 0.76 | / | 0.457 |
| makes feel capable of doing things | 4.13 | 1.03 | −1.29 | 1.32 | (S) −1.48 | 51 | 0.146 |
| helps live better | 4.43 | 0.84 | −1.85 | 4.41 | (S) −0.74 | 51 | 0.461 |
| is accessible to anyone who wants to do it | 2.94 | 1.38 | 0.12 | −1.25 | (S) −0.05 | 51 | 0.959 |
| helps manage the disability better | 4.22 | 0.91 | −1.35 | 2.14 | (S) −1.62 | 51 | 0.111 |
| it is important | 4.52 | 0.89 | −2.44 | 6.51 | (M) 2.15 | / | 0.032 |
| helps to accept one’s illness | 3.66 | 1.22 | −0.47 | −0.92 | (S) −0.00 | 51 | 0.997 |
| is necessary for the well-being | 4.41 | 0.91 | −1.98 | 4.49 | (S) −2.71 | 51 | 0.009 |
| makes feel the protagonist of the treatment | 4.05 | 0.98 | −0.96 | 0.64 | (S) −1.33 | 51 | 0.191 |
| is not boring | 3.58 | 1.25 | −0.40 | −0.85 | (S) −0.49 | 50 | 0.624 |
| helps understand one’s illness | 3.53 | 1.08 | −0.52 | −0.41 | (W) −1.02 | 51 | 0.311 |
| it is worth the effort | 4.34 | 0.96 | −1.79 | 3.33 | (W) −2.43 | 34 | 0.020 |
| helps feel better with others | 3.76 | 1.06 | −0.70 | −0.11 | (S) −1.07 | 51 | 0.288 |
| helps to make you independent in everyday life | 4.19 | 1.07 | −1.36 | 1.19 | (S) −1.33 | 51 | 0.191 |
| improves mood | 3.89 | 0.98 | −0.63 | 0.08 | (S) −2.08 | 51 | 0.043 |
| it does not take too long to get to where they make it | 3.24 | 1.31 | −0.30 | −0.90 | (W) −0.16 | 51 | 0.876 |
| is affordable | 2.97 | 1.24 | 0.13 | −0.85 | (W) −0.36 | 51 | 0.719 |
| is always different | 2.95 | 0.96 | −0.04 | 0.00 | (S) 0.71 | 51 | 0.483 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Realdon, O.; Adorni, R.; Ginelli, D.; Micucci, D.; Blasi, V.; Bellavia, D.; Schettini, F.; Carradore, R.; Polsinelli, P.; D’Addario, M.; et al. Embedding the Patient-Citizen Perspective into an Operational Framework for the Development and the Introduction of New Technologies in Rehabilitation Care: The Smart&Touch-ID Model. Healthcare 2023, 11, 1604. https://doi.org/10.3390/healthcare11111604
Realdon O, Adorni R, Ginelli D, Micucci D, Blasi V, Bellavia D, Schettini F, Carradore R, Polsinelli P, D’Addario M, et al. Embedding the Patient-Citizen Perspective into an Operational Framework for the Development and the Introduction of New Technologies in Rehabilitation Care: The Smart&Touch-ID Model. Healthcare. 2023; 11(11):1604. https://doi.org/10.3390/healthcare11111604
Chicago/Turabian StyleRealdon, Olivia, Roberta Adorni, Davide Ginelli, Daniela Micucci, Valeria Blasi, Daniele Bellavia, Fabrizio Schettini, Roberto Carradore, Pietro Polsinelli, Marco D’Addario, and et al. 2023. "Embedding the Patient-Citizen Perspective into an Operational Framework for the Development and the Introduction of New Technologies in Rehabilitation Care: The Smart&Touch-ID Model" Healthcare 11, no. 11: 1604. https://doi.org/10.3390/healthcare11111604
APA StyleRealdon, O., Adorni, R., Ginelli, D., Micucci, D., Blasi, V., Bellavia, D., Schettini, F., Carradore, R., Polsinelli, P., D’Addario, M., Gui, M., Messina, V., Foglia, E., Steca, P., Mantovani, F., & Baglio, F. (2023). Embedding the Patient-Citizen Perspective into an Operational Framework for the Development and the Introduction of New Technologies in Rehabilitation Care: The Smart&Touch-ID Model. Healthcare, 11(11), 1604. https://doi.org/10.3390/healthcare11111604










