Benefits of Best Practice Guidelines in Spine Fusion: Comparable Correction in AIS with Higher Density and Fewer Complications
Abstract
:1. Introduction
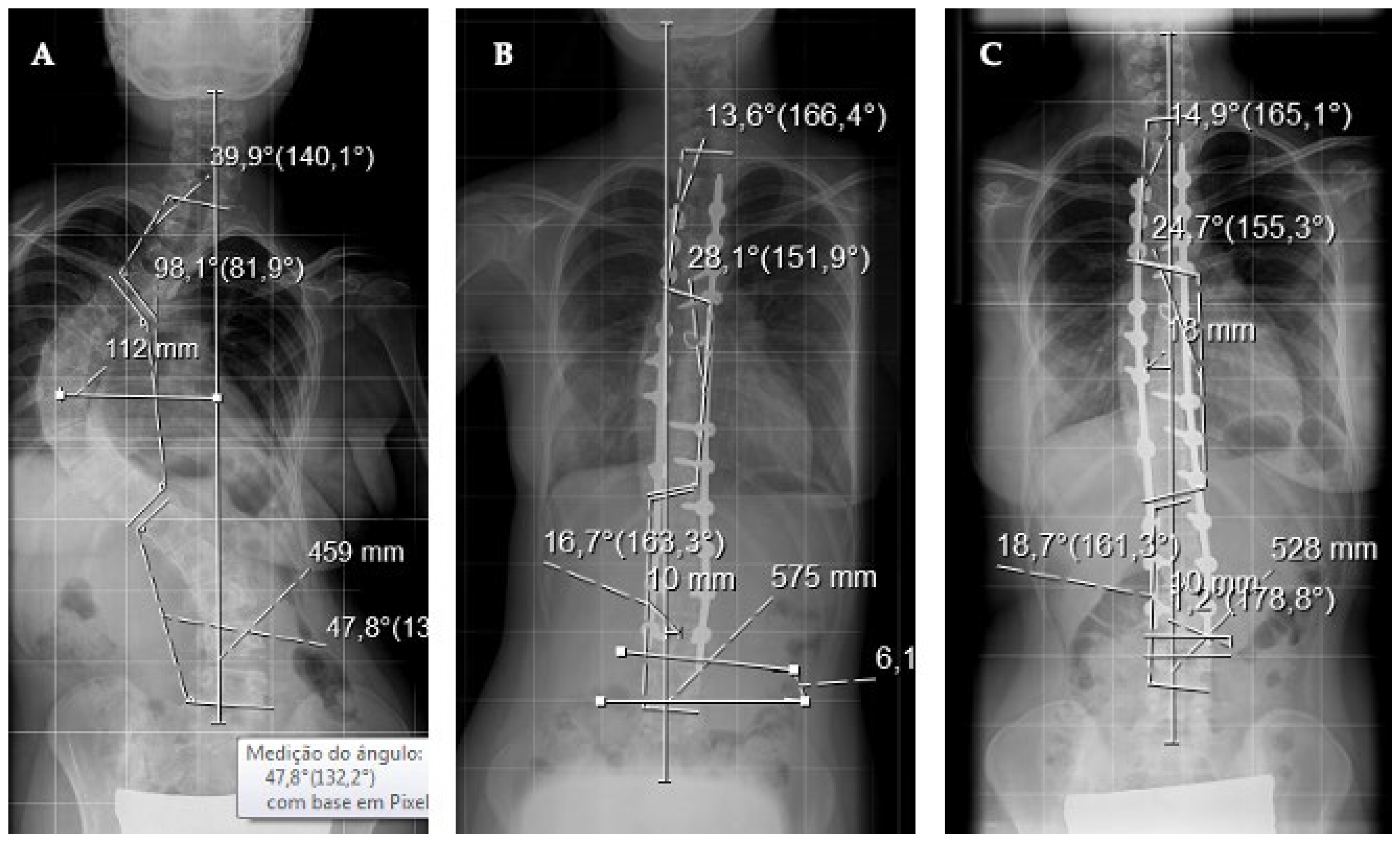
2. Materials and Methods
2.1. Quality and Safety Measures
2.2. Inclusion Criteria
2.3. Radiographic Analysis
2.4. Patient-Reported Outcomes
2.5. Statistical Analysis
3. Results
3.1. Sample
3.2. Two Samples Comparative Analysis
3.3. Major Complications (UORR)
3.4. Quality of Life
3.5. Cost Analysis
3.6. Curve Correction
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Vigneswaran, H.T.; Grabel, Z.J.; Eberson, C.P.; Palumbo, M.A.; Daniels, A.H. Surgical treatment of adolescent idiopathic scoliosis in the United States from 1997 to 2012: An analysis of 20, 346 patients. J. Neurosurg. Pediatr. 2015, 16, 322–328. [Google Scholar] [CrossRef]
- Carreon, L.Y.; Puno, R.M.; Lenke, L.G.; Richards, B.S.; Sucato, D.J.; Emans, J.B.; Erikson, M.A. Neurologic complications following surgery for adolescent idiopathic scoliosis. J. Bone Jt. Surg. Am. 2007, 89, 2427–2432. [Google Scholar] [CrossRef]
- Coe, J.D.; Arlet, V.; Donaldson, W.; Berven, S.; Hanson, D.S.; Mudiyam, R.; Perra, J.H.; Shaffrey, C.I. Complications in spinal fusion for adolescent idiopathic scoliosis in the new millennium. A report of the scoliosis research society morbidity and mortality committee. Spine 2006, 31, 345–349. [Google Scholar] [CrossRef] [PubMed]
- Reames, D.L.; Smith, J.S.; Fu, K.M.G.; Polly, D.W.; Ames, C.P.; Berven, S.H.; Perra, J.H.; Glassman, S.D.; McCarthy, R.E.; Knapp, R.D.; et al. Complications in the surgical treatment of 19,360 cases of pediatric scoliosis: A review of the scoliosis research society morbidity and mortality database. Spine 2011, 36, 1484–1491. [Google Scholar] [CrossRef]
- Mohamad, F.; Parent, S.; Pawelek, J.; Marks, M.; Bastrom, T.; Faro, F.; Newton, P. Perioperative complications after surgical correction in neuromuscular scoliosis. J. Pediatr. Orthop. 2007, 27, 392–397. [Google Scholar] [CrossRef] [PubMed]
- Pugely, A.J.; Martin, C.T.; Gao, Y.; Ilgenfritz, R.; Weinstein, S.L. The incidence and risk factors for short-term morbidity and mortality in pediatric deformity spinal surgery: An analysis of the NSQIP pediatric database. Spine 2011, 39, 1225–1234. [Google Scholar] [CrossRef]
- Institute of Medicine (US) Committee on Quality of Health Care in America. To Err Is Human: Building a Safer Health System; National Academies Press (US): Washington, DC, USA, 2000. [Google Scholar]
- Brooke, B.S.; Dominici, F.; Pronovost, P.J.; Makary, M.A.; Schneider, E.; Pawlik, T.M. Variations in surgical outcomes associated with hospital compliance with safety practices. Surgery 2012, 151, 651–659. [Google Scholar] [CrossRef]
- Tambornino, J.M.; Armbrust, E.N.; Moe, J.H. Harrington Instrumentation in Correction of Scoliosis. A Comparison with Cast Correction. J. Bone Jt. Surg. Am. 1964, 46, 313–321. [Google Scholar] [CrossRef]
- Sotelo, J.; Grueso, F.J. Cotrel-Dubousset instrumentation in neuromuscular spine deformity: A five to eleven-year follow-up study. Acta Orthop. Belg. 2000, 66, 69–76. [Google Scholar]
- Lonner, B.S.; Ren, Y.; Yaszay, B.; Cahill, P.J.; Shah, S.A.; Betz, R.R.; Samdani, A.F.; Shufflebarger, H.L.; Newton, P.O. Evolution of Surgery for Adolescent Idiopathic Scoliosis over 20 Years: Have Outcomes Improved? Spine 2018, 43, 402–410. [Google Scholar] [CrossRef]
- Suk, S.I.; Lee, C.K.; Kim, W.J.; Chung, Y.J.; Park, Y.B. Segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis. Spine 1995, 20, 1399–1405. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.J.; Lenke, L.G.; Cho, S.K.; Bridwell, K.H.; Sides, B.; Blanke, K. Comparative analysis of pedicle screw versus hook instrumentation in posterior spinal fusion of adolescent idiopathic scoliosis. Spine 2004, 29, 2040–2048. [Google Scholar] [CrossRef]
- Liljenqvist, U.; Lepsien, U.; Hackenberg, L.; Niemeyer, T.; Halm, H. Comparative analysis of pedicle screw and hook instrumentation in posterior correction and fusion of idiopathic thoracic scoliosis. Eur. Spine J. 2002, 11, 336–343. [Google Scholar] [CrossRef] [PubMed]
- Suk, S.I.; Kim, J.H.; Cho, K.J.; Kim, S.S.; Lee, J.J.; Han, Y.T. Is anterior release necessary in severe scoliosis treated by posterior segmental pedicle screw fixation? Eur. Spine J. 2007, 16, 1359–1365. [Google Scholar] [CrossRef] [PubMed]
- Geck, M.J.; Macagno, A.; Ponte, A.; Shufflebarger, H.L. The Ponte Procedure. J. Spinal Disord. Technol. 2007, 20, 586–593. [Google Scholar] [CrossRef] [PubMed]
- Bode, L.G.M.; Kluytmans, J.A.J.W.; Wertheim, H.F.L.; Bogaers, D.; Vandenbroucke-Grauls, C.M.J.E.; Roosendaal, R.; Troelstra, A.; Box, A.T.A.; Voss, A.; Van der Tweel, I.; et al. Preventing surgical-site infections in nasal carriers of Staphylococcus aureus. N. Engl. J. Med. 2012, 362, 9–17. [Google Scholar] [CrossRef]
- Darouiche, R.O.; Wall, M.J.; Itani, K.M.F.; Otterson, M.F.; Webb, A.L.; Carrick, M.M.; Miller, H.J.; Awad, S.S.; Crosby, C.T.; Mosier, M.C.; et al. Chlorhexidine–alcohol versus povidone–iodine for surgical-site antisepsis. N. Engl. J. Med. 2010, 362, 18–26. [Google Scholar] [CrossRef]
- Haynes, A.B.; Weiser, T.G.; Berry, W.R.; Lipsitz, S.R.; Breizat, A.H.S.; Dellinger, E.P.; Herbosa, T.; Joseph, S.; Kibatala, P.L.; Lapitan, M.C.M.; et al. A surgical safety checklist to reduce morbidity and mortality in a global population. N. Engl. J. Med. 2009, 360, 491–499. [Google Scholar] [CrossRef]
- Kurz, A.; Sessler, D.I.; Lenhardt, R. Perioperative normothermia to reduce the incidence of surgical-wound infection and shorten hospitalization. N. Engl. J. Med. 1996, 334, 1209–1216. [Google Scholar] [CrossRef]
- Silvestre, M.D.; Bakaloudis, G.; Lolli, F.; Giacomini, S. Late-developing infection following posterior fusion for adolescent idiopathic scoliosis. Eur. Spine J. 2011, 20 (Suppl. S1), 121–127. [Google Scholar] [CrossRef]
- Soultanis, K.C.; Pyrovolou, N.; Zahos, K.A.; Karaliotas, G.I.; Lenti, A.; Liveris, I.; Babis, G.C.; Soucacos, P.N. Late postoperative infection following spinal instrumentation: Stainless steel versus titanium implants. J. Surg. Orthop. Adv. 2008, 17, 193–199. [Google Scholar] [PubMed]
- Schwarzkopf, R.; Chung, C.; Park, J.J.; Walsh, M.; Spivak, J.M.; Steiger, D. Effects of perioperative blood product use on surgical site infection following thoracic and lumbar spinal surgery. Spine 2010, 35, 340–346. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, M.; Sakai, D.; Matsuyama, D.; Yamamoto, Y.; Sato, M.; Mochida, J. Risk factors for surgical site infection following spine surgery: Efficacy of intraoperative saline irrigation. J. Neurosurg. Spine 2010, 12, 540–546. [Google Scholar] [CrossRef]
- Parikh, S.N.; Grice, S.S.; Schnell, B.M.; Salisbury, S.R. Operating room traffic: Is there any role of monitoring it? J. Pediatr. Orthop. 2010, 30, 617–623. [Google Scholar] [CrossRef] [PubMed]
- Gruber, T.; Sharma, A.; Daneschvar, H.; Estfan, B. The hawthorne effect in the assessment of pain by house staff. Am. J. Hosp. Palliat. Care 2003, 20, 231. [Google Scholar] [CrossRef]
- Ramo, B.A.; Stephens, R.B. Repeat surgical interventions following “definitive” instrumentation and fusion for idiopathic scoliosis. Spine 2012, 37, 1211–1217. [Google Scholar] [CrossRef]
- Sponseller, P.D. Pediatric revision spinal deformity surgery: Issues and complications. Spine 2010, 35, 2205–2210. [Google Scholar] [CrossRef] [PubMed]
- Campos, M.; Lori, D.; Weinstein, S. Unanticipated Revision Surgery in Adolescent Idiopathic Scoliosis. Spine 2012, 37, 1048–1053. [Google Scholar] [CrossRef]
- Samdani, A.F.; Belin, E.J.; Bennett, J.T.; Pahys, J.M.; Marks, M.C.; Miyanji, F.; Ebarger, H.L.S.; Lonner, B.S.; Newton, P.O.; Betz, R.R.; et al. Unplanned return to the operating room in patients with adolescent idiopathic scoliosis; are we doing better with pedicle screws? Spine 2013, 38, 1842–1847. [Google Scholar] [CrossRef]
- Kuklo, T.R.; Potter, B.K.; Lenke, L.G.; Polly, D.W.; Sides, B.; Bridwell, K.H. Surgical revision rates of hooks versus hybrid versus screws versus combined anteroposterior spinal fusion for adolescent idiopathic scoliosis. Spine 2007, 32, 2258–2264. [Google Scholar] [CrossRef]
- Lee, S.M.; Suk, S.I.; Chung, E.R. Direct Vertebral Rotation: A New Technique of Three-Dimensional Deformity Correction with Segmental Pedicle Screw Fixation in Adolescent Idiopathic Scoliosis. Spine 2004, 29, 343–349. [Google Scholar] [CrossRef]
- Rose, P.S.; Lenke, L.G.; Bridwell, K.H.; Mulconrey, D.S.; Cronen, G.A.; Buchowski, J.M.; Schwend, R.M.; Sides, B.A. Pedicle screw instrumentation for adult idiopathic scoliosis: An improvement over hook/hybrid fixation. Spine 2009, 34, 852–857. [Google Scholar] [CrossRef] [PubMed]
- Vora, V.; Crawford, A.; Babekhir, N.; Boachie-Adjei, O.; Lenke, L.; Peskin, M.; Charles, G.; Kim, Y. A pedicle screw construct gives an enhanced posterior correction of adolescent idiopathic scoliosis when compared with other constructs: Myth or reality. Spine 2007, 32, 1869–1874. [Google Scholar] [CrossRef] [PubMed]
- Larson, A.N.; Aubin, C.E.; Polly, D.W.; Ledonio, C.G.T.; Lonner, B.S.; Shah, S.A.; Richards, B.S.; Erickson, M.A.; Emans, J.B.; Weinstein, S.L. Are more screws better? A systematic review of anchor density and curve correction in adolescent idiopathic scoliosis. Spine Deform. 2013, 1, 237–247. [Google Scholar] [CrossRef] [PubMed]
- Larson, A.N.; Polly, D.W.; Diamond, B.; Ledonio, C.; Richards, B.S.; Emans, J.B.; Sucato, D.J.; Johnston, C.E. Does higher anchor density result in increased curve correction and improved clinical outcomes in adolescent idiopathic scoliosis? Spine 2014, 39, 571–578. [Google Scholar] [CrossRef] [PubMed]
- Carreon, L.Y.; Sanders, J.O.; Diab, M.; Sucato, D.J.; Sturm, P.F.; Glassman, S.D. The minimum clinically important difference in scoliosis research society-22 appearance, activity, and pain domains after surgical correction of adolescent idiopathic scoliosis. Spine 2010, 35, 2079–2083. [Google Scholar] [CrossRef]
- Bagó, J.; Pérez-Grueso, F.J.S.; Les, E.; Hernández, P.; Pellisé, F. Minimal important differences of the SRS-22 Patient Questionnaire following surgical treatment of idiopathic scoliosis. Eur. Spine J. 2009, 18, 1898–1904. [Google Scholar] [CrossRef]
- Rushton, P.R.P.; Elmalky, M.; Tikoo, A.; Basu, S.; Cole, A.A.; Grevitt, M.P. The effect of metal density in thoracic adolescent idiopathic scoliosis. Eur. Spine. J. 2016, 25, 3324–3330. [Google Scholar] [CrossRef] [PubMed]
- Sanders, J.O.; Haynes, R.; Lighter, D.; Niederpruem, M.; Hollenback, C.; Johnson, L.; Nomura, S.; Arndt, D.; Bush, P.; Santiago, J.; et al. Variation in care among spinal deformity surgeons: Results of a survey of the Shriners Hospitals for Children. Spine 2007, 32, 1444–1449. [Google Scholar] [CrossRef]
- Cheng, I.; Kim, Y.; Gupta, M.C.; Bridwell, K.H.; Hurford, R.K.; Lee, S.S.; Theerajunyaporn, T.; Lenke, L.G. Apical sublaminar wires versus pedicle screws—Which provides better results for surgical correction of adolescent idiopathic scoliosis? Spine 2005, 30, 2104–2112. [Google Scholar] [CrossRef]
- Roach, J.W.; Mehlman, C.T.; Sanders, J.O. Does the outcome of adolescent idiopathic scoliosis surgery justify the rising cost of the procedures? J. Pediatr. Orthop. 2011, 31, S77–S80. [Google Scholar] [CrossRef] [PubMed]
- Le Navéaux, F.; Aubin, C.É.; Larson, A.N.; Polly, D.W., Jr.; Baghdadi, Y.M.; Labelle, H. Implant Distribution in Surgically Instrumented Lenke 1 Adolescent Idiopathic Scoliosis: Does It Affect Curve Correction? Spine 2015, 40, 462–468. [Google Scholar] [CrossRef] [PubMed]
- D’Andrea, L.P.; Betz, R.R.; Lenke, L.G.; Clements, D.H.; Lowe, T.G.; Merola, A.; Haher, T.; Harms, J.; Huss, G.K.; Blanke, K.; et al. Do radiographic parameters correlate with clinical outcomes in adolescent idiopathic scoliosis? Spine 2000, 25, 1795–1802. [Google Scholar] [CrossRef] [PubMed]
- Asher, M.; Lai, S.M.; Burton, D.; Manna, B. The Influence of Spine and Trunk Deformity on Preoperative Idiopathic Scoliosis Patients’ Health-related Quality of Life Questionnaire Responses. Spine 2004, 29, 861–868. [Google Scholar] [CrossRef] [PubMed]
- Parent, E.C.; Wong, D.; Hill, D.; Mahood, J.; Moreau, M.; Raso, V.J.; Lou, E. The association between scoliosis research society-22 scores and scoliosis severity changes at a clinically relevant threshold. Spine 2010, 35, 315–322. [Google Scholar] [CrossRef]
- Sanders, J.O.; Carreon, L.Y.; Sucato, D.J.; Sturm, P.F.; Diab, M. Preoperative and perioperative factors effect on adolescent idiopathic scoliosis surgical outcomes. Spine 2010, 35, 1867–1871. [Google Scholar] [CrossRef]
- Wilson, P.L.; Newton, P.O.; Wenger, D.R.; Haher, T.; Merola, A.; Lenke, L.; Lowe, T.; Clements, D.; Betz, R. A multicenter study analyzing the relationship of a standardized radiographic scoring system of adolescent idiopathic scoliosis and the Scoliosis Research Society outcomes instrument. Spine 2002, 27, 2036–2040. [Google Scholar] [CrossRef]
- Merola, A.A.; Haher, T.R.; Brkaric, M.; Panagopoulos, G.; Mathur, S.; Kohani, O.; Lowe, T.G.; Lenke, L.G.; Wenger, D.R.; Newton, P.O.; et al. A multicenter study of the outcomes of the surgical treatment of adolescent idiopathic scoliosis using the Scoliosis Research Society (SRS) outcome instrument. Spine 2002, 27, 2046–2051. [Google Scholar] [CrossRef]
- Hwang, C.J.; Lee, C.K.; Chang, B.S.; Kim, M.S.; Yeom, J.S.; Choi, J.M. Minimum 5-Year Follow-up Results of Skipped Pedicle Screw Fixation for Flexible Idiopathic Scoliosis: Clinical Article. J. Neurosurg.: Spine 2011, 15, 146–150. [Google Scholar] [CrossRef]
- Uehara, M.; Takahashi, J.; Kuraishi, S.; Shimizu, M.; Ikegami, S.; Futatsugi, T.; Oba, H.; Kato, H. Computer-Assisted Skip Pedicle Screw Fixation for Adolescent Idiopathic Scoliosis. J. Orthop. Sci. 2017, 22, 218–223. [Google Scholar] [CrossRef]
- Tsirikos, A.I.; Mataliotakis, G.; Bounakis, N. Posterior spinal fusion for adolescent idiopathic scoliosis using a convex pedicle screw technique: A novel concept of deformity correction. Bone Jt. J. 2017, 99, 1080–1087. [Google Scholar] [CrossRef]
- Cahill, P.J.; Pahys, J.M.; Asghar, J.; Yaszay, B.; Marks, M.C.; Bastrom, T.P.; Lonner, B.S.; Shah, S.A.; Shufflebarger, H.L.; Newton, P.O.; et al. The Effect of Surgeon Experience on Outcomes of Surgery for Adolescent Idiopathic Scoliosis. J. Bone Jt. Surg. Am. 2014, 16, 1333–1339. [Google Scholar] [CrossRef] [PubMed]
- Cahill, P.J.; Samdani, A.F.; Brusalis, C.M.; Blumberg, B.; Asghar, J.; Bastrom, T.P.; Pasha, S.; Refakis, C.A.; Pahys, J.M.; Flynn, J.M.; et al. Youth and Experience: The Effect of Surgeon Experience on Outcomes in Cerebral Palsy Scoliosis Surgery. Spine Deform. 2018, 6, 54–59. [Google Scholar] [CrossRef] [PubMed]
- Lonner, B.S.; Scharf, C.; Antonacci, D.; Goldstein, Y.; Panagopoulos, G. The learning curve associated with thoracoscopic spinal instrumentation. Spine 2005, 30, 2835–2840. [Google Scholar] [CrossRef] [PubMed]






| Characteristic | Pre-BPGP (34) Median ± IQ | Pos-BPGP (48) Median ± IQ | Mann–Whitney U p Value | Eta-Squared (η) |
|---|---|---|---|---|
| Age (Years) | 14 ± 3.3 | 14 ± 2.8 | 0.59 | 0.004 |
| Pre-op Hb | 12.5±1.8 | 13.8±1.3 | 0.01 | 0.11 |
| Risser | 4 ± 2 | 4 ± 1 | 0.343 | 0.011 |
| Major Cobb angle | 60° ± 17.3 | 60° ± 18.6 | 0.42 | 0.0081 |
| Major Flexibility (%) | 36 ± 23.4 | 36.3 ± 22.5 | 0.862 | 0.001 |
| Levels Fused (n) | 12 ±2.3 | 12 ± 3.0 | 0.98 | 0.001 |
| Operative Time (m) | 260.46 ± 45.4 | 286.72 ± 57.5 | 0.012 | 0.51 |
| Total density (%) | 57.5 ± 16.7 | 66.8 ± 12.03 | 0.002 | 0.114 |
| Density MC (%) | 50 ± 19.05 | 66.6 ± 20.3 | <0.001 | 0.22 |
| Convex_Density (%) | 50 ± 23.8 | 59.57 ± 35.0 | 0.027 | 0.06 |
| Concave_Density (%) | 50 ± 24 | 71.2 ± 28.1 | <0.001 | 0.25 |
| Density/Density MC | 1.22 ± 0 | 1.01 ± 0 | 0.001 | 0.15 |
| Cost (EUR) | 7700 ± 2025 | 8750 ± 2192.50 | 0.003 | 0.11 |
| Characteristic | Pre-BPGP (34) | Pos-BPGP (48) | Chi-Squared Difference (Sig.) | Effect (Odds Ratio) |
|---|---|---|---|---|
| Gender (F) | 77% | 90% | 0.11 | 2.646 |
| Additional Procedures (Yes) | 8.8% | 10.4% | 0.811 | 1.2 |
| Selective (Yes) | 44.1% | 33.3% | 0.312 | 0.633 |
| Hybrid (Yes) | 33.3% | 2.1% | <0.000 | 0.043 |
| Thoracoplasty (Yes) | 55.9% | 41.7% | 0.20 | 0.564 |
| Lenke 1, 2 (N) | 63.6% | 66.7% | 0.647 | 1.238 |
| Lenke 3, 4 (N) | 15.2% | 12.5% | 0.773 | 0.829 |
| Lenke 5, 6 (N) | 21.2% | 20.8% | 0.978 | 0.015 |
| Modificator A | 36.4% | 27.1% | 0.426 | 0.681 |
| Modificator B | 6.1% | 10.4% | 0.469 | 1.86 |
| Modificator C | 55.9% | 62.5% | 0.547 | 1.316 |
| Data | Pre-BPGP (34) | Post-BPGP (48) | p Value | Cohen’s D |
|---|---|---|---|---|
| Immediate (%) | 67.85 (23.20) | 70.10 (17.40) | 0.15 | 0.16 |
| Final (%) | 64.60 (23.68) | 66.50 (14.90) | 0.08 | 0.19 |
| Ratio (Immediate/Final) | 1.08 (0.14) | 1.02 (0.14) | 0.14 | 0.16 |
| Complications (%) | 26.5 (9) | 4.2 (2) | 0.01 | 0.12 |
| Returns to OR (%) | 26.5 (9) | 4.2 (2) | 0.01 | 0.12 |
| Score | Pre-BPGP | Post-BPGP | S (p) | Cohen’s D |
|---|---|---|---|---|
| SRS-22 total | 4.37 ± 1.92 | 4.52 ± 0.49 | 0.114 | 0.002 |
| Function | 4.2 ± 0.5 | 4.2 ± 0.6 | 0.657 | 0 |
| Pain | 4.4 ± 0.8 | 4.6 ± 0.8 | 0.122 | 0.25 |
| Self-image | 4.45 ± 1 | 4.4 ± 0.6 | 0.296 | 0.002 |
| Mental health | 4.2 ± 0.8 | 4.3 ± 1 | 0.263 | 0.11 |
| Satisfaction | 5 ± 0.5 | 5 ± 0 | 0.126 | 0 |
| Data | Corr 1 | Corr 2 | Ration Corr 1/Corr 2 | |||
|---|---|---|---|---|---|---|
| Beta | p Value | Beta | p Value | Beta | p Value | |
| Density | −0.393 | 0.01 | −0.180 | 0.237 | 0.017 | 0.911 |
| Convex_D | 0.017 | 0.899 | −0.138 | 0.306 | −0.3 | 0.027 |
| Concave_D | 0.293 | 0.038 | 0.263 | 0.069 | −0.011 | 0.937 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fernandes, P.; Flores, I.; Soares do Brito, J. Benefits of Best Practice Guidelines in Spine Fusion: Comparable Correction in AIS with Higher Density and Fewer Complications. Healthcare 2023, 11, 1566. https://doi.org/10.3390/healthcare11111566
Fernandes P, Flores I, Soares do Brito J. Benefits of Best Practice Guidelines in Spine Fusion: Comparable Correction in AIS with Higher Density and Fewer Complications. Healthcare. 2023; 11(11):1566. https://doi.org/10.3390/healthcare11111566
Chicago/Turabian StyleFernandes, Pedro, Isabel Flores, and Joaquim Soares do Brito. 2023. "Benefits of Best Practice Guidelines in Spine Fusion: Comparable Correction in AIS with Higher Density and Fewer Complications" Healthcare 11, no. 11: 1566. https://doi.org/10.3390/healthcare11111566
APA StyleFernandes, P., Flores, I., & Soares do Brito, J. (2023). Benefits of Best Practice Guidelines in Spine Fusion: Comparable Correction in AIS with Higher Density and Fewer Complications. Healthcare, 11(11), 1566. https://doi.org/10.3390/healthcare11111566






