Using Twitter Data Analysis to Understand the Perceptions, Beliefs, and Attitudes about Pharmacotherapy Used in Rheumatology: An Observational Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Data Source
2.2. Search Tool and Data Collection
2.3. Content Analysis Process and Creation of the Codebook
2.4. Ethical Considerations
2.5. Statistical Analysis
3. Results
3.1. Twitter Community Shows a Major Interest in the Most Prescribed Drugs
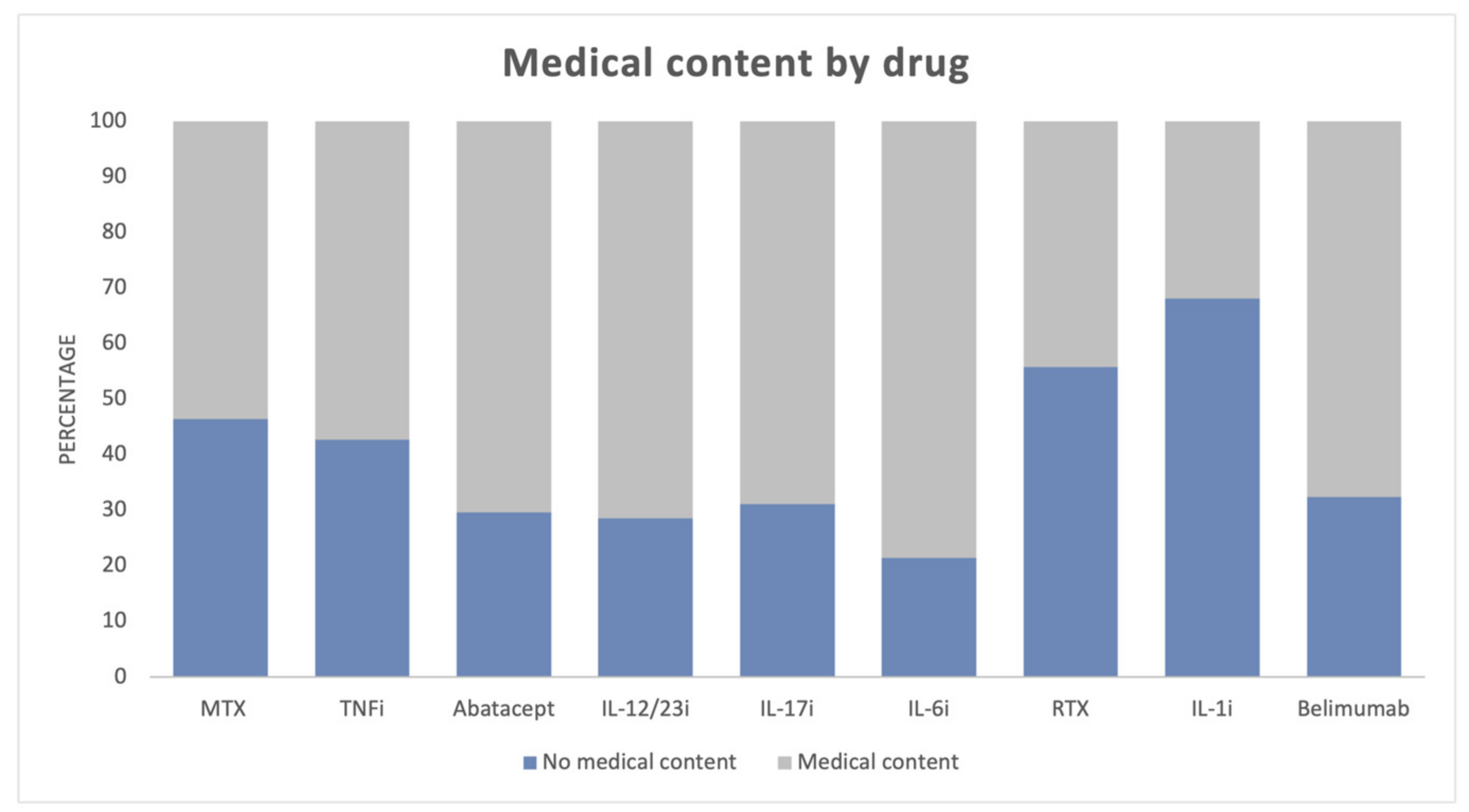
3.2. More Medical Content Is Tweeted Than Non-Medical Content and Fake Content Is Very Low
3.3. The Distribution of Medical and Non-Medical Content Varies According to the Type of User
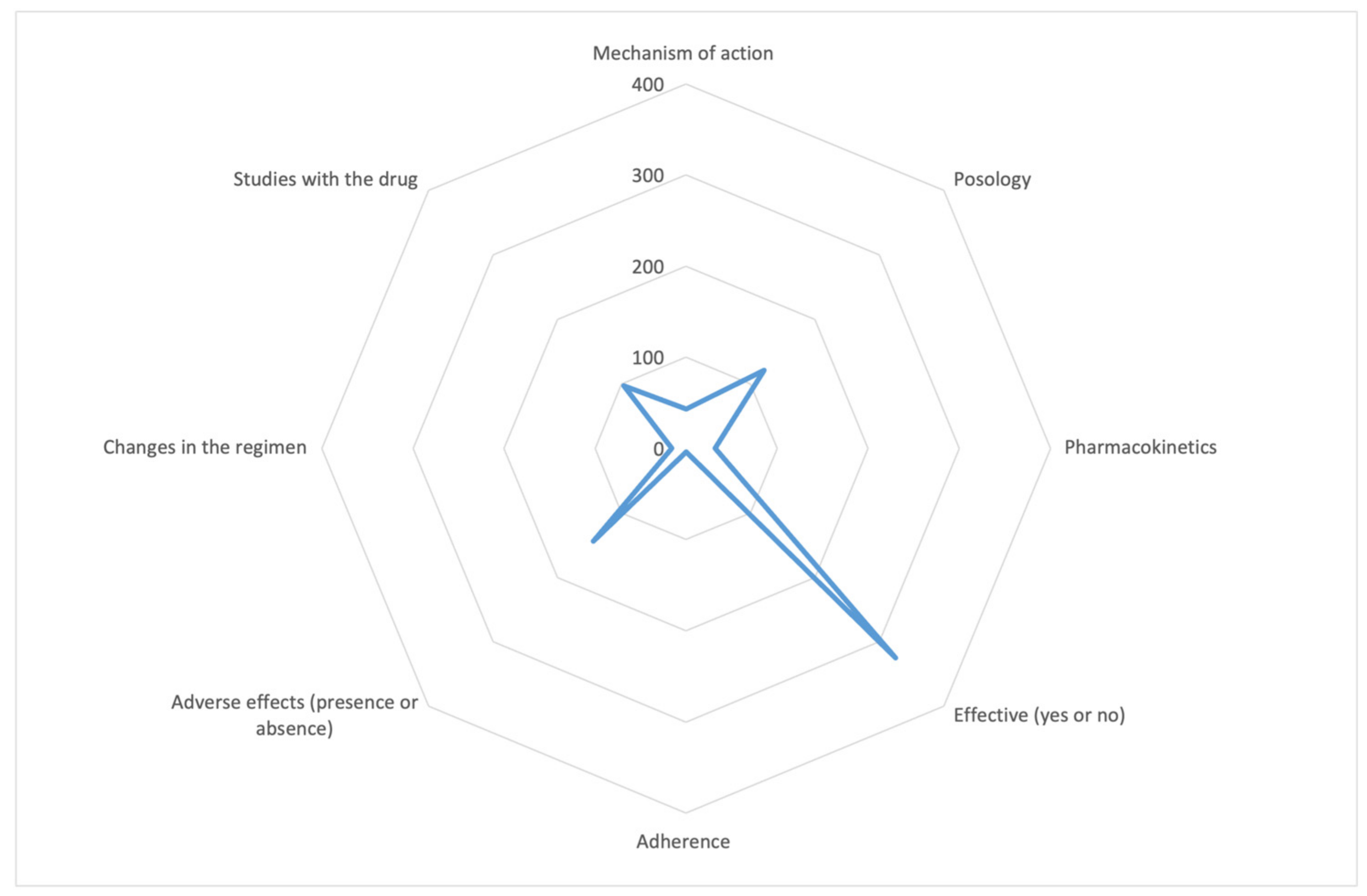
There Are Few Tweets about Adherence
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Demographics of Internet and Home Broadband Usage in the United States|Pew Research Center [Internet]. Available online: https://www.pewresearch.org/internet/fact-sheet/internet-broadband/ (accessed on 1 April 2022).
- Demographics of Social Media Users and Adoption in the United States|Pew Research Center [Internet]. Available online: https://www.pewresearch.org/internet/fact-sheet/social-media/ (accessed on 25 January 2023).
- Demographics of Social Media Users and Adoption in the United States|Pew Research Center [Internet]. Available online: https://www.pewresearch.org/internet/2021/04/07/social-media-use-in-2021/ (accessed on 1 April 2022).
- You Are What You Tweet: Analyzing Twitter for Public Health|Proceedings of the International AAAI Conference on Web and Social Media [Internet]. Available online: https://ojs.aaai.org/index.php/ICWSM/article/view/14137 (accessed on 1 April 2022).
- Lee, J.L.; DeCamp, M.; Dredze, M.; Chisolm, M.S.; Berger, Z.D. What Are Health-Related Users Tweeting? A Qualitative Content Analysis of Health-Related Users and Their Messages on Twitter. J. Med. Internet Res. 2014, 16, e237. [Google Scholar] [CrossRef] [PubMed]
- Yom-Tov, E.; Borsa, D.; Cox, I.J.; McKendry, R.A. Detecting Disease Outbreaks in Mass Gatherings Using Internet Data. J. Med. Internet Res. 2014, 16, e154. [Google Scholar] [CrossRef] [PubMed]
- Yuan, P.; Bare, M.G.; Johnson, M.O.; Saberi, P. Using Online Social Media for Recruitment of Human Immunodeficiency Virus-Positive Participants: A Cross-Sectional Survey. J. Med. Internet Res. 2014, 16, e117. [Google Scholar] [CrossRef] [PubMed]
- Nakagawa, K.; Yang, N.T.; Wilson, M.; Yellowlees, P. Twitter Usage Among Physicians From 2016 to 2020: Algorithm Development and Longitudinal Analysis Study. J. Med. Internet Res. 2022, 24, e37752. [Google Scholar] [CrossRef] [PubMed]
- Lawrence, R.C.; Felson, D.T.; Helmick, C.G.; Arnold, L.M.; Choi, H.; Deyo, R.A.; Gabriel, S.; Hirsch, R.; Hochberg, M.C.; Hunder, G.G.; et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis Rheum. 2008, 58, 26–35. [Google Scholar] [CrossRef]
- Helmick, C.G.; Felson, D.T.; Lawrence, R.C.; Gabriel, S.; Hirsch, R.; Kwoh, C.K.; Liang, M.H.; Kremers, H.M.; Mayes, M.D.; Merkel, P.A.; et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part I. Arthritis Rheum. 2008, 58, 15–25. [Google Scholar] [CrossRef] [PubMed]
- Prevalence and Most Common Causes of Disability Among Adults—United States, 2005 [Internet]. Available online: https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5816a2.htm (accessed on 4 April 2022).
- Alsobayel, H. Use of Social Media for Professional Development by Health Care Professionals: A Cross-Sectional Web-Based Survey. JMIR Med. Educ. 2016, 2, e15. [Google Scholar] [CrossRef] [PubMed]
- Nikiphorou, E.; Studenic, P.; Ammitzbøll, C.G.; Canavan, M.; Jani, M.; Ospelt, C.; Berenbaum, F. Social media use among young rheumatologists and basic scientists: Results of an international survey by the Emerging EULAR Network (EMEUNET). Ann. Rheum. Dis. 2017, 76, 712–715. [Google Scholar] [CrossRef] [PubMed]
- Kamruzzaman, A.K.M.; Chowdhury, M.R.; Islam, M.N.; Sultan, I.; Ahmed, S.; Shahin, A.; Alam, M.M.; Azad, M.A.; Hassan, M.M.; Amin, M.Z.; et al. The knowledge level of rheumatoid arthritis patients about their disease in a developing country. A study in 168 Bangladeshi RA patients. Clin. Rheumatol. 2020, 39, 1315–1323. [Google Scholar] [CrossRef]
- Bozbaş, G.T.; Gürer, G. Medical GGAC the J of, 2018 Undefined. The Knowledge Level of Turkish Rheumatoid Arthritis Patients about Their Diseases. dergipark.org.tr [Internet]. Available online: https://dergipark.org.tr/en/pub/anadoluklin/issue/34816/325831?publisher=hsv (accessed on 12 September 2022).
- Venuturupalli, R.S.; Sufka, P.; Bhana, S. Digital Medicine in Rheumatology: Challenges and Opportunities. Rheum. Dis. Clin. North Am. 2019, 45, 113–126. [Google Scholar] [CrossRef]
- American College of Rheumatology (@ACRheum)/Twitter [Internet]. Available online: https://twitter.com/acrheum?lang=en (accessed on 4 April 2022).
- Negrón, J.B. #EULAR2018: The Annual European Congress of Rheumatology—A Twitter hashtag analysis. Rheumatol. Int. 2019, 39, 893–899. [Google Scholar] [PubMed]
- Venuturupalli, S.; Kumar, A.; Bunyan, A.; Davuluri, N.; Fortune, N.; Reuter, K. Using Patient-Reported Health Data From Social Media to Identify Diverse Lupus Patients and Assess Their Symptom and Medication Expressions: A Feasibility Study. Arthritis Care Res. 2023, 75, 365–372. [Google Scholar] [CrossRef] [PubMed]
- Abbasi-Perez, A.; Alvarez-Mon, M.A.; Donat-Vargas, C.; Ortega, M.A.; Monserrat, J.; Perez-Gomez, A.; Sanz, I.; Alvarez-Mon, M. Analysis of Tweets Containing Information Related to Rheumatological Diseases on Twitter. Int. J. Environ. Res. Public Health 2021, 18, 9094. [Google Scholar] [CrossRef] [PubMed]
- De Castro, N.M.L.; Samartín-Ucha, M.; Martín-Vila, A.; Álvarez-Payero, M.; Piñeiro-Corrales, G.; Pego-Reigosa, J.M. Content analysis of Twitter in relation to biological treatments for chronic inflammatory arthropathies: An exploratory study. Eur. J. Hosp. Pharm. 2019, 26, 124. [Google Scholar] [CrossRef]
- Kataria, S.; Ravindran, V. Digital health: A new dimension in rheumatology patient care. Rheumatol. Int. 2018, 38, 1949–1957. [Google Scholar] [CrossRef]
- Erdogan, M.; Aydin, O.; Seyahi, E. Patients with rheumatic diseases are ready to use social media in clinical practice; what about rheumatologists? A cross-sectional survey. Rheumatol. Int. 2022, 42, 717. [Google Scholar] [CrossRef]
- Kwan, Y.H.; Phang, J.K.; Woon, T.H.; Liew, J.W.; Dubreuil, M.; Proft, F.; Ramiro, S.; Molto, A.; Navarro-Compán, V.; de Hooge, M.; et al. Social Media Use Among Members of the Assessment of Spondyloarthritis International Society: Results of a Web-Based Survey. J. Med. Internet Res. 2023, 25, e39155. [Google Scholar] [CrossRef]
- Schnall, R.; Liu, J.; Iribarren, S. Information Sources of Self-Care Strategies for Persons Living with HIV. Int. J. Med. Inform. 2018, 111, 1–6. [Google Scholar] [CrossRef]
- Reilly, E.; Sengupta, R. Back pain, ankylosing spondylitis and social media usage; a descriptive analysis of current activity. Rheumatol. Int. 2020, 40, 1493–1499. [Google Scholar] [CrossRef]
- Smolen, J.S.; Landewé, R.; Bijlsma, J.; Burmester, G.; Chatzidionysiou, K.; Dougados, M.; Nam, J.; Ramiro, S.; Voshaar, M.; van Vollenhoven, R.; et al. EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2016 update. Ann. Rheum. Dis. 2017, 76, 960–977. [Google Scholar] [CrossRef]
- Fanouriakis, A.; Kostopoulou, M.; Alunno, A.; Aringer, M.; Bajema, I.; Boletis, J.N.; Cervera, R.; Doria, A.; Gordon, C.; Govoni, M.; et al. 2019 update of the EULAR recommendations for the management of systemic lupus erythematosus. Ann. Rheum. Dis. 2019, 78, 736–745. [Google Scholar] [CrossRef] [PubMed]
- Cruz, B.H.; Garnica, I.U.; Parera, R.S.; Romero, E.R.; Gutiérrez, J.C.; Sánchez, A.G.; Escalera, C.R.; Sarabia, F.N. Disease-modifying antirheumatic drug prescription patterns in adult rheumatoid arthritis patients in routine clinical practice in Spain. Eur. J. Rheumatol. 2020, 7, 149–157. [Google Scholar] [CrossRef] [PubMed]
- Otón, T.; Carmona, L.; Andreu, J.L. Patient’s experiences of the barriers and facilitators to Methotrexate. Musculoskeletal Care 2022, 20, 158–166. [Google Scholar] [CrossRef] [PubMed]
- Pasma, A.; Van ’t Spijker, A.; Luime, J.J.; Walter, M.J.M.; Busschbach, J.J.V.; Hazes, J.M.W. Facilitators and Barriers to Adherence in the Initiation Phase of Disease-modifying Antirheumatic Drug (DMARD) Use in Patients with Arthritis Who Recently Started Their First DMARD Treatment. J. Rheumatol. 2015, 42, 379–385. [Google Scholar] [CrossRef] [PubMed]
- Leonardo, N.; Lester, S.; Graham, M.; Barrett, C.; Whittle, S.; Rowett, D.; Buchbinder, R.; Hill, C.L. Selection and perception of methotrexate treatment information in people with rheumatoid arthritis. Int. J. Rheum. Dis. 2020, 23, 805–812. [Google Scholar] [CrossRef]
- Pawar, A.; Desai, R.J.; Gautam, N.; Kim, S.C. Risk of admission to hospital for serious infection after initiating tofacitinib versus biologic DMARDs in patients with rheumatoid arthritis: A multidatabase cohort study. Lancet Rheumatol. 2020, 2, e84–e98. [Google Scholar] [CrossRef]
- Giles, J.T.; Sattar, N.; Gabriel, S.; Ridker, P.M.; Gay, S.; Warne, C.; Musselman, D.; Brockwell, L.; Shittu, E.; Klearman, M.; et al. Cardiovascular Safety of Tocilizumab Versus Etanercept in Rheumatoid Arthritis: A Randomized Controlled Trial. Arthritis Rheumatol. 2020, 72, 31–40. [Google Scholar] [CrossRef]
- Alvarez-Mon, M.A.; Llavero-Valero, M.; Del Barco, A.A.; Zaragozá, C.; Ortega, M.A.; Lahera, G.; Quintero, J.; Alvarez-Mon, M. Areas of Interest and Attitudes Toward Antiobesity Drugs: Thematic and Quantitative Analysis Using Twitter. J. Med. Internet Res. 2021, 23, e24336. [Google Scholar] [CrossRef]
- Madenidou, A.V.; Jeffries, A.; Madenidou, A.V.; Varughese, S.; Jones, S.; Sari-Kouzel, H.; Veevers, H.; Rao, C. Switching patients with inflammatory arthritis from Etanercept (Enbrel®) to the biosimilar drug, SB4 (Benepali®): A single-centre retrospective observational study in the UK and a review of the literature. Mediterr. J. Rheumatol. 2019, 30 (Suppl 1), 69. [Google Scholar] [CrossRef]
- Xu, H.; Li, Z.; Wu, J.; Xing, Q.; Shi, G.; Li, J.; Liu, X.; Wu, L.; Li, X.; Tan, W.; et al. IBI303, a biosimilar to adalimumab, for the treatment of patients with ankylosing spondylitis in China: A randomised, double-blind, phase 3 equivalence trial. Lancet Rheumatol. 2019, 1, e35–e43. [Google Scholar] [CrossRef]
- Hazlewood, G.S.; Bombardier, C.; Tomlinson, G.; Marshall, D. A Bayesian model that jointly considers comparative effectiveness research and patients’ preferences may help inform GRADE recommendations: An application to rheumatoid arthritis treatment recommendations. J. Clin. Epidemiol. 2018, 93, 56–65. [Google Scholar] [CrossRef] [PubMed]
- Hazlewood, G.S. Measuring Patient Preferences: An Overview of Methods with a Focus on Discrete Choice Experiments. Rheum. Dis. Clin. N. Am. 2018, 44, 337–347. [Google Scholar] [CrossRef] [PubMed]
- Hazlewood, G.S.; Bombardier, C.; Tomlinson, G.; Thorne, C.; Bykerk, V.P.; Thompson, A.; Tin, D.; Marshall, D.A. Treatment preferences of patients with early rheumatoid arthritis: A discrete-choice experiment. Rheumatology 2016, 55, 1959–1968. [Google Scholar] [CrossRef] [PubMed]
- Adherence to Long-Term Therapies: Evidence for Action [Internet]. Available online: https://apps.who.int/iris/handle/10665/42682 (accessed on 29 August 2022).
- Garcia-Gonzalez, A.; Richardson, M.; Garcia Popa-Lisseanu, M.; Cox, V.; Kallen, M.A.; Janssen, N.; Ng, B.; Marcus, D.M.; Reveille, J.D.; Suarez-Almazor, M.E. Treatment adherence in patients with rheumatoid arthritis and systemic lupus erythematosus. Clin. Rheumatol. 2008, 27, 883–889. [Google Scholar] [CrossRef]
- Vangeli, E.; Bakhshi, S.; Baker, A.; Fisher, A.; Bucknor, D.; Mrowietz, U.; Östör, A.J.; Peyrin-Biroulet, L.; Lacerda, A.P.; Weinman, J. A Systematic Review of Factors Associated with Non-Adherence to Treatment for Immune-Mediated Inflammatory Diseases. Adv. Ther. 2015, 32, 983–1028. [Google Scholar] [CrossRef]
- Alvarez-Mon, M.A.; de Anta, L.; Llavero-Valero, M.; Lahera, G.; Ortega, M.A.; Soutullo, C.; Quintero, J.; Asunsolo del Barco, A.; Alvarez-Mon, M. Areas of Interest and Attitudes towards the Pharmacological Treatment of Attention Deficit Hyperactivity Disorder: Thematic and Quantitative Analysis Using Twitter. J. Clin. Med. 2021, 10, 2668. [Google Scholar] [CrossRef]
- Choi, I.A.; Kim, J.H.; Chang, S.H.; Song, R.; Ha, Y.J.; Kim, H.W.; Lee, J.S.; Choi, B.; Oh, Y.J.; Moon, K.W. Patient perspectives on biological treatments for inflammatory arthritis: A multi-center study in Korea. Arch. Rheumatol. 2021, 36, 499–509. [Google Scholar] [CrossRef]
- Singh, J.A.; Tornberg, H.; Goodman, S.M. Pop a pill or give myself a shot? Patient perspectives of disease-modifying anti-rheumatic drug choice for rheumatoid arthritis. Joint Bone Spine 2021, 88, 105053. [Google Scholar] [CrossRef]
- Smolen, J.S.; Landewé, R.B.M.; Bijlsma, J.W.J.; Burmester, G.R.; Dougados, M.; Kerschbaumer, A.; McInnes, I.B.; Sepriano, A.; van Vollenhoven, R.F.; de Wit, M.; et al. EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2019 update. Ann. Rheum. Dis. 2020, 79, S685–S699. [Google Scholar] [CrossRef]
- Gossec, L.; Baraliakos, X.; Kerschbaumer, A.; De Wit, M.; McInnes, I.; Dougados, M.; Primdahl, J.; McGonagle, D.G.; Aletaha, D.; Balanescu, A.; et al. EULAR recommendations for the management of psoriatic arthritis with pharmacological therapies: 2019 update. Ann. Rheum. Dis. 2020, 79, S700–S712. [Google Scholar] [CrossRef]
- Greenwald, M.W.; Shergy, W.J.; Kaine, J.L.; Sweetser, M.T.; Gilder, K.; Linnik, M.D. Evaluation of the safety of rituximab in combination with a tumor necrosis factor inhibitor and methotrexate in patients with active rheumatoid arthritis: Results from a randomized controlled trial. Arthritis Rheum. 2011, 63, 622–632. [Google Scholar] [CrossRef] [PubMed]
- Schulze-Koops, H.; Krueger, K.; Vallbracht, I.; Hasseli, R.; Skapenko, A. Increased risk for severe COVID-19 in patients with inflammatory rheumatic diseases treated with rituximab. Ann. Rheum. Dis. 2020, 80, e67. [Google Scholar] [CrossRef] [PubMed]
- Marco-Franco, J.E.; Pita-Barros, P.; Vivas-Orts, D.; González-De-Julián, S.; Vivas-Consuelo, D. COVID-19, Fake News, and Vaccines: Should Regulation Be Implemented? Int. J. Environ. Res. Public Health 2021, 18, 744. [Google Scholar] [CrossRef]
- Alsyouf, M.; Stokes, P.; Hur, D.; Amasyali, A.; Ruckle, H.; Hu, B. ‘Fake News’ in urology: Evaluating the accuracy of articles shared on social media in genitourinary malignancies. BJU Int. 2019, 124, 701–706. [Google Scholar] [CrossRef] [PubMed]
- Seoane-Mato, D.; Sánchez-Piedra, C.; Silva-Fernández, L.; Sivera, F.; Blanco, F.J.; Pérez Ruiz, F.; Juan-Mas, A.; Pego-Reigosa, J.M.; Narváez, J.; Martí, N.Q.; et al. Prevalence of rheumatic diseases in adult population in Spain (EPISER 2016 study): Aims and methodology. Reumatol. Clin. 2019, 15, 90–96. [Google Scholar] [CrossRef] [PubMed]
- Sangha, O. Epidemiology of rheumatic diseases. Rheumatology 2000, 39 (Suppl 2), 3–12. [Google Scholar] [CrossRef]
- Reuter, K.; Danve, A.; Deodhar, A. Harnessing the power of social media: How can it help in axial spondyloarthritis research? Curr. Opin. Rheumatol. 2019, 31, 321–328. [Google Scholar] [CrossRef]
- Pehlivan, Y.; Orucoglu, N.; Pehlivan, S.; Kimyon, G.; Zengin, O.; Kucuk, A.; Sahin, A.; Tomas, N.; Oksuz, M.F.; Kisacik, B.; et al. Patients’ concerns regarding biological agents in rheumatology. Int. J. Rheum. Dis. 2018, 21, 1219–1226. [Google Scholar] [CrossRef]
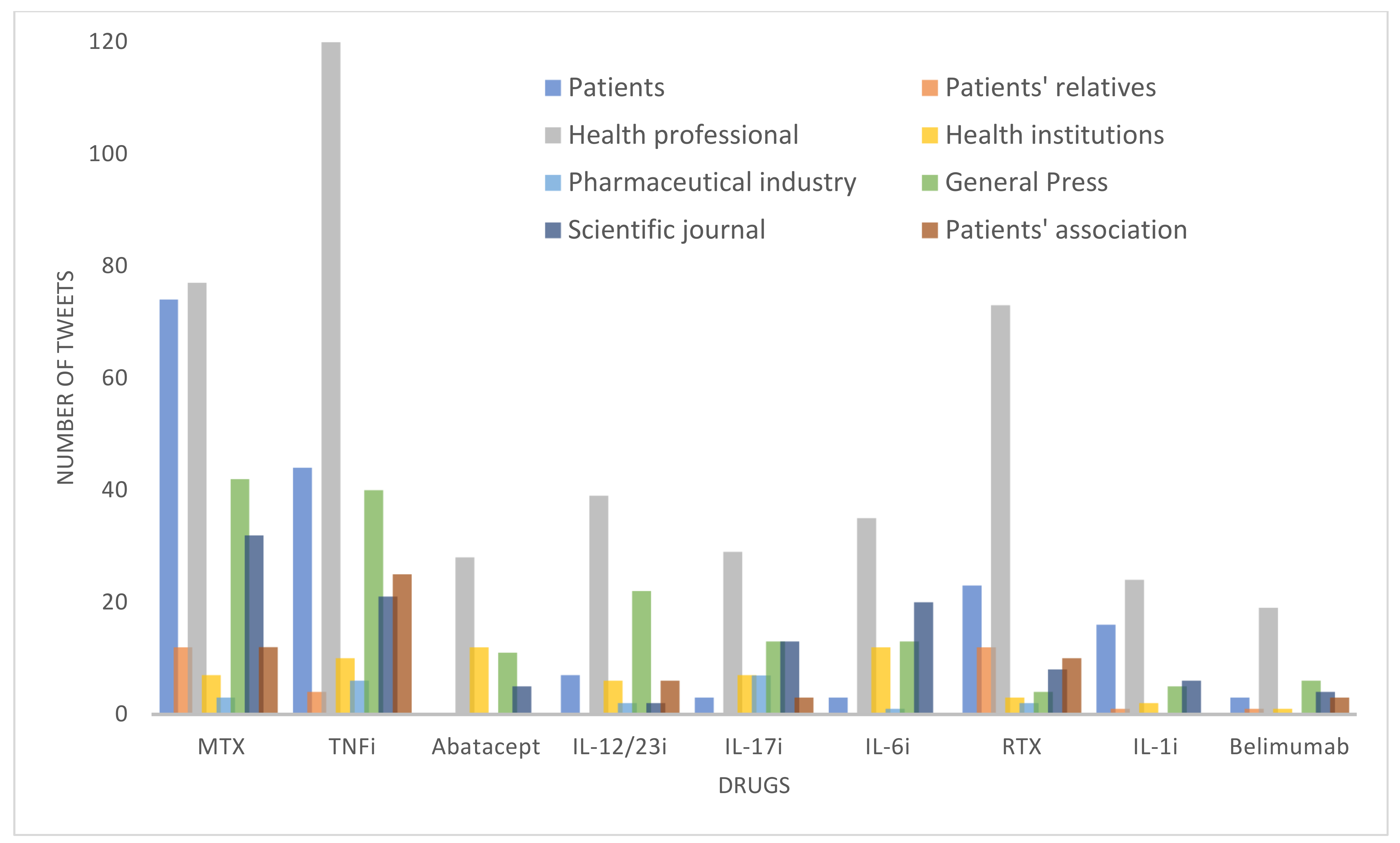

| MTX | TNFi | Abata-cept | IL-12/23i | IL-17i | Anti-IL 6 | RTX | IL-1i | Belimu-mab | TOTAL | |
|---|---|---|---|---|---|---|---|---|---|---|
| Undetermined | 10 | 10 | 8 | 0 | 2 | 0 | 3 | 0 | 0 | 33 |
| Patient | 74 | 44 | 0 | 7 | 3 | 3 | 23 | 16 | 3 | 173 |
| Patients’ relatives | 12 | 4 | 0 | 0 | 0 | 0 | 12 | 1 | 1 | 30 |
| Health professional | 77 | 121 | 28 | 39 | 29 | 35 | 73 | 24 | 19 | 445 |
| Health institution | 7 | 10 | 12 | 6 | 7 | 12 | 3 | 2 | 1 | 60 |
| Pharmaceutical industry | 3 | 6 | 0 | 2 | 7 | 1 | 2 | 0 | 0 | 21 |
| General press | 42 | 40 | 11 | 22 | 13 | 13 | 4 | 5 | 6 | 156 |
| Scientific journal | 32 | 21 | 5 | 2 | 13 | 20 | 8 | 6 | 4 | 111 |
| Patients’ association | 12 | 25 | 0 | 6 | 3 | 0 | 10 | 1 | 3 | 60 |
| Total | 269 | 281 | 64 | 84 | 77 | 84 | 138 | 55 | 37 | 1.089 |
| (%) | MTX | TNFi | Abatacept | IL-12/23i | IL-17i | Anti-IL 6 | RTX | IL-1i | Belimumab |
|---|---|---|---|---|---|---|---|---|---|
| Non-medical content | 46.47 | 42.7 | 29.69 | 28.57 | 31.17 | 21.43 | 55.8 | 68.09 | 32.43 |
| Medical content | 53.53 | 57.3 | 70.31 | 71.43 | 68.83 | 78.57 | 44.2 | 31.91 | 67.57 |
| % | MTX | TNFi | Abatacept | IL-12/23i | IL-17i | Anti-IL 6 | RTX | IL-1i | Belimumab | TOTAL |
|---|---|---|---|---|---|---|---|---|---|---|
| Not applicable | 35.42 | 20.5 | 35.56 | 25 | 5.66 | 6.06 | 8.2 | 23.8 | 8 | 21.07 |
| Scientific literature | 59.72 | 79.95 | 64.44 | 75 | 94.34 | 92.42 | 91.8 | 76.1 | 92 | 77.68 |
| Fake | 4.86 | 0 | 0 | 0 | 0 | 1.52 | 0 | 0 | 0 | 1.30 |
| User | No Medical Content, n (%) | Medical Content n (%) | TOTAL n (%) |
|---|---|---|---|
| Undetermined | 27 (81.82) | 6 (18.18) | 33 (100) |
| Patient | 165 (95.38) | 8 (4.62) | 173 (100) |
| Patients’ relatives | 29 (96.67) | 1 (3.33) | 30 (100) |
| Health professional | 145 (32.58) | 300 (67.42) | 445 (100) |
| Health institution | 17 (28.33) | 43 (71.67) | 60 (100) |
| Pharmaceutical industry | 13 (61.9) | 8 (38.1) | 21 (100) |
| General press | 20 (12.82) | 136 (87.18) | 156 (100) |
| Scientific journal | 3 (2.7) | 108 (97.3) | 111 (100) |
| Patients’ association | 34 (56.67) | 26 (43.33) | 60 (100) |
| Total | 453 (41.6) | 636 (58.4) | 1.089 (100) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abbasi-Perez, A.; Alvarez-Mon, M.A.; Donat-Vargas, C.; Ortega, M.A.; Monserrat, J.; Perez-Gomez, A.; Alvarez-Mon, M. Using Twitter Data Analysis to Understand the Perceptions, Beliefs, and Attitudes about Pharmacotherapy Used in Rheumatology: An Observational Study. Healthcare 2023, 11, 1526. https://doi.org/10.3390/healthcare11111526
Abbasi-Perez A, Alvarez-Mon MA, Donat-Vargas C, Ortega MA, Monserrat J, Perez-Gomez A, Alvarez-Mon M. Using Twitter Data Analysis to Understand the Perceptions, Beliefs, and Attitudes about Pharmacotherapy Used in Rheumatology: An Observational Study. Healthcare. 2023; 11(11):1526. https://doi.org/10.3390/healthcare11111526
Chicago/Turabian StyleAbbasi-Perez, Adrian, Miguel Angel Alvarez-Mon, Carolina Donat-Vargas, Miguel A. Ortega, Jorge Monserrat, Ana Perez-Gomez, and Melchor Alvarez-Mon. 2023. "Using Twitter Data Analysis to Understand the Perceptions, Beliefs, and Attitudes about Pharmacotherapy Used in Rheumatology: An Observational Study" Healthcare 11, no. 11: 1526. https://doi.org/10.3390/healthcare11111526
APA StyleAbbasi-Perez, A., Alvarez-Mon, M. A., Donat-Vargas, C., Ortega, M. A., Monserrat, J., Perez-Gomez, A., & Alvarez-Mon, M. (2023). Using Twitter Data Analysis to Understand the Perceptions, Beliefs, and Attitudes about Pharmacotherapy Used in Rheumatology: An Observational Study. Healthcare, 11(11), 1526. https://doi.org/10.3390/healthcare11111526











